Osteoporosis is a systemic metabolic bone disease characterized by pain, bone deformation, and susceptibility to fractures. Osteoporotic patients are often afflicted with comorbid conditions, such as cardiovascular diseases, diabetes, and neurodegenerative disorders. Over the past two decades, the global incidence of osteoporosis has reached approximately 18.3%. Proximal humerus fractures are the second most common upper-limb fractures after distal radius fractures, accounting for 10% of all fractures in individuals over 65 years of age and 17.5% of osteoporotic fractures in postmenopausal women over 50 years old (1). With an aging global population, the incidence of proximal humerus fractures is increasing and is projected to triple by 2030 (2).The severity of displacement and the likelihood of complications increase with age, particularly in large-displacement three- or four-part fractures. Such fractures result in elevated medical costs, functional impairment, and reduced quality of life. Conservative treatment may suffice for fractures with minimal displacement; however, for complex fractures, conservative management can lead to malunion, nonunion, stiffness, and persistent pain (3, 4).Current treatments for osteoporosis include calcium, vitamin D, bisphosphonates (e.g., alendronate and risedronate), and alternative therapies such as traditional Chinese medicine and massage. Surgical techniques, including percutaneous fixation, intramedullary nailing, and joint replacement, have been developed to address complex fractures (5). Open reduction and internal fixation using locked plates has gained widespread acceptance, yielding favorable clinical outcomes. However, complications such as screw loosening, humeral head necrosis, and fixation failure remain prevalent, particularly in older adult patients with poor bone quality, with complication rates as high as 34% (6, 7).To address these challenges, recent research has explored methods to enhance screw-bone interface strength, such as intramedullary fibular bracing and the use of bone cement (8, 9). This study retrospectively analyzed the clinical data of older adult patients treated with PHILOS plates combined with calcium sulfate, PHILOS plates alone, and hemi-shoulder joint replacement. The aim was to compare the efficacy and complication rates among these three treatment modalities.
2 Materials and methods 2.1 Inclusion and exclusion criteriaInclusion criteria: (i) According to the Neer classification, the proximal humerus fractures were either three-part or four-part fractures. (ii) Patients with osteoporotic fractures of the proximal humerus treated in our hospital from February 2018–August 2021. (iii) Unilateral fresh limb fracture, with no disease of the shoulder joint before injury. (iv) The patient and his or her family agree on the treatment plan. (v) Complete follow-up of clinical data.
Exclusion criteria: (i) Pathological fracture. (ii) Open fracture. (iii) Multiple fractures of the same limb, with obvious dysfunction of the shoulder joint before injury. (iv) Patients and their families refuse surgery. (v) Incomplete follow-up of clinical data.
2.2 General informationA total of 48 patients meeting the inclusion criteria were analyzed (18 males, 30 females), with a mean age of (68.6 ± 5.8) years (range: 60–81 years). The injuries were primarily caused by falls, impacts, and motor vehicle accidents. x-ray, CT, and MRI examinations were performed preoperatively. All procedures were completed within 7 days post-injury by the same surgical team. The patients were divided into three groups: Group A: PHILOS plate combined with calcium sulfate injection (16 cases: 10 three-part, 6 four-part fractures). Group B: PHILOS plate alone (16 cases: 9 three-part, 7 four-part fractures). Group C: Hemi-shoulder joint replacement (16 cases: 7 three-part, 9 four-part fractures).
2.3 Surgical techniquesAll eligible patients underwent general anesthesia, were placed in the supine position with the shoulder on the affected side elevated. Routine disinfection was performed in group A and group B, and iodine tincture disinfection was done in group C and for all surgical participants. Sterile sheets and films were applied in the surgical area.
