Global life expectancy is on the rise, leading to a significant increase in the elderly population worldwide. Projections indicate that by 2050, the number of individuals aged 80 years or older will triple, reaching 426 million (1). Within this demographic shift, gallbladder and biliary tract diseases emerge as prominent concerns within the spectrum of digestive tract disorders. Notably, women and the elderly are particularly vulnerable to these conditions (2). In fact, the prevalence of gallstones among the elderly ranges between 14% and 23%, while it approaches 80% among nonagenarians (3).
It´s crucial to recognize that elderly individuals with biliary disorders might initially exhibit mild symptoms but can rapidly decompensate without proper treatment. Conditions such as acute cholecystitis pose a significant threat as they can rapidly escalate to systemic inflammatory response syndrome, sepsis, and death (4). While age itself may not directly correlate with the severity of acute cholecystitis, the presence of multiple comorbidities in elderly patients can significantly contribute to the progression of the disease (5, 6).
The first therapeutic option in elderly patients with acute cholecystitis is supportive care, consisting of intravenous hydration, analgesia and antibiotics (3, 7). Although supportive care is a common treatment option because it avoids the risk associated with anesthesia and shortens the hospital stay, it does not solve the problem and carries a high risk of recurrence (7).
Currently, percutaneous gallbladder drainage is the most widely used non-surgical procedure in elderly patients with acute cholecystitis (3). It has been argued that it could be a definitive treatment for acute cholecystitis in high-risk elderly patients (8). However, other studies advocate percutaneous drainage as a bridge to laparoscopic cholecystectomy in high-risk elderly patients (9), as well as in octogenarians with acute cholecystitis (10).
Early or delayed cholecystectomy (during index admission) is the treatment of choice for acute cholecystitis in patients fit for surgery (3). The Tokyo guidelines (5), the American Association of Surgery of Trauma (AAST) system (11), and the American Association of Anesthesiologists (ASA) can be used to stratify patients. The surgical treatment of acute cholecystitis in elderly people has paralleled the evolution of laparoscopic techniques in recent decades (4, 6, 10, 12–27).
Recently, endoscopic ultrasonography (EUS)-guided drainage of the gallbladder is being used as definitive therapy or as a bridge to delayed cholecystectomy in patients with acute cholecystitis unfit for emergency surgery (28–40). EUS-guided gallbladder drainage has also been combined with endoscopic retrograde cholangiopancreatography (ERCP) in patients with coexisting choledochal biliary stones (38).
Whichever procedure is used, long-term follow-up of elderly patients is needed (3). Many studies included patients with acute cholecystitis in their 60s, 70s and 80s, but the age mix precluded drawing decade-tailored conclusions (41). Therefore, one-year outcomes in patients aged 70 years and older with acute cholecystitis were specifically compared in this single-center study.
Patients and methods Study designThis retrospective observational study examined a consecutive cohort of patients aged 70 years or older with acute cholecystitis (ICD-10 Codes: K81, K82) who were admitted between May 2021 and May 2022 at Doctor Balmis General University Hospital, Alicante, Spain. Patient care followed the established standard protocols of the hospital. Informed consent was not obtained from the patients due to the retrospective nature of the study. The study protocol adhered to the ethical guidelines of the 1975 Declaration of Helsinki (6th revision, 2008). This study was approved by the Research Ethics Committee of the Dr. Balmis Hospital (CEIm: PI2024-078). The study design and analysis complied with the STROCCS Reporting Guidelines for Cohort Studies (42).
Exclusion criteriaPatients meeting any of the following criteria were excluded from the study: (a) history of prior cholecystitis episodes, ERCP, or previous cholecystostomy; (b) concurrent diagnosis of pancreatitis or any terminal illness with a life expectancy of less than one year; (c) acute cholecystitis diagnosed as a secondary condition, or in conjunction with acute pancreatitis, cholangitis, bile duct disorders, or gastrointestinal malignancy; (d) acute cholecystitis discovered incidentally during another surgical procedure, Mirizzi syndrome, or prior diagnosis of gallbladder cancer. Incidental gallbladder cancer was not an exclusion criterion. We intentionally did not include four patients who underwent EUS-guided gallbladder drainage during the index admission, as the small number of patients would have prevented a statistical analysis.
Demographics, baseline characteristics, and diagnosisIn addition to demographic data and past medical and surgical history, Charlson comorbidity index (CCI) (43), ECOG and Karnofsky performance status were recorded. The ASA score was used to ascertain patient's surgical risk. The definitive diagnosis of acute cholecystitis was graded according to the Tokyo guidelines. Duration of symptoms >72 h prior to admission was selected to categorize patients as it defines grade II in the Tokyo guidelines (5). Given that the Tokyo guidelines flowchart adds the coexistence of jaundice (total bilirubin >2 mg/dl) as one of the negative predictive factors in grade III acute cholecystitis, this laboratory value at admission was also selected as threshold to categorize patients (44). Laboratory values at admission used to define grades II and III in the Tokyo guidelines (i.e., creatinine >2.0 mg/dl, INR >1.5, platelet count <100,000/mm3, and white blood cell count >18,000/mm3) were selected as thresholds to categorize patients (5).
Index treatment modalitiesSupportive care consisted of intravenous hydration, analgesia utilizing acetaminophen or non-steroidal anti-inflammatory drugs, and administration of antibiotics (3). Percutaneous gallbladder drainage was carried out through either transperitoneal or transhepatic routes, accompanied by a radiological assessment prior to drain removal. In instances where surgery was deemed necessary, laparoscopic cholecystectomy was the preferred approach in most cases.
