Increasing antimicrobial resistance (AMR) hastens the arrival of the post-antibiotic era, which is a concern necessitating a range of different activities (1, 2). Extensive misuse of antibiotics contributes to increasing AMR, potentially reversing decades of medical accomplishments (3, 4). In 2021, it was estimated globally, there were 1.14 million deaths due to AMR, with 1 in 5 deaths occurring in children under 5 years of age, with the highest rates of AMR in low- and middle-income countries (LMICs) (5, 6). This is set to rise to 8.22 million deaths by 2050 alongside considerable morbidity, combined with an annual economic loss of approximately $US1 trillion unless addressed (6–8).
Antibiotics are the most commonly prescribed medicines in the pediatric population in both community and hospital settings with potentially inappropriate usage, with consumption increasing 46% between 2000 and 2018 in children under 5 years of age (9, 10). Antibiotic consumption also appreciably increased among sick children under the age of 5 in LMICs between 2005 and 2017, greatest in South-East Asia (11). This is a concern increasing both AMR as well as adverse events (12), with rapidly increasing resistant organisms, including gram-negative bacilli and Staphylococcus aureus (13). The pediatric population is particularly vulnerable to the consequences of AMR, resulting in increasing morbidity and mortality (12, 14, 15). Addressing this is a critical issue to reach the agreed Sustainable Development Goal to reduce newborn mortality, with Pakistan a key country with high mortality rates compared to a number of other LMICs (16, 17). Moreover, limitations pertaining to eligibility to participate in clinical trials impact optimal data generation and development, potentially enhancing AMR (18).
Concerns with growing rates of AMR and associated consequences have resulted in the instigation of the Global Action Plan (GAP) by the World Health Organization (WHO) to tackle AMR, leading to the development of National Action Plans (NAPs) emanating from the GAP also mimic objectives laid out in the latter (19, 20). However, there have been concerns with the implementation of NAPs, including both personnel and resource issues, as seen in Pakistan and other LMICs (21–23). The WHO also developed the Global Antimicrobial Resistance and Use Surveillance (GLASS) in 2017, given the considerable need to track resistance development (24). However, there are considerable challenges with the current report accentuating the limited surveillance capacities of LMICs to record resistance and antibiotic use data (25, 26). The WHO also introduced the AWaRe classification system in 2017, categorizing antibiotics into Access, Watch and Reserve classes (27). The AWaRe framework intends to work as a means of surveillance and act as a stewardship tool (28, 29). Alongside this, the WHO developed its own Point Prevalence Survey (PPS) methodology to document antibiotic use in hospitals, building on Global and ECDC methodologies (30–33). Antibiotic stewardship programs (ASPs) are increasingly seen as an effective means to enhance the appropriate use of antibiotics and reduce AMR and costs (34–36). However, there can be concerns among LMICs to implement ASP due to human resource shortages, diagnostic inadequacies, poor antibiotic use monitoring and surveillance capacity, as well as personnel shortages (37–40). The WHO has also recently provided guidance on undertaking ASPs (41). ASP implementation is particularly important in promoting judicious antibiotic use in the pediatric population, given current challenges (10, 42–44).
Although the NAP Pakistan against AMR has been in effect since 2017, Pakistan acknowledges AMR as a potential threat, whereas the ground realities of the AMR situation are dissent from what was pledged in official documents (23, 45–47) and inadequacies are conspicuous in implementing ASP protocols (48, 49). Pakistan is struggling in the battle against growing bacterial resistance (50–52). There have also been reports of a high prevalence of multi-drug resistance organisms (MDRO) among children in pediatric wards in Pakistan (53). Consequently, there is a need to urgently document current antibiotic utilization patterns among neonates and children in hospitals across Punjab, Pakistan. We are aware of published papers documenting concerns with high use of antibiotics, including high use of “Watch” antibiotics with their greater resistance potential, among the pediatric population in a limited number of hospitals in Pakistan, including tertiary hospitals (54–57). However, there is a need to update this, including evidence from a greater number of hospitals, to inform future ASPs where concerns have been identified. Consequently, the current study intends to expand on previous PPS studies in the pediatric population using the WHO AWaRe classification.
