Spine surgery is a complex and delicate medical procedure that sometimes requires precise and accurate pedicle screw placement to ensure successful outcomes. Pedicle screw malposition can lead to severe neurovascular injuries (1–4). Efficient and accurate screw placement is fundamental in reducing iatrogenic complications and improving surgical outcomes. The limitations of human hands and visualization in achieving such precision can be challenging. Robotic assistance in spinal surgery minimizes these human errors. It ensures patient safety (5). Robot-assisted pedicle screw insertion has been introduced, to improve accuracy (6). Pedicle screw misplacement rates using conventional techniques range from 30% in the lumbar spine to 55% in the thoracic spine (7, 8). In contrast, a study has demonstrated that robotic-assisted pedicle screw placement achieves success rates exceeding 90% (9). A recent meta-analysis revealed that robotic-assisted techniques have a significantly lower complication rate compared to the freehand method (4.83% vs. 14.97%). However, the robotic-assisted group did not show a significant advantage in clinical efficacy (10). This technical note aims to describe the steps in performing robotic assistance pedicle screw placement in thoracolumbar spine surgery.
Materials and equipments Robotic device and patient positioningIn this article, a robotic ExcelsiusGPS (Globus Medical; Audobon, PA, USA) for pedicle screw placement in thoracolumbar surgery was used (Figure 1) (11). The patient is positioned prone on a Jackson table (Figure 2). An area beneath the table is needed to place the image intensifier. Tools used in the procedure are shown in Figure 3.
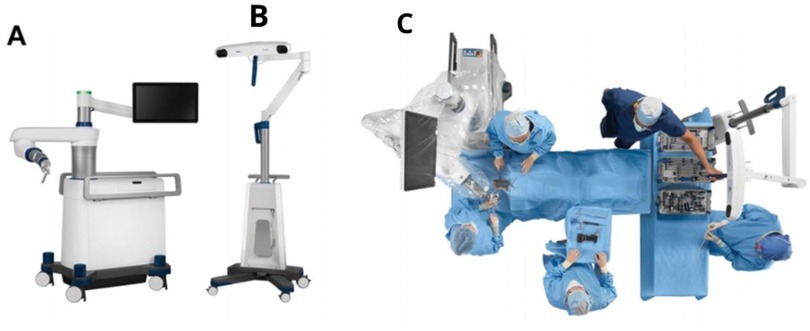
Figure 1. (A) ExclesiusGPS with a floor-fixable base and rigid robotic arm. (B) Navigation camera (C) Simulated operating theater using ExclesiusGPS (11).

Figure 2. The patient is positioned on a Jackson table. A cushion and an armrest can be used under the patient to ensure proper positioning and comfort during the procedure.

Figure 3. Tools used in the procedure. (1) Scalpel, (2A) Low profile quattro spike, bine clamp, and guide post, (2B) Surveillance marker, (3) Awl and array, (4) Drill and array, (5) High burr and array, (6) Tapper and array, (7) Dynamic Reference Base, (8) Intraoperative Cone-beam Tomography.
Methods Surgical planning/workflowSeveral surgical workflows can be applied: preoperative, fluoroscopy, and intraoperative. This technical note will discuss only the intraoperative workflow. An intraoperative CT scan using O-arm (Medtronic Sofamor Danek, Inc., Memphis, TN) is performed (Figure 4) to allow real-time imaging screw placement planning.
