Structural abnormalities of the heart and/or great vessels present at birth are referred to as congenital heart disease (CHD) (1), with a global incidence of roughly 0.8%–1.2% in live births (2, 3). CHD subtypes span from comparatively uncomplicated and minor lesions, including ventricular septal defect (VSD) and atrial septal defect (ASD), to more intricate and infrequent lesions like hypoplastic left heart syndrome (HLHS), tetralogy of Fallot (ToF), and transposition of the great arteries (TGA) (4). Pharmacological interventions to alleviate symptoms, complications, and conventional surgery or minimally invasive interventional surgery, are the main methods for treating CHD (5, 6). The introduction of cardiopulmonary bypass has rendered the disease manageable (7). Despite significant reductions in mortality achieved through progress in surgery over recent decades, CHD continues to be a primary cause of deaths related to birth defects (2, 8).
Adverse events after surgery in children with CHD (mortality, length of hospital stay, complication rates, etc.) remain a focus concern. In China, the mortality rate of CHD is rising (9). Compared to older children, neonates and infants are more susceptible to adverse events after CHD surgery (10, 11). Amirnovin et al. (10) found that higher perioperative BNP levels were associated with a greater likelihood of adverse outcomes after surgery. Hunt et al. (12) discovered that elevated preoperative von Willebrand factor (VWF) activity was associated with postoperative thrombosis in children with CHD. Gupta et al. (13) confirmed that elevated NT-proBNP may be a useful marker of adverse outcomes after cardiac surgery in children with CHD. To date, several biomarkers have been shown to be associated with adverse outcomes after CHD surgery, but no meta-analysis has combined the data. This article comprehensively searched and analyzed existing studies to explore the value of biomarkers in predicting adverse outcomes in children with CHD after surgery and to lay a theoretical foundation for constructing a more accurate risk prediction model for postoperative outcomes in children with CHD in clinical practice.
2 Materials and methods 2.1 Literature searchThe meta-analysis following PRISMA guidelines (14) and was registered in PROSPERO (CRD42024512753). PubMed, Embase, Cochrane Library, and Web of Science databases for literature searching up to February 2024 to identify English-language literature on the value of biomarkers in predicting postoperative outcomes in children with CHD. Terms followed were included: “congenital heart disease”, “factor”, “randomized controlled trial”, “cohort study”, and “case-control study”. The search strategy for PubMed is as follows: (((((((((((Defect, Congenital Heart [Title/Abstract]) OR (Heart Abnormality [Title/Abstract])) OR (Congenital Heart Defect [Title/Abstract])) OR (Heart, Malformation Of [Title/Abstract])) OR (Malformation Of Heart [Title/Abstract])) OR (Defects, Congenital Heart [Title/Abstract])) OR (Heart Abnormalities [Title/Abstract])) OR (Heart Defect, Congenital [Title/Abstract])) OR (Congenital Heart Disease [Title/Abstract])) OR (Disease, Congenital Heart [Title/Abstract])) OR (Heart Disease, Congenital [Title/Abstract])) OR (Congenital Heart Defects [Title/Abstract]) AND (((((((((Operative Procedures [Title/Abstract]) OR (Procedure, Operative [Title/Abstract])) OR (Surgical Procedure, Operative [Title/Abstract])) OR (Operative Surgical Procedures [Title/Abstract])) OR (Procedure, Operative Surgical [Title/Abstract])) OR (Surgical Procedures [Title/Abstract])) OR (Procedure, Surgical [Title/Abstract])) OR (Operative Surgical Procedure [Title/Abstract])) OR (Ghost Surgery [Title/Abstract])) OR (surgery [Title/Abstract]) AND (factor [Title/Abstract]) AND ((((((randomized controlled trial [All fileds]) OR (randomized controlled trial [All fileds])) OR (RCT [All fileds])) OR (clinical trial [All fileds])) OR (cohort [All fileds])) OR (case-control [All fileds])) OR (clinical study [All fileds]). Furthermore, the reference lists of every qualifying study underwent a manual review. Two researchers, working independently, conducted searches and evaluated the studies that met the inclusion criteria. Any disagreements that arose during the literature search process were resolved through consensus-based discussions.
2.2 Inclusion and exclusion criteriaInclusion criteria: (1) study design was randomized controlled, cohort, or case-control; (2) study subjects were children with CHD; (3) Biomarker data can be extracted: The continuous variable data contains the mean ± standard deviation, and the categorical variable contains the odds ratios (ORs) and the corresponding 95% Confidence Interval (95% CI); (4) at least one of the following outcomes was assessed: mortality, length of hospital stay, complication rates, or infection rates; (5) sufficient data were available to calculate odds ratios (ORs) or standardized mean differences (SMDs). We excluded reviews, letters, editorials, case reports, conference abstracts, unpublished articles, and non-English articles.
2.3 Data extraction and quality assessmentTwo researchers (SF Zhou. and L Liu) extracted data independently. Any discrepancies were resolved by a third researcher (SF Ma) who made the final decision. First author, year of publication, study period, country, study design, sample size, age, weight, gender, disease type, biomarker, detection time, threshold, and incidence of adverse outcomes were extracted. When continuous variables were reported as medians with ranges or interquartile ranges in the studies, we calculated means ± standard deviations using validated mathematical methods (15, 16). In instances where data was incomplete or not reported in the studies, we reached out to the corresponding authors to request the missing information. Newcastle-Ottawa Scale (NOS) was utilized to evaluate the quality, with scores ranging from 7 to 9 points indicating high-quality research (17). The assessment of quality and evidence level for eligible studies was carried out independently by two researchers. Any disagreements that arose during this process were resolved through open discussions.
