Hemophilia is a coagulation disorder caused by deficiencies in specific coagulation factors.[1,2] The joints are the most common sites for bleeding in hemophilia patients, and the knee is the most affected joint. This is thought to be due both to the large size of the synovial membrane and to rotational forces.[3,4] Repetitive intra-articular bleeding and iron accumulation in the synovium can cause blood-induced synovitis and cartilage injury, which results in progressive joint damage and hemophilic arthropathy.[3,5,6]
Total knee arthroplasty (TKA) is an effective treatment for end-stage hemophilic arthropathy with severe joint deterioration.[3,7] However, during TKA surgery for hemophilic arthropathy, it was observed that the knees of hemophilic patients exhibited different anatomies for which standard implants were not always suitable; standard TKA implants matching the anterior-posterior (AP) plane were not appropriate for use in the mediolateral plane. Based on the authors’ experience and the difficulties encountered during surgery, a comparison was undertaken; the bone structures of the knee joints of TKA patients with a diagnosis of hemophilic arthropathy were compared with those of primary knee osteoarthritis patients using standard implants.
In this study, the anatomical differences of the bony structure of the knee joint in patients with hemophilia were evaluated, and the results were compared with the knees of patients with primary gonarthrosis and no arthrosis.
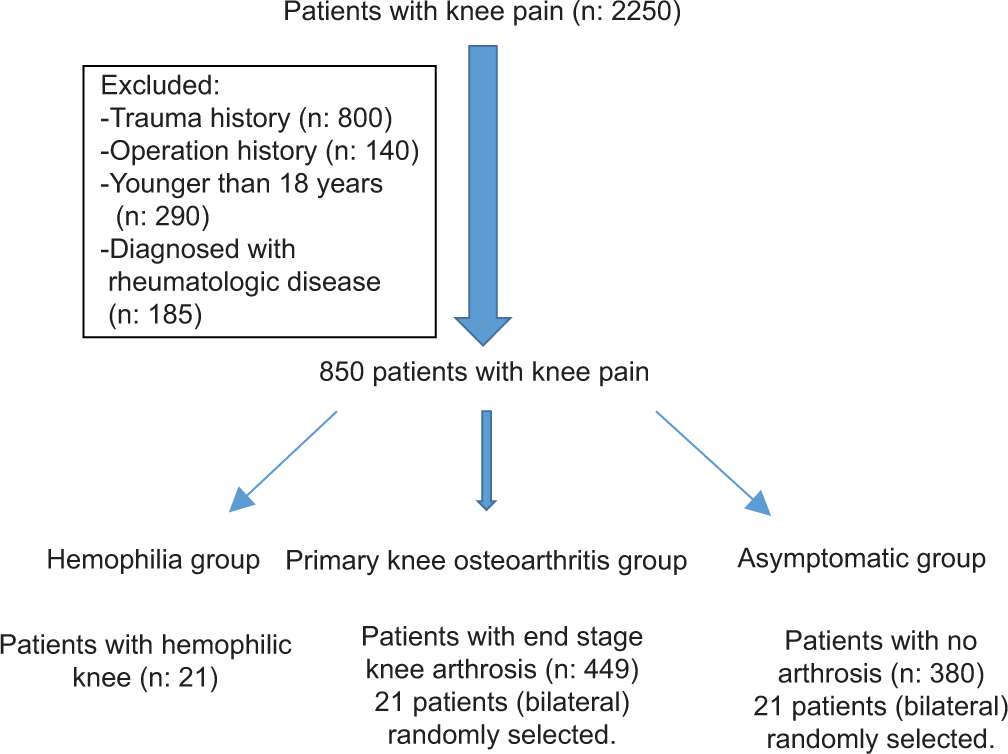
MATERIAL AND METHODSThis study reviewed 41 knees in 21 patients (with an Arnold-Hilgartner classification[8] of Stages 4 and 5 hemophilic arthropathy) who underwent TKA in the authors’ institution. This research has been approved by the IRB (Institutional Review Board 2017/146) of the authors’ affiliated institutions. Informed consent was obtained from each patient. Two control groups including asymptomatic patients and primary knee osteoarthritis patients were formed to compare the measurements with the group of patients with hemophilia. All the hemophilic patients were male who were diagnosed with hemophilia A; the patients in both control groups were randomly selected (see flaw chart). All asymptomatic patients were recruited through their presentation at the authors’ outpatient clinic with knee pain; they had no arthrosis findings on X-rays. The patients with primary knee osteoarthritis were selected from those patients in the clinic who had primary TKA with the diagnosis of primary knee osteoarthritis [Table 1].
Table 1:: Average values of the measurements (in mm).