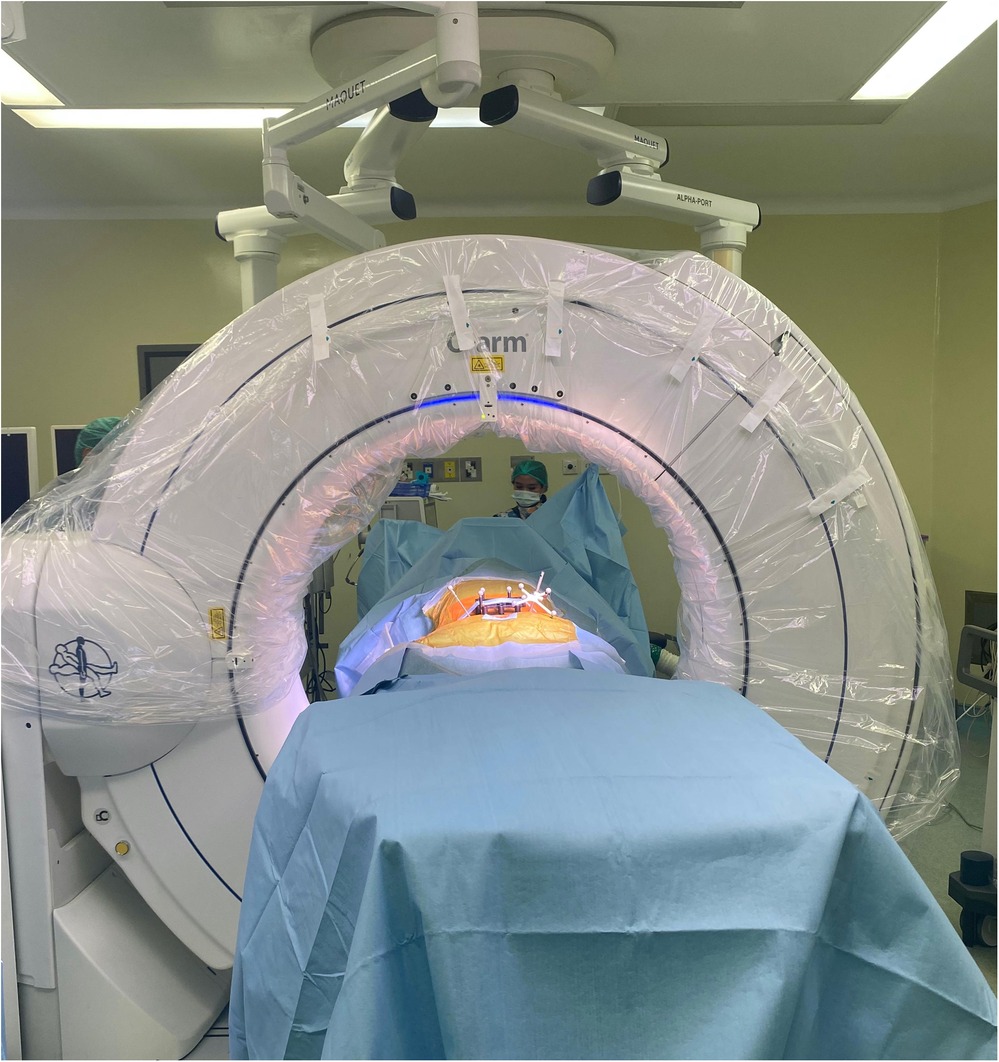
Figure 4. Intraoperative CT scan using O-arm for intraoperative workflow.
Placement of dynamic reference base & ICTThe DRB (dynamic reference base) was positioned with a low-profile quattro spike in the right posterior superior iliac spine (PSIS) with a stab incision and placed within 18 cm of the surgical field. The surveillance marker (SM) was placed in the left PSIS (Figure 5). The ICT (Intraoperative Cone-Beam Tomography) was attached to the spinous process and positioned near the desired screw level, parallel to the floor, and as close as possible to the skin without touching it. The DRB and ICT must remain visible to the navigation camera, even after inserting the O-arm. Proper positioning and stability of the DRB, ICT, and surveillance marker (SM), along with verifying anatomical landmarks before screw planning, are crucial for ensuring accuracy and effectiveness during surgery and achieving reliable surgical outcomes.
