Pregnancy loss (PL) is defined as the spontaneous termination of a pregnancy before fetal viability (1). PL can cause significant harm to women, including adverse psychological and physiological effects. It has been reported that approximately 8% to 20% of recognizable natural pregnancies end in PL (2, 3).
PL has been shown to be associated with an increased risk of various physiological and psychological disorders. Studies suggest that PL is linked to subsequent mental health disorders such as depression, anxiety, and others (4). Furthermore, mothers who experience PL often receive little social attention, further complicating their situation. Additionally, studies suggest a close association between PL and the development of type 2 diabetes (5), cardiovascular diseases (6), and even malignant tumors (7), although the evidence is not yet conclusive. Hence, there is a strong desire among both patients and healthcare providers for a method to predict and prevent PL.
Researches have investigated the factors that impact the rate of PL. Many studies have explored the factors contributing to PL, including maternal age, obesity, embryonic factors, hormone levels during ovarian stimulation, but have not reached consistent conclusions. In recent years, some studies have started to explore the mechanisms underlying PL at deeper levels, such as genes (8, 9), cytokines (10), miRNA (11), and so on. This also provides a broader perspective for more effective research on the mechanisms of PL.
The etiology of early miscarriage is commonly attributed to chromosomal abnormalities, while the reasons for PL following transfer of euploid blastocysts remain unclear. The aim of this study is to investigate the factors influencing the rate of PL after ART treatment in order to better understand its mechanisms. In this study, we aimed to establish an image based on multiple risk factors to effectively predict the probability of patients experiencing PL, thus offering robust evidence for clinical consultation.
Materials and methodsStudy designThis study was a single-center retrospective cohort study. It was conducted in the Assisted Reproduction Center, Northwest Women’s and Children’s Hospital in Xi ‘an, Shaanxi Province, China and was approved by the ethics committee of the Northwest Women’s and Children’s Hospital (number 2023003). Patients who underwent frozen-thawed embryo transfer (FET) after PGT-A between2017 and 2022 were included. The data were extracted from the electronic medical record system (Wuhan Huchuang, Co., Ltd.; version 9.2.5.8).
PatientsThe study enrolled patients who met the following criteria: (1) The initial cycle of thawing and transferring an euploid embryo following PGT-A; (2) Women under 38 years old. The following cycles were excluded: (1) Patients suffering from uterine infertility caused by conditions such as intrauterine adhesions, endometrial polyps, uterine fibroids, and congenital uterine malformations; (2)Patients with hypertension, diabetes, and systemic autoimmune diseases; (3) Women with ectopic pregnancies, molar pregnancies, continuing pregnancies, and induced abortions.
From 2017 to 2022, according to the inclusion and exclusion criteria, a total of 352 patients were enrolled. Among them, 278 cases resulted in clinical pregnancies. After excluding 8 cases with incomplete clinical data information, a total of 270 patients were included in the study. Ultimately, 234 cases resulted in live births, while 36 cases experienced PL. Patients were divided into the live birth group and the PL group.
IVF ProceduresFor ovarian stimulation, patients receive recombinant and/or urinary gonadotropin therapy in a long protocol with gonadotropin-releasing hormone (GnRH) agonist or GnRH antagonist. In this study, the patients underwent intracytoplasmic sperm injection (ICSI) for fertilization. The embryos were cultured in the 40 μL G1(Vitrolife, Sweden) medium. The embryos were assessed on the third day following the methodology described in our previous study. If the criteria were met, extended culture would be performed to the blastocyst stage. On the 5th and 6th day, according to the Gardner criteria (12), embryos would be graded. Embryos with an expansion grade of 4 or higher, and inner cell mass and trophectoderm grade of C or higher, would undergo biopsy and be cryopreserved by vitrification. The vitrification was performed according to the standard procedure using the Cryotop, an open system (Kitazato BioPharmaCo, Japan).
Blastocyst morphologyBlastocyst morphological analysis was conducted on the 5th day and 6th day following ICSI fertilization. The content of this article only included the expanded blastocysts, encompassing stages 4, 5, and 6. The evaluation of the inner cell mass (ICM) and trophectoderm (TE) was mainly determined by the cell count and the level of compactness in their organization. The tight packing of numerous cells of ICM/TE was identified as “A”. The clustering of several cells together was identified as” B”. Loose arrangement of a few cells was identified as” C”. In this study, top-quality grade blastocysts referred to those with a grade of BB and above, including AB, BA, BB, and AA. The remaining blastocysts were considered lower quality, including BC, CB, AC, CA, and CC grades.