Methods Study design and settingThis point prevalence survey (PPS) was conducted using the standardized Global Point Prevalence Survey on Antimicrobial Consumption and Resistance (Global-PPS) methodology developed by the University of Antwerp. The Anatomical Therapeutic Chemical (ATC) and AWaRe classification system of the WHO were employed to classify the different antibiotics used. Data were collected from 23 wards across 14 hospitals in Punjab, the most populous province of Pakistan, known for its diverse healthcare challenges and significant role in national health outcomes. The hospitals surveyed included a mix of seven secondary and six tertiary care facilities, one specialized cancer hospital, and a combination of ten public and four private sector hospitals. Participation in the survey was voluntary, ensuring that only those institutions willing to engage in this study were included, as mentioned in the Global PPS method.
Sampling and inclusion criteriaPediatric patients (0–18 years) admitted to medical and surgical wards, pediatric intensive care units, and neonatal units at 8:00 a.m. on the day of the survey were included. Patients receiving at least one systemic antibiotic at the time of data collection formed the numerator, while all admitted pediatric patients on the surveyed wards comprised the denominator.
Data collection toolsData collection was conducted using the standardized Global-PPS ward and patient forms. At the ward level, data included the total number of admitted patients, the total number of beds, and type of ward. At the patient level, detailed information was collected on demographics (age and gender), diagnosis and type of infection (e.g., community-acquired or hospital-acquired), the indication for antibiotic use (therapeutic or prophylactic), and the antimicrobial agent(s) prescribed, including the dose, route, and frequency of administration.
Data collection procedureAll pediatric inpatients receiving antimicrobial therapy at 08:00 a.m. were included, and data collection forms were completed for these patients only. All prescribed antimicrobials at the time of the survey were recorded. Patients who were transferred to another ward after 08:00 a.m. were included as part of the initial ward of admittance. Neonates born before 08:00 a.m. on the day of the survey were included. The last prescribed antibiotic was recorded if the prophylaxis or treatment was changed on the day of the survey before or at 08:00 a.m. Surgical wards were not surveyed on a day following a holiday but on other weekdays to capture information about prophylaxis in the last 24 h. Surgical prophylaxis included agents to prevent surgical site infections, and long-acting antibiotics or intermittent treatments given within 24 h before the survey were included. Medical prophylaxis was defined as the use of antibiotics to prevent infections in patients with specific medical conditions. Infections were classified as community-acquired infections (CAIs) if symptoms started less than 48 h from admission to the hospital or were present on admission. Hospital-acquired infections (HAIs) were defined as infections with symptoms starting 48 h after admission. The data collection was conducted by using the Global PPS standardized methodology to ensure consistency and adherence to standards. All available information documented in the Global PPS form was thoroughly collected. The detailed method is described on the Global-PPS website (58). Information included patients' demographics, diagnosis, infection type and prescribed antibiotics details. Data was collected from patients' medical notes and prescribing charts. Additional details from patients' medical case notes were recorded after discussions with nursing staff and physicians, when necessary, especially if crucial data such as antibiotic selection was missing. However, in most cases, only patients' notes were reviewed. The collected data were double-checked for completeness and accuracy to rule out any missing or inconsistent information. There was no direct contact with any patient during the data collection process in line with other PPS studies. Data from each ward being completely surveyed within 1 day to minimize the effect of patient movement between wards and within the hospital. The data was collected in March 2024. Patients' anonymity was maintained throughout the process.
Statistical analysisData were exported from the Global-PPS web application into a Microsoft Excel database for analysis. Statistical analyses were performed using SPSS version 25 (IBM Corporation, Armonk, NY, USA). In this study, we utilized both descriptive and inferential statistical methods to analyze the patterns of antibiotic usage across the AWaRe classifications (Access, Watch, Reserve) under varied clinical settings. Initially, descriptive statistics provided a foundational understanding of the data distribution and characteristics. Further, cross-tabulations were employed to examine the distribution and usage patterns of antibiotics classified as Access, Watch, and Reserve, highlighting the frequency and context of their utilization across different patient groups and departments. Subsequent to the descriptive analysis, logistic regression was applied to more deeply investigate the factors influencing the likelihood of antibiotics being classified under the “Watch” category. This method facilitated the quantification of the impact of various factors, including department type, patient age group, and diagnosis, on the AWaRe classification, allowing for a critical analysis of trends and associations within the data. The “Access” vs. “Watch” ratio was also calculated to assess the relative use given concerns with the increasing use of “Watch” antibiotics in LMICs in recent years, facilitating the identification of targets for stewardship interventions (59). The United Nations General Assembly (UNGA), in its meeting in September 2024, has set a global target of “Access” antibiotics to account for 70% of total utilization to counter AMR (60).
