Members of the Burkholderia cepacia complex (Bcc) consisting of 22 species are oxidase-positive, rod-shaped, non-fermenting Gram-negative bacteria (NFGNB)1,2. They are found ubiquitously in various natural and man-made habitats owing to their exceptional metabolic adaptability3. These opportunistic pathogens are responsible for a wide range of infections and complications in immunocompromised individuals4,5. Their ability to cause life-threatening infections in intensive care settings and paediatric patients is well recognized.
Bcc causes severe pulmonary infections in cystic fibrosis (CF) and chronic granulomatous disease (CGD) patients6,7. Additionally, it induces bacteremia in patients, with host and environmental risk factors like prolonged hospital stay, medical co-morbidities, use of central venous catheters (CVC) and exposure to medical products, like ultrasound gels and devices8,9.The bacteria’s survival and replication in indwelling invasive devices, resistance to disinfectants, and ability to persist in moist environments and surfaces like water tanks, sinks, taps and others with restricted nutrition highlight its significance as an emerging nosocomial pathogen globally. Bcc’s endurance to pharmaceutical products and devices makes them function as a potential reservoir of infection in hospital settings, facilitating outbreaks in the event of breaches in infection prevention and control practices (IPC)3,5,10. The patient-to-patient transmission also contributes to Bcc colonization. Bcc exhibits a distinctive antimicrobial profile, posing challenges to treatment. Intrinsic resistance, especially to antibiotics like polymyxins and aminoglycosides, and rising multi-drug resistance further complicates management2,11. Moreover, a limited understanding of pathogenicity, laboratory identification and differentiation from other NFGNBs leads to underreporting and inadequate treatment of Bcc infections.
Numerous Bcc outbreaks from hospital settings have been reported globally, including those from India. Bcc has been known to contaminate many medical products, such as ultrasound gel12, detergents, and moisturizing creams13, pharmaceutical preparations like IV fluids14, chlorhexidine solutions and mouthwash15, rubber stoppers of drug vials16, nebulized salbutamol17 and devices like respiratory equipment17. It is known to survive in distilled water by utilizing trace amounts of organic compounds and carbon dioxide as energy sources18,19. Intravenous (IV) medications, including antiemetic drug vials and multidose amikacin vials, have been identified as sources of infection. These outbreaks have been reported in ICU settings and dialysis units and are common among paediatric populations16,20. However, in the available literature, a comprehensive study analyzing the Bcc outbreaks, specifically of Indian origin, is lacking. To address this gap and create awareness, we conducted a scoping review on nosocomial Bcc outbreaks from India that were published in peer-reviewed scientific journals. The objective of the review was to analyze infection sources, outbreak investigations, affected patient populations, and control strategies in the Indian context.
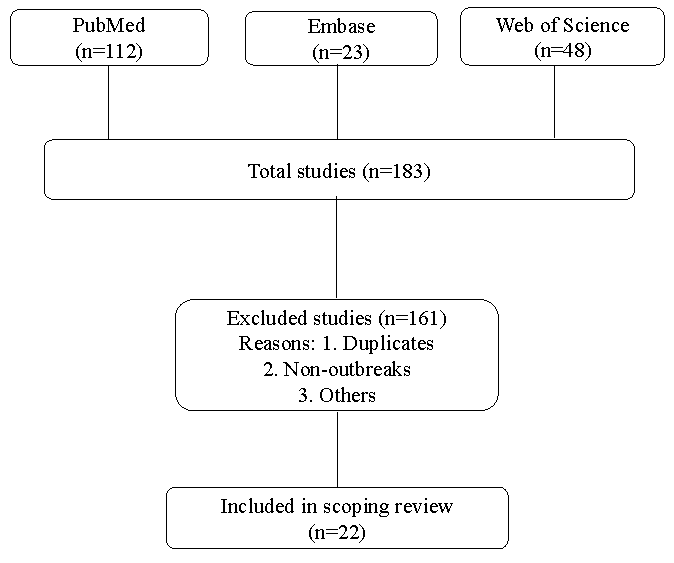
Materials & MethodsThe study followed PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) guidelines. The PRISMA-ScR 22 points checklist (Supplementary Table) has been referred to while formulating this review. Databases such as ‘PubMed’ (https://pubmed.ncbi.nlm.nih.gov), ‘Embase’ (https://www.embase.com) and ‘Web of Science’ (https://clarivate.com) were utilized. Literature published between 1993 and September 2024 and only in English was included in this review. Furthermore, the references cited in the included studies were assessed (Figure). The combination of search terms used was as follows: (Burkholderia cepacia complex OR Burkholderia species OR Pseudomonas cepacia; MeSH Terms) AND (outbreak; MeSH Terms) AND (India; MeSH Terms) (Supplementary Material). Search terms like contaminated drugs or pharmaceuticals were not used as they would limit the search results.
