Dear Editor,
Cutaneous dirt-adherent disease (CDAD) is a rare relapsing dermatosis that manifests with persistent adherence of dirt like substances occurring mainly on cheeks, forehead, breasts, and other areas with increased sebaceous activity.1 Erythematotelangiectatic rosacea (ETR) is the most common subtype of rosacea and is characterised by persistent erythema and flushing of the face.2 Traditionally, treatment methods including keratolytics, emollients, antifungal agents, and retinoids play an important role in the treatment of CDAD or ETR. However, these treatment modalities sometimes elicit a poor response or recurrence. New treatment options are needed in clinical practice.
Recent studies have indicated that psychological factors and neuroinflammation could be involved in the pathogenesis of the two diseases.1,3 Transcutaneous auricular vagus nerve stimulation (taVNS) is an efficacious non-invasive neuromodulation strategy that modulates the activity of the auricular branch of the vagus nerve by stimulating the outer conchal cavity.4 This manipulation has been demonstrated to ameliorate symptoms in patients with epilepsy, depression, migraine, and other functional neurological/psychological disorders.5 Hence, we propose that taVNS may be beneficial for the treatment of CDAD and ETR. Here, we report a case of patients with refractory CDAD and ETR that responded well to taVNS.
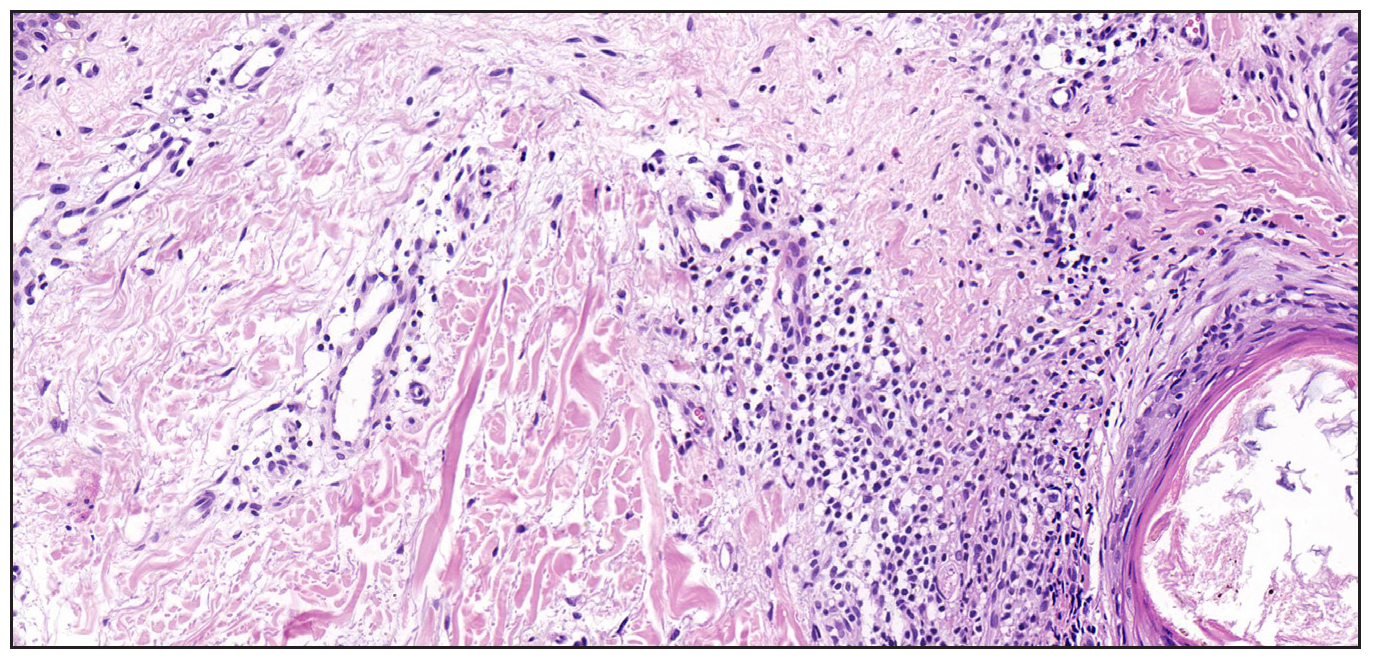
A 22-year-old girl presented to our department with a 4-year recurring history of rough, hypertrophic, yellowish-brown, and hard-to-peel adherent serous crusts densely covering the cheeks, eyelids, temporal regions, and eyebrows [Figure 1a]. She also had a 6-year history of facial flushing and erythema accompanied by itching [Figure 1b] and histopathology from the cheek was consistent with rosacea [Figure 2]. The patient consistently wore masks and hats to avoid social contact. The psychological self-questionnaire and psychologist evaluation indicated the presence of anxiety and depression [Table 1]. The patient underwent a range of treatments, including oral isotretinoin, H2-antagonists, doxycycline, topical emollients, and antifungal agents. Temporary symptomatic relief was achieved, typically lasting 1–2 months before relapse. This was generally followed by the occurrence of aggravated lesions. Cessation of medical treatment and stress also contributed to increased severity of lesions. Consequently, she consented to an off-label treatment with daily taVNS therapy, characterised by stimulation pulses at a frequency of 30 Hz and pulse width of 300 μs for 30 minutes per day. Concurrently, the importance of proper facial hygiene and the establishment of a facial cleaning diary were explained. After 3 weeks of treatment, she presented a significant reduction in adherent crusts, erythema, and flushing [Figure 3a]. In addition, she also experienced a significant reduction in the symptoms of anxiety and depression. No relapse was observed during the 6-months treatment-free follow-up period [Figure 3b].