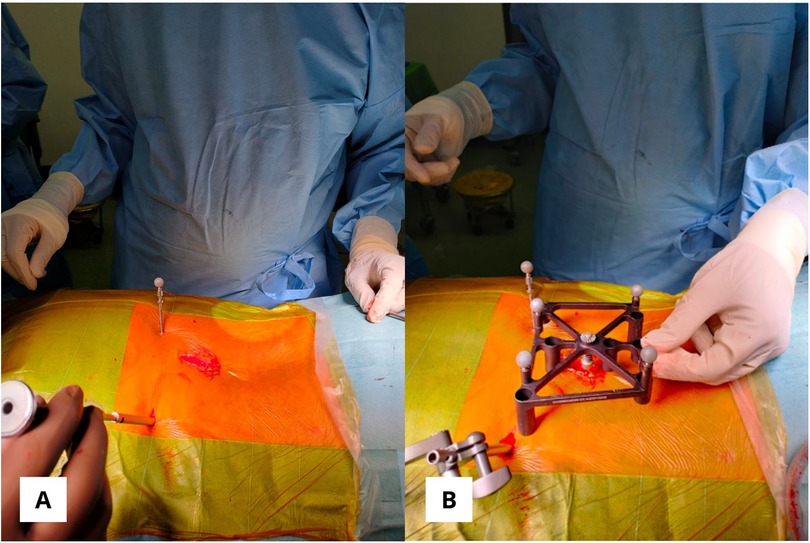
Figure 5. (A) The posterior superior iliac spine bilaterally is used for dynamic reference base and surveillance marker positioning. (B) ICT (Intraoperative Cone-Beam Tomography) was attached to the spinous process without touching the skin.
Screw planningEffective screw planning using the O-arm and ExcelsiusGPS surgical system involves careful registration of navigated instruments and precise screw trajectory planning to avoid complications (Figures 6, 7). For thoracic screws, it is crucial to prevent the transverse process slope, while lumbar screw planning must account for the superior articular process. Ensuring screw trajectory alignment without collisions and using 3D projections for accuracy are vital steps. In extremely obese patients, adjusting the end effector closer to the skin can help address the challenges posed by increased skin-to-bone distance, ensuring the robotic tools can reach the target effectively.
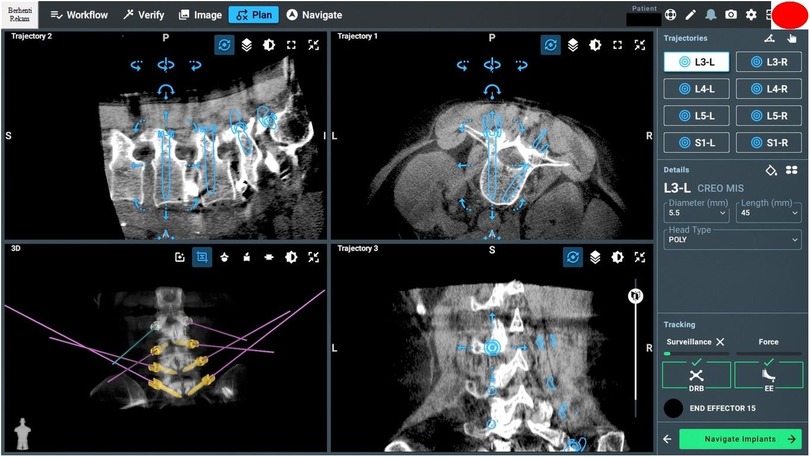
Figure 6. Screw planning includes entry points, trajectories, screw length, and width.
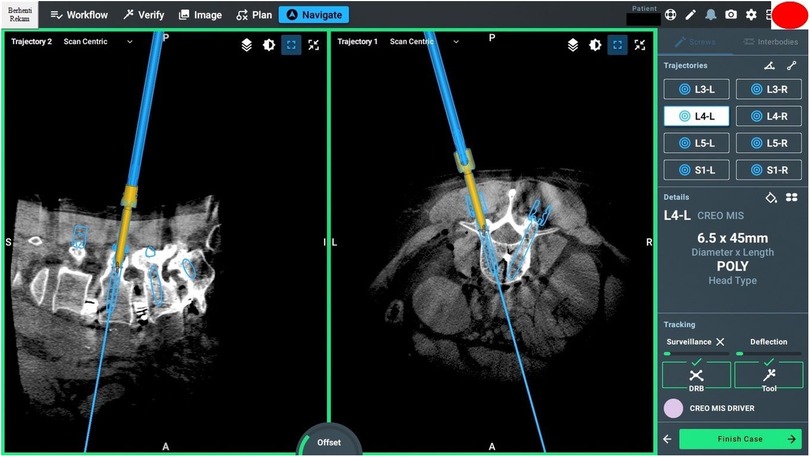
Figure 7. Intraoperative pedicle screw placement using the ExcelsiusGPS robotics system demonstrates the placement of a left-sided L4 pedicle screw.
