Gender health equity is a critical issue in healthcare and education, particularly in surgical fields where disparities persist (1–4). The culture of delay of pregnancy among female practitioners begins in the phases of pre-graduation training, when it would be the desirable biological age (5) and persists for the training phase based on population studies conducted (6, 7). In general, it is a real slippage of personal decisions, which tend to be taken late compared with non-medical women in view of a conflict with career goals (8). Many physicians both in their residency programs or immediately after, decide to postpone childbirth, often recurring to oocyte cryopreservation (9). Therefore, social freezing, a process where individuals choose to freeze their eggs or embryos for future use, has become increasingly relevant also for women pursuing medical careers, as it allows female medical professionals to extend their fertility. In general, the set of challenges for both surgical and forensic pathology residents are largely overlapping and can be summarized in exposure to chemical, physical and biological hazards, physical strain and psychological stress. The two residency programs (obstetrics &gynecology and forensic pathology) have been chosen for implications in legislative terms and for their similarity in requiring that part of the training is specifically dedicated to surgical procedures, yet one performed in surgical room and the other in autopsy room. The results of a 2021 Italian ministerial survey on the opinion of medical and surgical residents enrolled from the second year of the course have been recently published. The survey was conducted using CAWI (Computer-Assisted Web Interviewing). Specific questions were asked with the objective of investigating maternity/parenting protection. To the question: “Are you aware of any situations in your school where incidents of non-recognition of compulsory or optional maternity/paternity leave have occurred?” the percentages of positive responses were 0.3% for Obstetrics and 3.2% for Forensic Medicine. Incidents of non-recognition of breastfeeding or other daily rest allowances were reported from 2.2% of Obstetrics and Gynecology residents and 1.9% of Forensic Medicine residents who reported incidents of non-recognition of breastfeeding or other daily rest allowances (10). Working with patients or handling dead bodies (as for Forensic Pathologist) can expose residents to infectious diseases, including bloodborne pathogens (e.g., HIV, hepatitis B and C). However, forensic pathologists have additional issues related to working with cadavers and biological materials. In addition to this the use of formaldehyde and other chemicals in autopsy procedures may pose specific risks. Both disciplines can lead to physical strain, particularly during surgical sessions or autopsies, because of heavy lifting or long hours at work.
Materials and methodsA preliminary global analysis about the technologies for safe practice and training during pregnancy was carried out based on research gathered by Pubmed, Scholar, Embase, Scopus, etc. The identification of 32,221 articles was based on the keywords “medicine” AND “education” AND/OR “pregnancy” without time limit. 3,642 Articles in the English language were filtered according to the evidence of the scientific research (based on the strength of the evidence, sample size, quality of the studies, etc.). 3,620 Duplicates, research in other languages than English, data not specific or not relevant for the topic (i.e., about gynecological diseases or other forensic aspects) were excluded (Flowchart, Figure 1). Our narrative review is written following PRIOR Guidelines (11) (Supplementary Material).

Figure 1. Flowchart. The diagram details our search and selection process applied during the overview. Figure related to “pregnancy” AND “education” AND “medicine”. No results reported about “metaverse” AND “education” AND “pregnancy”.
ResultsThe 22 articles in our review are only related to the online search about “pregnancy” AND “education” AND “medicine”. The literature highlighted no results about “metaverse” AND “education” AND “pregnancy” (Table 1).
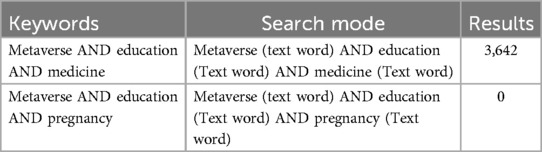
Table 1. Literature review results using the pubMed database.