Ethical considerationsEthical clearance for the study was obtained from the Human Ethics Division of the Department of Pharmacy Practice at the Faculty of Pharmacy, Bahauddin Zakariya University, Multan (Ref: BZU-FOPDPP-2446). Permission to conduct the study within the selected hospitals was also granted by their respective management teams. To ensure confidentiality, all patient data were anonymized at the time of collection. Unique, non-identifiable survey numbers generated by the Global-PPS software were used to maintain the anonymity of the data.
ResultsThe PPS was conducted across 23 pediatric wards of 14 hospitals, encompassing a total of 692 beds. Out of 498 pediatric patients assessed, 409 patients were prescribed antibiotics, giving a prevalence of 82.1%. The survey recorded a total of 734 instances where antibiotics were used across these pediatric cases. Around 327 patients were using more than one antibiotic. Only 2% of antibiotic use was based on culture sensitivity reports, and in only 23.2% of cases was the reason for prescribing an antibiotic mentioned on the patient notes. “Watch” antibiotics accounted for 72.1% (529) of the 734 antibiotics prescribed, followed by 25.7% of antibiotics in the “Access” category (Table 1). The highest prescribing of antibiotics was in the pediatric medical wards at 83.5%, with the distribution of antibiotics based on the AWaRe categories closely mirrored the overall findings. The Intensive Care Unit, although smaller in scale, showed a higher proportion of Reserve category antibiotics at 5.9% for central nervous system infections and prophylaxis, suggesting a focused approach to managing severe or high-risk infections. Parenteral administration dominated the route of administration, comprising 96.6% of the prescriptions.
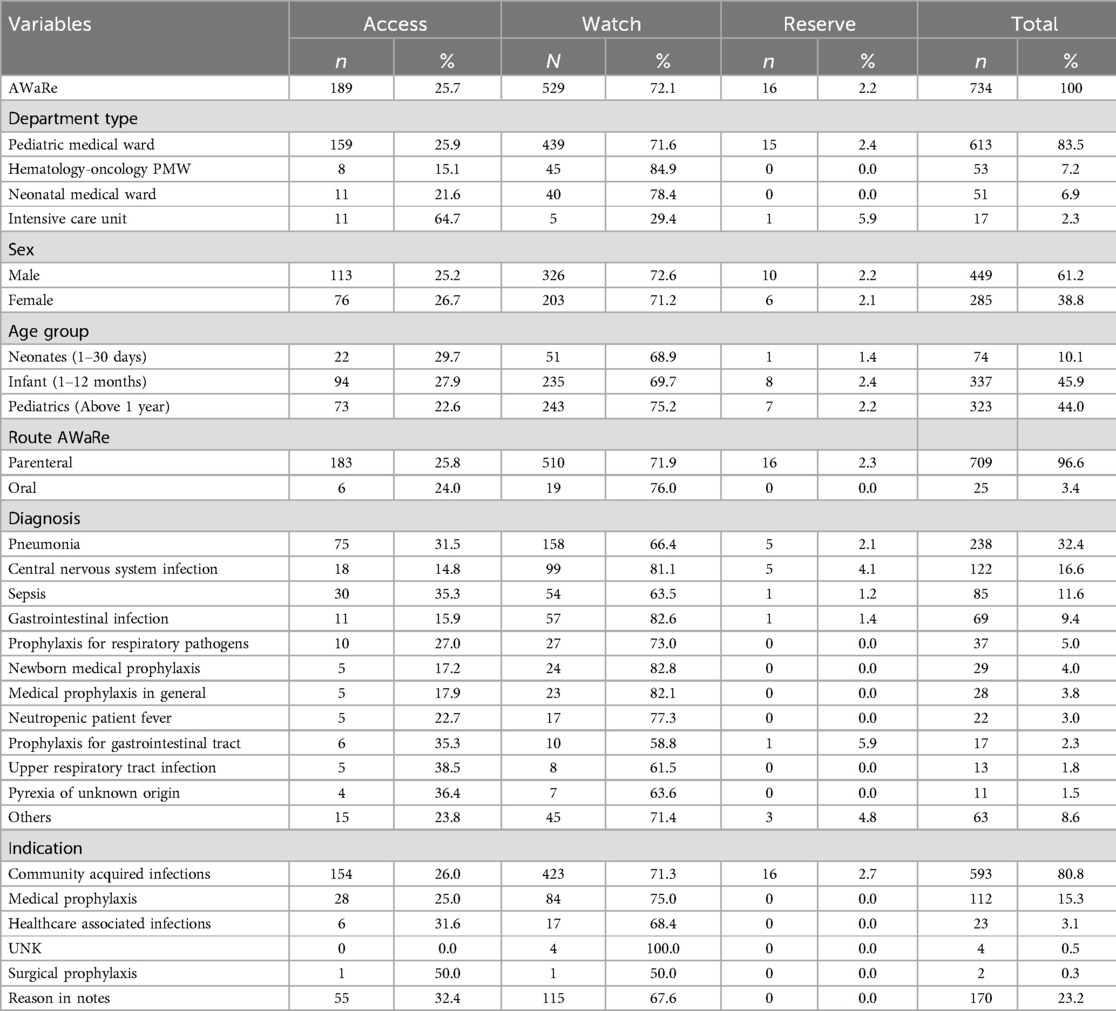
Table 1. Distribution of antibiotic use by AWaRe classification.
