Non-venereal genital dermatoses are those genital dermatoses which are not sexually transmitted.1 Based on aetiology, non-venereal genital dermatoses are broadly classified into three types: physiological conditions, infections and infestations, and non-infectious diseases. Non-venereal genital dermatoses may cause emotional distress and interpersonal issues, especially if they are noticed after sexual intercourse.2 Assessing the impact of these dermatoses on the quality of life can help in providing appropriate treatment and counselling services.2
The scope of dermoscopy is vast and it is being currently utilised to examine diseases of the mucosa (mucoscopy).3 Due to concerns about spreading infection, dermatologists were hesitant to perform regular mucoscopy. Innovative solutions, such as the usage of cling film and barrier footplates, have now allayed these concerns.3 By providing a better view of the lesions, it may prevent unnecessary biopsies.
The aim of the present study was to determine the clinical and epidemiological pattern of non-venereal genital dermatoses, describe their dermoscopy findings and determine their impact on the quality of life.
MethodsThis was a prospective, cross-sectional observational study conducted in the Dermatology outpatient department and also included cases referred from the Gynaecology and Urology departments, done over a period of 18 months from September 2021 to March 2023, after obtaining approval from Institutional Ethics Committee (Certificate reference no. AIIMS/IEC/2021/3597 dated 06/09/2021).
All patients with external genital lesions with or without extragenital lesions were included after obtaining informed consent. Patients who were partially treated or taking treatment from outside, and those presenting with a venereal disease diagnosed clinically or based on laboratory investigations (HIV, HbsAg, Anti HCV and RPR) were excluded from the study.
Detailed history and clinical examination were recorded in a structured proforma. Detailed sexual history regarding number of partners, practices, frequency and last exposure, protected or unprotected or influence of intoxicating agent if any, contraception practices, past history of STD in self and partner were recorded. A baseline clinical image of lesions was taken. The dermoscopy examination was performed by two authors (SS and AB) to maintain the uniformity in evaluation using a manual hand-held dermotoscope Heine delta 30 at 10× magnification, polarised mode and 12 megapixels (MP) mobile camera was used for photographic documentation. Disposable overhead projector transparent sheets were used between the dermotoscope lens and genital skin to maintain hygiene and avoid transmission of infections. Further relevant investigations like skin biopsy were done where indicated. The impact of disease on the quality of life was assessed by a dermatology life quality index questionnaire.
Statistical AnalysisCategorical variables were expressed in the form of numbers and percentages. Quantitative data with normal distribution were presented as means ± SD. To determine the statistical differences in quantitative variables, t-test and one-way ANOVA test were employed. The final data analysis was done using SPSS ver. 23 software and a p-value of <0.05 was considered statistically significant.
ResultsOut of 93,399 outpatients examined during the 18-month study period, the total number of patients who came with genital complaints was 939, of which 427 (45.5%) were sexually transmitted infections (STIs) and 512 (54.5%) were non-venereal genital dermatoses. Out of these 512 patients, 9 cases were inconclusive (where final diagnosis could not be reached on clinical and histological assessment) and 503 patients fulfilling inclusion and exclusion criteria were recruited in the study. Among these 503 patients, a total of 44 patients were referred from Gynaecology and Urology department. Excluding these referred cases, the overall prevalence of non-venereal genital dermatoses was found to be 49.1 per 10,000 dermatology outpatients. The age of the patients ranged from 4 months to 87 years with a mean age of 34.9 ± 16.5 years. Most patients belonged to the age group of 20–29 years (n=154, 30.6%). Males (n=429 patients) outnumbered females (n=74 patients) in a ratio of 5.8:1. Most of the patients (n=299, 59.4%) were married and resided in rural regions (n=283, 56.2%).
Four hundred and fifty-seven patients (90.9%) had single dermatoses, whereas multiple dermatoses were found in 46 patients (9.1%). Hence, a total of 550 cases were counted in the final analysis.
Dermoscopic features corroborated the clinical diagnosis in 407 (74%) cases and histopathology was done for 59 (10.7%) doubtful cases for confirmation of the diagnosis.
A total of 49 different dermatoses were noted in this study [Table 1]. The most common group of dermatoses was infections and infestations 126 (22.9%), of which scabies was the most common disease 97 (17.6%). It was followed in frequency by eczematous disorders 78 (14.2%), miscellaneous disorders 76 (13.8%), physiological conditions 56 (10.2%) and vitiligo 54 (9.8%).