ExposureOnce the end effector is in place, the surgeon will mark the skin incision using a scalpel inserted through the guide tube. The end effector is adjusted to accommodate a larger incision. During the incision, ensure that the fascia is adequately dissected beforehand. After the incision, the end effector is repositioned to its original position. The key to ensuring a good trajectory is achieving adequate exposure. Medial excision of the fascia is necessary to enable the proper trajectory for reaching the screw entry point.
Screw insertion and placementThe initial bur is positioned on the bone at the screw entry point to make an initial hole. The power burr is used before reaching the bone to prevent changes in bone alignment. Screws like Creo MIS screws or K-wire system are placed through the guide tube in the end effector. If using the K-wire system, insert the inner cannula into the guide tube after tapping. Once the K-wire is through the inner cannula, detach the cannula and reposition the end effector. Screws can be inserted with K-wire guidance. The screw is inserted until resistance from the tulip head against the bone is felt.
DiscussionRobotic-assisted spine surgery is gaining popularity due to its multiple advantages. However, there are concerns regarding appropriate screw placement under various conditions. In highly flexible bones, alignment often changes with breathing. If this occurs, the anesthesiologist should hold the patient's breath in the expiratory phase, similar to during scanning. During this phase, the initial burr and high-speed drill can be performed. During tapping, the patient can resume normal breathing. After the tapping phase, screw placement follows. Furthermore, during screw placement, tactile feedback and deflection monitoring are crucial for making real-time adjustments and maintaining the instrument's trajectory. Deflection often occurs due to inadequate soft tissue or fascia release and the weight of the power drill. Using a hamburger grip can help counteract this weight (Figure 8).

Figure 8. The hamburger grip technique was used to facilitate screw insertion with a power drill system.
With the growing and widespread adoption of navigation technology, numerous studies have reported superior outcomes and lower complication rates compared to free-hand techniques. A meta-analysis reported fewer complication rates were found in robotic spine-assisted surgery, including less intraoperative blood loss, lower revision rate, fewer complications, and shorter length of hospital stay (12). An extensive meta-analysis of twenty RCTs reported a lower complication rate in the robot-assisted group than in free-hand techniques (4.83% vs. 14.97%) (Figure 9) (10).
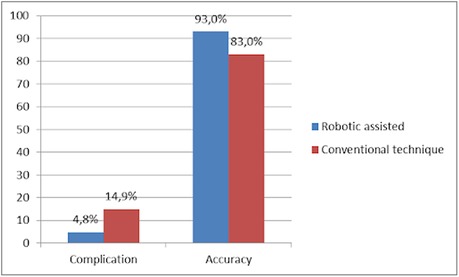
Figure 9. The comparison of outcomes between robotic-assisted and conventional techniques in complication and accuracy (10, 17).
Orthopedic surgeons are concerned about radiation exposure. Robotic systems reduce this exposure by avoiding the initial CT scan and minimizing intraoperative radiation. Research shows robotic procedures lower surgeon exposure significantly, with up to a tenfold decrease compared to fluoroscopy-guided techniques (13). Robotic-assisted surgery reduces radiation exposure by 54%–74% compared to conventional CT scans (14).
The precision of pedicle screw placement is crucial, as misplaced screws can lead to devastating vascular, pulmonary, and neurologic complications and even dural leaks (15). A study found that in spine surgery with robot assistance, 91.7% of pedicle screws were accurately placed, with only 6.8% deviating by less than 2 mm (16). Furthermore, most surgeons agree that a screw deviation of ≤2 mm is considered acceptable (15). Yue et al. showed that robot-assisted screw placement is more accurate than fluoroscopy-assisted placement, with a 93% vs. 83% accuracy rate and fewer superior facet joint devastations (Figure 9) (17).
Robotic spine surgery conserves energy for deformity correction, thus enabling less stressful surgery. The utilization of robotic navigation in spine surgery offers a range of advantages and disadvantages (Table 1).
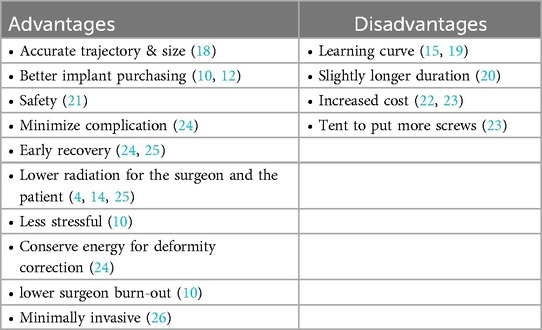
Table 1. Advantages and disadvantages of robotic spine surgery.