Group A: The surgical approach was the deltoid and pectoralis major approach. Blunt separation was used to expose the cephalic vein, with emphasis on protection to avoid damage to the axillary nerve and the long head tendon of the biceps. The insertion of the deltoid muscle was partially severed, and the broken end of the fracture was fully exposed. The fracture was reduced and temporarily fixed with the cross of a Kirschner's needle. The locking plate was placed behind the intertubercular sulcus and 0.5 cm below the apex of the greater tubercle. A lag screw was temporarily fixed in a non-locking hole. C-arm X-ray was used to determine the appropriate height and position of the steel plate. Then, the locking screw and the humerus talus screw of sufficient length were screwed in respectively. The middle nail hole of the locking plate was chosen, and the prepared calcium sulfate was evenly injected into the humerus head and the defect of the humerus talus using a calcium sulfate injector. At the same time, the injection was pumped back into the injector until it could not be injected. Finally, the position of the steel plate, the length of the screw, and the filling of calcium sulfate were re-examined under the C-arm. The rotator cuff was repaired by suture. The rotator cuff was rinsed repeatedly, and the passive shoulder joint had good motion. A drainage tube was placed under the skin, and the incision was closed layer by layer (Figure 1).

Figure 1. Follow-up imaging of comminuted fracture of proximal left humerus. (A,B) Preoperative X-rays showed fracture displacement, humeral head inversion, and displacement of large and small tubercles. (C,D) Preoperative CT scan of the left shoulder showed fracture inversion, separation and displacement of large and small nodules. (E,F) Postoperative x-rays showed that the fracture was well reduced and the humerus head was adequately filled with calcium sulfate injection. (G,H) Postoperative shoulder joint CT showed that injection of calcium sulfate filled the humerus skull defect adequately. (I,J) At the last follow-up, the fracture healed and calcium sulfate was completely degraded and absorbed.
Group B: The deltoid-pectoralis major space approach was used to incise the skin and bluntly separate it to the deep. The head vein and the long head tendon of the biceps were protected, and the deltoid-muscle insertion was bluntly peeled to fully expose the humerus head and fracture block. The humerus head and fracture block were fully exposed, and the humerus head and fracture block were reduced under direct vision, and a Kirschner's needle was used for temporary fixation. The locking plate was placed in the anterolateral internodal groove at 0.5 cm. The position of the plate was determined by C-arm fluoroscopy. Locking screws of appropriate length were screwed in turn. The fractures were re-reduced by fluoroscopy, and the steel plate height was appropriate. The rotator cuff and soft tissue were sutured, hemostasis was fully achieved, drainage tubes were thoroughly rinsed, and the incision was sutured.
Group C: The deltoid-pectoralis space approach was taken to protect the head vein, axillary nerve, and rotator cuff tissue, fully expose the proximal end of the humerus, mark the humerus osteotomy plane and perform osteotomy, expand the medullary canal, irrigate, reduce the prosthesis test model, locate the X-ray prosthesis test model, determine the prosthesis height and retrograde angle of the humerus head, remove the test model, fill the medullary cavity with bone cement, and select the appropriate prosthesis for installation. After the bone cement hardened and the shoulder joint was reduced, the large and small nodules were reconstructed, the rotator cuff was repaired, full hemostasis was achieved, and the incision was closed.
A 68- year-old female patient suffered a comminuted fracture of the proximal left humerus (Neer type IV) caused by a fall. (A, B) Preoperative anterolateral X-rays of the left shoulder showed a proximal humerus fracture, varus involvement of the fracture in the medial humerus talus, displacement of large and small tubercle fractures, and an increased retrograde humerus head; (C, D) Left-shoulder CT and 3D reconstruction clearly showed fracture inversion, involvement of the humerus talus, prominence, separation, and displacement of the large and small tubercles; (E, F) Post-operative X-ray results showed anatomic reduction of the fractures, correction of the varus, support of the humerus talus screw for varus, and the injectable calcium sulfate fully filled the humerus head and the defect of the humerus talus; (G, H) Sagittal and coronal CT images of the proximal humerus of the left shoulder after surgery showed sufficient calcium sulfate implantation in the humerus head and the bone defect within the humerus talus, and the screws were evenly surrounded by calcium sulfate. (I, J) Three months after surgery, the left shoulder was re-examined in the anterolateral position, showing fracture healing, complete degradation of calcium sulfate, and fusion of normal bone tissue.