The most frequently reported diagnosis was pneumonia (32.4%), predominantly treated with Watch group antibiotics. Among the individual antibiotics, ceftriaxone, a “Watch” antibiotic, was the most commonly prescribed antibiotic, accounting for 37.2% of all antibiotics used, categorized under the Watch group, followed by vancomycin (13.5%) (Table 2). In examining the determinants influencing the use of “Watch” antibiotics, logistic regression analysis revealed several significant factors. The intercept, or constant term, of the model, was positive (coefficient = 1.96, p-value = 0.00), indicating the baseline log-odds of an antibiotic being classified as “Watch” when all other variables are zero. This result suggests a baseline propensity towards the “Watch” classification in the absence of modifying factors. Significantly, antibiotics administered within the ICU were substantially less likely to be classified as “Watch,” with a coefficient of −3.89 (p-value = 0.01) and an odds ratio of 0.02. This indicates a 98% decrease in the odds of “Watch” classification for antibiotics used in the ICU compared to the reference department, underscoring a conservative approach to antibiotic use in this high-risk setting (Table 3).
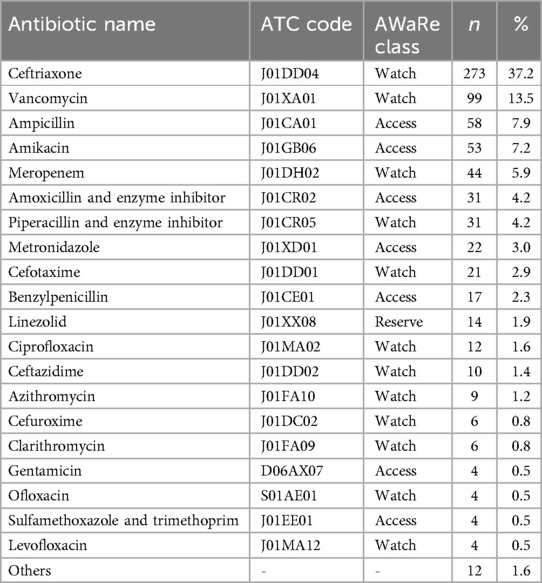
Table 2. Commonly prescribed antibiotics.
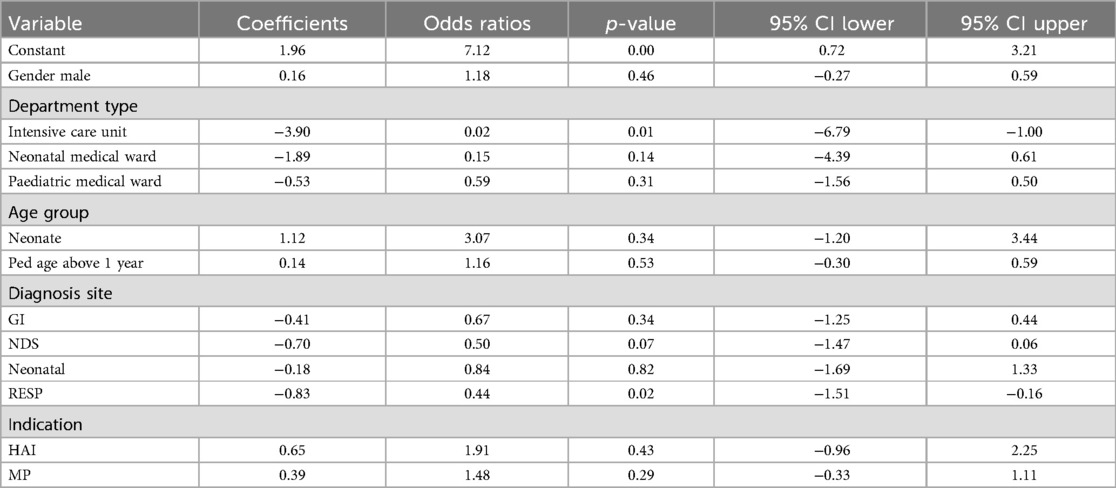
Table 3. Factors influencing the use of “watch” category antibiotics.