2.4 Statistical methodsReview Manager version 5.4 was utilized to conduct evidence synthesis. Data were pooled using SMDs for continuous variables and ORs for dichotomous variables. All indicators were reported with 95% confidence intervals (CIs). The chi-squared (χ2) test (Cochran's Q) and inconsistency index (I2) were applied for the evaluation of the heterogeneity of each outcome. χ2P value more than 0.05 or I2 < 50% indicating non-significant heterogeneity and a fixed-effects model used for data synthesis. Conversely, when χ2P value less than 0.05 or I2 ≥ 50%, a random-effects model was used. Moreover, we conducted sensitivity analysis to evaluate how the incorporated studies influenced the pooled findings for outcomes exhibiting substantial heterogeneity. To visually assess potential publication bias for outcomes with three or more included studies, we employed Egger's regression test utilizing the statistical software Stata, version 15.0. For publication bias, statistical significance was indicated by a P-value below 0.05.
3 Results 3.1 Identification of relevant studiesThe initial search yielded a total of 6,747 potentially relevant studies. Duplicate studies were eliminated, leaving 6,085 unique records. After reviewing titles, abstracts, and full-text articles against the predefined inclusion and exclusion criteria, 17 studies met the eligibility requirements. These qualified studies encompassed a total of 2,888 children (involved patients younger than 18 years), which were included in the pooled analysis (10, 12, 13, 18–31). The flow chart was shown in Figure 1.
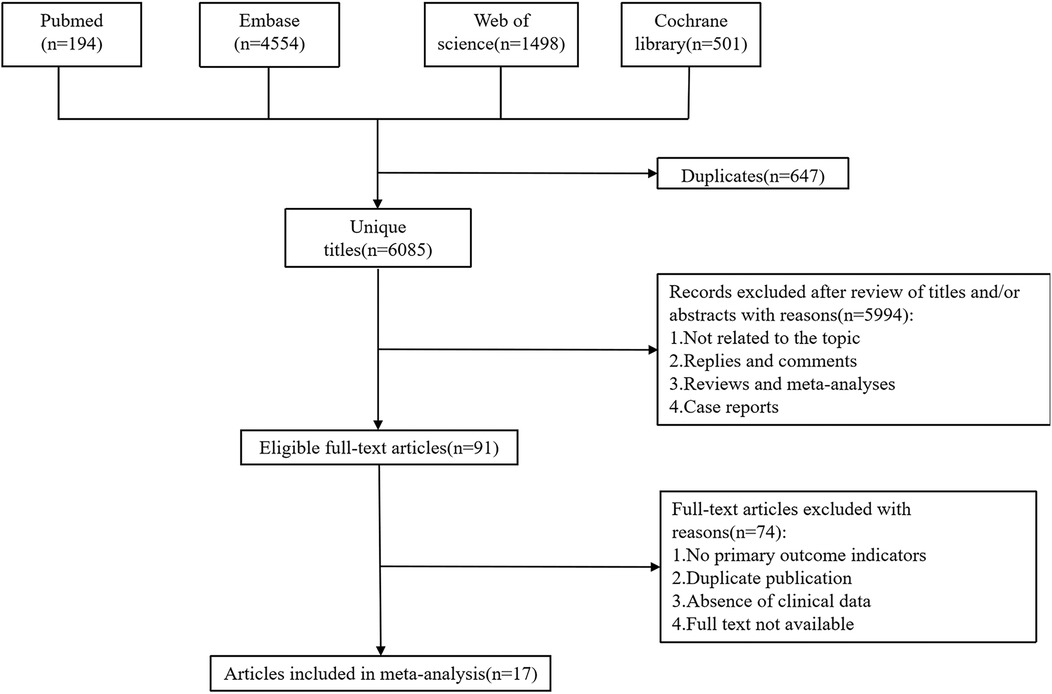
Figure 1. Flowchart onf the systematic search and selection process.
3.2 Study characteristics and quality assessmentAmong the 17 included studies, 8 were prospective studies and 9 were retrospective studies. Regarding the time of biomarker measurement, 10 studies were preoperative, 6 were postoperative, and 1 was not mentioned (Table 1). Three studies used serum lactate as a biomarker, two used NT-ProBNP, two used PaO2, and the remaining studies used serum creatinine, C1-INH activity, ST2, serum chloride concentration, GH, glycemia, cTOI, NLR, serum albumin, or glucose levels as biomarkers. The observed outcomes varied by study: 7 studies used mortality as an outcome, 4 studies reported the incidence of postoperative AKI, and the remaining studies used thrombosis (coronary thrombosis, arterial thrombosis, deep venous thrombosis, arterial stroke, cerebral sinus thrombosis, shunt thrombosis), prolonged hospitalization (Neonate >46 days, infant >17 days), capillary leak syndrome (the development of generalized noncardiac edema, ascites, pleural effusion, and a weight gain of more than 10%), prolonged PICU length of stay (>3 days), infection rate (positive culture from blood, urine, or wound), prolonged mechanical ventilation time (Neonate >184 h, infant >22 h) as outcome events. The quality evaluation utilizing the NOS scale revealed that 10 of the incorporated studies achieved scores ranging from 7 to 9 points, suggesting good quality and a low risk of bias. The characteristics and quality ratings of the eligible studies are presented in Table 1.