Future directionsThe integration of robotic systems in spine surgery is progressing rapidly, with advancements aimed at enhancing efficiency and surgical workflow through improved imaging software and automation. The scope of robotic systems is expected to broaden to include cervical and pelvic fixation and more complex spinal procedures.
ConclusionRobotic-assisted spine surgery has improved the accuracy of pedicle screw insertion by providing real-time planning, precise trajectory guidance, and intraoperative adjustments. This enhanced precision reduces complications, including misplacement, while also minimizing radiation exposure to the surgeon and the patient. However, these benefits come with increased costs and a higher usage of screws, necessitating careful evaluation of the procedure's cost-effectiveness and its overall impact on patient outcomes and healthcare resources.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementWritten informed consent was obtained from the patient for publication and any accompanying images.
Author contributionsLG: Conceptualization, Project administration, Writing – original draft, Writing – review & editing. PP: Conceptualization, Project administration, Resources, Writing – original draft, Writing – review & editing. SH: Resources, Writing – original draft, Writing – review & editing. HM: Resources, Writing – original draft, Writing – review & editing. AR: Resources, Writing – original draft, Writing – review & editing. MM: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. KG: Data curation, Formal Analysis, Writing – original draft, Writing – review & editing. EK: Data curation, Project administration, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
AcknowledgmentsWe thank Maharani Asmara Putri from Mapson Arya Parahita and William Kingston Xie for the technical support.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, et al. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. (2012) 21(2):247–55. doi: 10.1007/s00586-011-2011-3
PubMed Abstract | Crossref Full Text | Google Scholar
4. Farber SH, Pacult MA, Godzik J, Walker CT, Turner JD, Porter RW, et al. Robotics in spine surgery: a technical overview and review of key concepts. Front Surg. (2021) 8:8578674. doi: 10.3389/fsurg.2021.578674
PubMed Abstract | Crossref Full Text | Google Scholar
5. Kalidindi KKV, Sharma JK, Jagadeesh NH, Sath S, Chhabra HS. Robotic spine surgery: a review of the present status. J Med Eng Technol. (2020) 44(7):431–7. doi: 10.1080/03091902.2020.1799098
PubMed Abstract | Crossref Full Text | Google Scholar
6. Togawa D, Kayanja MM, Reinhardt MK, Shoham M, Balter A, Friedlander A, et al. Bone-mounted miniature robotic guidance for pedicle screw and translaminar facet screw placement: part 2–evaluation of system accuracy. Neurosurgery. (2007) 60(2):129–39. doi: 10.1227/01.NEU.0000249257.16912.AA.
Crossref Full Text | Google Scholar
8. Weinstein JN, Spratt KF, Spengler D, Brick C, Reid S. Spinal pedicle fixation: reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine (Phila Pa 1976). (1988) 13(9):1012–8. doi: 10.1097/00007632-198809000-00008
PubMed Abstract | Crossref Full Text | Google Scholar
9. Gao S, Wei J, Li W, Zhang L, Cao C, Zhai J, et al. Accuracy of robot-assisted percutaneous pedicle screw placement under regional anesthesia: a retrospective cohort study. Pain Res Manag. (2021) 2021(3):178–80. doi: 10.1155/2021/6894001
Crossref Full Text | Google Scholar
10. Sun WX, Huang WQ, Li HY, Wang HS, Guo SL, Dong J, et al. Clinical efficacy of robotic spine surgery: an updated systematic review of 20 randomized controlled trials. EFORT open Rev. (2023) 8(11):841–53. doi: 10.1530/EOR-23-0125
PubMed Abstract | Crossref Full Text | Google Scholar