Table 1: Distribution of various dermatoses (n=550) along with DLQI (n=537) and Venerophobia (n=76)
S. no Disease Male Female Total [n=550] (%) DLQI [n=537] Venereophobia [n=76] (% of respective diseases) Mean ± SD Range (Min-Max) Physiological conditions [n=56, (10.2%)] 1. Pearly penile papules 23 0 23 (4.2) 3 ± 2.0 0–8 9 (39.1) 2. Melanosis 22 0 22 (4) 2.1 ± 1.9 0–7 1 (4.5) 3 Fordyce spots 10 0 10 (1.8) 3.2 ± 2.3 0–8 8 (80) 4 Benign vulvar vestibular papillomatosis 0 1 1 (0.2) 8 - 1 (100) Infections and infestations [n=126, (23%)] 5 Scabies 95 2 97 (17.6) 3.3 ± 1.1 1–7 0 (0) 6 Candidiasis 9 4 13 (2.4) 3.3 ± 1.8 1–7 2 (15.4) 7 Tinea cruris 8 1 9 (1.6) 3 ± 1.3 2–6 1 (11.1) 8 Pityriasis versicolor 0 1 1 (0.2) 3 - 0 (0) 9 Mucormycosis 1 0 1 (0.2) 5 - 0 (0) 10 Pyoderma 2 0 2 (0.4) 3 ± 0.0 3–3 0 (0) 11 Surgical site infection 2 0 2 (0.4) 7 ± 2.8 5–9 0 (0) 12 Necrotising fasciitis 1 0 1 (0.2) 8 - 0 (0) Eczematous disorders [n=78, (14.2%)] 13 Lichen simplex chronicus 33 10 43 (7.8) 4.3 ± 1.6 1–8 2 (4.7) 14 Scrotal dermatitis 22 0 22 (4) 4.2 ± 1.9 1–10 0 (0) 15 Irritant contact dermatitis 11 0 11 (2) 4.4 ± 2.4 2–9 0 (0) 16 Atopic dermatitis 0 1 1 (0.2) - - 0 (0) 17 Seborrheic dermatitis 1 0 1 (0.2) 2 - 0 (0) Papulosquamous disorders [n=33, (6%)] 18 Psoriasis 25 8 33 (6) 4.2 ± 1.9 1–9 1 (3) Lichenoid disorders [n=47, (8.5%)] 19 Lichen planus 37 2 39 (7.1) 3.7 ± 1.4 1–6 17 (43.6) 20 Lichen nitidus 8 0 8 (1.4) 3.3 ± 1.9 2–7 4 (50) Sclerosing disorders [n=43, (7.8%)] 21 Lichen sclerosus 23 20 43 (7.8) 5.3 ± 2.4 1–11 4 (9.3) Neutrophilic dermatoses [n=3, (0.5%)] 22 Behcet’s disease 2 1 3 (0.5) 5.3 ± 0.6 5–6 2 (66.7) Vesiculobullous disorders [n=2, (0.4%)] 23 Pemphigus vulgaris 1 1 2 (0.4) 6.5 ± 0.7 6–7 0 (0) Drug reactions [n=9, (1.6%)] 24 Fixed drug eruption 5 0 5 (0.9) 6.2 ± 1.3 5–8 0 (0) 25 Stevens-Johnson syndrome 2 2 4 (0.7) 11.7 ± 2.2 10–15 0 (0) Pigmentary disorders [n=54, (9.8%)] 26 Vitiligo 48 6 54 (9.8) 3.4 ± 1.6 0–7 6 (11.1) Vascular lesions [n=18, (3.3%)] 27 Angiokeratoma 14 2 16 (2.9) 2.8 ± 1.7 1–7 1 (6.3) 28 Vulvar varicosities 0 2 2 (0.4) 0.50 ± 0.7 0–1 0 (0) Premalignant and malignant [n=5, (1%)] 29 Bowen’s disease 1 0 1 (0.2) 3 - 0 (0) 30 Pseudoepitheliomatous keratotic and micaceous balanitis 1 0 1 (0.2) 10 - 0 (0) 31 Squamous cell carcinoma 1 1 2 (0.4) 6.5 ± 0.7 6–7 1 (50) 32 Cutaneous metastasis 0 1 1 (0.2) 6 - 0 (0) Miscellaneous [n=76, (13.8%)] 33 Idiopathic scrotal calcinosis 27 0 27 (4.9) 2.1 ± 1.2 1–6 2 (7.4) 34 Steatocystoma 7 1 8 (1.4) 3.6 ± 3.6 0–11 1 (12.5) 35 Cutaneous horn 1 0 1 (0.2) 1 - 0 (0) 36 Zoon’s balanitis 20 0 20 (3.6) 3.8 ± 2.1 1–10 10 (50) 37 Circinate balanitis 4 0 4 (0.7) 6.2 ± 3.3 4–11 2 (50) 38 Lymphangiectasia 1 1 2 (0.4) 1.5 ± 0.7 1–2 0 (0) 39 Seborrheic keratosis 2 0 2 (0.4) 3 ± 2.8 1–5 1 (50) 40 Porokeratosis 1 0 1 (0.2) 1 - 0 (0) 41 Verrucous epidermal naevus 0 1 1 (0.2) - - 0 (0) 42 Incontinentia pigmenti 0 1 1 (0.2) - - 0 (0) 43 Systemic lupus erythematous 0 1 1 (0.2) 7 - 0 (0) 44 Lipschutz ulcer 0 1 1 (0.2) 10 - 0 (0) 45 Calciphylaxis 1 0 1 (0.2) 11 - 0 (0) 46 Genital Crohn’s disease 0 2 2 (0.4) 6.5 ± 2.1 5–8 0 (0) 47 Angiomyxoma 0 1 1 (0.2) 11 - 0 (0) 48 Pseudodfolliculitis 0 1 1 (0.2) 1 - 0 (0) 49 Topical steroid induced atrophy 2 0 2 (0.4) 2.5 ± 0.7 2–3 0 (0)Among males (474 cases), the most common dermatosis noted was scabies 95 (20%) followed by vitiligo 48 (10.1%) and lichen planus 37 (7.8%). In females (76 cases), the most common dermatosis was lichen sclerosus 20 (26.3%) followed by lichen simplex chronicus 10 (13.1%).