Follow-upAdditional procedures, hospital readmissions due to acute cholecystitis-related complications, and outpatient encounters throughout the initial year following the index admission were recorded. Additional procedures included delayed cholecystectomy, percutaneous or endoscopy-guided gallbladder drainage procedures, and ERCP performed to remove stones or sludge from the common bile duct. Readmission episodes attributed to acute cholecystitis complications, encompassing recurrence, cholangitis, liver abscesses, common bile duct stones, and biliary colic were analyzed. Throughout the one-year outpatient follow-up, both planned appointments and unplanned encounters were documented. The latter encompassed instances where patients presented with complaints or symptoms pertaining to acute cholecystitis.
EndpointsThe primary endpoints of the study were defined as follows: (a) additional procedures within the first year; (b) hospital readmissions within the first year attributable to biliary causes, and (c) outpatient encounters over the course of the first year, including both planned appointments and unscheduled visits.
Data collectionAnonymized data was collected and managed using REDCap tools (REDCap®, Research Electronic Data Capture, University of Vanderbilt, Nashville, Tennessee, US) hosted at Asociación Española de Gastroenterología (AEG; https://www.redcap.aegastro.es) (45).
Analysis of dataDescriptive statistics was used to analyze the demographic and baseline characteristics of the patients. Quantitative variables were presented as median and interquartile range (IQR), while categorical variables were expressed as absolute and relative frequencies. Group comparisons were performed using the Chi-square test or Fisher's exact test for categorical data, the T-test for parametric quantitative data, and the Mann–Whitney U test for quantitative non-parametric data. Although propensity score matching analysis has been used primarily for the comparison of two groups of subjects in observational studies, it has recently been considered for the analysis of more than two groups (46). However, due to the small number of subjects in this study, it was not possible to use it for