Dear Editor,
Combination of topical cholesterol and statin has been successfully used in several subtypes of porokeratosis, including disseminated superficial actinic porokeratosis.1 Nonetheless, this preparation is not commercially available and self-compounding is increasingly difficult due to regulatory reasons. Thus, we reported our experience of using topical duck egg yolk oil (4% cholesterol) twice daily with oral rosuvastatin 10 mg once daily for disseminated superficial actinic porokeratosis in two patients with success after six months of therapy.
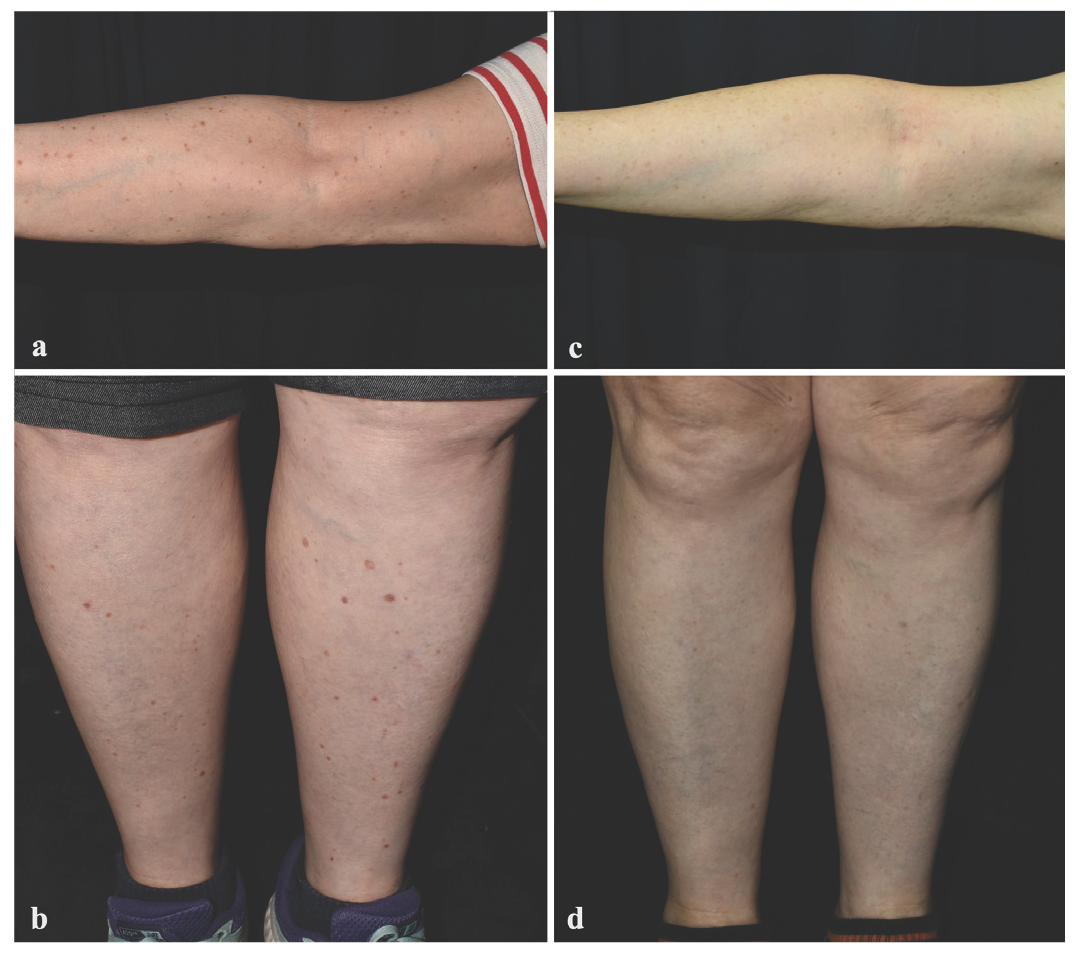
The first patient was a 75-year-old woman who developed scaly, hyperkeratotic plaques on the extremities and abdomen after Moderna COVID-19 (messenger ribonucleic acid [mRNA]-1273) vaccination in 2022. Dermoscopic examination of the lesion revealed a characteristic keratin rim and atrophic centre, and a diagnosis of disseminated superficial actinic porokeratosis was made clinically. Other family members were unaffected. She had tried topical diclofenac, rapamycin, and retinoic acid but the response was limited. She started applying topical duck egg yolk oil twice daily with oral rosuvastatin 10 mg once daily since May 2023 [Figure 1a, 1b]. Partial improvement was noticed since September 2023 and the patient showed almost complete clearing of active lesions in May 2024 [Figure 1c, 1d]. Only mild skin irritation was noted, but it did not necessitate treatment discontinuation.