In males (n=474 cases), scrotum (260/474, 54.6%) was the most common site of involvement and in females (n=76 cases), commonest site was labia majora (62/76, 81.6%).
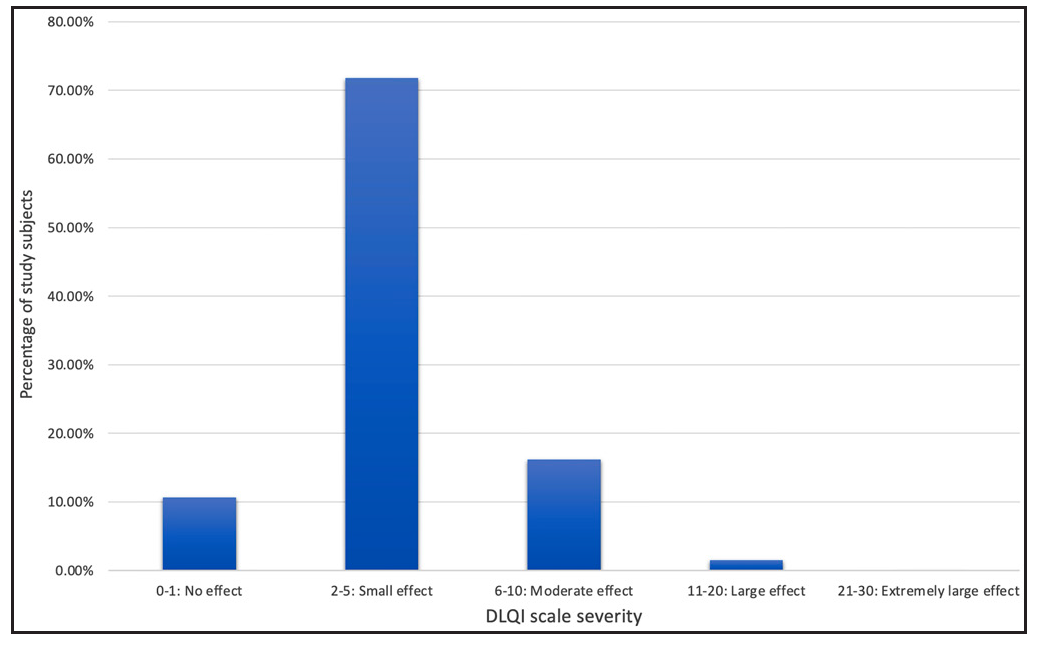
Quality of life was calculated for 537 cases [Figure 1] and it was adversely affected in 527 (98.1%) patients. There was a large effect in 8 (1.5%), moderate effect in 87 (16.2%) and small effect in 385(71.8%) patients. Fifty-seven (10.7%) cases were not bothered by the illnesses. DLQI was significantly increased in females than males. When DLQI in individual dermatoses were calculated [Table 1], it was noticed that angiomyxoma of the vulva, pseudoepitheliomatous keratotic and micaceous balanitis (PKMB) and Lipschutz ulcer had a significant impact on the quality of life. Premalignant and malignant diseases had moderate impact. However, lichen sclerosus had a moderate impact and chronic conditions like psoriasis, lichen planus, vitiligo and Zoon’s balanitis had a small impact on daily activities.
Export to PPT
A total of 76 (15.1%) patients had venerophobia and out of them, 74 were men (17.2% of total male patients). A total of 20 diseases had some components of venerophobia [Table 1]. A few physiological conditions like benign vulvar vestibular papillomatosis, Fordyce spots, pearly penile papules and chronic inflammatory conditions like Zoon’s balanitis and lichen planus had a significant degree of venerophobia.
The clinical and dermoscopic features of individual dermatoses are described below.
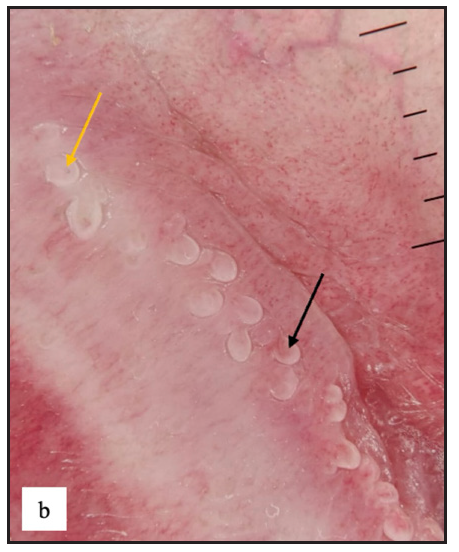
Pearly penile papulesA total of 23 (4.2%) cases of pearly penile papules were observed. Clinically, patients presented with pearly white round discrete 1–2 mm sized papules circumferentially over the coronal sulcus in a single or double row and were most prominent over the dorsolateral aspect [Figure 2a]. Dermoscopic examination revealed white to pinkish cobblestone appearance (n=23, 100%), central curved vessel (n=15, 65.2%) and dotted vessel (n=13, 56.5%) [Figure 2b].