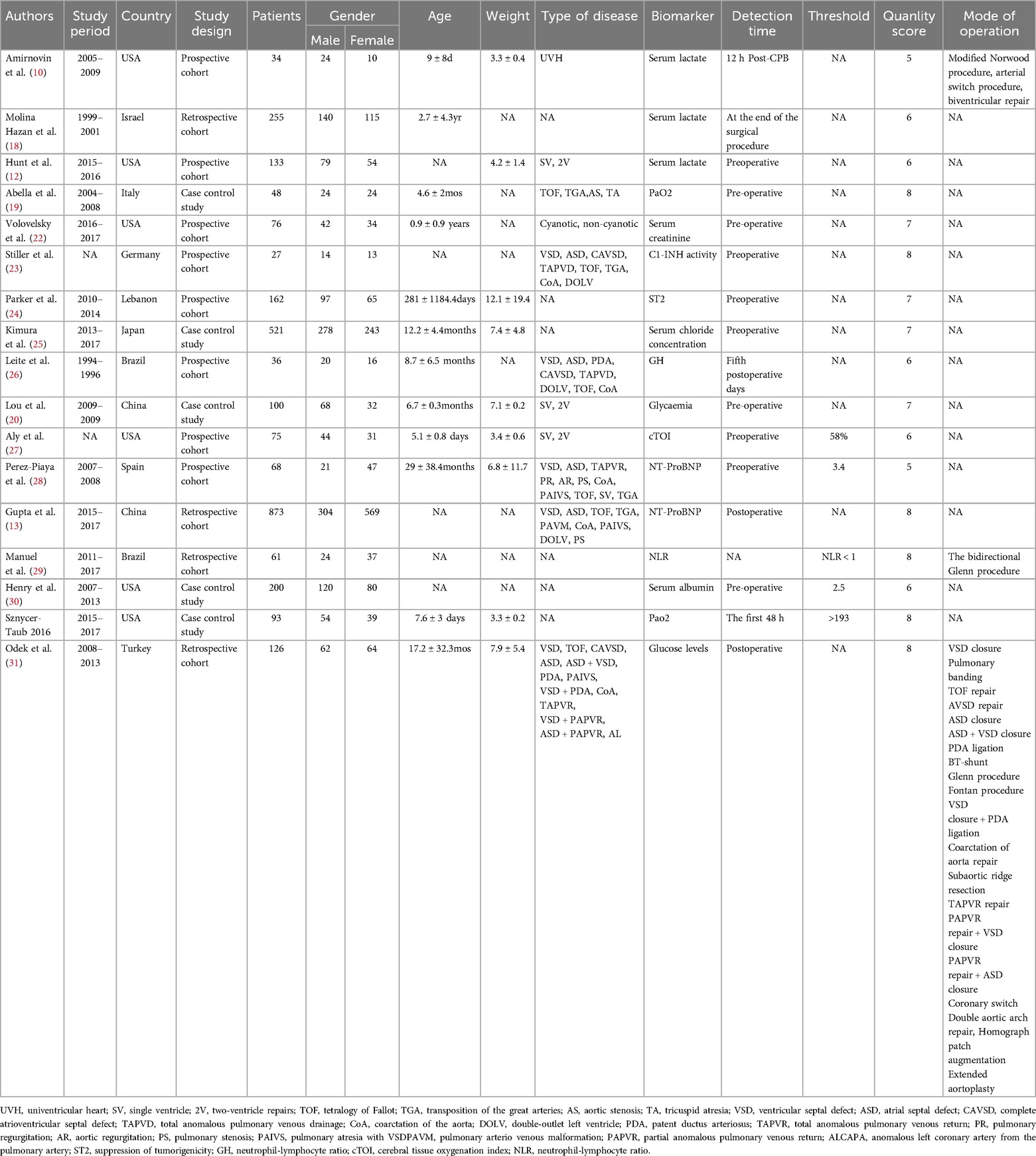
Table 1. Baseline characteristics of include studies and methodological assessment.
3.4 preliminary study synthesis 3.4.1 The pooled data for continuous variable showed1.1 A summary analysis of the 95% CIs corresponding to the biomarkers and their outcomes extracted from the included studies showed that the serum lactate level was higher in the postoperative death group compared to the survival group in children with CHD (SMD: 1.18, 95% CI: 0.59–1.77), with significant heterogeneity (I2 = 68%, P < 0.0001) and a random-effects model used (Figure 2A).
1.2 The BNP level was higher in children who died after CHD surgery compared to those who survived (SMD: 7.72, 95% CI: 0.55–14.89), with significant heterogeneity (I2 = 97%, P = 0.03) and a random-effects model used (Figure 2B).
1.3 Preoperative VWF activity was higher in children with CHD who developed thrombosis after surgery compared to those without thrombosis (SMD: 0.58, 95% CI: 0.20–0.96), with a random-effects model used (Figure 2E).
1.4 Serum creatinine levels were not significantly associated with the occurrence of acute kidney injury (AKI) after surgery in children with CHD (SMD: 0.03, 95% CI: −1.02 to 1.08), with significant heterogeneity (I2 = 95%, P = 0.95) (Figure 2C).
1.5 Activation of the serum complement system was not significantly associated with the occurrence of capillary leak syndrome (CLS) after surgery in children with CHD (SMD: 0.20, 95% CI: −0.10 to 0.50) (Figure 2D).
1.6 No statistically significant difference was observed in the blood glucose levels of the two groups, whether they experienced complications after surgery or not (SMD: −0.13, 95% CI: −0.44 to 0.19) (Figure 2F).