Parameters Asymptomatic Gonarthrosis Hemophilic FAW 83.9±28 mm 67.4±5.7 mm 62.5±5.1 mm FMW 90.8±8 mm 86.36±4.9 mm 87±6.6 mm FD 35.2±3.6 mm 35.8±4.6 mm 25±3.2 mm TD 28.2±2.7 mm 30±5.2 mm 22.7±3.2 mm ATJLD 47.2±6.1 mm 50.2±5.6 mm 49.3±6.5 mm TPW 85.6±5 mm 88.8±6.4 mm 83.56±5.4 mm MTPW 42.2±3.2 mm 44.6±3.96 mm 41.83±3.4 mm LTPW 42.8±4.1 mm 44.2±3.3 mm 41.87±3.5 mm SLOPE 15.3±19.9º 9.2±2.3° 5.6±6.4° MPTA 87.6±1.6° 84.4±3.3° 84.6±4.8° TAW 54.5±4.8 mm 50.6±5.2 mm 53.1±5.5 mm Radiographic measurementsPre-operative full-leg radiographs were obtained, including AP and lateral images of both knees with patients in a bipedal stance with their feet in neutral rotation and the patellae pointing forward. A picture archiving and communication system (Extreme PACS, Ankara, Turkey) was used for all measurements. All measurements were recorded independently by the same author (M.E.K). The distance between the beam origin and the detector plate was 120 cm in all cases. This software made it possible to measure the distances on the AP and lateral knee radiographs with full accuracy and to eliminate changes related to the magnification. Patients were excluded from the study if any of the following applied: They had X-rays taken because of knee trauma or a fracture extending to the knee joint, they had undergone previous knee surgery, they were diagnosed with a metabolic or inflammatory rheumatological disease, they were prescribed steroid therapy for more than 6 months for any reason, or they exhibited an advanced degree of lower extremity malalignment (more than 20° of varus or 10° of valgus deformity).
Export to PPT
The following items were measured:
Femoral mediolateral width (FMW): The line between the medial and lateral epicondyles at their most prominent points (|AB|) [Figure 1].
Femoral AP width (FAW): The distance between the anterior and posterior tangential and perpendicular line according to diaphysis on the distal femoral condyles (|IJ|) [Figure 2].
Femur diaphysis (FD) width and tibia diaphysis (TD) width: The width of the femur and tibia on their middiaphysis.
Adductor tubercle joint line distance (ATJLD): The perpendicular distance between the adductor tubercle and the joint line of the knee (|EF|) [Figure 3].
Tibial plateau width (TPW): The line between the most prominent points of the medial and lateral edge of the plateau (|CD|) [Figure 1].
Tibial AP width (TAW): The distance between two lines on the tibial plateau that is perpendicular to the diaphysis of the tibia and tangent to the anterior and posterior edges of the tibial plateau on the lateral radiographs (|KL|) [Figure 2].
Medial TPW and lateral TPW: The distances between the medial and lateral tibial eminences and the most prominent points of the medial and lateral edges of the plateau (|CD| - |GH| and |GH|) [Figure 3].
Medial proximal tibial angle (MPTA): The angle between the tibial plateau and the tibial mechanical axis [Figure 4].
Tibial slope: The angle between the line of the diaphyseal axis and the line drawn using the highest two points of the anterior and posterior edges of the medial plateau [Figure 2].