Export to PPT

Export to PPT
Export to PPT
Table 1: Patient examination before and after treatment
Before treatment (week 0) After treatment (3 weeks) follow-up (6 months after treatment) Assessment of CADA/ETR Crust Cheeks, eyelids, temporal, and eyebrows None None Swellinga 2 0 0 Itchingb 2 0 0 Sting/burnc 1 0 0 Clinician’s Erythema Assessment (CEA) scored 3 2 1 Patient Self-Assessment (PSA) scoree 3 1 1 Global Flushing Severity Scale (GFSS) scoref 7 2 0 Psychological examination Patient Health Questionnaire-9 (PHQ-9) scoreg 7 3 3 Generalized Anxiety Disorder-7 (GAD-7) scoreh 14 5 2
Export to PPT

Export to PPT
The diagnosis of CDAD and ETR is primarily clinical, given the scarcity of definitive biological markers. The assessment hinges on a meticulous review of the patient’s medical history with particular attention to the recurrent episodes of facial erythema and flushing that typically precede the formation of crusts. These clinical features are instrumental in establishing a diagnosis of CDAD complicated with ETR.
TaVNS has emerged as a promising therapeutic modality for functional neurological and psychological disorders.5 It has been demonstrated to ameliorate both facial dermatological symptoms and concomitant psychological manifestations. Studies have implicated taVNS in modulating the inflammatory response by regulating cholinergic signalling pathways, both peripherally and centrally. This modulation is positioned to enhance synaptic plasticity within key brain regions of the central nervous system, thereby improving cognitive function and alleviating mental symptoms. Moreover, studies have also shown that taVNS is linked to the neuro-skin axis that regulates the relationship between brain regions to alleviate neuroinflammatory effects.5,6 We propose that CDAD and ETR could be manifestations of underlying neurological or psychological conditions, sharing similarities in their clinical presentations and underlying pathophysiological mechanisms. The presence of facial destructive lesions has been correlated with the onset of psychological distress in affected individuals. Furthermore, the exacerbation of psychological stressors is believed to contribute to the progression or relapse of CDAD and ETR.7 Therefore, we postulated that taVNS may be an effective treatment for CDAD and ETR. Besides, we treated other 10 cases of refractory ETR by TaVNS and all the patients achieved satisfactory improvement in facial erythema and flushing symptoms.
The therapeutic effect of taVNS and the detailed mechanism of CDAD or ETR require further exploration. To our knowledge, this is the first reported case of CDAD complicated with ETR that was successfully treated using taVNS. TaVNS is expected to be a new therapeutic option to treat patients with ETR or CDAD.
留言 (0)