2.4 Postoperative management and evaluation of curative effectAfter the operation, antibiotics were routinely administered for 3 days to prevent infection. In group A and group B, the shoulder and elbow straps were suspended and fixed. Passive pendulum—type functional exercises were performed 2 weeks after the operation to avoid shoulder joint adhesion. Passive abduction, forward flexion, and backward extension activities were started 3 weeks after the operation, and full shoulder joint activities were gradually carried out 4–6 weeks after the operation. In group C, an abduction brace was fixed. To avoid the rotator cuff pulling the greater tubercle and resulting in greater tubercle displacement, passive functional exercises were performed 2 weeks after the surgery, and shoulder joint functional exercises were gradually started 3 weeks after the surgery. Anterolateral X-rays of the shoulder joint were periodically reviewed at 2, 4, 8, 12, 6, and 12 weeks after the surgery to evaluate fracture healing and internal fixation.
The operative time, blood loss, incision length, and surgical cost of the three groups were compared, and the shoulder joint motion at the last follow-up was recorded. The shoulder joint function was evaluated using the American Shoulder and Elbow Surgical Score (ASES), the visual analogue pain score (VAS), the University of California Shoulder Joint Score (UCLA), and the Brief Shoulder Joint Function Test score (SST).
2.5 Statistical analysisStatistical analysis was performed using IBM SPSS 26.0 software. The Shapiro-Wilk test was applied to assess the normality of the data distribution. Measurement data conforming to normality and homogeneity of variance were expressed as mean ± standard deviation (x ± s). The chi-square (χ²) test was used to compare categorical data. A P-value of <0.05 was considered statistically significant.
3 Resultshere were no statistically significant differences in gender, age, injured limb, time to surgery, or Neer classification among Groups A, B, and C (P > 0.05), confirming comparability (Table 1). All patients underwent surgery successfully, with primary healing of surgical incisions and no incidences of infection. The mean follow-up duration was (16.5 ± 2.6) months.
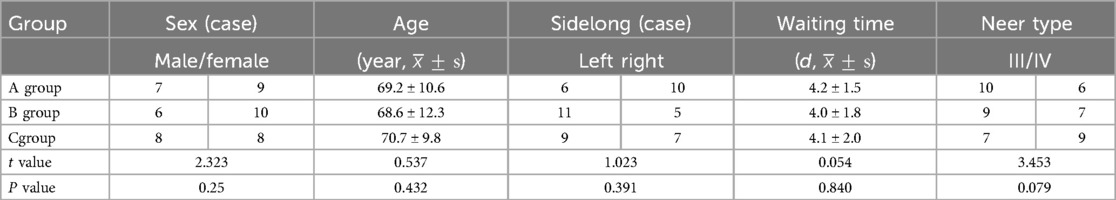
Table 1. Basic data of three groups of patients (n = 16).
Patients in group A, group B and group C had no statistical significance in terms of operation time, blood loss and incision length (P > 0.05), but the operation cost in group C was higher than that in the other two groups, and the pairings were statistically significant (P < 0.05) (Table 2).
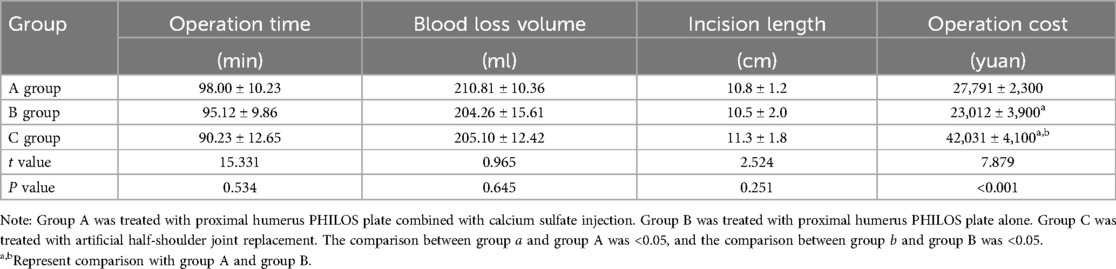
Table 2. Comparison of operation time, blood loss, incision length and operation cost among three groups (x ± s, n = 16).