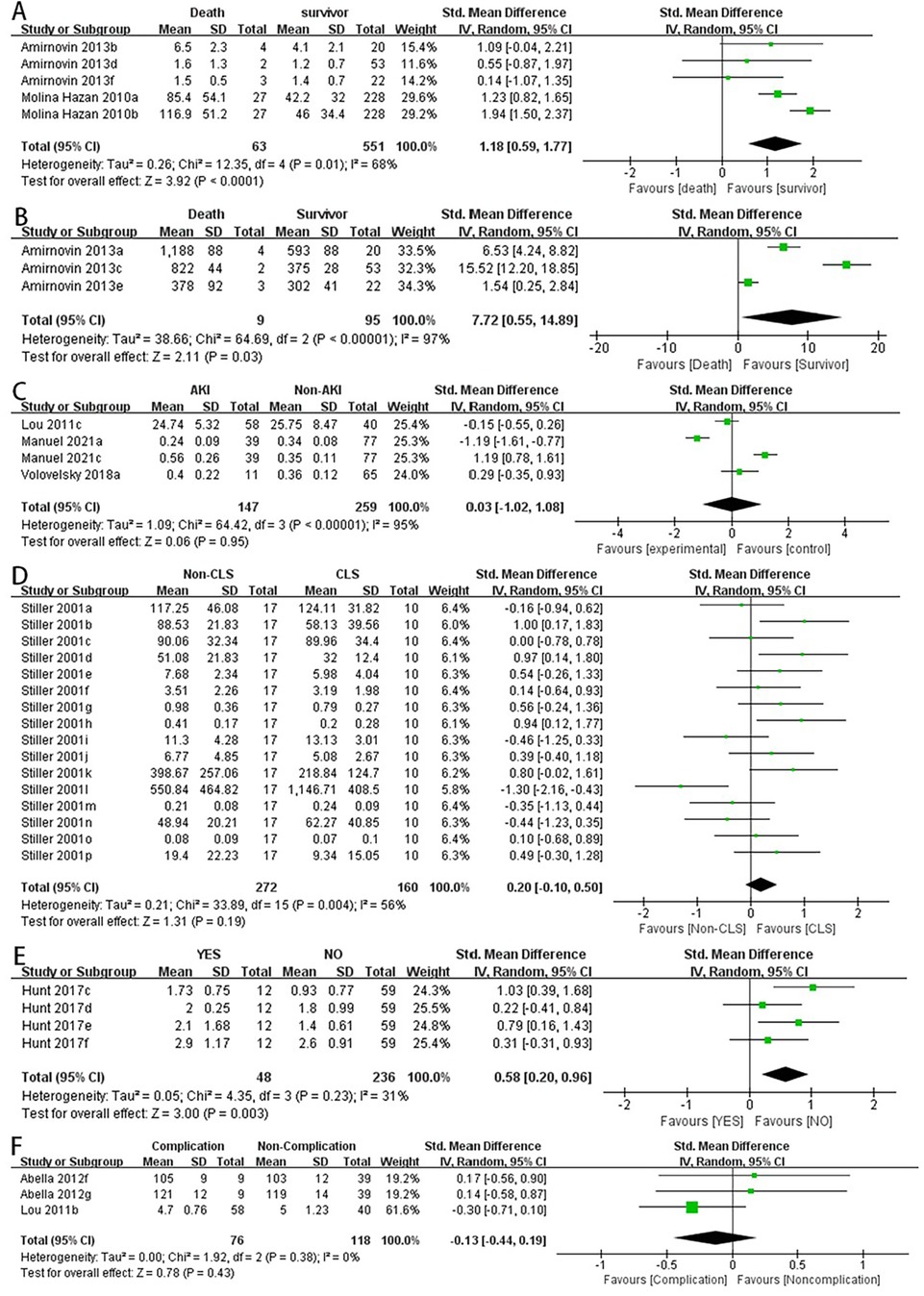
Figure 2. Forest plot of preliminary studies synthesis,lactic acid levels were compared between the dead group and the surviving group (A), BNP levels were compared between the dead group and the surviving group (B), serum creatinine levels were compared between the two groups whether AKI occurred (C), comparison of activation of the serum complement system and the occurrence of CLS after surgery in children with CHD (D), comparison of preoperative VWF activity between the two groups for postoperative thrombosis (E), comparison of blood glucose levels between the two groups for postoperative complications (F).
3.4.2 The pooled data for categorical variables showed2.1 Lower serum albumin levels were associated with an increased incidence of postoperative hypoalbuminemia in children with CHD (OR: 3.12, 95% CI: 1.66–5.84) (Figure 3C).
2.2 Lower serum albumin levels were associated with longer hospital stays in children with CHD after surgery (OR: 2.13, 95% CI: 1.14–3.97) (Figure 3D).
2.3 NT-pro BNP levels were not significantly associated with prolonged PICU stay in children after surgery (OR: 0.86, 95% CI: 0.23–3.29) (Figure 3A).
2.4 There was no significant difference in postoperative mortality between the high NLR and low NLR groups in children with CHD (OR: 1.09, 95% CI: 0.41–2.92) (Figure 3B).
2.5 There were no significant differences in postoperative mortality or infection rates between the high serum albumin and low serum albumin groups (OR: 1.45, 95% CI: 0.56–3.76) (Figure 3E) (OR: 1.30, 95% CI: 0.29–5.73) (Figure 3F).