11. Vaccaro AR, Harris JA, Hussain MM, Wadhwa R, Chang VW, Schroerlucke SR, et al. Assessment of surgical procedural time. Pedicle screw accuracy, and clinician radiation exposure of a novel robotic navigation system compared with conventional open and percutaneous freehand techniques: a Cadaveric investigation. Glob Spine J. (2020) 10(7):814–25. doi: 10.1177/2192568219879083
Crossref Full Text | Google Scholar
12. Ahmed AK, Zygourakis CC, Kalb S, Zhu AM, Molina CA, Jiang B, et al. First spine surgery utilizing real-time image-guided robotic assistance. Comput Assist Surg. (2019) 24(1):13–7. doi: 10.1080/24699322.2018.1542029
PubMed Abstract | Crossref Full Text | Google Scholar
14. Villard J, Ryang YM, Demetriades AK, Reinke A, Behr M, Preuss A, et al. Radiation exposure to the surgeon and the patient during posterior lumbar spinal instrumentation: a prospective randomized comparison of navigated versus non-navigated freehand techniques. Spine (Phila Pa 1976). (2014) 39(13):1004–9. doi: 10.1097/BRS.0000000000000351
PubMed Abstract | Crossref Full Text | Google Scholar
15. Schatlo B, Martinez R, Alaid A, von Eckardstein K, Akhavan-Sigari R, Hahn A, et al. Unskilled unawareness and the learning curve in robotic spine surgery. Acta Neurochir (Wien). (2015) 157(10):1819–23. doi: 10.1007/s00701-015-2535-0
PubMed Abstract | Crossref Full Text | Google Scholar
16. Keric N, Doenitz C, Haj A, Rachwal-Czyzewicz I, Renovanz M, Wesp DMA, et al. Evaluation of robot-guided minimally invasive implantation of 2067 pedicle screws. Neurosurg Focus. (2017) 42(5):30–4. doi: 10.3171/2017.2.FOCUS16552
Crossref Full Text | Google Scholar
17. Kosmopoulos V, Theumann N, Binaghi S, Schizas C. Observer reliability in evaluating pedicle screw placement using computed tomography. Int Orthop. (2007) 31(4):531–6. doi: 10.1007/s00264-006-0230-8
PubMed Abstract | Crossref Full Text | Google Scholar
18. Pechlivanis I, Kiriyanthan G, Engelhardt M, Scholz M, Lücke S, Harders A, et al. Percutaneous placement of pedicle screws in the lumbar spine using a bone mounted miniature robotic system: first experiences and accuracy of screw placement. Spine (Phila Pa 1976). (2009) 34(4):392–8. doi: 10.1097/BRS.0b013e318191ed32
PubMed Abstract | Crossref Full Text | Google Scholar
19. Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res. (2014) 472(6):1839–44. doi: 10.1007/s11999-013-3291-1
PubMed Abstract | Crossref Full Text | Google Scholar
20. Ringel F, Stüer C, Reinke A, Preuss A, Behr M, Auer F, et al. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomized comparison to conventional freehand screw implantation. Spine (Phila Pa 1976). (2012) 37(8):E496–501. doi: 10.1097/BRS.0b013e31824b7767
PubMed Abstract | Crossref Full Text | Google Scholar
21. Devito DP, Kaplan L, Dietl R, Pfeiffer M, Horne D, Silberstein B, et al. Clinical acceptance and accuracy assessment of spinal implants guided with SpineAssist surgical robot: retrospective study. Spine (Phila Pa 1976). (2010) 35(24):2109–15. doi: 10.1097/BRS.0b013e3181d323ab
PubMed Abstract | Crossref Full Text | Google Scholar
24. Li J, Fang Y, Jin Z, Wang Y, Yu M. The impact of robot-assisted spine surgeries on clinical outcomes: a systemic review and meta-analysis. Int J Med Robot. (2020) 16(6):1–14. doi: 10.1002/rcs.2143
PubMed Abstract | Crossref Full Text | Google Scholar
25. Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions: a randomized controlled trial. Spine (Phila Pa 1976). (2017) 42(6):353–8. doi: 10.1097/BRS.0000000000001778
PubMed Abstract | Crossref Full Text | Google Scholar
26. Fu W, Tong J, Liu G, Zheng Y, Wang S, Abdelrahim MEA, et al. Robot-assisted technique vs conventional freehand technique in spine surgery: a meta-analysis. Int J Clin Pract. (2021) 75(5). doi: 10.1111/ijcp.13964
留言 (0)