There was no significant difference in anterior flexion and external rotation of shoulder between groups A, B and C at the last follow-up (P > 0.05). Outreaching activity: The difference between group A and group C was statistically significant (P < 0.05) (Table 3).
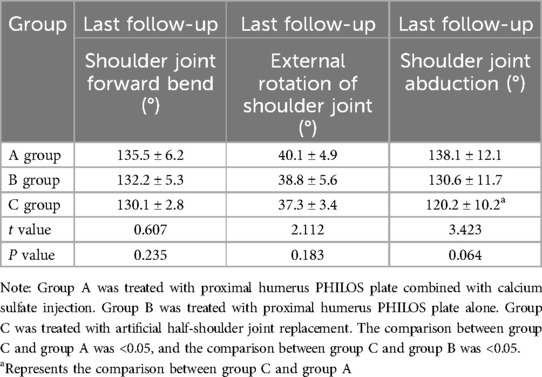
Table 3. Comparison of shoulder joint flexion, external rotation and abduction motion between the three groups to the last follow-up (x ± s, n = 16).
At the last follow-up, there were no significant differences in ASES score, VAS pain score, UCLA score and SST score among the three groups (P > 0.05). (Table 4) Complications of A, B, and C: 1 case in group A showed extravasation of injected calcium sulfate, which was absorbed by itself during follow-up. In group B, 1 screw was cut out, 1 screw was inverted, and 1 screw was loosened. In group C, there were 2 cases of macrotuberous absorption and 2 cases of joint stiffness. The difference among the three groups was statistically significant (P < 0.05).
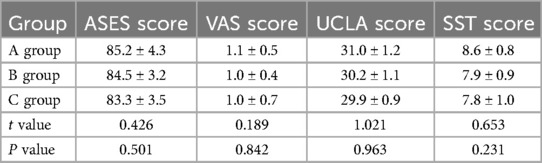
Table 4. Comparison of ASES scores, VAS pain scores, UCLA scores and SST scores in the three groups from the last follow-up (x ± s, n = 16).
4 DiscussionTreatment options for proximal humerus fractures in older adults, especially osteoporotic fractures, are challenging, as these fractures account for 6% of adult fractures and their incidence continues to increase with age, as the majority of the population occurs over the age of 65 (10). At present, osteoporotic fractures of the proximal humerus in the older adult have always been a difficult problem for orthopedic surgeons in clinical practice, because fractures of the proximal humerus can lead to severe pain and loss of function of the shoulder joint, which seriously affects the quality of life. The treatment options include conservative treatment, open reduction and internal fixation, joint replacement, etc (11). However, there is no consensus on the treatment of 3 or 4 partial fractures of the proximal humerus, and each option has its own advantages and disadvantages, so there is a lack of management consistency in the selection of treatment options. Regardless of the treatment, the primary goal for this fracture is to promote uncomplicated bone healing to re-establish a painless mobility, stability and function of the shoulder joint.