Export to PPT
Included were prospective, retrospective and cohort studies assessing Bcc outbreaks due to any source in Indian hospital settings. However, conference abstracts and case reports (less than 3 patients infected) were excluded. Studies that only reported the outbreak up to the point of identification, without investigating potential sources, were also excluded. This was based on the rationale that without investigating the possible source, no valid conclusions can be drawn; neither would it substantially contribute to infection prevention strategies for avoiding such nosocomial outbreaks. We thoroughly documented essential details, encompassing outbreak features, patient population, nature of infections, investigation for infection source, and the implementation of infection prevention and control (IPC) strategies to manage the outbreak. ‘Extrinsic contamination’ of medical products is defined as the introduction of contamination during product utilization, while ‘intrinsic contamination’ refers to contamination occurring before use, specifically at the level of manufacturing21.
Three reviewers (AS, SM, and LS) charted the data to extract data from the included studies. The table was created in two parts. First, the general characteristics of the published studies were charted with the following information: author, year of outbreak, city/State of India, number of patients affected, patient population, source of outbreak, type of Burkholderia species identified, infection type, and what method of molecular typing, if used, was done. The charted data was then rearranged according to a common denominator: the outbreak’s source. Source categories were pharmaceutical preparations, medical products, environment, medical devices, and no source identified. The second table compiled the data of studies that successfully identified the source of the outbreak, and the relevant infection prevention and control (IPC) strategies used to curb the outbreaks. The assessment of potential bias and heterogeneity was not conducted. Basic statistical methods like percentages were used to summarize and communicate key trends in the data.
ResultsFor this analysis, our search identified 22 published studies of hospital-acquired Burkholderia cepacia complex outbreaks across India, which met our criteria (Table I)12,15,16,19,20,22-38. Ten outbreaks were reported from southern States of India12,19,22,23-29 (6 from Tamil Nadu, 2 from Karnataka, 1 from Puducherry, & 1 from Kerala), six outbreaks were reported from western States15,16,20,30-32 (5 from Maharashtra & 1 from Rajasthan), five from northern States33-37 (2 from Delhi, 1 each from Haryana, Chandigarh and Jammu & Kashmir) and one from the eastern State of West Bengal38.
Table I: Literature review of hospital outbreaks of Burkholderia cepacia complex in India
S. No. Author Year of the Outbreak State of India No. & patient population affected Source Burkholderia species isolated Infection type Molecular confirmation Source: Pharmaceutical preparations (10) 1. Singhal et al20 2009 Mumbai, Maharashtra 13 Adults, Chemotherapy day care unit Antiemetic granisetrone IV medication Burkholderia cepacia Bacteremia Not performed 2. Tandel et al15 2010 Pune, Maharashtra 12, Surgical ICU Cetrimide + Chlorhexidine solution for skin antisepsis Burkholderia cepacia Bacteremia Not performed 3. Lalitha et al22 December 2011-February 2012 Madurai, Tamil Nadu 13, post-cataract surgery patients Topical anaesthetic eye drops Burkholderia cepacia Endophthalmitis BOX-PCR 4. Mali et al16 June 2012-January 2013 Mumbai, Maharashtra 76, Paediatric ICU & Paediatric ward Rubber stopper of amikacin vials Burkholderia cepacia complex Bacteremia recA PCR & E-MLST 5. Paul et al19 January 2014 Mangalore, Karnataka 12, NICU Opened IV fluid 5% Dextrose, Normal saline & CPPV humidifier water (Also included in Environment category) Burkholderia cepacia Bacteremia Not performed 6. Shrivastava et al31 October 2015 Mumbai, Maharashtra 7, NICU Unopened & opened vials of caffeine citrate Burkholderia cepacia Bacteremia Not performed 7. Fomda et al35 October 2017 -October 2018 Srinagar, Jammu & Kashmir 121, Surgical ICU Unopened Normal saline, Chlorhexidine mouthwash Burkholderia cepacia Bacteremia Not performed 8. Sridharan et al23 February-March 2019 Chennai, Tamil Nadu 40, Cardiac care unit Unopened vials of Diltiazem Burkholderia cepacia Bacteremia Not performed 9. Murugesan et al24 March 2019 Vellore, Tamil Nadu 11, Cardiology ward Opened & unopened vials of Diltiazem Burkholderia contaminans Bacteremia MLST 10. Ghafur et al25 August- December 2021 Chennai, Tamil Nadu 56, Oncology ward Antiemetic palonosetron IV medication Burkholderia cenocepacia Bacteremia MLST