FET protocolsThe endometrial preparation was performed using the natural cycle or the hormonal treatment cycle. During a natural menstrual cycle, follicles and hormone levels were monitored to identify the timing of spontaneous ovulation or to induce ovulation using a 1000IU hCG injection. The blastocyst transfer procedure was scheduled for day 6 post-ovulation. In the hormonal cycle, oral E2 valerate (Progynova; Bayer Schering Pharma AG) with a dose of 6mg/day was administered from the 5th day of menstrual cycle. Once the endometrial thickness reaches 7-8mm as detected by ultrasound monitoring, the administration of 60mg of progesterone daily for luteal support should commence until a negative hCG levels was obtained or until the 8th week of pregnancy. The blastocyst transfer is typically scheduled on the 7th day of progesterone initiation.
Outcome measurementThe collected data were analyzed according to the following sections: 1.The population information of two cohorts were analyzed, comprising the age, BMI, and infertility status of the female subjects. 2. Compared the ovarian stimulation variables between two groups of patients during the fresh cycle, such as hormone concentrations on trigger day, initial and total amount of gonadotropin (Gn), etc. 3. Analyzed the impact of various factors on PL.
Clinical pregnancy is defined as the presence of a gestational sac on early ultrasound examination, with or without fetal heart activity. Live birth was characterized by the birth of a viable infant after 28 weeks of gestation post embryo transfer. PL refers to the clinical pregnancy that ultimately did not result in a live birth.
Statistical analysisAll data analysis was conducted using the Statistical Package for the Social Sciences (SPSS) software, version 26. Continuous variables were expressed as the mean ± standard deviation and a normality test was conducted. Variables conforming to a normal distribution are evaluated using the Student’s t-test, whereas variables deviating from a normal distribution are assessed using the Mann-Whitney U test. Categorical variables were depicted as counts and proportions, and the chi-square test was employed to assess the differences. A multivariate logistic regression was conducted to evaluate the risk factors that affecting PL. The results were presented as odds ratios (ORs) and 95% confidence intervals (CIs). A P-value of less than 0.05 indicated a statistically significant difference.
ResultsWe compared of population characteristics between the live birth group and the PL group (Table 1). Our analysis revealed no statistically significant differences in maternal age, paternal age, paternal BMI, infertility duration, antral follicle count, dose of gonadotrophins and basic hormone (E2, FSH, LH) levels between the two groups. A statistically significant difference in maternal BMI was observed between the two groups (P=0.016). When comparing manipulations in the fresh cycle, differences were found in E2, LH on the HCG trigger day (P=0.007, P=0.023) and the number of oocytes retrieved (P=0.044) between the two groups.
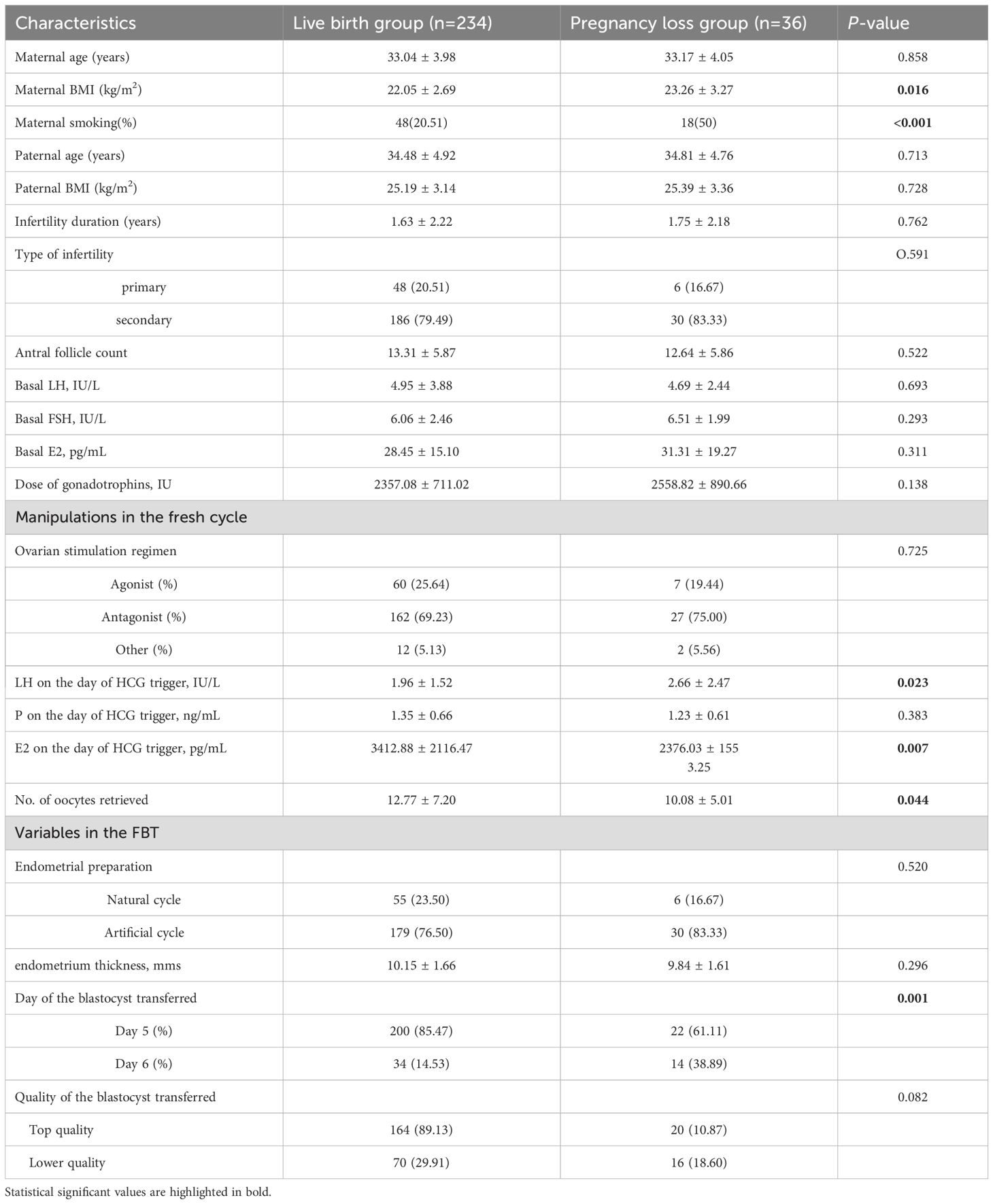
Table 1. Population characteristics of the live birth group and the pregnancy loss group.