Proximal humerus locking plate (PHILOS) is an anatomical locking plate designed by AO/OTA to improve functional outcomes, especially in patients with osteoporosis. The locking capability of the screw provides better locking of osteoporotic bone to the plate, gives the structure angular stability, and maintains postoperative reduction during early functional rehabilitation, avoiding joint stiffness. It has become the implant of choice for internal fixation of proximal humerus fractures (12). Despite this, the incidence of complications in open reduction and internal fixation is still high, Thanasas et al. (13). Results showed that lock-plate internal fixation was associated with fracture displacement (12.2%), screw removal (11.6%), fracture nonunion (13%), and avascular necrosis (7.9%). Therefore, people gradually realized the importance of these complications, and treatment strategies began to focus on the internal structure of the humerus head, such as bone cement reinforcement and bone graft support to avoid reducing the incidence of complications (14, 15). Schultz et al. (16) applied PHILOS plate combined with fibula support to treat proximal humeral fracture patients with medial talar column fracture, and this method showed that it could reduce internal fixation complications and obtain good clinical results. However, for patients with varus angulation, two - and three-part proximal humeral fractures, there was no statistical significance in the clinical effect of the addition of a fibula brace vs. the absence of a fibula brace, and for older adult patients with osteoporotic fractures of the proximal humerus, the use of an autofibula brace, if used, was not statistically significant. Older adult patients have poor bone conditions and increased surgical trauma, so the clinical promotion of this treatment plan has certain limitations (17). Researchers began to fill the bone defect by implanting filler into the humerus head to increase the screw grip and accelerate bone healing (18). The commonly used filler bone cement has a good biological type advantage. VanVeelen et al. (19) used hollow bone cement to strengthen screw fixation in osteoporotic fractures of the proximal humerus, and the results showed that it could reduce the complications of internal fixation failure such as screw loosening and removal. However, the temperature of PMMA during the polymerization stage can be as high as 100°C, which may lead to bone and cartilage necrosis (20). In view of the above situation, more solutions should be sought. It has been reported that shoulder joint replacement for osteoporotic fractures of the proximal humerus can achieve good clinical efficacy and effectively relieve the pain symptoms of patients, but the prognosis is also different. If the greater tubercle can achieve anatomic reduction and healing, good function can be achieved. The incidence of non-union of the greater tubercle is higher in older adult patients, which directly affects shoulder joint function and correspondingly reduces shoulder joint score (21, 22).
In the face of internal bone defects in the humerus head, resulting in decreased screw control, autologous cancellous bone transplantation is the gold standard, but there are limitations such as donor site morbidity and insufficient filling. Currently, there are many substitute bone transplantation materials, each with its own shortcomings, limiting clinical application. Calcium sulfate is an early bone graft material with good self-consolidation, shape ability, and degradation absorption rate close to the new bone formation rate. During absorption, a large number of bone trabeculae and bone marrow are formed and connected to each other to form a structure similar to normal bone tissue. The remaining calcium sulfate continues to play the role of bone conduction scaffold, and the residual or exudated calcium sulfate in the joint space is absorbed within 15 days. It has advantages over other bone graft materials (23, 24). Based on the above advantages of calcium sulfate, our team used PHILOS combined with injectable calcium sulfate to treat older adult patients with osteoporotic fractures of the proximal humerus. Calcium sulfate was injected into the bone defect of the humerus head to increase the bone mass in the head, improve the screw holding ability, and finally calcium sulfate degradation fused with normal bone tissue. Satisfactory clinical efficacy was achieved through clinical follow-up. It provides a new treatment method for senile proximal humerus osteoporotic fracture.
5 ConclusionsIn summary, for the treatment of older adult proximal humerus osteoporotic fractures, the proximal humerus locking plate (PHILOS) combined with calcium sulfate injection, the simple proximal humerus locking plate, and artificial half-shoulder replacement can effectively relieve pain and restore joint function. However, the proximal humerus locking plate (PHILOS) combined with calcium sulfate injection has fewer complications, costs less than artificial half-shoulder replacement, and has better abductor motion than joint replacement. Moreover, its clinical efficacy is reliable, making it one of the effective options for older adult proximal humerus osteoporotic fractures. Nevertheless, in clinical practice, the choice of surgery requires clinicians to make a comprehensive consideration based on the fracture type, surgical indications, and the individual patient.