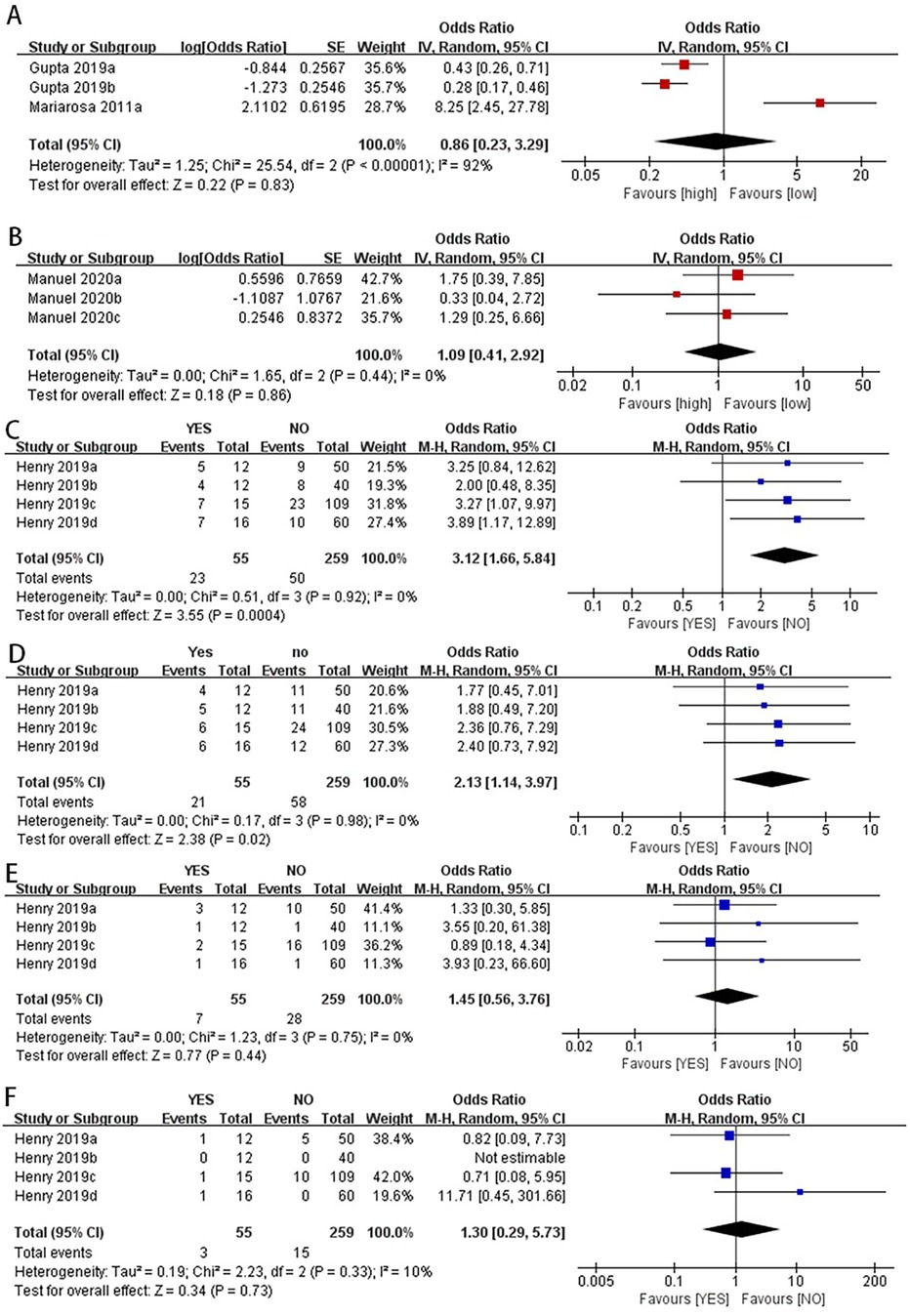
Figure 3. Categorical variables combined data analysis.NT-proBNP levels were not significantly associated with prolonged PICU stay in children after surgery (A). There was no significant difference in postoperative mortality between the high NLR and low NLR groups in children with CHD (B) the pooled data for categorical variables showed that lower serum albumin levels were associated with an increased incidence of postoperative hypoalbuminemia in children with CHD (C) lower serum albumin levels were associated with longer hospital stays in children with CHD after surgery (D) there were no significant differences in postoperative mortality or infection rates between the high serum albumin and low serum albumin groups (E,F).
We also statistically pooled studies that used mortality, AKI incidence, and thrombosis as outcome indicators, with details shown in Tables 2–4.
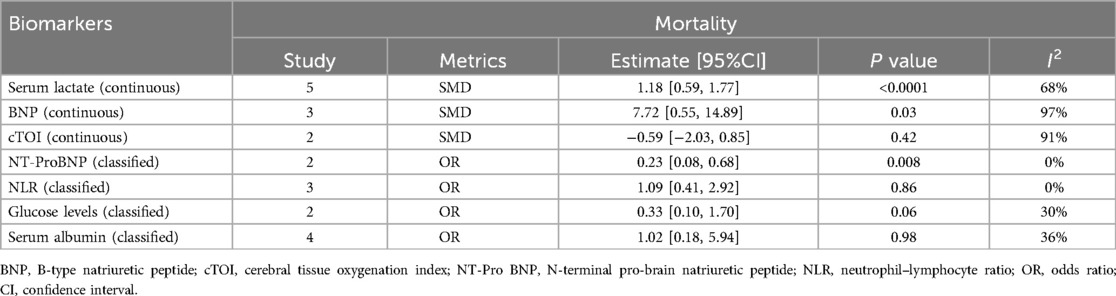
Table 2. Data pooled with mortality as an outcome indicator.
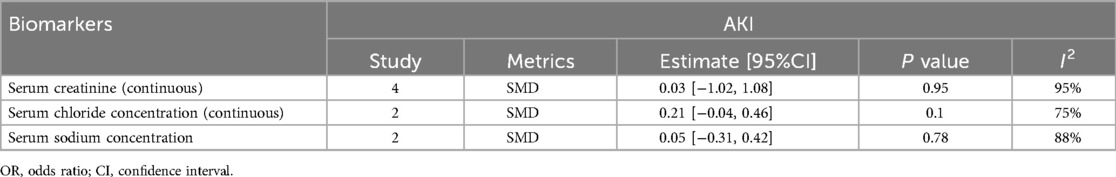
Table 3. Data merging with AKI as an outcome indicator.
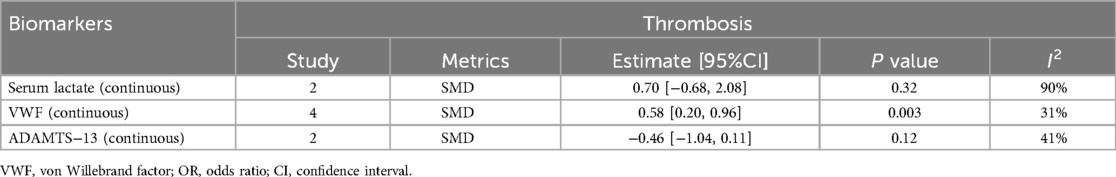
Table 4. Data merging with thrombosis as an outcome indicator.