Export to PPT
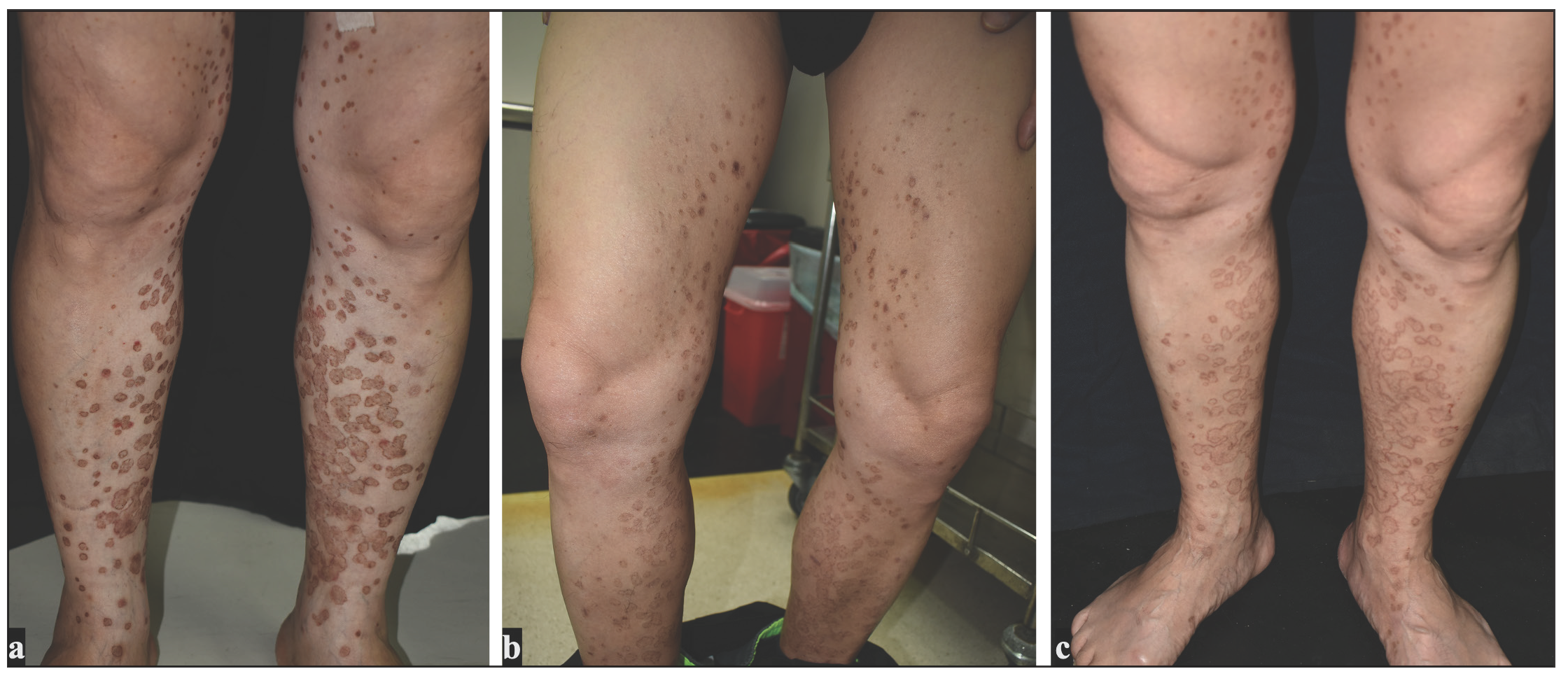
The second patient was a 55-year-old man with hypercholesterolemia, on treatment with 10 mg rosuvastatin daily for many years, presented with itchy, brownish, hyperkeratotic, confluent plaques on the lower extremities since early 2023. Dermoscopy showed brownish dots, central atrophy, and an annular border with scales. Histopathology confirmed the diagnosis of porokeratosis with typical cornoid lamella. Other family members were unaffected and the patient gave no history of recent new medications. He failed to improve with topical clobetasol, tacrolimus, diclofenac, and photodynamic therapy. He began to apply topical duck egg yolk oil twice daily since September 2023 [Figure 2a] and noticed flattening of the lesions one month later. He kept using topical preparation twice daily. Only hyperpigmentation on the borders of lesions remained after six months of treatment ([Figure 2b]. The patient stopped topical egg yolk oil for two months from March 2024 onwards and the lesions gradually worsened with enlargement and coalescing larger plaques [Figure 2c]. Rechallenge with topical egg yolk oil led to an improvement in the porokeratotic lesions again. Oral rosuvastatin 10 mg/day for underlying hypercholesterolemia was continued during the whole course.
Export to PPT
Many reports of topical statins have shown the effectiveness for porokeratosis, including lovastatin1 and simvastatin2 with or without the combination of topical cholesterol. Statin derivative inhibits the proliferation of keratinocytes and causes the G0/G1 arrest.3 Mutation of some genes in the mevalonate pathway causes cholesterol deficiency, early apoptosis of keratinocytes disrupting the stratum corneum, whereas buildup of byproducts can cause keratinocyte dysmaturation, leading to porokeratosis development. Topical egg yolk oil may be helpful in porokeratosis by replenishing the cholesterol and