As for the variables in the FBT, there existed a statistically significant disparity in the day of blastocyst transfer between the two cohorts, with a notably reduced incidence of PL observed on day5 blastocyst transfer (9.91% vs 29.17, P=0.001). No significant differences were observed in the endometrial preparation protocols, endometrium thickness and quality of the blastocyst transferred examined in our study.
In response to practical requirements in real-world applications, we conducted an analysis on the combined impact of blastocyst quality and day of transfer on PL. As shown in Table 2, we observed differences in the probability of PL among the four groups (day 5top, day 5lower, day 6top, day 6lower) when we divided the enrolled patients into these groups (P=0.003). The corresponding PL rates for the four groups were 10.06%, 9.43%, 20.00%, and 33.33%, as shown in Figure 1. The results of logistic regression indicate that compared to day 6lower embryos, the day 5top and day 5lower groups may potentially reduce the occurrence rate of PL. The results of logistic regression indicate that compared to day 6lower embryos, the day 5top and day 5lower groups may potentially reduce the occurrence rate of PL (day 5top: OR=0.224, 95%CI=0.093-0.539, P=0.001; day 5lower: OR=0.208, 95%CI=0.065-0.672, P=0.009) (Table 3).
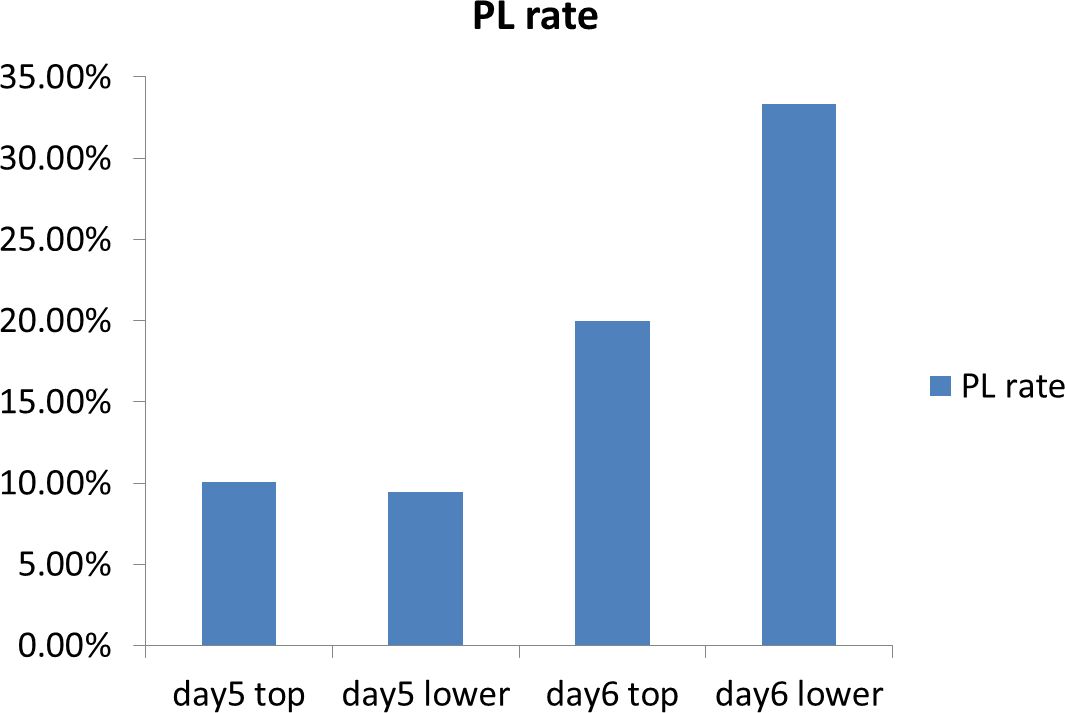
Figure 1. Pregnancy loss (PL) rate stratified by blastocyst day and quality.