more than two groups. Surgery was designated as the reference group for comparisons. Propensity score matching (1:1 optimal match) was performed using the MatchIt package for R software. The propensity score was determined via logistic regression, incorporating demographic and pre-procedure characteristics to mitigate the impact of selection bias, with a 0.1-caliper width employed. The procedure's impact was assessed by comparing outcomes (medians for continuous data, proportions for dichotomous data) following matching (47). Survival curves were generated utilizing the Kaplan–Meier method and subsequently compared using the log-rank test. P values of less than.05 were considered statistically significant. All analyses were performed using RStudio, version 1.2.5001 (Integrated Development for R. RStudio, Inc., Boston, MA, USA).
Results Baseline population characteristicsA cohort of 50 patients diagnosed with acute cholecystitis were included in the study. Among them, 21 patients were septuagenarians, while 29 were octogenarians or older. During the index admission, cholecystectomy was performed on nine patients (18%), while 19 patients (38%) received supportive care. Additionally, percutaneous gallbladder drainage was carried out in 22 patients (44%).
Patients who received supportive care exhibited higher ASA scores (ASA 1, 21.1%; ASA 2, 63.2%; ASA 3, 15.8%) compared to those who underwent cholecystectomy (ASA 1, 77.8%; ASA 2, 22.2%) (P = .02) (Table 1). Patients who underwent percutaneous gallbladder drainage exhibited higher Charlson Comorbidity Index scores (7.5 [4.3–9.8] vs. 5 [4–5], P = .04), poorer ECOG performance status (P = .04), and elevated ASA scores (ASA 1, 18.2%; ASA 2, 63.6%; ASA 3, 18.2%) when compared to patients who underwent cholecystectomy (P = .01) (Table 2).
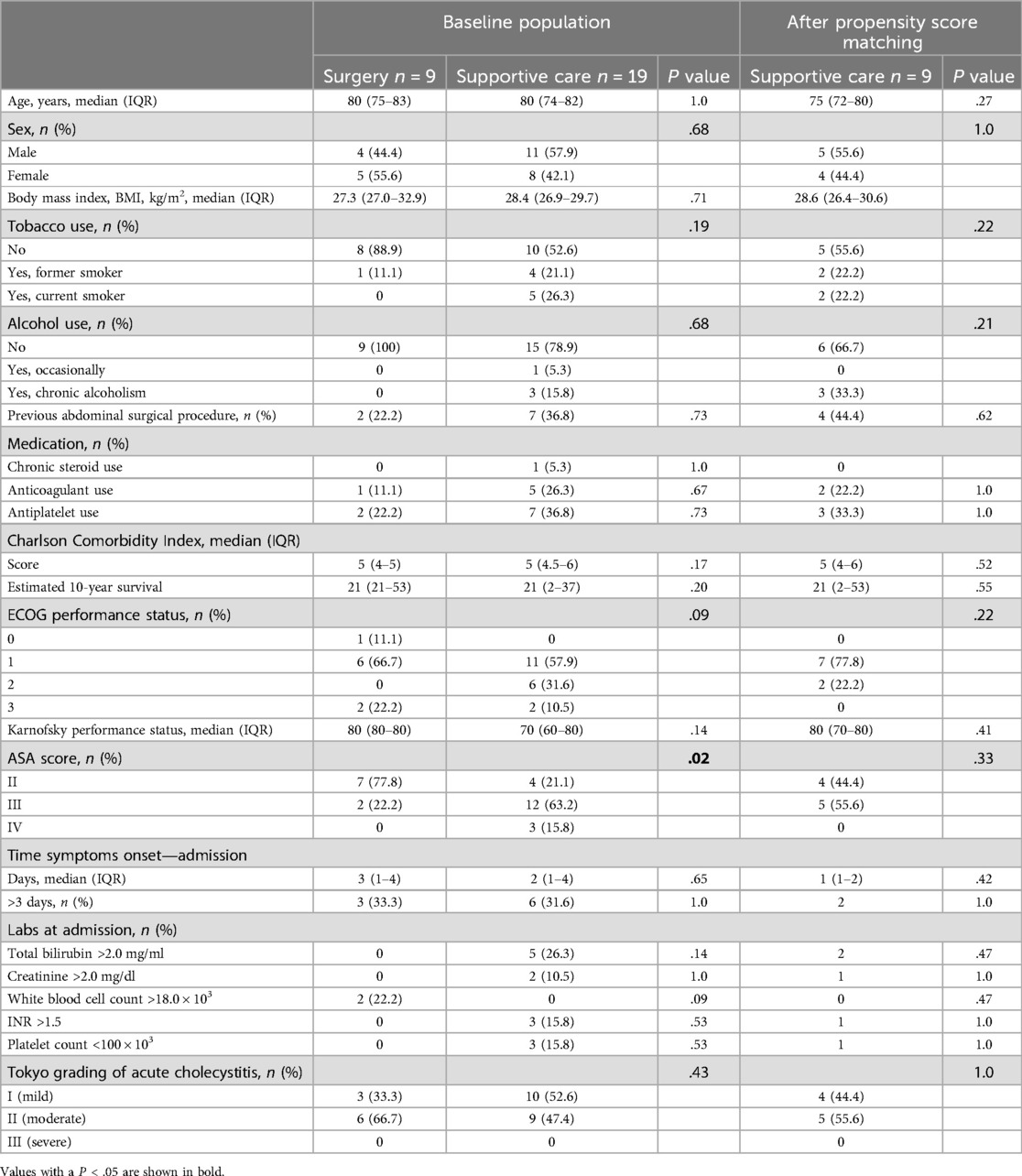
Table 1. Demographic and preoperative characteristics of septuagenarians and octogenarians undergoing surgery or supportive care for acute cholecystitis.
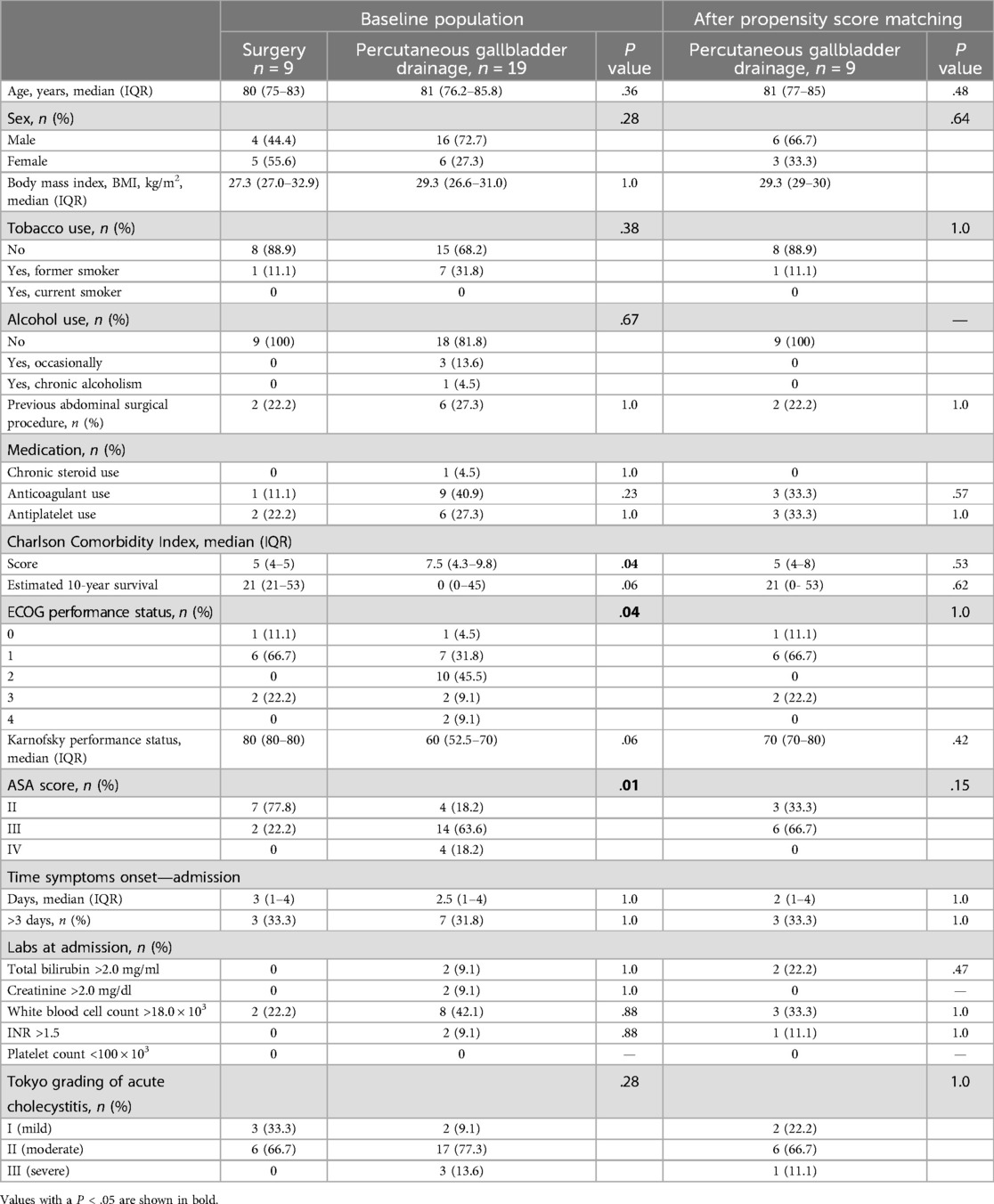
Table 2. Demographic and preoperative characteristics of septuagenarians and octogenarians undergoing surgery or percutaneous gallbladder drainage for acute cholecystitis.