6 LimitationsThere are some limitations in this study: (i) The number of studies and patients is small, so more sample size needs to be included; (ii) All the included samples were admitted to our hospital and were single-center studies, so the results may be biased and need to be verified by large-sample multi-center studies; (iii) The follow-up time is short, and long-term follow-up is needed to observe the clinical effect; (iv) This study is a retrospective case-control study, and there may be some selective bias in the selection of cases, which needs to be verified by a large sample randomized controlled study.
Data availability statementThe datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statementThe studies involving humans were approved by the Ethics Committee of the Affiliated Zhongshan Hospital of Dalian University. The studies were conducted in accordance with local legislation and institutional requirements. Participants provided their written informed consent to participate in this study.
Author contributionsZW: Formal Analysis, Conceptualization, Writing – original draft. TW: Funding acquisition, Writing – original draft. SQ: Data curation, Writing – original draft. JW: Writing – original draft.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. Interdisciplinary project of dalian university, Item number: DLUXK−2024-YB-009.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Chu SP, Kelsey JL, Keegan TH, Sternfeld B, Prill M, Quesenberry CP, et al. Risk factors for proximal humerus fracture. Am J Epidemiol. (2004) 160:360–7. doi: 10.1093/aje/kwh224
PubMed Abstract | Crossref Full Text | Google Scholar
2. Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. (2006) 442:87–92. doi: 10.1097/01.blo.0000194672.79634.78
PubMed Abstract | Crossref Full Text | Google Scholar
3. Bergdahl C, Ekholm C, Wennergren D, Nilsson F, Möller M. Epidemiology and patho-anatomical pattern of 2,011 humeral fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. (2016) 17:159. doi: 10.1186/s12891-016-1009-8
PubMed Abstract | Crossref Full Text | Google Scholar
4. Lopiz Y, Alcobía-Díaz B, Galán-Olleros M, García-Fernández C, Picado AL, Marco F. Reverse shoulder arthroplasty versus nonoperative treatment for 3- or 4-part proximal humeral fractures in older adult patients: a prospective randomized controlled trial. J Shoulder Andelbow Surg. (2019) 28:2259–71. doi: 10.1016/j.jse.2019.06.024
Crossref Full Text | Google Scholar
5. Lander ST, Mahmood B, Maceroli MA, Byrd J, Elfar JC, Ketz JP, et al. Mortality rates of humerus fractures in the elderly: does surgical treatment matter? J Orthop Trauma. (2019) 33:361–5. doi: 10.1097/BOT.0000000000001449
PubMed Abstract | Crossref Full Text | Google Scholar
6. Sudkamp N, Bayer J, Hepp P, Voigt C, Oestern H, Kaab M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. (2009) 91:1320–8. doi: 10.2106/JBJS.H.00006
PubMed Abstract | Crossref Full Text | Google Scholar
7. Jost B, Spross C, Grehn H, Gerber C. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome. J Shoulder Elbow Surg. (2013) 22:542–9. doi: 10.1016/j.jse.2012.06.008
PubMed Abstract | Crossref Full Text | Google Scholar
8. Schliemann B, Seifert R, Rosslenbroich SB, Theisen C, Wahnert D, Raschke MJ, et al. Screw augmentation reduces motion at the bone-implant interface: a biomechanical study of locking plate fixation of proximal humeral fractures. J Shoulder Elbow Surg. (2015) 24:1968–73. doi: 10.1016/j.jse.2015.06.028
PubMed Abstract | Crossref Full Text | Google Scholar