Figure 1:: Demonstration of radiographic measurement of femoral mediolateral width (|AB|) and tibial plateau width (|CD|).
Export to PPT

Figure 2:: Demonstration of radiographic measurement of femoral anteroposterior width (|IJ|), tibial anteroposterior width (|KL|), and tibial slope (TS).
Export to PPT

Figure 3:: Demonstration of radiographic measurement of adductor tubercle joint line distance (|EF|), medial tibial plateau width, and lateral tibial plateau width (|CD| - |GH| and |GH|).
Export to PPT

Figure 4:: Demonstration of radiographic measurement of medial proximal tibial angle.
Export to PPT
The femoral and tibial aspect ratios were calculated by dividing the measured ML widths by the measured AP widths on the X-rays (femoral aspect ratio: FMW/FAW and tibial aspect ratio: TPW/TAW). The aspect ratio allows for the estimation of prosthesis shape and the underhanging/ overhanging of the components.[8]
The ratio between the height of the femur metaphysis and the FMW (distal femoral ratio: ATJLD/FMW), the ratio of the FD and the FMW (FD/FMW), and the tibial plateau (TD/TPW) distances were evaluated to better assess the knee anatomy.
PCL-substituting Genesis II knee arthroplasty (Smith and Nephew, Memphis, TN, USA) was used in all patients through a medial parapatellar approach. Patella resurfacing prosthesis was not utilized, while patellar denervation was done in all patients [Figures 5-8].

Figure 5:: Pre-operative anteroposterior radiograph of patient with hemophilic arthropathy.
Export to PPT

Figure 6:: Pre-operative lateral radiograph of patient with hemophilic arthropathy.
Export to PPT

Figure 7:: Post-operative anteroposterior radiograph of patient with hemophilic arthropathy.
Export to PPT

Figure 8:: Post-operative lateral radiograph of patient with hemophilic arthropathy. The mismatch was especially evident in the tibial component.
Export to PPT
Statistical analysisThe data were analyzed using SPSS software (version 22.0 for Windows) (SPSS Inc., Chicago, USA). Mean, median, standard deviation, maximum, and minimum were used as descriptive statistical methods. Normality of distribution was tested using the Shapiro–Wilk test. Comparisons were made using a one-way ANOVA test, and the significance value was accepted as P < 0.05 at a 95% confidence interval. For comparisons between the groups, Tukey’s range test was used among the post hoc assessments.
RESULTSThe FMW was measured as 87 ± 6.6 mm, and the knee joints were significantly narrower compared with both healthy individuals and the primary knee osteoarthritis group (P < 0.05). However, the TPW was measured at 83.56 ± 5.4 mm, which was similar to the asymptomatic group (P = 0.9) but significantly narrower compared with the primary knee osteoarthritis group (P < 0.05). With the correlation in the TPW measurements, the medial and lateral plateaus were significantly narrower in the hemophilic arthropathy group (P < 0.05).
There was no difference in the primary knee osteoarthritis and hemophilic arthropathy groups for tibial slope measurements (P = 0.213). However, a smaller slope was evident in hemophilic patients compared with asymptomatic individuals (P < 0.05).
No significant difference in the MPTA measurements was detected between the hemophilic and primary knee osteoarthritis groups (P = 0.811), but the MPTA was less when compared with the asymptomatic group (P < 0.05). There were no significant differences in ATJLD between all the groups. For the hemophilic group, the TD and FD were significantly narrower – as in the FD and TD measurements (P < 0.05) [Table 1].
The hemophilic patients demonstrated larger femoral aspect ratios than the asymptomatic group (1.38 [95% CI, 1.13–1.79] vs. 1.32 [95% CI, 1.20–1.65], P < 0.05); however, there were no observable differences with the primary knee osteoarthritis group. For the tibial aspect ratios, the hemophilic group had a smaller ratio than the primary knee osteoarthritis group (1.58 [95% CI, 1.24–2.19] vs. 1.76 [95% CI, 1.50–2.04], P < 0.05), and there were no significant differences with the asymptomatic group. This evidence reveals that the knees of patients with hemophilia are mismatched between the femoral and tibial sides in comparison with the other groups [Figure 9].