Export to PPT
Export to PPT
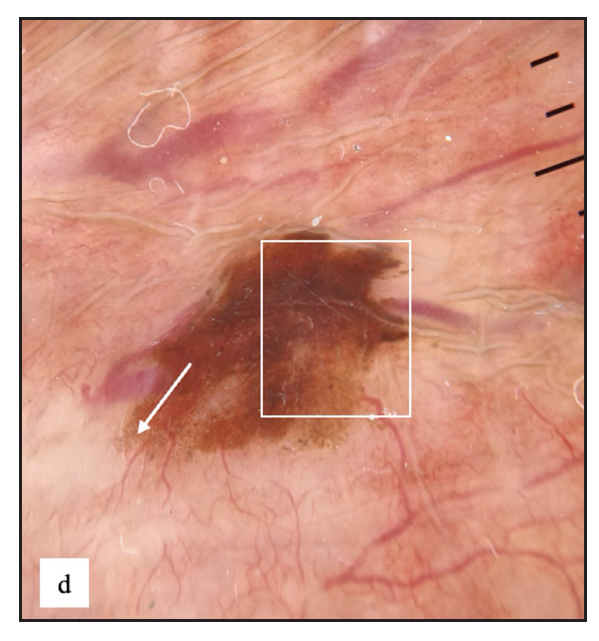
Genital melanosisTwenty-two males (4%) complained of melanosis on the external genitalia. All patients presented with asymptomatic brown to black well-defined single to multiple hyperpigmented macules, most commonly over the penile shaft in 20 (90.9%) cases [Figure 2c]. The most common dermoscopic parameter was brown structureless areas that were characterised by different shades of brown to black in 21 (95.5%) cases and black dots in 11 (50%) cases [Figure 2d].

Export to PPT
Export to PPT
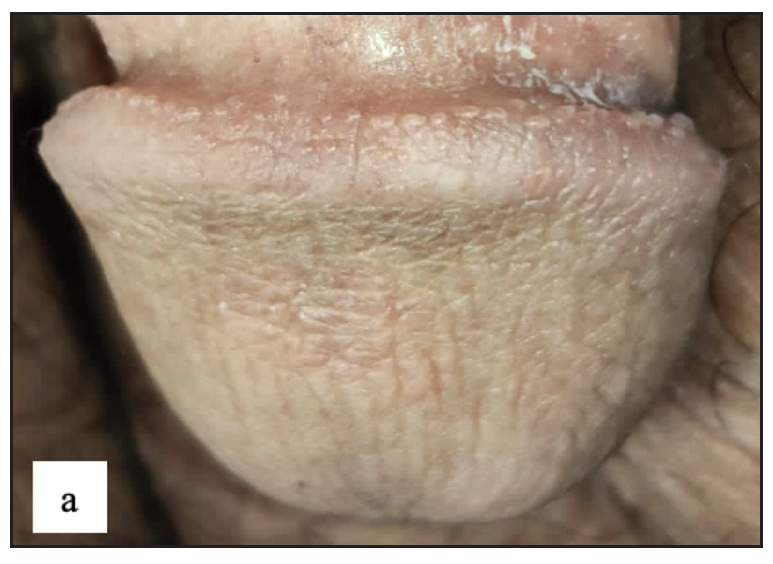
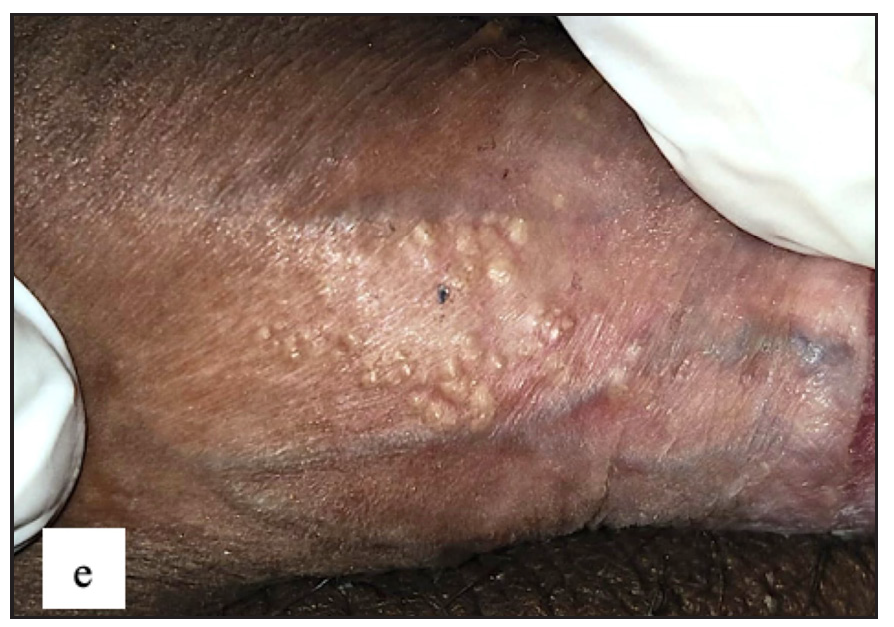
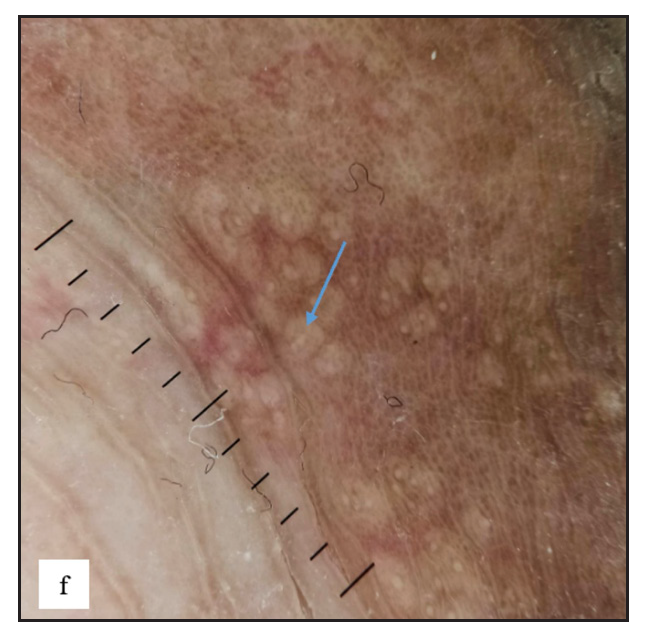
Fordyce spotsFordyce spots were observed in 10 (1.8%) cases. Multiple, discrete, whitish-yellow, pinhead-sized barely elevated papules were seen in a grouped fashion over the penile shaft in nine and the prepuce in two cases [Figure 2e]. Extragenital involvement of lips and buccal mucosa was noted in three cases. Dermoscopy showed white to yellow ovoid structures with central opacity in all cases which were occasionally surrounded by straight vessels (10%) [Figure 2f].
Export to PPT
Export to PPT
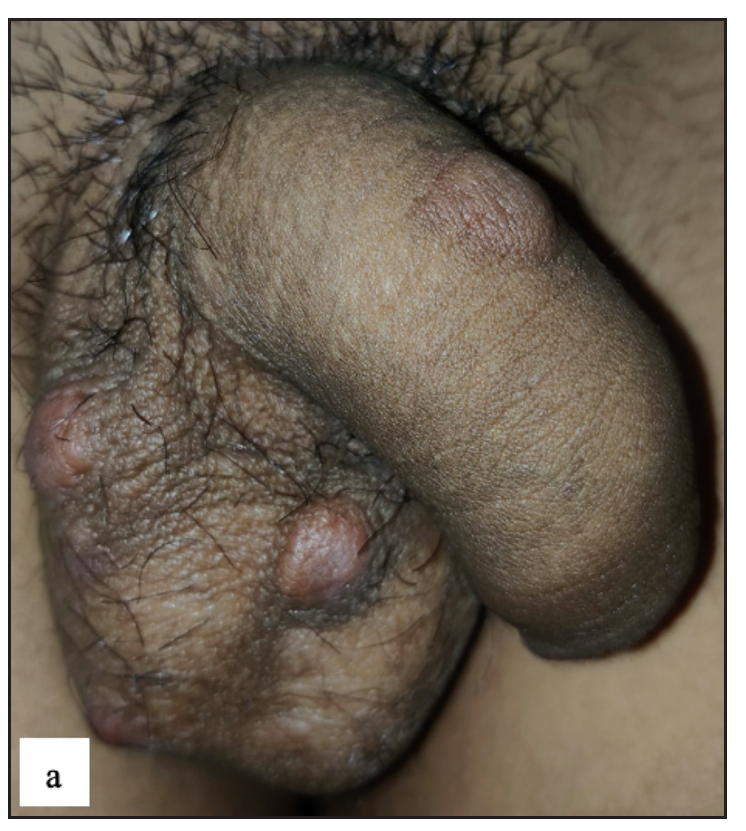
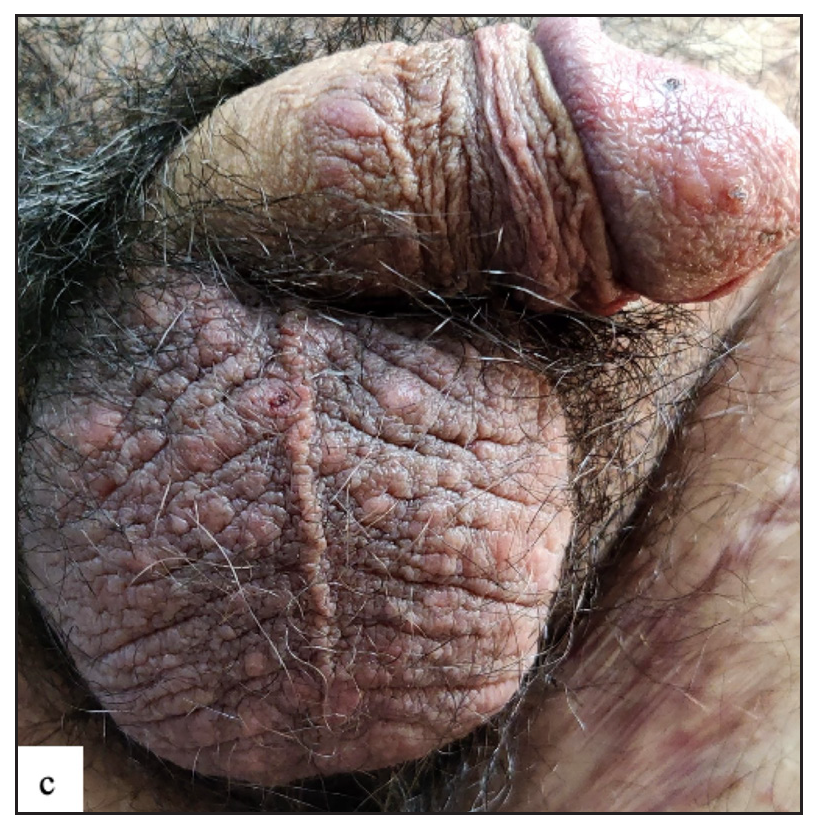
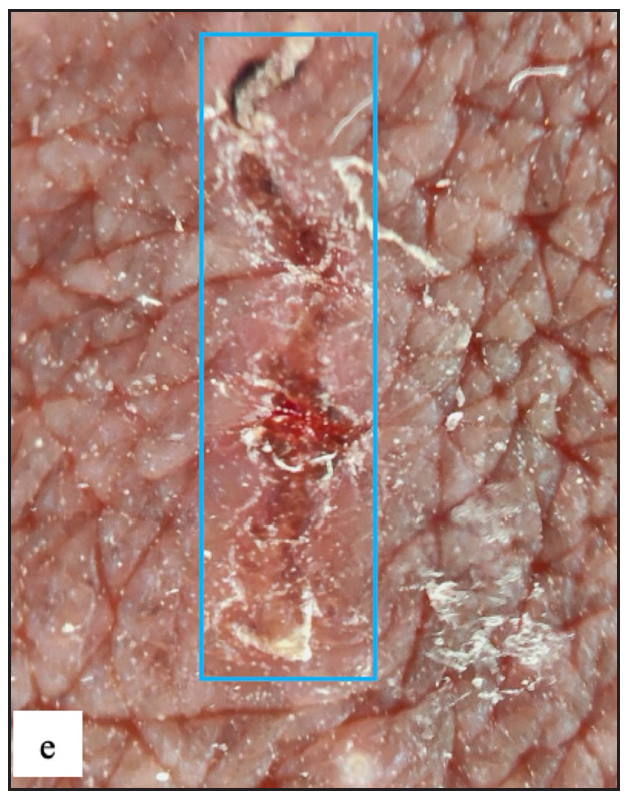
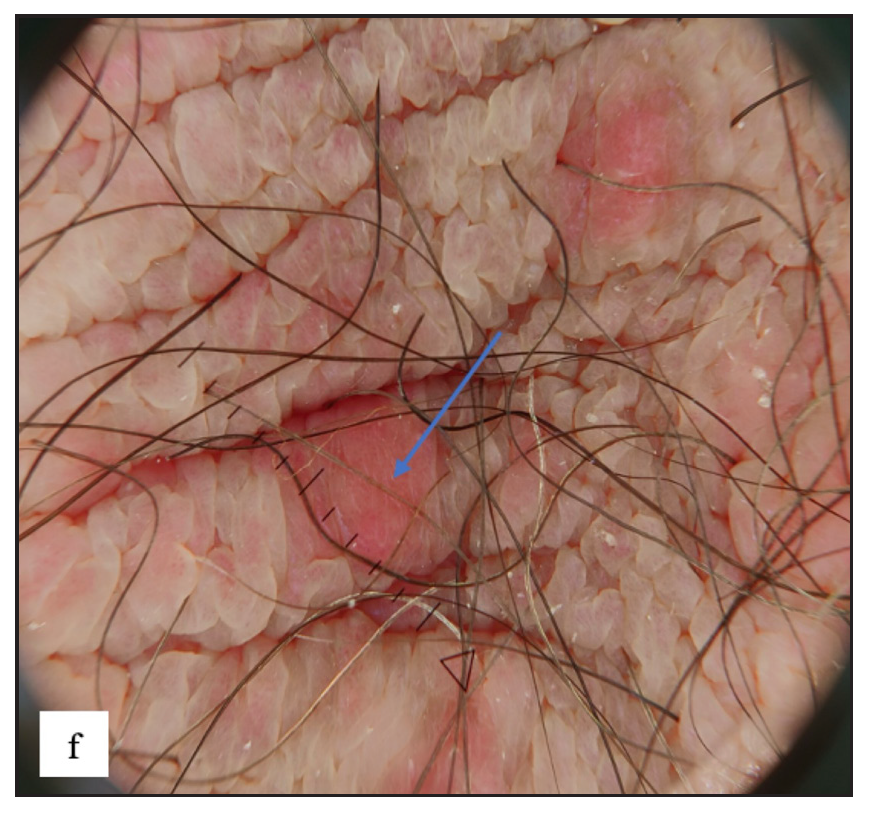
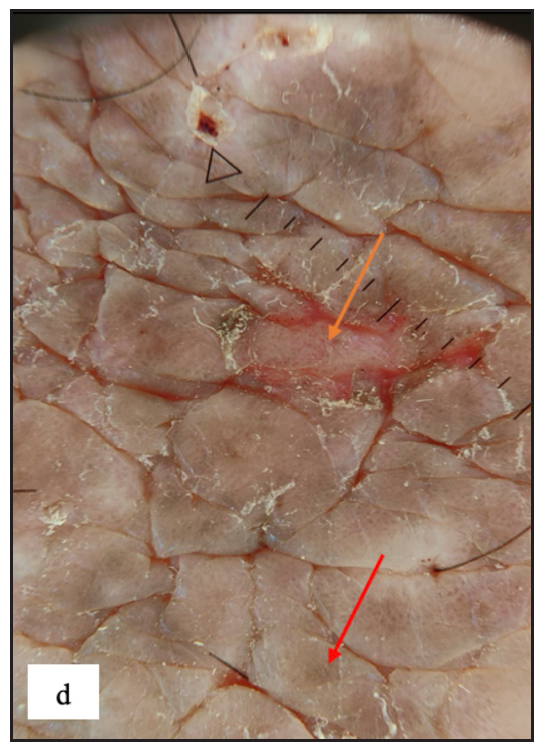