Outcomes in the baseline populationA greater proportion of patients who received supportive care (47.4%) required additional procedures within one year compared to those who underwent cholecystectomy (0%) (P = .02) (Table 3, Figure 1). Furthermore, patients who received supportive care during their index admission required a higher number of additional procedures compared to those who underwent surgery (0 [0–1] vs. 0 [0–0], P = .02) (Table 3).
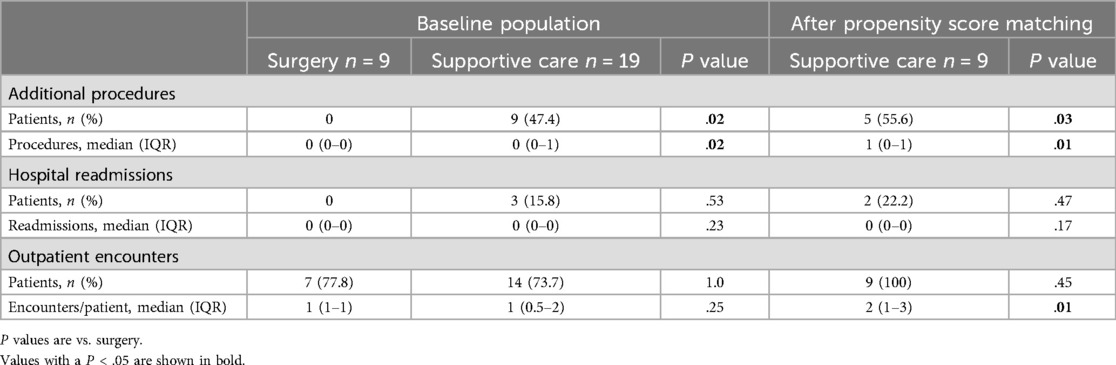
Table 3. One-year outcomes of septuagenarians and octogenarians with acute cholecystitis undergoing surgery or supportive care.
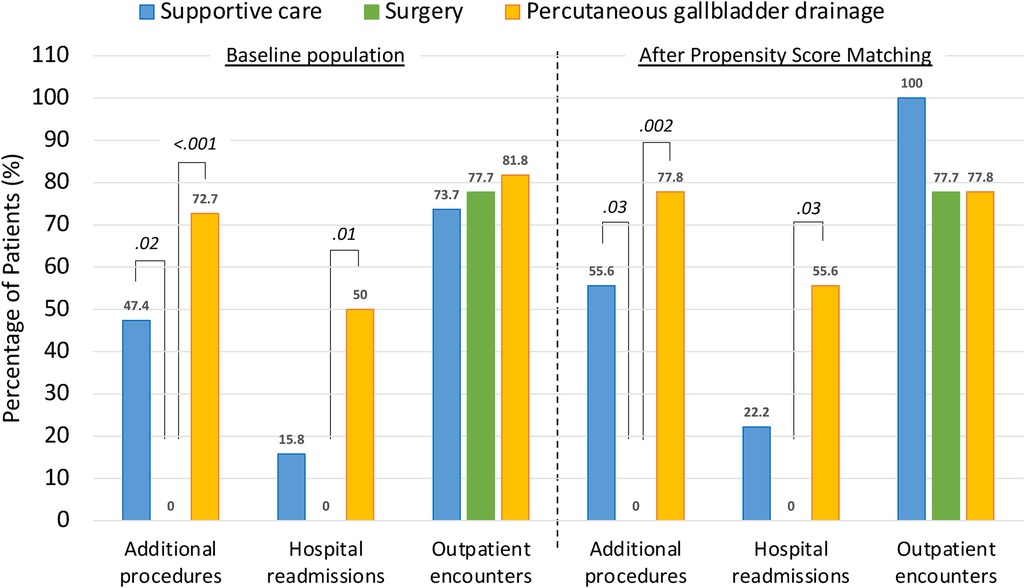
Figure 1. One-year outcomes of septuagenarians and octogenarians with acute cholecystitis undergoing either supportive care, surgery or percutaneous gallbladder drainage at index admission. Data labels indicate the percentage of patients who met a specific outcome after each index treatment modality, both in the baseline population (left panel) and after propensity score matching analysis (right panel). P-values (in Italic) were obtained considering surgery as reference.
Similarly, significantly more patients undergoing percutaneous gallbladder drainage required additional procedures within one year (72.7% vs. 0%, p < 0.001) and experienced 1-year readmissions (50% vs. 0%, p = .01) compared to surgery (Table 4, Figure 1). In addition, the number of additional procedures (1 [0.25–1.75] vs. 0 [0–0], P < .001) and readmissions (0.5 [0–1] vs. 0 [0–0], P = .01) was significantly higher in patients who had percutaneous gallbladder drainage compared to those who had surgery during the index admission (Table 4).