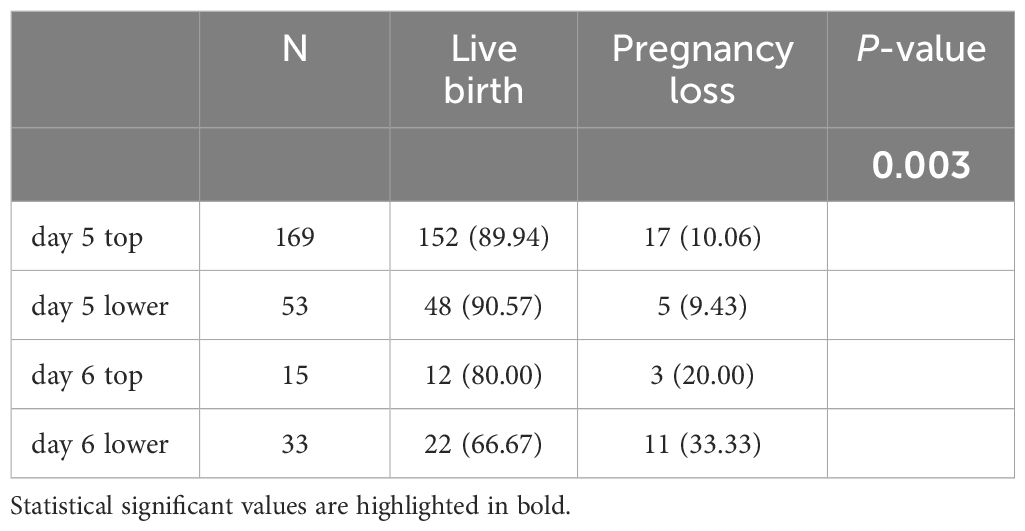
Table 2. Comparison of the day and score amongst the live birth group and the pregnancy loss group.
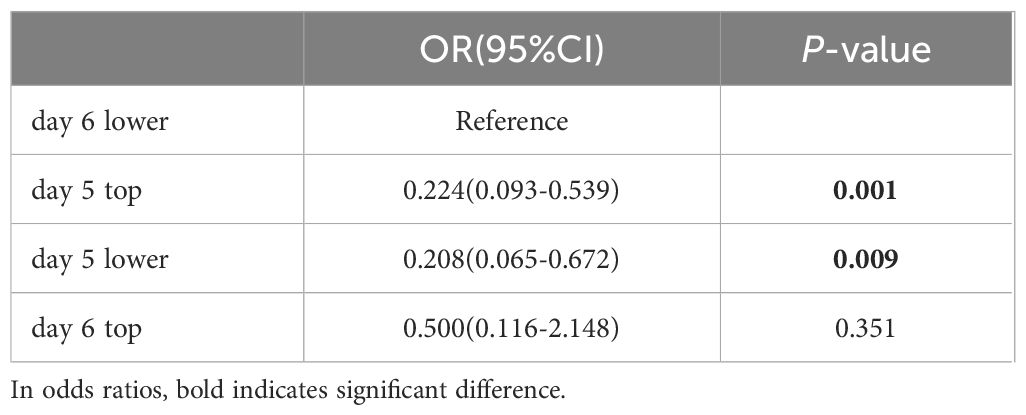
Table 3. Logistic regression model of blastocyst day and score with regard to risk of pregnancy loss.
A logistic regression analysis was conducted based on Table 1 to explore various factors associated with PL. The results were presented in Table 4. We could see that a lower E2 and higher LH levels on the trigger day of the fresh cycle corresponding to the blastocysts transferred appeared to be associated with an increased risk of PL (LH: OR=1.304, 95%CI=1.054-1.613, P=0.015; E2: OR=0.438, 95%CI=0.242-0.794, P=0.007). Simultaneously, transferring a day 6 blastocyst (OR=4.610, 95%CI=1.907-11.141, P=0.001) and maternal smoking (OR=4.574, 95%CI=1.974-10.601, P<0.001) also had been shown to increase the risk of PL.