ScabiesScabies was the most common disease noted in the study, constituting 97 (17.6%) of cases. Ninety-five (97.9%) of these cases were male. Twenty-four (24.7%) of the cases had isolated genital involvement while the rest had extragenital lesions also. The most common site involved in males was the scrotum (87, 91.5%) while labia majora was the most common site involved in females (2, 100%). The most common morphology found was discrete erythematous 2–4 mm sized papules in 96 (99%) cases [Figure 3a, 3b and 3c]. Dermoscopic examination revealed red structureless areas in 89 (91.8%) cases with white scales in 62 (63.9%). Serpiginous tracts which are specific to scabies were found only in 20 (20.6%) cases [Figure 3d, 3e, 3f and Table 2].
Export to PPT

Export to PPT
Export to PPT

Export to PPT
Export to PPT
Export to PPT
Table 2: Dermoscopic examination of the most commonly found non-venereal genital dermatoses
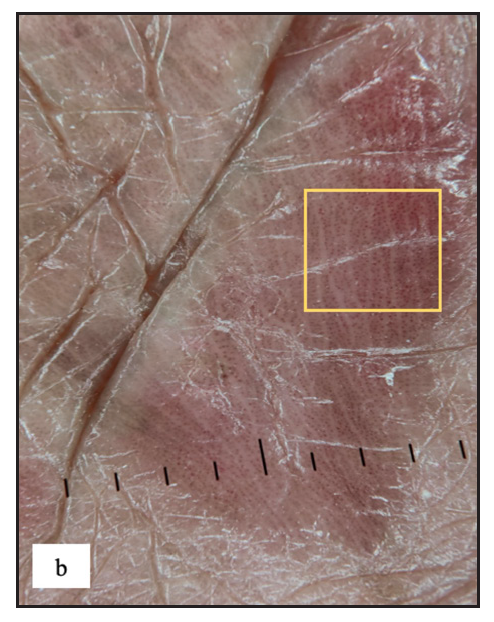
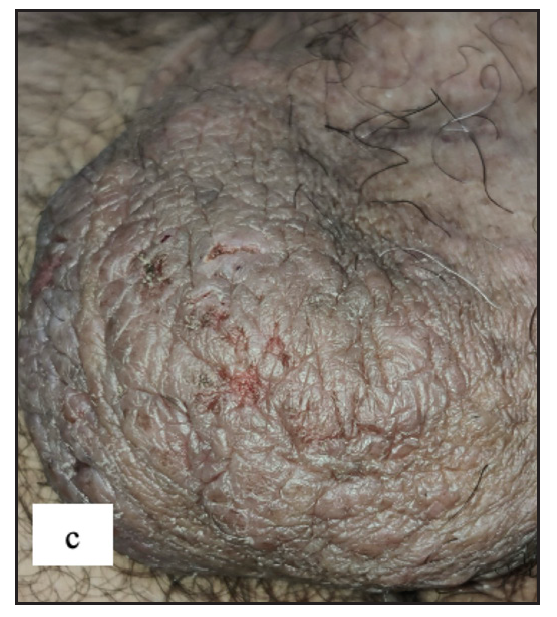
Characteristics Frequency Percentage Genital scabies (n = 97) Red structureless area 89 91.8 White scales 62 63.9 Dotted vessels 51 52.6 Patchy scales 38 39.2 Haemorrhagic crusts 35 36.1 Brown dots and globules 34 35.1 Central scales 33 34 Serpiginous tracts 20 20.6 Yellow crusts 16 16.5 Yellow scales 13 13.4 Peripheral scales 11 11.3 Background erythema 9 9.3 Brown scales 5 5.2 Erosions 5 5.2 Straight vessels 1 1 Wavy vessels 1 1 Genital psoriasis (n = 33) Background erythema 32 97 Regular dotted vessels 28 84.8 White scales 27 81.8 Brown dots 15 45.5 Yellow scales 