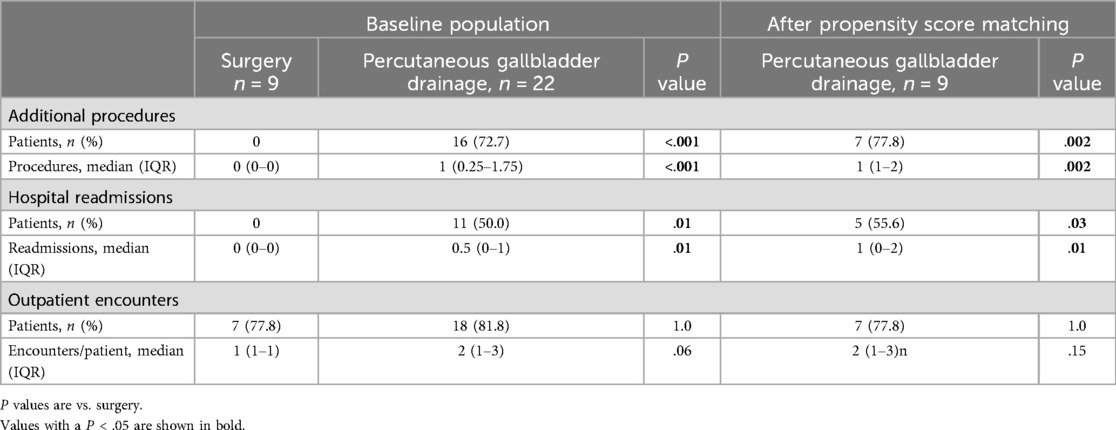
Table 4. One-year outcomes of septuagenarians and octogenarians undergoing surgery or percutaneous gallbladder drainage for acute cholecystitis.
Additional procedures performed and reasons for readmission by treatment modality are summarized in Supplementary Table 1. In the supportive care group, nine of the 19 patients required a total of 14 additional procedures. Of these, three patients required six readmissions, all due to recurrence of acute cholecystitis. In addition, a total of 26 additional procedures were required in 16 of the 22 patients who underwent percutaneous gallbladder drainage. Of these patients, 11 required 15 readmissions, primarily for recurrent acute cholecystitis.
One patient receiving supportive care and four patients undergoing percutaneous gallbladder drainage died during the follow-up period. Survival analysis was performed by index treatment modality within the baseline population. No survival differences were noted among the three index treatment modalities (Figure 2).
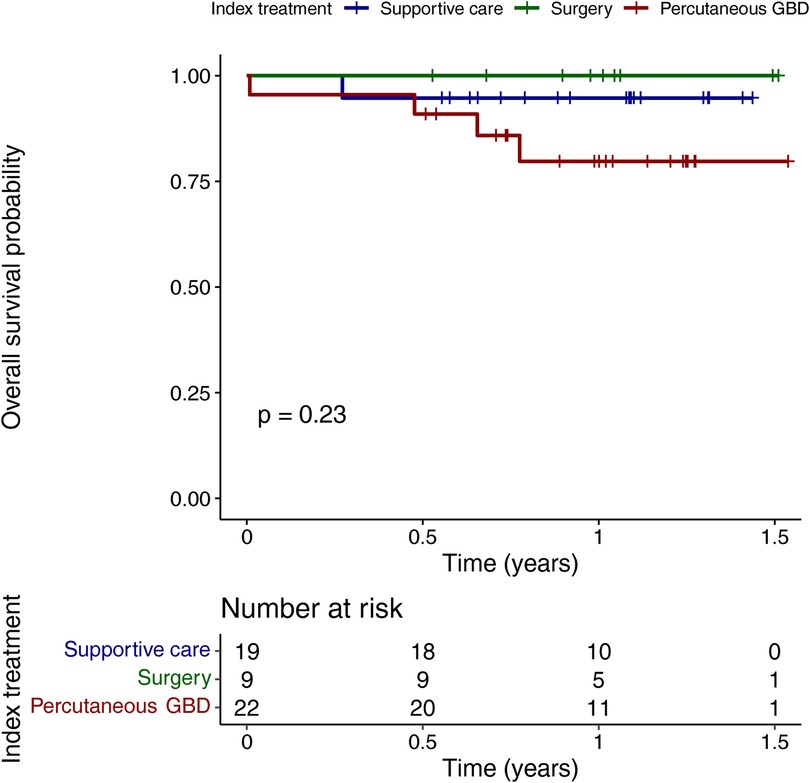
Figure 2. Overall survival of septuagenarians and octogenarians with acute cholecystitis by index treatment modality. GBD, gallbladder drainage.
Outcomes after propensity score matching analysisAfter propensity score matching, there were no demographic or preoperative differences between the groups (Tables 1, 2). A higher proportion of supportive care patients required additional procedures within one year compared to surgery patients (55.6% vs. 0%, P = .03) (Table 3, Figure 1). In addition, the median number of additional procedures (1 [0–1] vs. 0 [0–0], P = .01) and outpatient encounters (2 [1–3] vs. 1 [1–1], P = .01) was significantly higher in patients who received supportive care compared to those who underwent surgery (Table 3).
Similarly, patients undergoing percutaneous gallbladder drainage were significantly more likely to require additional procedures within one year (77.8% vs. 0%, P = .002) and to be readmitted within one year (55.6% vs. 0%, P = .03) than patients undergoing surgery (Table 4, Figure 1). In addition, median numbers of additional procedures (1 [1–2] vs. 0 [0–0], P = .002) and rehospitalizations (1 [0–2] vs. 0 [0–0], P = .01) were significantly higher in patients undergoing percutaneous gallbladder drainage than in those undergoing cholecystectomy (Table 4).
After propensity score matching, the specific types of additional procedures performed and reasons for 1-year readmission attributed to acute cholecystitis-related complications are shown in Supplementary Table 1. A total of seven additional procedures were required in five patients who received supportive care. Additionally, two patients required four readmissions, all related to recurring acute cholecystitis. Among those who underwent percutaneous gallbladder drainage during the index admission, seven patients required a total of 12 additional procedures, with five patients requiring 10 readmissions for recurrent acute cholecystitis and other reasons.