DiscussionThe targeted literature review conducted shows that a real cultural shift is required to reconcile motherhood and a surgical career. with still little attention paid to the potential of new technological tools when specifically applied to the training of female residents in the areas of training with the highest risk for pregnancy. Results from a survey conducted among young female physicians to assess fertility, childbearing history, reflections regarding decision-making, and perceptions of workplace support, showed that 28.6% would have attempted conception earlier, 17.1% would have gone into a different specialty, and 7.0% would have used cryopreservation to extend fertility (12). Compared with male surgeons, female surgeons were more likely to delay having children because of surgical training and were more likely to use assisted reproductive technology. Compared with female non-surgeon partners, female surgeons were more likely to have major pregnancy complications, especially those operating 12 or more hours per week (13). Discriminations regarding career goals has been explored in a survey by Giantini et al. that demonstrated that a notably higher number of women expressed worries regarding the time available to date or marry (P = 0.042), the time they could spend with family (P = 0.015), the ability to find time to have a child during residency (P < 0.0001), the challenges of taking maternity or paternity leave while in residency (P < 0.0001), and concerns about being too old to have a child after completing residency (P < 0.0001) (14). Pregnant medical residents often face significant stress due to the physical demands of their training and a lack of support from colleagues and their department (15). It's since 1986 that it has been observed that if proper arrangements were made, pregnancy would not be a major problem for either the training program or the pregnant residents (16). Nevertheless, according to Rangel (17) a total of 135 interviewed (39.0%) strongly considered leaving surgical residency, and 102 (29.5%) would discourage female medical students from a surgical career, specifically because of the difficulties of balancing pregnancy and motherhood with training. Female surgeons face specific reproductive hazards that can impact their fertility and pregnancy outcomes pertaining both to intrinsic factors, such as delayed childbearing that involves age related fertility issues or extrinsic factors such as mechanical or biological hazards (18, 19). Forensic pathology is a field for which no data is available, although hazards and stress perceived might be like that of training surgeons. Surgical specialties have specific challenges related to the rigor of training, length and cultural factors related to a masculine interpretation of surgical specialties (19, 20); Forensic Pathology seems to be not seen as a male specialty. Flexible career pathways and work patterns are required to overcome the cultural barrier in surgical specialties (20). In Italy, there are specific regulations designed to protect pregnant workers, including those in forensic pathology. Regulations surrounding pregnancy and maternity leave for female surgeons and healthcare professionals are structured to ensure both health equity and workplace safety. There is a complete prohibition for pregnant workers to be exposed to some physical, chemical and biological agents. Italian regulation applicable to pregnant female healthcare workers is analyzed in detail. Law n 151/2001 (21), Article 7, prohibits assigning female workers to tasks involving the transport and lifting of weights, as well as to dangerous, strenuous, and unhealthy jobs. Among these hazardous tasks are those that pose risks of exposure to agents and working conditions listed in Annex B. During the period of prohibition, the worker will be assigned to other duties. Biological agents classified as risk groups 2, 3, and 4 according to Article 268 and Annex XLVI of Legislative Decree No. 81 of April 9, 2008 (22), are also included (Table 2).
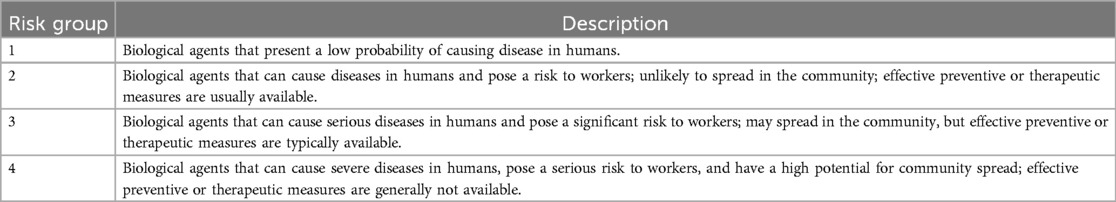
Table 2. Classification of biological agents based on their infection risk.