6 18.2 Brown globules 4 12.1 Genital lichen planus (n = 39) Brown-blue dots 31 79.5 Purple structureless areas 23 59 Wickham striae 20 51.3 White scales 12 30.8 Brown globules 9 23.1 Grey reticular lines 6 15.4 Brown peripheral rim 3 7.7 Yellow scales 2 5.1 Grey peripheral rim 2 5.1 Red peripheral rim 2 5.1 Grey radial lines 1 2.6 Grey parallel lines 1 2.6 Dotted vessels 1 2.6 Lichen sclerosus (n = 43) White structureless areas 43 100 Background erythema 35 81.3 Curved vessels 21 48.8 Looped vessels 15 34.9 Dotted vessels 14 32.6 Wavy vessels 7 16.3 Straight vessels 5 11.6 Branched vessels 5 11.6 White scales 4 9.3 Erosions 4 9.3 Brown dots 1 2.3 Genital vitiligo (n = 54) White structureless areas 53 98.1 Absent pigment network 53 98.1 Telangiectasia 18 33.4 Background erythema 17 31.5 Perifollicular pigmentation 12 22.2 Reduced pigment network 9 16.7 Marginal pigmentation 6 11.1 White globules 5 9.3 Reverse pigment network 5 9.3 White scales 2 5.6 Brown background 2 3.7 Microkoebnerisation 15 27.7 Leukotrichia 12 22.2 Starburst pattern 11 20.3 Polka dot sign 6 11.1 Zoon’s balanitis (n = 20) Dotted vessels 20 100 Reddish orange structureless areas 19 95 Curved vessels 19 95 Looped vessels 15 75 Wavy vessels 15 75 Cayenne pepper appearance 13 65 Red globules 9 45 Straight vessels 9 45 Branched vessels 7 35 Spiral vessels 5 25 Coiled vessels 1 5 PsoriasisPsoriasis involving genitalia was seen in 33 (6%) of cases. Majority 25 (75.8%) were males. Twenty-six (78.8%) patients had extragenital involvement. Scrotum (19, 76%) in males and labia majora (7, 87.5%) in females were commonly involved. On clinical examination, erythematous plaques (28, 84.8%) with scaling (25, 75.8%) were the most common findings [Figure 4a]. On dermoscopy, most lesions showed regularly arranged dotted vessels in 28 (84.8%) over an erythematous background in 32 (97%) with white scales in 27 (81.8%) cases [Figure 4b and Table 2].

Export to PPT
Export to PPT
Lichen simplex chronicusLichen simplex chronicus (LSC) was noted in 43 (7.8%) cases. Thirty-three (76.7%) of them were male. Scrotum in males and labia majora in females were the only sites involved Figure 4c]. On dermoscopy, LSC was characterised by exaggerated skin markings in 40 (93%) and white scales in 37 (86%) cases [Figure 4d].
Export to PPT
Export to PPT
Scrotal dermatitisTwenty-two (4%) patients had scrotal dermatitis. Scrotal dermatitis is typically seen as a disorder comparable to contact dermatitis that occurs elsewhere and is not recognised as a distinct disease entity. Some authors categorise the condition as a distinct disease entity due to its multifactorial aetiology. Scrotal dermatitis is characterised by severe itching, erythema, scaling and lichenification of the scrotal skin. It can be caused by a variety of factors, the most common of which are psychological stress and either allergic or irritant contact dermatitis. Because of the extensive use of antiseptics and over-the-counter