Source: Environment (2+1) 11. Rastogi et al33 April-November 2014 New Delhi 48, Neurotrauma ICU Water supply & RO water Burkholderia cepacia Bacteremia, CLABSI, VAP MLST 12. Antony et al26 2016 Mangalore, Karnataka 3, Paediatric ICU Distilled water used for nebulizers & humidification of oxygen Burkholderia cepacia Bacteremia Not performed Source: Medical products (4) 13. Solaimalai et al12 October 2016 Vellore, Tamil Nadu 7, Paediatric ICU In-use Ultrasound gel Burkholderia cepacia complex Bacteremia MLST 14. Yamunadevi et al27 November 2016-January 2017 Chennai, Tamil Nadu 24, Cardiac care unit Ultrasound gel Burkholderia cepacia Bacteremia Not performed 15. Dogra et al37 February 2020 Chandigarh 4, Paediatric surgical ward In-use Ultrasound gel Burkholderia multivorans Bacteremia MALDI-TOF, MLST 16. Raj et al28 June 2018- December 2020 Thiruvananthapuram, Kerala 84, inborn nursery In-use Ultrasound gel Burkholderia cepacia Bacteremia Not performed Source: Medical device (1) 17. Bharara et al36 March 2019 Gurgaon, Haryana 4, NICU Suction apparatus Burkholderia cepacia complex Bacteremia Not performed Source: Not identified (5) 18. Bhise et al30 April 2013 Nagpur, Maharashtra 10, NICU No source identified Burkholderia cepacia Bacteremia Not performed 19. Bhatia et al34 August 2015-July 2016 New Delhi 147, Various ICU’s No source identified Burkholderia cepacia Bacteremia Not performed 20. Gupta et al32 September-October 2016 Jaipur, Rajasthan 14, Oncology ward No source identified Burkholderia cepacia CLABSI Not performed 21. Baul et al38 September 2016 – February 2017 Kolkata, West Bengal 29, Haemato-oncology ward No source identified Burkholderia cepacia complex Bacteremia PCR & PFGE 22. Deb et al29 July-August 2019 Puducherry 5, (4 post-cataract & 1 post-keratoplasty) No source identified Burkholderia cepacia complex Endophthalmitis Not performed Sources of Bcc outbreaks in IndiaOut of the 22 Bcc outbreak studies, a source could be identified in 17 studies while in five studies29,30,32,34,38, no source was identified. The majority of the outbreak investigations (n=10) were concerned with pharmaceutical products, which included IV antiemetics granisetron20 and palonosetron25, topical anaesthetic eyedrops22, upper surface of rubber stopper of sealed multidose amikacin vials16, opened IV fluids19,35 (5% Dextrose, normal saline), unopened and opened vials of caffeine citrate31, diltiazem vials23,24, cetrimide and chlorhexidine solution for skin antisepsis15 and chlorhexidine mouthwash35. The source was identified to be distilled water used for nebulization and oxygen humidification in two studies19,26. The gel used during Ultrasonography (USG) was recognized as the source of the Bcc outbreak in four studies12,27,28,37. One study each was associated with contaminated water supply, including RO (reverse osmosis) water33 and suction apparatus36.
Among the identified sources of the outbreaks, the source was associated with pharmaceutical preparations in 45.4 per cent of the studies, the environment 13.6 per cent, medical products in 18.1 per cent, and devices in 4.5 per cent. Out of the 14 studies implicating medical and pharmaceutical products as culprits, intrinsic contamination was present in 10 compared to four outbreaks having extrinsic contamination.
General characteristics of the Indian Bcc outbreaksSeven hundred and forty patients were affected across these 22 outbreaks. With pharmaceutical preparations as the source of the outbreak, the majority occurred in intensive care unit (ICU) settings as reported in five studies15,19,23,31,35 involving 192 patients. Hospital wards were affected in three studies with a total of 80 patients, including chemotherapy day care unit20, cardiology ward24, and oncology ward25. One study reported a Bcc outbreak among 13 post-cataract surgery patients associated with anaesthetic eyedrops22. Another study reported an outbreak associated with contaminated rubber stoppers of amikacin vials, involving both paediatric ICU and ward16, affecting 76 children. The majority of the patients were adults (n=266), where as paediatric population associated with pharmaceutical preparation-related outbreaks comprised 95 individuals. Among these 19 (20%) were exclusively confined to the neonatal intensive care unit (NICU). Out of the 10 studies, three mentioned outcomes in terms of mortality, which were nil (0/13) in Singhal et al20, 27.6 per cent (21/76) in Mali et al16, and 16.6 per cent (2/12) in Paul et al19. In one study by Lalitha et al22 involving cataract surgery patients, 69 per cent (9/13) had a final visual acuity of 6/60 or better, 23 per cent (3/13) had a vision of perception of light and 7.6 per cent (1/13) had a final vision of 1/60.