Apart from these absolute prohibitions there are many protection measures that tend to support maternity. For example, under the Italian budget law effective from January 1, 2019 (23), pregnant women can choose to work until childbirth if certified healthy by their doctor. They are entitled to five months of compulsory maternity leave following the birth of their child. This is a significant change from previous regulations, which divided maternity leave into two segments: two months before and three months after childbirth. Compulsory maternity leave is compensated at 80% of the salary used to calculate social security contributions. Pregnant employees cannot be dismissed from their jobs from the start of pregnancy until the child is one year old, with very few exceptions. Employers are required to adjust tasks for pregnant employees in physically demanding roles to ensure their safety and that of the unborn child. The privileged care attributed to pregnant women is suggested by the peculiar attention given by several directives of the Council of Europe that also supports maternity leave and breastfeeding. No one can force a pregnant woman to work in risky conditions or to work at night (24–27). Differently from European context, in US there is not a specific ban for pregnant women to perform surgery and continue their trainee program. In fact, operating during pregnancy may be safe if the right conditions are met (28). In the majority of OECD nations (Organization for Economic Co-operation and Development), paid parental leave with employment protection is a key component of family policy. By allowing both parents to take time off from paid employment to care for a very young child, paid parental leave primarily seeks to support parents and kids. An overview of parental leave policies and their implementation in OECD nations may be found in the OECD Family Database. All but one OECD nation provides paid maternity and paternity leave during childbirth at the national level as of April 2022; however, the length, cost, and adoption of these laws vary greatly throughout nations. Paid maternity leave lasts 18.5 weeks on average throughout the OECD, but it can vary from 43 weeks in Greece to none at all in the US (29). In the United States there has been the intervention of the Accreditation Council for Graduate Medical Education (ACGME) that has obtained the requirement of lactation facilities and the mandatory leaving for at least 6 weeks for all residency boards. In August 2020, the American Community Survey (ACS) and the ACGME Residency Review Committee released a statement outlining the following measures to protect pregnant residents: the residency program should support trainees' medical needs; it should design a flexible and equitable schedule that allows trainees to take time off while taking into account the needs of other health care professionals; and it should offer at least six weeks of paid parental leave for either or both parents (30). A schematic representation of the comparison between US and EU is provided in Table 3.
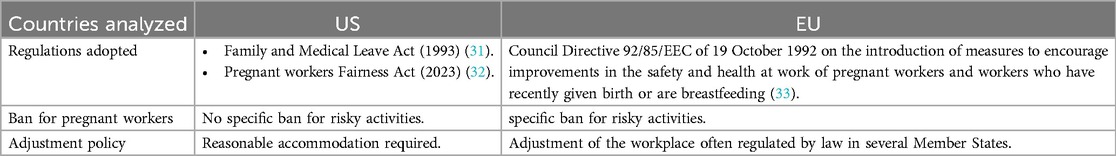
Table 3. Comparison between US and EU on the protection of pregnant workers.
Up to 12 weeks of unpaid, job-protected leave are granted to qualified employees annually under the Family and Medical Leave Act (FMLA) (31). It also mandates that their group health benefits be maintained while they are on leave. Companies with 50 or more employees, as well as all public and private primary and secondary institutions, are covered by the FMLA. For any of the following reasons, these employers are required to offer up to 12 weeks of unpaid leave annually to an eligible employee: for the birth and upbringing of a worker's newborn; for a kid in foster care or adoption to be placed with the staff; to take care of a parent, spouse, kid, or other member of one's immediate family who has a serious illness; or to take medical leave when an employee is unable to work due to a serious illness. In addition to this, more recently, the Pregnant workers Fairness Act (PWFA) for eligible candidates or workers with known restrictions, the PWFA offers appropriate accommodations. Physical or mental conditions associated with, impacted by, or resulting from pregnancy, childbirth, or related medical conditions are considered “limitations” under the PWFA (32). “Reasonable accommodations” are changes that could be provided in the work environment or the way things are usually done at work. Nevertheless, if making a reasonable accommodation would put an unreasonable burden on the employer, the PWFA does not require the employer to do so (“undue hardship”). Differently from the US, in Europe the discipline is more stringent (33), since risky activities are outlined by law and divided into generic and specific hazards. Generic hazards include nocturnal work, hazards resulting from inappropriate rest/nutrition/hygene, standing activities, sitting activities, occupational stress, etc. whereas specific hazards include risk deriving from all chemical, biological and physical agents. Employers must take action to protect female employees when hazards are discovered, for as by giving them leave or relocating them to a different role. Workers who are pregnant are exempt from working night shifts as long as they can provide a medical certificate. During working hours, pregnant employees are permitted to have prenatal medical exams without losing their wages. A minimum of 14 consecutive weeks of maternity leave, including at least two weeks of mandatory maternity leave, are required under the regulation before and/or after delivery. There are safeguards against every risk mentioned by the European directive and employers are responsible for choosing the measures that best suit their needs while adhering to local, state, and federal laws.