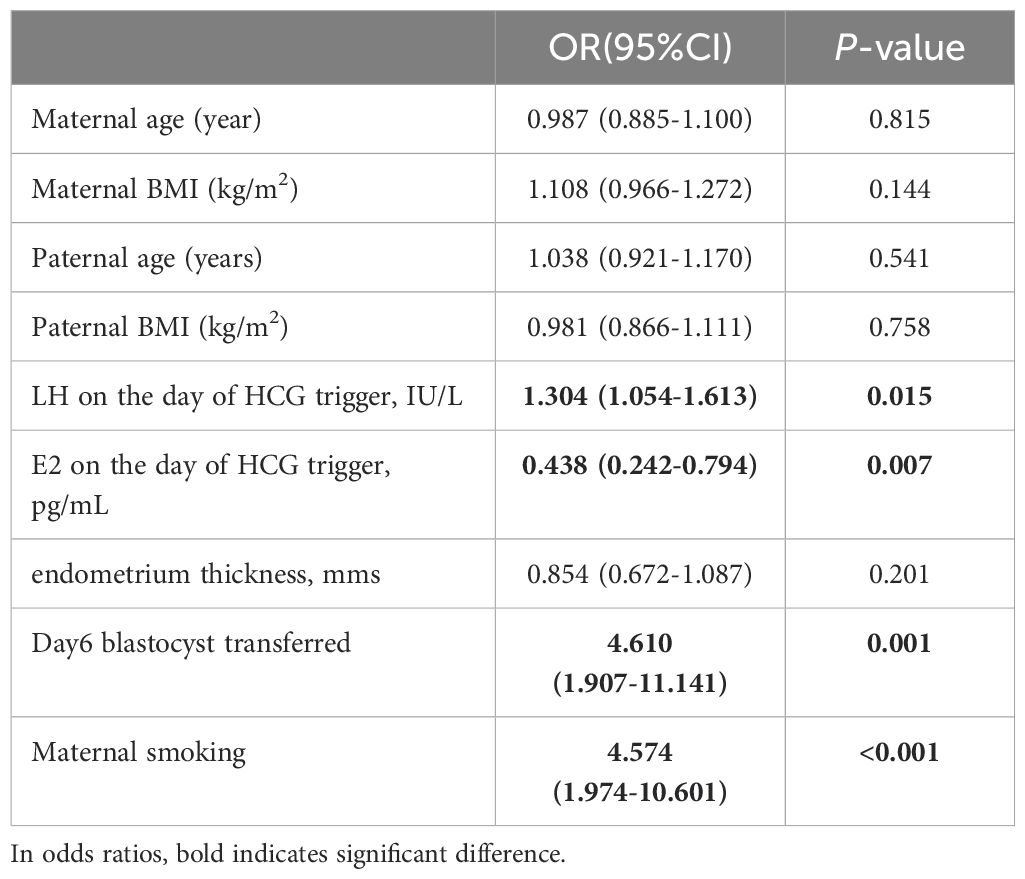
Table 4. Logistic regression model of PL after transfer of euploid blastocyst.
DiscussionBased on the findings of this study, higher levels of LH and lower levels of E2 on the trigger day of the fresh cycle, day 6 blastocyst transfer and maternal smoking appeared to elevate the risk of PL in cycles involving the transfer of euploid blastocysts.
The documented incidence of PL in natural conceptions varies from 8% to 20% (2, 3, 13). It is estimated that approximately 30% of pregnancies result in miscarriage, with some cases potentially going undetected (13, 14). Because of the unique characteristics of the ART population, this proportion is expected to be higher. Cai et al (15) showed that among the population undergoing IVF, the PL rate for patients with PCOS was 23%, compared to 21.9% for non-PCOS patients. Therefore, we speculate that there may be certain factors during the IVF process that could increase the risk of PL. Chromosome imbalance, also known as aneuploidy, is the primary factor leading to PL in humans (16). In this study, patients underwent transferring with euploid embryos, allowing for a more precise examination of the impact of factors other than the embryos on PL.
Numerous studies have been conducted to investigate potential factors contributing to PL. Reports indicated a strong correlation between maternal age and the incidence of PL, including both early and late miscarriages (17, 18). Our study did not observe a significant alteration in the rate of PL as maternal age increased. This was easy to understand, which means that age alone may not be the determining factor for PL when all transferred embryos were euploid. A study conducted by Spandorfer et al. (19) revealed that among PLes in women over 40 years old, 82% were attributed to chromosomal abnormalities in the fetus, compared to 65% in younger women. This also aligns with the perspective that aneuploidy serves as the predominant factor leading to PL in women of advanced age (20).
With regard to gamete or embryo manipulation, prior investigation indicated that the type of ovarian stimulation protocols used and human chorionic gonadotropin (HCG) levels on the 14th day are associated with PL (21). Our research results suggest that there is no correlation between ovarian stimulation protocols and HCG levels on the 14th day post-transfer with PL. Nevertheless, lower levels of E2 and higher levels of LH on the trigger day could potentially heighten the likelihood of PL.
The impact of LH levels post controlled ovarian stimulation (COS) on assisted reproductive technology (ART) outcomes remains a topic of debate. Benmachiche et al. (22) discovered that higher levels of LH were associated with increased live-birth rate and reduced PL rate. Similarly, according to Westergaard et al. (23), a LH concentration <0.5 on the 8th day of COS significantly reduces the success LBR and increases the risk of early miscarriage. However, some study (24) have indicated that the levels of LH on trigger day do not have an impact on live birth rates (LBR) and miscarriage rates. LH plays a crucial role in the development of ovarian follicles. Could elevated levels of LH potentially have a detrimental effect on oocyte quality, consequently raising the likelihood of PL? This warrants further investigation.