Three outbreaks linked to environmental contamination occurred in neurotrauma33, neonatal19, and paediatric26 ICUs, involving 63 patients. Of these, 48 were adults, and 15 were in paediatric age group. Two out of three studies mentioned outcomes in terms of mortality, nil (0/3) in Antony et al26, and 16.6 per cent (2/12) in Paul et al19. Bcc outbreaks linked to medical products, specifically ultrasound gel, were reported in four studies. Two of these outbreaks involved ICU patients12,27, while one occurred in a paediatric ward37 and another in an inborn nursery28. Twenty-four adults were affected, whereas 95 were paediatric patients, of which 84 (88.4%) were neonates. Two studies out of four mentioned outcomes as 42.8 per cent (3/7) mortality by Solaimalai et al12, and a case fatality rate of 26 per cent by Raj et al28. One study pinpointed suction apparatus36 (medical device) as the source, involving four patients in the neonatal ICU, and the mortality rate was 25 per cent (1/4).
Outbreaks in which sources could not be identified, the majority occurred in ICU settings, as reported in two studies30,34, involving a total of 157 patients. Oncology32 and hemato-oncology38 wards were affected in two studies with 43 patients. One outbreak was reported among five post-operative patients following cataract and keratoplasty surgery29. Outbreaks with no source identified affected 195 adults and ten neonates. Mortality outcomes were reported in two studies: Bhise et al30 documented a rate of 30 per cent (3/10), while Baul et al38 reported 3.5 per cent (1/28). One study by Gupta et al32 reported the removal of central venous catheters as an outcome, with a rate of 71.4 per cent (10/14). In a study by Deb et al29 involving five patients with endophthalmitis, the outcomes recorded were as follows: two patients achieved a best-corrected visual acuity (BCVA) of 20/60, two had a BCVA better than 20/200, and one patient had no perception of light.
In 20 studies, patients presented with Bcc bacteremia12,15,16,19,20,23-28,30-38. Out of these, two studies had central line-associated bloodstream infections (CLABSI)32,33, and one study also reported ventilator-associated pneumonia (VAP)33. In the remaining two outbreak studies, endophthalmitis was the clinical presentation22,29. Only four studies specified the exact antibiotic treatment administered, while the rest stated that susceptibility patterns guided treatment without specifying the drugs. Ceftazidime in combination with meropenem/levofloxacin12, and cotrimoxazole in combination with meropenem/ceftazidime28 were used for treatment in one study each.
The species identified in 14 outbreaks was Burkholderia cepacia15,19,20,22,23,26-28,30,31-35. In five studies, Burkholderia cepacia complex12,16,29,36,38 was identified, and B. cenocepacia25, B. multivorans37 and B. contaminans24 was identified as the causative agent in three independent outbreaks. Bcc identification was performed using conventional phenotypic methods in seven studies12,15,20,22,27,30,32. Seven studies employed the automated Vitek 2 system19,25,26,28,31,34,36, and five studies used Matrix-assisted laser desorption/ionization-time of flight (MALDI-TOF)23,24,29,35,37. Additionally, recA PCR was used in two studies16,33, and one study utilized the automated MicroScan panel for identification38.
Molecular methods used for clonal associationMulti-locus sequence typing (MLST) was predominantly used to assess clonality in isolates for six outbreaks12,16,24,25,33,37. Other techniques, such as repetitive extragenic palindromic-polymerase chain reaction (PCR) (BOX-PCR)22, pulse field gel electrophoresis (PFGE)38 in one outbreak each, and MALDI-TOF37 in another, were utilized to study clonal association. In 14 of the documented outbreaks, microbial typing was not conducted.
Management of Indian Bcc outbreaksVarious IPC strategies were used to curb the outbreaks (Table II). In most studies, contaminated stocks of pharmaceutical products were discarded. The concerned manufacturers were informed, and regular sterility testing was implemented15,16,19,20,22-24,
留言 (0)