Despite this important set of institutional protection for pregnant workers, residents need also to potentiate their practice during gestational period and continue their training. It would be possible with specific tools, as metaverse. From the research conducted, there are 0 articles with metaverse related to healthcare education in pregnancy as shown in Table 1. On the other hand, thousands of articles in the last few years analyzed the use of metaverse for training purposes in medicine. The results demonstrate that the analyzed regulations are particularly restrictive, effectively prohibiting pregnant women from accessing environments that pose health risks. Scientific societies and the broader scientific community continue to discuss achieving equitable training standards for pregnant women (34), given the prevailing culture that views time spent away from practice as time lost (35). While there are objective limitations in identifying options to adapt to careers, there is also a pressing need to identify informed policies to guide workplace adaptations for physicians who are pregnant (36). New technologies possess substantial potential to transform healthcare significantly. By integrating with the Internet of Medical Devices, quantum computing, and robotics, the metaverse is positioned to redefine healthcare systems (37). The metaverse offers limitless possibilities and is expected to influence future advancements in medical science and technology (38). Telemedicine can greatly diminish barriers for patients seeking medical treatment, enabling healthcare providers to overcome geographical constraints and optimize the use of medical resources. Furthermore, sharing patient data can facilitate advancements in clinical research (38). Nevertheless, until this moment, metaverse and augmented reality have been analyzed for their specific potential for medical (39) and surgical training without a gender-based perspective. Pregnant surgeons could benefit from AR and metaverse by participating in surgeries through remote guidance without compromising safety. Surgeons can practice skills and collaborate remotely without physical constraints. This immersive platform would allow pregnant surgeons to engage in training and mentoring without direct exposure to surgical risks. Pregnant surgeons can engage in surgical procedures through AR, minimizing physical strain and exposure to hazardous conditions. Telemedicine also appears as a great tool to continue receiving patients, letting pregnant women continue their activity even in case of presence of a biohazard that discourages direct contact with patients. These technologies could reduce exposure to harmful agents while maintaining surgical proficiency, although no data is available in literature.
ConclusionsThe intersection of gender health equity in surgical practices and forensic pathology reveals significant gaps in addressing the unique challenges faced by young female surgeons during pregnancy. By comparing regulations across both fields, we identify critical areas for improvement. Furthermore, technological advancements such as AR and the metaverse present promising solutions that allow pregnant surgeons to continue their practice, while minimizing biological risks. Future efforts should focus on developing comprehensive guidelines that prioritize gender equity and leverage technology to create safer working environments for all healthcare professionals. Most of the papers concentrate on the repercussions of metaverse on training without a specific gender-based approach. Gynecology and forensic pathology are united by the important role attributed to anatomy, that requires constant practice in surgical and sector room and the biological risk that occurs during pregnancy. For both residency programs, as for all pregnant healthcare professionals, exposure to biological risk is forbidden during pregnancy. Even if metaverse has been largely analyzed, especially in the last few years regarding its applications in education, there is still a lack of evidence regarding its specific role in bridging the gap for pregnant surgeons to keep them in in training even in the period the surgical/sector room is forbidden by law, without keeping in training especially in what concerns manual dexterity. Italy's regulatory framework protects against gender disparities (40), supporting female workers and in particular surgeons during pregnancy by providing comprehensive maternity leave policies, job protection, and access to healthcare services. However, there remains a need for continuous improvement in workplace accommodations and the integration of technology to enhance safety and professional development for young female surgeons, including those in training as gynecologists or forensic pathologists. By ensuring that these professionals can continue practicing during pregnancy, while minimizing risks through innovative technologies, Italy can further advance gender health equity in surgical fields. Further studies are also needed to assess whether this is a real need for practicing pregnant surgeons.