Figure 9:: Graphic showing the comparison of the femoral and tibial aspect ratios between all groups.
Export to PPT
DISCUSSIONThe knee is the most commonly involved joint in end-stage hemophilic arthropathy, and TKA is a complex and challenging procedure.[9,10] The knee’s anatomy is distorted due to physeal overgrowth in childhood, widening of the femoral intercondylar notch, large osteophytes, and squaring of the patella.[10,11] The larger femoral and tibial surfaces cause a mismatch in implant sizing as they are wider in the mediolateral plane compared with the AP plane.[10,11] Restoring the mechanical axis and achieving accurate alignment are difficult in such a scenario.[11] Using conventional jigs, standard operation techniques and implants that rely on visual confirmation of alignment accuracy can lead to high possibilities of error, unsuitable implant size, poor implant fit, and an increased incidence of outliers.
One of the most important factors for successful TKA is that the components to be implanted must be in proper rotational alignment.[12-14] The previous studies recommend that the femoral component should be inserted parallel to the transepicondylar axis or the AP axis.[14-18] Trochlear wear or intercondylar osteophytes sometimes make it difficult to detect both the medial and lateral epicondyles or to accurately locate the AP axis.[16,19]
Almost all of the TKA implants are produced in accordance with the anthropometric characteristics of Western, male,[19] White patients,[20,21] although TKA is regarded as a highly successful surgery resulting in pain reduction, an improved quality of life, and enhanced knee joint function.[22]
The use of TKA implants that do not fit the anthropometrical features of the patient may cause more blood loss, overhang/ underhang, early loosening, irritation, unstable implant fixation, and ROM restriction. To prevent these complications and obtain better results, implants suitable for a patient’s own knee morphometry should be used.
The anthropometric characteristics of the bony structures of the knee (distal femur and proximal tibia) between different ethnicities and genders have been evaluated in numerous studies.[23-27] Kim et al. found that the AP dimensions and the mediolateral width of the distal femur and plateau tibia of Korean patients were smaller compared with Western patients.[28] They discovered that the knees of black patients had larger AP dimensions than the knees of White patients in their study.[27] The anatomical differences of the distal femur and proximal tibia were also compared between males and females. The distal femurs and proximal tibias of the males tended to be larger than in the females.[21,29] However, according to the best of the authors’ knowledge, this is the first study to evaluate the bony dimensions of the knee in hemophilic patients suffering with severe hemophilic arthropathy, arthritic patients who have undergone TKA, and asymptomatic healthy individuals. It was anticipated that this study would simplify research for the clinical implications of these anthropometric differences and ascertain whether TKA manufacturers would give price to address the potential for compromised implant fit.
The aspect ratios were described as the mediolateral width divided by the AP width of the distal femur or the proximal tibia. These calculations can be used as a guide for femoral component sizing. A higher ratio means a greater mediolateral width for the AP size, while a lower ratio means a smaller mediolateral dimension for the AP size.
It is important to note that aspect ratios can be useful for predicting component sizing, and femoral and tibial shapes can be better understood and maintain a measure of the knee dimension between patients. In this study, the knees of hemophilia patients had smaller AP dimensions compared with the asymptomatic patients’ knees in terms of femoral aspect ratio. This correlates with the relatively higher ML/ AP aspect ratio. This analysis of tibial aspect ratios revealed that the knees of hemophilic patients had larger AP dimensions than did the knees of patients suffering from primary arthrosis (which results in a smaller tibial aspect ratio). This could result in mismatches where standard tibial components would be relatively small and incompatible for patients with hemophilia in terms of AP dimensions. Ultimately, an unsuitable fit could also result in the underhang/overhang of the components, which could lead to soft-tissue impingements, ROM restrictions, pain, and early loosening.[30]
The limitations of this research are that it is a retrospective study and the measurements were performed on AP and lateral radiographs. In addition, the results could be more useful if they were supplemented with pre-operative anatomical measurements or 3D computed tomography (CT) analysis of the knees. Although the bony anatomy of the knee joint is better determined by CT analysis, the templating of the TKA designs is performed preoperatively on standard AP and lateral radiographs of the knee to obtain the proper size and position of the TKA implant. Therefore, analysis of the anatomical measurements on standard radiographs is not a misapplication in clinical practice.
The findings confirm that the knees of hemophilic patients have a mismatch between the femoral and tibial sides in comparison with the other groups. The use of unsuitable implants may lead to complications, such as early loosening and limitation of knee motion, and TKA implants produced for standard patient populations may not be suitable for patients with hemophilia. For satisfactory results, patient-specific implants should be considered for use in hemophilic patients.
CONCLUSIONThe hemophilic knees have a mismatch between the femoral and tibial sides. The hemophilic patients demonstrated larger femoral aspect ratios than the asymptomatic group. For the tibial aspect ratios, the hemophilic group had a smaller ratio than the primary knee osteoarthritis group, and there were no significant differences with the asymptomatic group.
留言 (0)