topical treatments, this condition is very frequent in modern culture. Persistent scrotal skin inflammation induces the production of numerous inflammatory mediators or proteolytic agents, resulting in pruritus and a vicious itch-scratch cycle that eventually results in an erythematous or lichenified scrotum, sometimes known as a ‘wash leather scrotum’.4 The most common morphology was erythematous plaques seen in 22 (100%) cases followed by scales in 17 (77.3%) cases [Figure 4e]. Background erythema in 16 (72.7%) with white scales in 17 (77.3%)cases were the most common findings seen in dermoscopy. Irregular dotted vessels were seen in 11 (50%) cases [Figure 4f].

Export to PPT

Export to PPT
Lichen planusGenital lichen planus was present in 39 (7.1%) of all cases. The majority of patients were men (94.9%). Lesions were present over the penile shaft in 22 (59.4%) and glans penis in 21 (56.7%) males. Violaceous papules were noted in 27 (69.2%), plaques in 10 (25.6%) [Figure 5a and 5b] and hyperpigmented macules in 14 (35.9%) cases. Mostly, papules were round in shape in 31 (79.5%) but annular lichen planus was also found in 10 (25.6%) [Figure 5c] and erosive variant in 2 (5.1%) patients [Figure 5d]. Extragenital lesions were noted in 19 (48.7%) patients. The most common findings noted in dermoscopy were blue-brown dots (31, 79.5%) and purple structureless areas (23, 59%). Wickham striae were noted in 20 (51.3%) cases [Figure 5e, 5f, 5g, and Table 2].

留言 (0)