3.5 Sensitivity analysisThe sensitivity analysis aimed to assess the robustness of the findings by altering certain assumptions and provide an initial exploration into the potential sources contributing to the heterogeneity observed across the included studies. Our sensitivity analysis showed that when we excluded the data reported by Mariarosa et al. in 2011 (28), the new OR value changed from non-significant to significant (OR: 0.35, 95% CI: 0.23–0.53) (Figure 4C).
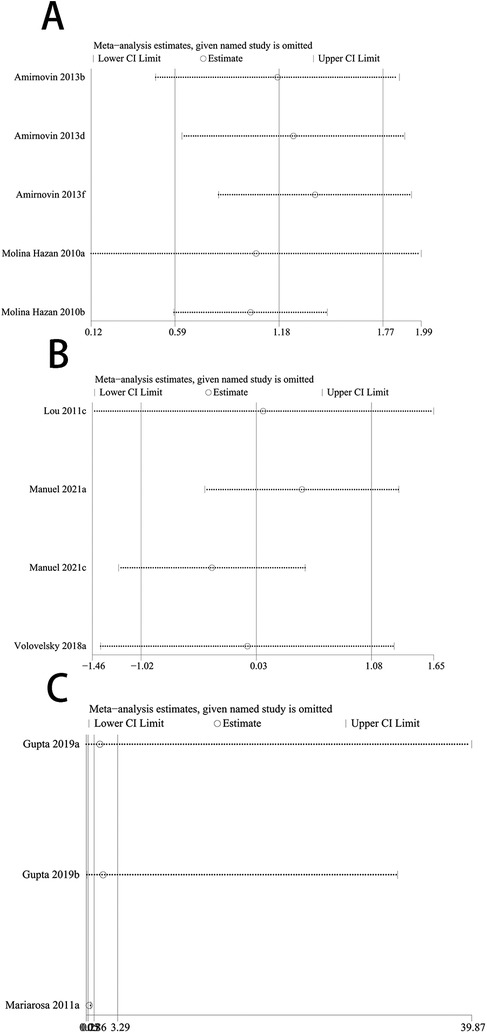
Figure 4. Forest plot of re-synthesis after eliminating one study identified by sensitivity analysis. Sensitivity analysis was performed for studies with I2 greater than 50%, I2 = 68% (A) I2 = 95% (B) both studies showed stability after the analysis was completed, When we excluded the data reported by Mariarosa et al. in 2011, the new OR value changed from non-significant to significant (C).
3.6 Publication bias assessmentConsidering the limited number of included studies, Egger's test was used to assess publication bias for serum creatinine, glycemia, BNP, serum lactate, VWF, serum albumin, NLR, NT-ProBNP, and serum complement system activation. The results showed significant publication bias for glycemia (P = 0.02), VWF (P = 0.009), and NLR (P = 0.04), as well as publication bias for serum albumin in predicting postoperative mechanical ventilation time (P = 0.04) and mortality (P = 0.04); there was no significant publication bias for serum lactate (P = 0.21) and BNP (P = 0.10) in predicting postoperative mortality, serum creatinine (P = 0.18) in predicting postoperative AKI incidence, serum complement system activation (P = 0.82) in predicting postoperative CLS incidence, and serum albumin in predicting postoperative infection rate (P = 0.09), total hospital stay (P = 0.16), and prolonged PICU stay (P = 0.14).
4 DiscussionCongenital heart disease occur during cardiac development and are present at birth (32)and is a major global health problem (33). Although great progress has been made in the treatment of CHD in recent years, it remains a significant cause of childhood mortality (34). Among children undergoing surgery for CHD, 10% to 20% are unexpectedly readmitted within 30 days, and 4% of surgeries result in death (35–38). Repeated hospitalizations of children place an emotional and economic burden on patients’ families and strain the healthcare system (39). There is strong interest in identifying early markers to predict impending major adverse events following surgical repair of CHD defects, driven by the significant mortality risk associated with most such surgeries (19, 40, 41). Currently, little attention is paid to the prediction of readmission, mortality, or postoperative complications in children after congenital heart surgery, especially the evaluation of biomarkers compared to standalone clinical models (13).
Our study found that the serum lactate level was higher in the postoperative death group compared to the survival group in children with CHD after surgery (SMD: 1.18, 95% CI: 0.59–1.77). The end-product of glycolysis, pyruvate, is converted into serum lactate. In the presence of oxygen, lactate is converted back to pyruvate through mitochondrial processes. However, under anaerobic conditions, cellular lactate concentrations increase, resulting in elevated serum lactate levels. Therefore, hyperlactatemia may reflect tissue oxygen debt, and serum lactate levels can also serve as a clinical indicator of tissue perfusion and systemic oxygen delivery after CHD surgery (42). In response to increased pressure overload, volume expansion, and myocardial wall stress, ventricular myocytes synthesize and secrete NT-proBNP into the bloodstream (43). NT-proBNP has recently emerged as a potential prognostic marker for early postoperative outcomes in pediatric and congenital cardiac surgery (44–46). Nevertheless, inconsistencies exist regarding the findings. For instance, Qu et al. demonstrated NT-proBNP levels 1 h postoperatively strongly predicted prolonged mechanical ventilation, intensive care unit (ICU) stay, and inotropic therapy requirement (13). Our study found that lower postoperative NT-proBNP levels were associated with lower mortality (OR: 0.23, 95% CI: 0.08–0.68) and shorter mechanical ventilation times (OR: 0.40, 95% CI: 0.18–0.90) in children with CHD after surgery. Hypoalbuminemia caused by decreased serum albumin levels can develop through a combination of decreased synthesis, increased degradation, and the dilutional effect of resuscitation (30); our study found that children with higher serum albumin levels had longer hospital stays (random-effects model, OR: 3.12, 95% CI: 1.66–5.84). For infants with preoperative hypoalbuminemia, treating and/or preventing potential protein malnutrition or heart failure, rather than supplementing albumin, may have a greater impact on improving postoperative outcomes.