E2, as the most potent estrogen, is synthesized by ovarian granulosa cells using androstenedione and testosterone as precursors (25). In COS, the level of E2 on the trigger day can reflect the quantity of retrieved oocytes. In our study, we found a significant correlation between lower levels of E2 and PL. The dose of Gn in the PL (PL) group was comparable to that in the live birth group, and in some cases even higher in the PL group (although not statistically different). However, the PL group had a lower number of retrieved oocytes and lower E2 levels, reflecting a poorer response to ovarian stimulation in patients in the PL group. This may indicate the responsiveness of the patient’s ovaries to stimulant drugs, which may predict the probability of subsequent PL.
The incidence of aneuploidy increases with prolonged blastulation duration [16], leading to an elevated rate of miscarriages (26). It has been shown that the miscarriage rate of day 6 blastocysts is higher than that of day 5 blastocysts transferred (27). When the transferred blastocysts were all euploid, the results were also inconsistent. In our study, the miscarriage rate of blastocysts on day 6 was significantly higher (29.17% vs 9.91%). After including various confounding factors such as material/paternal age, BMI, pre-transfer endometrial thickness, maternal smoking, and number of miscarriages in a binary logistic regression analysis, this difference still exists. This is consistent with the majority of previous research findings (28). nevertheless, a study Abdala et al. (29) demonstrated comparing clinical outcomes of euploid blastocysts of day5 and day6 transferred found no difference in miscarriage rates. The discrepancy may stem from variations in the criteria employed by different centers for the inclusion of biopsiable blastocysts.
We also found that maternal smoking can significantly increase the incidence of PL. A study based on genetic data conducted by Yuan et al. (30) indicated a potential causal relationship between maternal smoking and miscarriage. In our study, after controlling for embryo-specific factors, maternal smoking as an independent factor significantly increased the rate of PL. Consistent with our research, a well-established negative correlation between maternal smoking and miscarriage has been identified (31–33). Therefore, it is essential to implement preconception counseling and public health initiatives targeting women of reproductive age to discourage smoking, particularly during pregnancy.
The main limitation of this study is attributed to the small sample size of euploidy blastocyst transfers, leading to inadequate statistical power to discern any disparities in the live birth and the PL group. Due to the limitation of sample size, we did not stratify the analysis based on the quality of the blastocysts for further investigation. This limitation should be addressed in future studies.
In conclusion, after the transfer of euploid blastocysts, there are still factors such as higher levels of LH and lower levels of E2 on the trigger day, day6 blastocyst transfer and smoke independently contribute to PL.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by the ethics committee of the Northwest Women’s and Children’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributionsXD: Formal Analysis, Software, Writing – original draft, Writing – review & editing. JS: Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – review & editing. XL: Data curation, Investigation, Project administration, Software, Writing – review & editing. DL: Data curation, Methodology, Software, Writing – review & editing. WL: Data curation, Formal Analysis, Software, Writing – review & editing. XZ: Methodology, Software, Writing – review & editing. XX: Conceptualization, Project administration, Resources, Supervision, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Shaanxi Provincial Health and Reproductive Medicine Research and Innovation Team (2023TD-04), Shaanxi Provincial Key Industry Chain Project - Research on Assisted Reproductive New Technologies and development of a Precision Prevention System for Pre-pregnancy Genetic Diseases (2023-ZDLSF-48).