A laparoscopic approach was used in all patients who underwent cholecystectomy during the index admission. In contrast, two patients who had a delayed cholecystectomy after supportive care or percutaneous gallbladder drainage required an open approach or conversion to an open approach (Supplementary Table 2). No cases of common bile duct injury or need for reoperation were observed in either group.
DiscussionIn summary, no additional procedures or readmissions were required in septuagenarians and octogenarians who underwent cholecystectomy during the index admission. In contrast, subsequent procedures and readmissions occurred in patients who received supportive care or underwent percutaneous gallbladder drainage. Based on the present study data, nine patients receiving supportive care and another nine patients undergoing percutaneous gallbladder drainage may have benefited from cholecystectomy during the index admission. Using this strategy, 27 of the 50 septuagenarians and octogenarians (54% of the baseline population) would have been eligible for surgery during their initial hospital admission.
A 4.4% rate of additional 30-day procedures was observed in a comprehensive Danish registry of more than 4,000 patients treated for acute cholecystitis, primarily by laparoscopic cholecystectomy (48). The majority of these were ERCP. The remainder were related to various surgical complications. In the Danish cohort, advanced age emerged as a notable determinant of the increased risk of needing additional procedures within 30 days. In contrast, the present study sought to determine whether additional procedures occurred within the first year following treatment. Of note, none of our elderly patients who underwent cholecystectomy had a need for additional procedures during the subsequent year. In contrast, the results obtained after propensity score matching showed that more than half of our patients who received supportive care (55.6%) and about three quarters of our patients who underwent percutaneous gallbladder drainage (77.8%) required subsequent procedures.
Planned readmissions, which occurred for scheduled procedures such as delayed cholecystectomy, endoscopic therapies, or interventional radiology procedures, were excluded from the readmission count within the first year. Unplanned readmissions included episodes of recurrent acute cholecystitis, as well as cases of acute cholangitis, liver abscess, common bile duct stone, and surgical site infection. Only the unplanned readmissions within the first year were included. In the present study, 1-year readmission rates varied significantly by treatment modality. Specifically, the rates were 0%, 15.8%, and 50% for surgery, supportive care, and percutaneous gallbladder drainage, respectively. These findings are consistent with those of a 5-year randomized controlled trial of 142 high-risk patients (APACHE II score ≥7). The trial demonstrated a significantly higher incidence of 30-day major complications, surgical and radiological re-interventions, readmissions, and emergency department visits after percutaneous gallbladder drainage compared to laparoscopic cholecystectomy (49). On the other hand, a comprehensive analysis of Medicare claims data from 1996 to 2005 emphasized the importance of performing a cholecystectomy during the initial hospitalization of elderly patients with acute cholecystitis. This approach was advocated to reduce risk of recurrent cholecystitis, multiple readmissions, and associated costs (50). Of note, differences in study design, patient demographics, hospital environment, and lack of propensity score matching analysis may contribute to the observed differences in readmission rates across previous studies (Supplementary Table 3).
A 100% 1-year survival rate was observed among those who underwent surgery in our cohort of patients. No statistically significant differences were observed among those who opted for alternative therapeutic modalities, especially after percutaneous gallbladder drainage. This may be due to the relatively small sample size. A 1-year survival rate of 82.2% after percutaneous cholecystostomy was reported in a study of 73 patients with acute cholecystitis in China with a median age of 82 years (8). Similarly, in Spain, a study of 113 octogenarian patients showed a 1-year survival rate of 86% after both emergency and delayed (beyond 48 h after stabilization) cholecystectomy (14). The Medicare study found a 1-year survival rate of 85% after cholecystectomy. This compares to 80.6% without definitive therapy (50).
The results of these studies highlight the importance of refinement of selection criteria for older patients with acute cholecystitis to be considered for surgery during their index hospitalization. This may spare them unnecessary, costly, and risky procedures, reduce the probability of readmissions and outpatient visits, and significantly improve their overall quality of life. The goal of treatment is to improve the patient's quality of life with minimal physiologic stress, ideally allowing the patient to return to previous levels of performance. Lifestyle considerations are an increasingly important part of the decision-making process for medical interventions in the elderly. Percutaneous gallbladder drainage, especially if it requires frequent catheter changes, can significantly impact quality of life.
LimitationsThere are several limitations to our study. First, it included retrospective data from a single center with a relatively small patient cohort. Second, only four patients underwent EUS-guided gallbladder drainage during the study period. Therefore, they could not be included in the statistical analysis. Third, a notable gap in this study is the lack of data on patient-reported outcomes, particularly quality of life. Research has shown that acute cholecystitis in the elderly population can have a profound impact on their perception of quality of life. Therefore, this aspect is of particular importance (2, 8, 32, 35, 51–53). Finally, statistical comparisons between variables were limited by the heterogeneous data collection for cholecystectomies performed during index and delayed admissions. Despite this, all index cholecystectomies were performed laparoscopically, whereas some delayed cholecystectomies began as open procedures or were converted to open. Notably, intense fibrosis around the common bile duct or adjacent viscera was observed in more than half of the delayed cholecystectomies.
ConclusionThis study suggests that the decision to proceed with surgery during the index admission may result in superior one-year outcomes compared with supportive care or percutaneous gallbladder drainage in at least 50% of septuagenarians and octogenarians who are diagnosed with acute cholecystitis. Additional prospective data are needed to determine whether healthcare providers responsible for initial triage should identify older patients suitable for surgery during the index admission and prioritize this approach within acute care surgical protocols.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Research Ethics Committee of the Dr. Balmis Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because the study was retrospective in nature. Clinical decision-making was not influenced by the present study.