Author contributionsEC: Investigation, Supervision, Writing – original draft. MM: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. CA: Validation, Writing – review & editing. PD: Formal Analysis, Writing – original draft. CC: Data curation, Visualization, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2025.1513832/full#supplementary-material
References1. Di Donna G, Di Lorenzo P, Aquino CI, Marisei M, Casella C, Surico D, et al. Gender violence during the three ages of life and the impact of the COVID-19 pandemic: a review. Int J Soc Determinants Health Health Serv. (2024) 54(4):423–35. doi: 10.1177/27551938241247776
PubMed Abstract | Crossref Full Text | Google Scholar
3. Adesoye T, Mangurian C, Choo EK, Girgis C, Sabry-Elnaggar H, Linos E, et al. Physician moms group study group. Perceived discrimination experienced by physician mothers and desired workplace changes: a cross-sectional survey. JAMA Intern Med. (2017) 177:1033–6. doi: 10.1001/jamainternmed.2017.1394
PubMed Abstract | Crossref Full Text | Google Scholar
4. Di Lorenzo P, Casella C, Marisei M, Sarno L, Aquino CI, Osuna E, et al. A COVID dilemma: how to manage pregnancies in case of severe respiratory failure? Healthcare (Basel). (2023) 11(4):486. doi: 10.3390/healthcare11040486
PubMed Abstract | Crossref Full Text | Google Scholar
6. Cusimano MC, Baxter NN, Sutradhar R, McArthur E, Ray JG, Garg AX, et al. Delay of pregnancy among physicians vs nonphysicians. JAMA Intern Med. (2021) 181(7):905–12. doi: 10.1001/jamainternmed.2021.1635
PubMed Abstract | Crossref Full Text | Google Scholar
7. Cusimano MC, Baxter NN, Sutradhar R, Ray JG, Garg AX, McArthur E, et al. Reproductive patterns, pregnancy outcomes and parental leave practices of women physicians in Ontario, Canada: the dr mom cohort study protocol. BMJ Open. (2020) 10:e041281. doi: 10.1136/bmjopen-2020-041281
PubMed Abstract | Crossref Full Text | Google Scholar
9. Nasab S, Shah JS, Nurudeen K, Jooya ND, Abdallah ME, Sibai BM. Physicians’ attitudes towards using elective oocyte cryopreservation to accommodate the demands of their career. J Assist Reprod Genet. (2019) 36:1935–47. doi: 10.1007/s10815-019-01541-7
PubMed Abstract | Crossref Full Text | Google Scholar
11. Gates M, Gates A, Pieper D, Fernandes RM, Tricco AC, Moher D, et al. Reporting guideline for overviews of reviews of healthcare interventions: development of the PRIOR statement. Br Med J. (2022) 378:e070849. doi: 10.1136/bmj-2022-070849
PubMed Abstract | Crossref Full Text | Google Scholar
12. Stentz NC, Griffith KA, Perkins E, Jones RD, Jagsi R. Fertility and childbearing among American female physicians. J Womens Health (Larchmt). (2016) 25:1059–65. doi: 10.1089/jwh.2015.5638
PubMed Abstract | Crossref Full Text | Google Scholar
13. Rangel EL, Castillo-Angeles M, Easter SR, Atkinson RB, Gosain A, Hu YY, et al. Incidence of infertility and pregnancy complications in US female surgeons. JAMA Surg. (2021) 156(10):905–15. doi: 10.1001/jamasurg.2021.3301. Erratum in: JAMA Surg. (2021) 156(10):991. doi: 10.1001/jamasurg.2021.445034319353
PubMed Abstract | Crossref Full Text | Google Scholar