preventing the accumulation of toxic metabolites.4 Egg yolk oil also exerts an anti-inflammatory effect via regulating the Nrf2/NF-κB (nuclear factor erythroid 2-related factor/kappa light chain enhancer of activated B cells) pathway,5 but whether these additional benefits/ingredients contribute to the success in porokeratosis treatment remains to be studied.
In contrast with a previous study showing no significant difference between topical lovastatin with or without cholesterol,1 our observation in the second patient demonstrated a beneficial role of oral statin in treating porokeratosis only after adding topical cholesterol. Egg yolk oil typically compromises about 65% triglycerides, 28.3% phospholipids, and 5.2% cholesterol.6 According to the package insert, the carbon dioxide supercritical fluid extracted duck egg yolk oil used in both of these patients, consists of approximately 3.9% carbohydrate, 0.2% protein, and 95.9% lipid. The lipid part is composed of 65% triglycerides, 30% phospholipid, 4% cholesterol, and trace glycolipid. According to existing literature, egg yolk oil has been used as a topical preparation in traditional Chinese medicine for several centuries and its use was mentioned in a famous traditional Chinese medicine textbook Compendium of Materia Medica in 1578, with good skin compatibility and there are no reported skin adverse effects.7 It is a commercial cosmetic product available in many countries like Japan, Taiwan, Hong Kong and Australia. Due to the lack of proprietary preparation of topical statins with cholesterol, the use of oral statin and topical egg yolk oil might offer a potentially cost-effective alternative for patients with disseminated superficial actinic porokeratosis. Nonetheless, the sustainability and whether recurrence or other complications could occur on prolonged follow-up remains unknown. Thus, more studies are needed to confirm its efficacy and safety.
留言 (0)