Author contributionsNL: Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing, Software, Supervision, Conceptualization, Data curation, Formal Analysis, Investigation, Methodology. CV: Conceptualization, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LG: Conceptualization, Investigation, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. ID: Conceptualization, Investigation, Writing – original draft, Writing – review & editing, Supervision, Validation, Visualization. PZ: Conceptualization, Formal Analysis, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing, Software, Visualization. BM: Conceptualization, Investigation, Supervision, Validation, Writing – original draft, Writing – review & editing, Visualization. JA: Conceptualization, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing, Visualization. FL: Conceptualization, Formal Analysis, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. Ed: Conceptualization, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Funding acquisition.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
AcknowledgmentsThe authors are indebted to Mercedes Alfaro and Mary Paz Sánchez, Department of Admission and Clinical Documentation, Hospital General Universitario Dr. Balmis, Alicante, for their help in collecting data for the present study.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2025.1500700/full#supplementary-material
References2. Li J, Jin X, Ren J, Li R, Du L, Gao Y, et al. Global burden of gallbladder and biliary diseases: a systematic analysis for the global burden of disease study 2019. J Gastroenterol Hepatol. (2022) 37(7):1389–99. doi: 10.1111/jgh.15859
PubMed Abstract | Crossref Full Text | Google Scholar
4. Loozen CS, Van Ramshorst B, Van Santvoort HC, Boerma D. Early cholecystectomy for acute cholecystitis in the elderly population: a systematic review and meta-analysis. Dig Surg. (2017) 34(5):371–9. doi: 10.1159/000455241
PubMed Abstract | Crossref Full Text | Google Scholar
5. Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, et al. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. (2018) 25(1):41–54. doi: 10.1002/jhbp.515
PubMed Abstract | Crossref Full Text | Google Scholar
6. Escartín A, González M, Cuello E, Pinillos A, Muriel P, Merichal M, et al. Acute cholecystitis in very elderly patients: disease management, outcomes, and risk factors for complications. Surg Res Pract. (2019) 2019:9709242. doi: 10.1155/2019/9709242
PubMed Abstract | Crossref Full Text | Google Scholar
7. Wiggins T, Markar SR, Mackenzie H, Jamel S, Askari A, Faiz O, et al. Evolution in the management of acute cholecystitis in the elderly: population-based cohort study. Surg Endosc. (2018) 32(10):4078–86. doi: 10.1007/s00464-018-6092-5
PubMed Abstract | Crossref Full Text | Google Scholar
8. Li M, Li N, Ji W, Quan Z, Wan X, Wu X, et al. Percutaneous cholecystostomy is a definitive treatment for acute cholecystitis in elderly high-risk patients. Am Surg. (2013) 79(5):524–7. doi: 10.1177/000313481307900529
PubMed Abstract | Crossref Full Text | Google Scholar
9. Hu YR, Pan JH, Tong XC, Li KQ, Chen SR, Huang Y. Efficacy and safety of B-mode ultrasound-guided percutaneous transhepatic gallbladder drainage combined with laparoscopic cholecystectomy for acute cholecystitis in elderly and high-risk patients. BMC Gastroenterol. (2015) 15(1):2–7. doi: 10.1186/s12876-015-0294-2
PubMed Abstract | Crossref Full Text | Google Scholar
10. Pan YL, Wu PS, Chen JH, Chen LY, Fang WL, Chau GY, et al. Early cholecystectomy following percutaneous transhepatic gallbladder drainage is effective for moderate to severe acute cholecystitis in the octogenarians. Arch Gerontol Geriatr. (2023) 106(Sept. 2022):104881. doi: 10.1016/j.archger.2022.104881
PubMed Abstract | Crossref Full Text | Google Scholar
11. Hernandez M, Murphy B, Aho JM, Haddad NN, Saleem H, Zeb M, et al. Validation of the AAST EGS acute cholecystitis grade and comparison with the Tokyo guidelines. Surgery (United States). (2018) 163(4):739–46. doi: 10.1016/j.surg.2017.10.041
PubMed Abstract | Crossref Full Text | Google Scholar
12. Costi R, DiMauro D, Mazzeo A, Boselli AS, Contini S, Violi V, et al. Routine laparoscopic cholecystectomy after endoscopic sphincterotomy for choledocholithiasis in octogenarians: is it worth the risk? Surg Endosc Other Interv Tech. (2007) 21(1):41–7. doi: 10.1007/s00464-006-0169-2
PubMed Abstract | Crossref Full Text | Google Scholar
13. D’Acapito F, Cucchetti A, Di Pietrantonio D, Tauceri F, Mirarchi MT, Framarini M, et al. Forecasting outcomes after cholecystectomy in octogenarian patients. Surg Endosc. (2022) 36(6):4479–85. doi: 10.1007/s00464-021-08801-7
Crossref Full Text | Google Scholar
14. De la Serna S, Ruano A, Pérez-Jiménez A, Rojo M, Avellana R, García-Botella A, et al. Safety and feasibility of cholecystectomy in octogenarians. Analysis of a single center series of 316 patients. HPB (Oxford). (2019) 21(11):1570–6. doi: 10.1016/j.hpb.2019.03.373