AcknowledgmentsThe authors would like to express their gratitude to the patients who generously provided their medical data for this study. Additionally, they wish to thank all colleagues who supported the research work.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Bender Atik R, Christiansen OB, Elson J, Kolte AM, Lewis S, Middeldorp S, et al. Eshre guideline: recurrent pregnancy loss. Hum Reprod Open. (2018) 2018:hoy004. doi: 10.1093/hropen/hoy004
PubMed Abstract | Crossref Full Text | Google Scholar
3. Linnakaari R, Helle N, Mentula M, Bloigu A, Gissler M, Heikinheimo O, et al. Trends in the incidence, rate and treatment of miscarriage-nationwide register-study in Finland, 1998-2016. Hum Reprod. (2019) 34:2120–8. doi: 10.1093/humrep/dez211
PubMed Abstract | Crossref Full Text | Google Scholar
4. Delgado L, Cobo J, Giménez C, Fucho-Rius GF, Sammut S, Martí L, et al. Initial impact of perinatal loss on mothers and their partners. Int J Environ Res Public Health. (2023) 20:1304. doi: 10.3390/ijerph20021304
PubMed Abstract | Crossref Full Text | Google Scholar
5. Egerup P, Mikkelsen AP, Kolte AM, Westergaard D, Rasmussen S, Knop FK, et al. Pregnancy loss is associated with type 2 diabetes: A nationwide case-control study. Diabetologia. (2020) 63:1521–9. doi: 10.1007/s00125-020-05154-z
PubMed Abstract | Crossref Full Text | Google Scholar
6. Peters SAE, Yang L, Guo Y, Chen Y, Bian Z, Tian X, et al. Pregnancy, pregnancy loss, and the risk of cardiovascular disease in chinese women: findings from the China kadoorie biobank. BMC Med. (2017) 15:148. doi: 10.1186/s12916-017-0912-7
PubMed Abstract | Crossref Full Text | Google Scholar
7. Mikkelsen AP, Egerup P, Ebert JFM, Kolte AM, Nielsen HS, Lidegaard Ø. Pregnancy loss and cancer risk: A nationwide observational study. EClinicalMedicine. (2019) 15:80–8. doi: 10.1016/j.eclinm.2019.08.017
PubMed Abstract | Crossref Full Text | Google Scholar
8. Hromadnikova I, Kotlabova K, Krofta L. First-trimester screening for miscarriage or stillbirth-prediction model based on microrna biomarkers. Int J Mol Sci. (2023) 24:10137. doi: 10.3390/ijms241210137
PubMed Abstract | Crossref Full Text | Google Scholar
9. Maksiutenko EM, Barbitoff YA, Nasykhova YA, Pachuliia OV, Lazareva TE, Bespalova ON, et al. The landscape of point mutations in human protein coding genes leading to pregnancy loss. Int J Mol Sci. (2023) 24:17572. doi: 10.3390/ijms242417572
PubMed Abstract | Crossref Full Text | Google Scholar
10. Spathakis M, Filidou E, Pappa C, Arzou BC, Georgiadis A, Kontomanolis EN, et al. Spontaneous abortion is associated with differentially expressed angiogenic chemokines in placenta and decidua. Arch Gynecol Obstet. (2023) 308:821–30. doi: 10.1007/s00404-022-06725-8
PubMed Abstract | Crossref Full Text | Google Scholar
11. Galaziou A, Filidou E, Spathakis M, Arvanitidis K, Arzou BC, Galazios G, et al. Imbalance of growth factors mrna expression associated with oxidative stress in the early pregnancy loss. J maternal-fetal neonatal Med. (2022) 35:6150–6. doi: 10.1080/14767058.2021.1907337
PubMed Abstract | Crossref Full Text | Google Scholar
12. Gardner DK, Lane M, Stevens J, Schlenker T, Schoolcraft WB. Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertil Steril. (2000) 73:1155–8. doi: 10.1016/s0015-0282(00)00518-5
PubMed Abstract | Crossref Full Text | Google Scholar
13. Wang X, Chen C, Wang L, Chen D, Guang W, French J. Conception, early pregnancy loss, and time to clinical pregnancy: A population-based prospective study. Fertil Steril. (2003) 79:577–84. doi: 10.1016/s0015-0282(02)04694-0
PubMed Abstract | Crossref Full Text | Google Scholar
14. Griebel CP, Halvorsen J, Golemon TB, Day AA. Management of spontaneous abortion. Am Family physician. (2005) 72:1243–50.
15. Cai H, Mol BW, Gordts S, Wang H, Wang T, Li N, et al. Early and late pregnancy loss in women with polycystic ovary syndrome undergoing ivf/icsi treatment: A retrospective cohort analysis of 21 820 pregnancies. BJOG: an Int J obstetrics gynecology. (2021) 128:1160–9. doi: 10.1111/1471-0528.16590
PubMed Abstract | Crossref Full Text | Google Scholar
16. Gruhn JR, Zielinska AP, Shukla V, Blanshard R, Capalbo A, Cimadomo D, et al. Chromosome errors in human eggs shape natural fertility over reproductive life span. Sci (New York NY). (2019) 365:1466–9. doi: 10.1126/science.aav7321
PubMed Abstract | Crossref Full Text | Google Scholar
17. Lidegaard Ø, Mikkelsen AP, Egerup P, Kolte AM, Rasmussen SC, Nielsen HS. Pregnancy loss: A 40-year nationwide assessment. Acta Obstet Gynecol Scand. (2020) 99:1492–6. doi: 10.1111/aogs.13860