14. Giantini Larsen AM, Pories S, Parangi S, Robertson FC. Barriers to pursuing a career in surgery: an institutional survey of harvard medical school students. Ann Surg. (2021) 273(6):1120–6. doi: 10.1097/SLA.0000000000003618
PubMed Abstract | Crossref Full Text | Google Scholar
17. Rangel EL, Smink DS, Castillo-Angeles M, Kwakye G, Changala M, Haider AH, et al. Pregnancy and motherhood during surgical training. JAMA Surg. (2018) 153(7):644–52. doi: 10.1001/jamasurg.2018.0153
PubMed Abstract | Crossref Full Text | Google Scholar
18. Hodson L, Ovesen J, Couch J, Hirst D, Lawson C, Lentz TJ, et al. Managing Hazardous Drug Exposures: Information for Healthcare Settings. US Department of Health and Human Services, Centers for Disease Control and Prevention. National Institute for Occupational Safety and Health, DHHS (NIOSH) (2023). doi: 10.26616/NIOSHPUB2023130
Crossref Full Text | Google Scholar
20. Hirayama M, Fernando S. Organizational barriers to and facilitators for female surgeons’ career progression: a systematic review. J R Soc Med. (2018) 111(9):324–34. doi: 10.1177/0141076818790661
PubMed Abstract | Crossref Full Text | Google Scholar
27. Sterbling HM, Kelly CH, Stafford A, Willey S, Dort J. Pregnancy curriculum: advocating for a healthier pregnancy in general surgery residency. J Surg Educ. (2023) 80(12):1799–805. doi: 10.1016/j.jsurg.2023.08.004
PubMed Abstract | Crossref Full Text | Google Scholar
28. Dowgiałło-Gornowicz N, Zięty JJ, Gornowicz M, Sztaba K, Osowiecka K, Lech P. To be a pregnant surgeon—is there anything to be afraid of? Int J Environ Res Public Health. (2023) 20(3):2265. doi: 10.3390/ijerph20032265
Crossref Full Text | Google Scholar
30. Jackson R, Birsner ML, Terman S, Morris L. ACOG Committee opinion No. 733: employment considerations during pregnancy and the postpartum period. Obstet Gynecol. (2018) 131(4):e115–23. doi: 10.1097/AOG.0000000000002589
PubMed Abstract | Crossref Full Text | Google Scholar
34. Mertens LS, Pignot G, Afferi L, Vásquez JL, Mir C, Pradere B. Pregnancy and urology residency: towards equity-centred practice. Eur Urol. (2023) 84(2):152–3. doi: 10.1016/j.eururo.2023.05.020
PubMed Abstract | Crossref Full Text | Google Scholar
36. Marsters CM, Stafl L, Bugden S, Gustainis R, Nkunu V, Reimer R, et al. Pregnancy, obstetrical and neonatal outcomes in women exposed to physician-related occupational hazards: a scoping review. BMJ Open. (2023) 13(2):e064483. doi: 10.1136/bmjopen-2022-064483
PubMed Abstract | Crossref Full Text | Google Scholar
39. Mazzoni D, Pagin MM, Amadori R, Surico D, Triberti S, Aquino CI, et al. Chapter 6. The dual path of the technology acceptance model: an application of machine learning cardiotocography in delivery rooms. In: Artificial Intelligence for Medicine. (2024). doi: 10.1016/B978-0-443-13671-9.00002-8
Crossref Full Text | Google Scholar
40. Mazzoni D, Pagin MM, Amadori R, Surico D, Triberti S, Aquino CI, et al. The dual path of the technology acceptance model: an application of machine learning cardiotocography in delivery rooms. In: Ben-David S, Curigliano G, Koff D, Jereczek-Fossa BA, La Torre D, Pravettoni G, editors. An Applied Reference for Methods and Applications Advanced Studies in Complex Systems: Theory and Applications. Academic Press (2024). p. 73–80. doi: 10.1016/B978-0-443-13671-9.00002-8
留言 (0)