PubMed Abstract | Crossref Full Text | Google Scholar
16. Hazzan D, Geron N, Golijanin D, Reissman P, Shiloni E. Laparoscopic cholecystectomy in octogenarians. Surg Endosc Other Interv Tech. (2003) 17(5):773–6. doi: 10.1007/s00464-002-8529-z
PubMed Abstract | Crossref Full Text | Google Scholar
17. Kim SM, Shin MH, Choi NK. Safe and feasible outcomes of cholecystectomy in extremely elderly patients (octogenarians vs. nonagenarians). J Minim Invasive Surg. (2021) 24(3):139–44. doi: 10.7602/jmis.2021.24.3.139
PubMed Abstract | Crossref Full Text | Google Scholar
18. Leandros E, Alexakis N, Archontovasilis F, Albanopoulos K, Dardamanis D, Menenakos E, et al. Outcome analysis of laparoscopic cholecystectomy in patients aged 80 years and older with complicated gallstone disease. J Laparoendosc Adv Surg Tech. (2007) 17(6):731–5. doi: 10.1089/lap.2007.0018
PubMed Abstract | Crossref Full Text | Google Scholar
20. Nikfarjam M, Yeo D, Perini M, Fink MA, Muralidharan V, Starkey G, et al. Outcomes of cholecystectomy for treatment of acute cholecystitis in octogenarians. ANZ J Surg. (2014) 84(12):943–8. doi: 10.1111/ans.12313
PubMed Abstract | Crossref Full Text | Google Scholar
21. Oldani A, Calabrò M, Maroso F, Deiro G, Ravizzini L, Gentile V, et al. Early surgical management of acute cholecystitis in ultra-octogenarian patients: our 5-year experience. Minerva Chir. (2019) 74(6):203–6. doi: 10.23736/S0026-4733.18.07719-2
PubMed Abstract | Crossref Full Text | Google Scholar
22. Park Y, Hwang DW, Lee JH, Song KB, Jun E, Lee W, et al. Clinical outcomes of octogenarians according to preoperative disease severity and comorbidities after laparoscopic cholecystectomy for acute cholecystitis. J Hepatobiliary Pancreat Sci. (2020) 27(6):307–14. doi: 10.1002/jhbp.719
PubMed Abstract | Crossref Full Text | Google Scholar
23. Peker Y, Ünalp HR, Durak E, Karabuǧa T, Yilmaz Y, Genç H, et al. Laparoscopic cholecystectomy in patients aged 80 years and older: an analysis of 111 patients. Surg Laparosc Endosc Percutan Tech. (2014) 24(2):173–6. doi: 10.1097/SLE.0b013e31828f6be4
PubMed Abstract | Crossref Full Text | Google Scholar
24. Sánchez-Beorlegui J, Soriano P, Monsalve E, Moreno N, Cabezali R, Navarro A. Colecistectomía laparoscópica en pacientes octogenarios. Estudio comparativo entre dos poblaciones en edad geriátrica. Cir Esp. (2009) 85(4):246–51. doi: 10.1016/j.ciresp.2008.11.001
Crossref Full Text | Google Scholar
25. Uecker J, Adams M, Skipper K, Dunn E. Cholecystitis in the octogenarian: is laparoscopic cholecystectomy the best approach? Am Surg. (2001) 67(7):637–40. doi: 10.1177/000313480106700709
PubMed Abstract | Crossref Full Text | Google Scholar
26. Vaccari S, Lauro A, Cervellera M, Palazzini G, Casella G, Santoro A, et al. Cholecystectomy for acute cholecystitis in octogenarians: impact of advanced age on postoperative outcome. Minerva Chir. (2019) 74(4):289–96. doi: 10.23736/S0026-4733.19.07891-X
PubMed Abstract | Crossref Full Text | Google Scholar
28. Ahmed O, Ogura T, Eldahrouty A, Khalaf H, Mohammed E, Okasha H, et al. Endoscopic ultrasound-guided gallbladder drainage: results of long-term follow-up. Saudi J Gastroenterol. (2018) 24(3):183–8. doi: 10.4103/sjg.SJG_506_17
PubMed Abstract | Crossref Full Text | Google Scholar
29. Irani S, Ngamruengphong S, Teoh A, Will U, Nieto J, Abu Dayyeh BK, et al. Similar efficacies of endoscopic ultrasound gallbladder drainage with a lumen-apposing metal stent versus percutaneous transhepatic gallbladder drainage for acute cholecystitis. Clin Gastroenterol Hepatol. (2017) 15(5):738–45. doi: 10.1016/j.cgh.2016.12.021
PubMed Abstract | Crossref Full Text | Google Scholar
30. Jang JW, Lee SS, Song TJ, Hyun YS, Park DH, Seo DW, et al. Endoscopic ultrasound-guided transmural and percutaneous transhepatic gallbladder drainage are comparable for acute cholecystitis. Gastroenterology. (2012) 142(4):805–11. doi: 10.1053/j.gastro.2011.12.051
PubMed Abstract | Crossref Full Text | Google Scholar
31. Kanno Y, Kozakai F, Koshita S, Ogawa T, Kusunose H, Masu K, et al. Technical issues stemming from endoscopic-ultrasound-guided gallbladder drainage: a single center experience. Turk J Gastroenterol. (2019) 30(12):1055–61. doi: 10.5152/tjg.2019.181032
PubMed Abstract | Crossref Full Text | Google Scholar
32. Law R, Grimm IS, Stavas JM, Baron TH. Conversion of percutaneous cholecystostomy to internal transmural gallbladder drainage using an endoscopic ultrasound-guided, lumen-apposing metal stent. Clin Gastroenterol Hepatol. (2016) 14(3):476–80. doi: 10.1016/j.cgh.2015.10.026
PubMed Abstract | Crossref Full Text | Google Scholar
33. Magahis PT, Westerveld D, Simons M, Mahadev SH. A surprising culprit for delayed gastrointestinal bleeding after endoscopic ultrasound-guided cholecystoduodenostomy: the double-pigtail stent. Clin J Gastroenterol. (2022) 16(2):279–82. doi: 10.1007/s12328-022-01749-8
留言 (0)