9. Sheng N, Wang Q, Chu G, Wang L, Cheng M, Weng Z, et al. Cancellous bone allograft is comparable to fibular strut allograft for augmentation in three- or four-part proximal humeral fractures. J Shoulder Elbow Surg. (2021) 30:2065–72. doi: 10.1016/j.jse.2020.11.029
PubMed Abstract | Crossref Full Text | Google Scholar
10. Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res. (2012) 64:407–14. doi: 10.1002/acr.21563
PubMed Abstract | Crossref Full Text | Google Scholar
11. Kyriakides PW, Schultz BJ, Egol K, Leucht P. The fragility and reverse fragility indices of proximal humerus fracture randomized controlled trials: a systematic review. Eur J Trauma Emerg Surg. (2022) 48:4545–52. doi: 10.1007/s00068-021-01684-2
PubMed Abstract | Crossref Full Text | Google Scholar
12. Ricchetti ET, DeMola PM, Roman D, Abboud JA. The use of pre contoured humeral locking plates in the management of displaced proximal humerus fracture. J Am Acad Orthop Surg. (2009) 17:582–90. doi: 10.5435/00124635-200909000-00005
PubMed Abstract | Crossref Full Text | Google Scholar
13. Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plate: a systematic review. J Shoulder Elbow Surg. (2009) 18:837–44. doi: 10.1016/j.jse.2009.06.004
PubMed Abstract | Crossref Full Text | Google Scholar
14. Foruria AM, Martinez-Catalan N, Valencia M, Morcillo D, Calvo E. Proximal humeral fracture locking plate fixation with anatomic reduction, and a short-and-cemented-screws configuration, dramatically reduces the implant related failure rate in older adult patients. JSES Int. (2021) 5:992–1000. doi: 10.1016/j.jseint.2021.06.004
PubMed Abstract | Crossref Full Text | Google Scholar
15. Kim D-S, Lee D-H, Chun Y-M, Shin S-J. Which additional augmented fixation procedure decreases surgical failure after proximal humeral fracture with medial comminution: fibular allograft or inferomedial screws?. J. Shoulder Elb Surg. (2018) 27:1852–8. doi: 10.1016/j.jse.2018.03.020
PubMed Abstract | Crossref Full Text | Google Scholar
16. Schultz BJ, Lowe DT, Egol KA, Zuckerman LD. Shoulder hemiarthroplasty for proximal humerus fracture. J Orthop Trauma. (2021) 35(Suppl2):S3–4. doi: 10.1097/BOT.0000000000002158
PubMed Abstract | Crossref Full Text | Google Scholar
17. Shu Y, Chen MJ, Yu WG, Ge Z, Hu H, Zhang XC, et al. PHILOS plate plusoblique insertion of autologous fibula for 2-part proximal humerus fractures with medial column disruption: aretrospective study. Geriatr Orthop Surg Rehabil. (2021) 12:2151459321992666. doi: 10.1177/2151459321992666
PubMed Abstract | Crossref Full Text | Google Scholar
18. Belkoff SM, Molloy S. Temperature measurement during poly-merization of poly methylmethacrylate cement used for verte-broplasty. Spine (Phila Pa 1976). (2003) 28:1555–9.12865844
PubMed Abstract | Google Scholar
19. van Veelen NM, Beeres FJ, Link BC, Babst R. Augmentation in the treatment of proximal humeral and femoral fractures. Unfallchirurg. (2022) 125(6):436–42. doi: 10.1007/s00113-022-01172-1
Crossref Full Text | Google Scholar
21. Antuña SA, Sperling JW, Cofield RH. Shoulder hemiarthroplasty for acute fractures of the proximal humerus: a minimum five-year follow-up. J Shoulder Elbow Surg. (2008) 17:202–9. doi: 10.1016/j.jse.2007.06.025
PubMed Abstract | Crossref Full Text | Google Scholar
22. Antonios T, Bakti N, Phadkhe A, Gulihar A, Singh B. Outcomes following arthroplasty for proximal humeral fractures. J Clin Orthop Trauma. (2020) 11(Suppl1):S31–6. doi: 10.1016/j.jcot.2019.07.008
PubMed Abstract | Crossref Full Text | Google Scholar
23. Turner TM, Urban RM, Gitelis S, Haggard WO, Richelsoph K. Resorption evaluation of a large bolus of calcium sulfate in a canine medullary defect. Orthopedics. (2003) 26(5 Suppl):s577–9. doi: 10.3928/0147-7447-20030502-10
留言 (0)