PubMed Abstract | Crossref Full Text | Google Scholar
18. Bu Z, Hu L, Su Y, Guo Y, Zhai J, Sun YP. Factors related to early spontaneous miscarriage during ivf/icsi treatment: an analysis of 21,485 clinical pregnancies. Reprod BioMed Online. (2020) 40:201–6. doi: 10.1016/j.rbmo.2019.11.001
PubMed Abstract | Crossref Full Text | Google Scholar
19. Spandorfer SD, Davis OK, Barmat LI, Chung PH, Rosenwaks Z. Relationship between maternal age and aneuploidy in in vitro fertilization pregnancy loss. Fertil Steril. (2004) 81:1265–9. doi: 10.1016/j.fertnstert.2003.09.057
PubMed Abstract | Crossref Full Text | Google Scholar
20. Verdyck P, Altarescu G, Santos-Ribeiro S, Vrettou C, Koehler U, Griesinger G, et al. Aneuploidy in oocytes from women of advanced maternal age: analysis of the causal meiotic errors and impact on embryo development. Hum Reprod. (2023) 38:2526–35. doi: 10.1093/humrep/dead201
PubMed Abstract | Crossref Full Text | Google Scholar
21. Hu L, Du J, Lv H, Zhao J, Chen M, Wang Y, et al. Influencing factors of pregnancy loss and survival probability of clinical pregnancies conceived through assisted reproductive technology. Reprod Biol Endocrinol. (2018) 16:74. doi: 10.1186/s12958-018-0390-6
PubMed Abstract | Crossref Full Text | Google Scholar
22. Benmachiche A, Benbouhedja S, Zoghmar A, Humaidan P. Low lh level on the day of gnrh agonist trigger is associated with reduced ongoing pregnancy and live birth rates and increased early miscarriage rates following ivf/icsi treatment and fresh embryo transfer. Front Endocrinol (Lausanne). (2019) 10:639. doi: 10.3389/fendo.2019.00639
PubMed Abstract | Crossref Full Text | Google Scholar
23. Westergaard LG, Laursen SB, Andersen CY. Increased risk of early pregnancy loss by profound suppression of luteinizing hormone during ovarian stimulation in normogonadotrophic women undergoing assisted reproduction. Hum Reprod. (2000) 15:1003–8. doi: 10.1093/humrep/15.5.1003
PubMed Abstract | Crossref Full Text | Google Scholar
24. Luo X, Li L, Lin N, Ma R, Li Y, Wu Z. Low endogenous lh on the cos initiation day of a gnrh-agonist regimen increases the risk of early pregnancy loss and adverse art outcomes. Front Endocrinol (Lausanne). (2022) 13:830567. doi: 10.3389/fendo.2022.830567
PubMed Abstract | Crossref Full Text | Google Scholar
25. Wu CH, Kuo TC, Wu HH, Yeh GP, Tsai HD. High serum estradiol levels are not detrimental to in vitro fertilization outcome. Taiwan J Obstet Gynecol. (2007) 46:54–9. doi: 10.1016/s1028-4559(08)60108-4
PubMed Abstract | Crossref Full Text | Google Scholar
26. Tiegs AW, Sun L, Patounakis G, Scott RT. Worth the wait? Day 7 blastocysts have lower euploidy rates but similar sustained implantation rates as day 5 and day 6 blastocysts. Hum Reprod. (2019) 34:1632–9. doi: 10.1093/humrep/dez138
PubMed Abstract | Crossref Full Text | Google Scholar
27. Park DS, Kim JW, Chang EM, Lee WS, Yoon TK, Lyu SW. Obstetric, neonatal, and clinical outcomes of day 6 vs. Day 5 vitrified-warmed blastocyst transfers: retrospective cohort study with propensity score matching. Front Endocrinol (Lausanne). (2020) 11:499. doi: 10.3389/fendo.2020.00499
PubMed Abstract | Crossref Full Text | Google Scholar
28. Boynukalin FK, Gultomruk M, Cavkaytar S, Turgut E, Findikli N, Serdarogullari M, et al. Parameters impacting the live birth rate per transfer after frozen single euploid blastocyst transfer. PloS One. (2020) 15:e0227619. doi: 10.1371/journal.pone.0227619
PubMed Abstract | Crossref Full Text | Google Scholar
29. Abdala A, Elkhatib I, Bayram A, Arnanz A, El-Damen A, Melado L, et al. Day 5 vs day 6 single euploid blastocyst frozen embryo transfers: which variables do have an impact on the clinical pregnancy rates? J Assist Reprod Genet. (2022) 39:379–88. doi: 10.1007/s10815-021-02380-1
PubMed Abstract | Crossref Full Text | Google Scholar
30. Yuan S, Liu J, Larsson SC. Smoking, alcohol and coffee consumption and pregnancy loss: A mendelian randomization investigation. Fertil Steril. (2021) 116:1061–7. doi: 10.1016/j.fertnstert.2021.05.103
PubMed Abstract | Crossref Full Text | Google Scholar
31. Pineles BL, Park E, Samet JM. Systematic review and meta-analysis of miscarriage and maternal exposure to tobacco smoke during pregnancy. Am J Epidemiol. (2014) 179:807–23. doi: 10.1093/aje/kwt334
PubMed Abstract | Crossref Full Text | Google Scholar
33. Ghimire PR, Akombi-Inyang BJ, Tannous C, Agho KE. Association between obesity and miscarriage among women of reproductive age in Nepal. PloS One. (2020) 15:e0236435. doi: 10.1371/journal.pone.0236435
留言 (0)