In addition, our study found that the BNP level was higher in the postoperative death group compared to the survival group in children with CHD (SMD: 7.72, 95% CI: 0.55–14.89). BNP, a cardiac hormone with diuretic, natriuretic, and vasodilatory properties, is primarily secreted by the ventricles in response to volume expansion and pressure overload. BNP levels are elevated in various cardiovascular diseases, such as heart failure and myocardial infarction (47). Although BNP serves as a biomarker for diagnosing, risk stratifying, and managing heart failure in adults, its applications in neonates and infants undergoing surgical repair or palliation of congenital heart defects remain unestablished (10). VWF, a large multimeric glycoprotein, mediates platelet-platelet and platelet-subendothelial adhesion. After release from activated platelets and endothelial cells, VWF exists primarily as large, highly reactive multimers (12). Our analysis found that preoperative VWF activity was higher in children who developed thrombosis after surgery compared to those without thrombosis (SMD: 0.58, 95% CI: 0.20–0.96).
However, our meta-analysis also has certain limitations, we focused on the short-term predictive value of biomarkers after CHD surgery, and the data we could collect were too small to conduct a meta-analysis on the long-term prognosis (cardiac output, neurodevelopment eta.), which also suggests that a larger number of studies are needed to provide original data. The type of surgery received by patients and albumin was used preoperatively as resuscitation fluid may affect the predictive value of biomarkers. However, the data provided by the included literature were limited, and there was no way to conduct subgroup analysis, which led to a certain risk of bias in the study results, which needs to be solved by further research. Despite removing a highly sensitive study and re-synthesizing the data, moderate heterogeneity persisted even with a random-effects model, potentially compromising the robustness of our conclusions. Secondly, some of the included studies were retrospective, with poor control of confounding factors, resulting in lower quality of some studies. Although this analysis included a wide range of biomarkers, the detailed data for each indicator were not sufficient, and some studies had high heterogeneity and publication bias. However, our study is the first and largest to explore the value of biomarkers in predicting adverse outcomes in children with CHD after surgery from an evidence-based medicine perspective. The analysis was relatively comprehensive and can provide guidance for future clinical treatment and a theoretical basis for constructing clinical risk prediction models.
5 ConclusionSerum lactate, NT-proBNP, and serum albumin are valuable biomarkers for predicting adverse outcomes in children with CHD, as higher serum lactate and NT-proBNP levels and lower serum albumin levels indicate poorer postoperative prognosis in children with CHD. Nonetheless, further investigation is warranted to elucidate the relationship between these biomarkers and CHD prognosis.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributionsSZ: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing. LL: Data curation, Formal Analysis, Investigation, Validation, Writing – review & editing. XJ: Conceptualization, Supervision, Visualization, Writing – review & editing. DD: Supervision, Writing – review & editing. SM: Conceptualization, Supervision, Visualization, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Liu Y, Chen S, Zühlke L, et al. Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol. (2019) 48(2):455–63. doi: 10.1093/ije/dyz009
PubMed Abstract | Crossref Full Text | Google Scholar
3. van der Linde D, Konings EE, Slager MA, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. (2011) 58(21):2241–7. doi: 10.1016/j.jacc.2011.08.025
PubMed Abstract | Crossref Full Text | Google Scholar
4. Maddhesiya J, Mohapatra B. Understanding the genetic and non-genetic interconnections in the aetiology of isolated congenital heart disease: an updated review: part 1. Curr Cardiol Rep. (2024) 26(3):147–65. doi: 10.1007/s11886-024-02022-9
PubMed Abstract | Crossref Full Text | Google Scholar
5. Cao M, Liu Y, Sun Y, Han R, Jiang H. Current advances in human-induced pluripotent stem cell-based models and therapeutic approaches for congenital heart disease. Mol Cell Biochem. (2025) 480(1):159–72. doi: 10.1007/s11010-024-04997-z
PubMed Abstract | Crossref Full Text | Google Scholar
6. Baumgartner H, De Backer J, Babu-Narayan SV, et al. 2020 ESC guidelines for the management of adult congenital heart disease. Eur Heart J. (2021) 42(6):563–645. doi: 10.1093/eurheartj/ehaa554
PubMed Abstract | Crossref Full Text | Google Scholar
7. Wu W, He J, Shao X. Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990–2017. Medicine (Baltimore). (2020) 99(23):e20593. doi: 10.1097/MD.0000000000020593
PubMed Abstract | Crossref Full Text | Google Scholar
8. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392(10159):1736–88. doi: 10.1016/S0140-6736(18)32203-7
PubMed Abstract | Crossref Full Text | Google Scholar
9. Hu Z, Yuan X, Rao K, Zheng Z, Hu S. National trend in congenital heart disease mortality in China during 2003 to 2010: a population-based study. J Thorac Cardiovasc Surg. (2014) 148(2):596–602.e591. doi: 10.1016/j.jtcvs.2013.08.067
PubMed Abstract | Crossref Full Text | Google Scholar
10. Amirnovin R, Keller RL, Herrera C, et al. B-type natriuretic peptide levels predict outcomes in infants undergoing cardiac surgery in a lesion-dependent fashion. J Thorac Cardiovasc Surg. (2013) 145(5):1279–87. doi: 10.1016/j.jtcvs.2012.07.067
PubMed Abstract | Crossref Full Text | Google Scholar
11. Diller GP, Kempny A, Liodakis E, et al. Left ventricular longitudinal function predicts life-threatening ventricular arrhythmia and death in adults with repaired tetralogy of fallot. Circulation. (2012) 125(20):2440–46. doi: 10.1161/CIRCULATIONAHA.111.086983
PubMed Abstract | Crossref Full Text | Google Scholar
12. Hunt R, Hoffman CM, Emani S, et al. Elevated preoperative von willebrand factor is associated with perioperative thrombosis in infants and neonates with congenital heart disease. J Thromb Haemostasis. (2017) 15(12):2306–16. doi: 10.1111/jth.13860
PubMed Abstract | Crossref Full Text | Google Scholar
13. Gupta RK, Zheng H, Cui Y, et al. Change in N-terminal pro B-type natriuretic peptide levels and clinical outcomes in children undergoing congenital heart surgery. Int J Cardiol. (2019) 283:96–100. doi: 10.1016/j.ijcard.2019.02.025
PubMed Abstract | Crossref Full Text | Google Scholar
15. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
PubMed Abstract | Crossref Full Text | Google Scholar
16. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. (2018) 27(6):1785–805. doi: 10.1177/0962280216669183
PubMed Abstract | Crossref Full Text | Google Scholar
17. Kim SR, Kim K, Lee SA, et al. Effect of red, processed, and white meat consumption on the risk of gastric cancer: an overall and dose-response meta-analysis. Nutrients. (2019) 11(4):826. doi: 10.3390/nu11040826
PubMed Abstract | Crossref Full Text | Google Scholar
18. Molina Hazan V, Gonen Y, Vardi A, et al. Blood lactate levels differ significantly between surviving and nonsurviving patients within the same risk-adjusted classification for congenital heart surgery (RACHS-1) group after pediatric cardiac surgery. Pediatr Cardiol. (2010) 31(7):952–60. doi: 10.1007/s00246-010-9724-7
PubMed Abstract | Crossref Full Text | Google Scholar
19. Abella R, Satriano A, Frigiola A, et al. Adrenomedullin alterations related to cardiopulmonary bypass in infants with low cardiac output syndrome. J Matern Fetal Neonatal Med. (2012) 25(12):2756–61. doi: 10.3109/14767058.2012.718393
PubMed Abstract | Crossref Full Text | Google Scholar
20. Lou S, Ding F, Long C, Liu J, Zhao J, Feng Z. Effects of peri-operative glucose levels on adverse outcomes in infants receiving open-heart surgery for congenital heart disease with cardiopulmonary bypass. Perfusion. (2011) 26(2):133–9. doi: 10.1177/0267659110389843
PubMed Abstract | Crossref Full Text | Google Scholar
21. Manuel V, Miana LA, Turquetto A, Guerreiro GP, Fernandes N, Jatene MB. The role of the neutrophil-lymphocyte ratio for pre-operative risk stratification of acute kidney injury after tetralogy of fallot repair. Cardiol Young. (2021) 31(6):1009–14. doi: 10.1017/S1047951121001943
PubMed Abstract | Crossref Full Text | Google Scholar
22. Volovelsky O, Terrell TC, Swain H, Bennett MR, Cooper DS, Goldstein SL. Pre-operative level of FGF23 predicts severe acute kidney injury after heart surgery in children. Pediatr Nephrol. (2018) 33(12):2363–70. doi: 10.1007/s00467-018-4024-1
PubMed Abstract | Crossref Full Text | Google Scholar
23. Stiller B, Sonntag J, Dähnert I, et al. Capillary leak syndrome in children who undergo cardiopulmonary bypass: clinical outcome in comparison with complement activation and C1 inhibitor. Intensive Care Med. (2001) 27(1):193–200. doi: 10.1007/s001340000704
PubMed Abstract | Crossref Full Text | Google Scholar
24. Parker DM, Everett AD, Stabler ME, et al. Biomarkers associated with 30-day readmission and mortality after pediatric congenital heart surgery. J Card Surg. (2019) 34(5):329–36. doi: 10.1111/jocs.14038
PubMed Abstract | Crossref Full Text | Google Scholar
25. Kimura S, Iwasaki T, Shimizu K, et al. Hyperchloremia is not an independent risk factor for postoperative acute kidney injury in pediatric cardiac patients. J Cardiothorac Vasc Anesth. (2019) 33(7):1939–45. doi: 10.1053/j.jvca.2018.12.009
PubMed Abstract | Crossref Full Text | Google Scholar
26. Leite HP, Fisberg M, Vieira JGH, De Carvalho WB, Chwals WJ. The role of insulin-like growth factor I, growth hormone, and plasma proteins in surgical outcome of children with congenital heart disease. Pediatr Crit Care Med. (2001) 2(1):29–35. doi: 10.1097/00130478-200101000-00007
PubMed Abstract | Crossref Full Text | Google Scholar
27. Aly SA, Zurakowski D, Glass P, Skurow-Todd K, Jonas RA, Donofrio MT. Cerebral tissue oxygenation index and lactate at 24hours postoperative predict survival and neurodevelopmental outcome after neonatal cardiac surgery. Congenit Heart Dis. (2017) 12(2):188–95. doi: 10.1111/chd.12426
PubMed Abstract | Crossref Full Text | Google Scholar
28. Perez-Piaya M, Abarca E, Soler V, et al. Levels of N-terminal-pro-brain natriuretic peptide in congenital heart disease surgery and its value as a predictive biomarker. Interact Cardiovasc Thorac Surg. (2011) 12(3):461–6. doi: 10.1510/icvts.2010.245803
PubMed Abstract | Crossref Full Text | Google Scholar
29. Manuel V, Miana LA, Guerreiro GP, et al. Prognostic value of the preoperative neutrophil-lymphocyte ratio in patients undergoing the bidirectional glenn procedure. J Card Surg. (2020) 35(2):328–34. doi: 10.1111/jocs.14381
PubMed Abstract | Crossref Full Text | Google Scholar
30. Henry BM, Borasino S, Ortmann L, et al. Perioperative serum albumin and its influence on clinical outcomes in neonates and infants undergoing cardiac surgery with cardiopulmonary bypass: a multi-centre retrospective study. Cardiol Young. (2019) 29(6):761–7. doi: 10.1017/S1047951119000738
PubMed Abstract | Crossref Full Text | Google Scholar
31. Odek C, Kendirli T, Yildirim-Yildiz N, et al. Perioperative factors associated with hypergl
留言 (0)