DiscussionUnequivocally, topnotch surveillance of antibiotic use is of prime importance to inform stewardship interventions, in which the PPS methodology offers a preeminent surveillance potential to monitor the use of antibiotics and acts as a baseline to inform policies regarding the correct utilization of antibiotics in hospital settings (11, 30). We believe this is the first comprehensive study undertaken in Pakistan to assess current antibiotic utilization rates among pediatric patients along with providing a comprehensive breakdown of antibiotic use across indications, wards and age groups. The prevalence rate of 82.1% for antibiotic use is similar to previous studies in Pakistan, including Mustafa et al. at 95.5% (56) and 97.5% (55) as well as Ambreen et al., with rates varying between 91% for the pediatric medical ward to 99% for pediatric intensive care and the neonatal medical ward (57). In addition, similar to a study in South Africa with a prevalence rate of 92% among hospitalized children (61) and in India, where up to 89% of neonates in NICUs were prescribed antibiotics (62). However, lower than seen in China (56.8%–66.1%) (63, 64), another study in India (61.5%) (65), Jordan at 75.6% overall, although up to 82.2% in Pediatric wards (66), Myanmar at 63.4% (67) and another study in South Africa at 49.7% (68). This compares with high-income countries that have shown decreasing trends in antibiotic utilization rates potentially enhanced by established ASPs, as well as adequate diagnostic and monitoring facilities compared to LMICs (69), where there is a dire need to upgrade existing laboratory infrastructure coupled with improving quality standards through international accreditation and standardizing procedures (70). The lack of monitoring of patient records as part of ASPs may help explain the fact that in only 23.2% of instances in our study, it was the reason for prescribing antibiotics mentioned in patients' notes. This compares to a Belgian study in which, on 81.9% of occasions, the indication for antibiotic use was recorded (33).
The high prevalence if antibiotic use may also have been exacerbated by the fact that in only 2% of occasions was culture and sensitivity testing undertaken. Whilst this is similar to other studies in Pakistan due to financial constraints (54, 56, 71), this is a concern going forward that needs to be urgently addressed along with addressing the lack of antibiograms to guide prescribing building on treatment recommendations in the recently launched AWaRe book (40, 72–74).
Our study findings revealed that pneumonia was the most prevalent infection for which antibiotics were prescribed (32.4%), similar to other studies from Pakistan (54–56). Given the epidemiological pattern, current diagnostic procedures may also need to be standardized as well because of the unreliability issues with the typically opted procedure of respiratory rate count in LMICs (75). An Ethiopian study also identified pneumonia as the most prevalent underlying infectious disease (28.6%) requiring antibiotics (76). However, a Jordanian study reported a lower prevalence of pneumonia at 20.6% among the underlying clinical conditions for the prescribing of antibiotics (66). Surprisingly, healthcare-associated infections (HAIs) were only noted in 3.1% of the patients as compared to 80.8% for community-acquired infections (CAIs). However, similar to the findings of Mustafa et al. (2022) (56). This result could be due to a lower reporting rate of HAIs in our study due to limited diagnostic modalities available, with Arif et al. (2021) reporting a higher rate at 20.3% (54). HAIs need to be addressed by strengthening the implementation of infection prevention and control programs (IPC) within hospital settings where this is an issue due to concerns about developing infections with multi-drug resistant organisms (MDROs). Hospitals may also benefit from the synergistic effect of combining infection prevention and control programs (IPCs) and ASPs to minimize resistant infections and antibiotic use (77, 78). This will be monitored in the future.
Parenteral administration was high at 96.6%, which is similar to other studies undertaken: Brazil (91%) (79), Pakistan (91.5%) (80), Ethiopia (90.5%) (76) and India (77.9%) (81). This also needs to be looked at in the future as part of possible ASPs with parenteral formulations and routes associated with an increased risk of infection (catheter-related infection) and higher costs if IV-to-oral switching is delayed (82). Increasing evidence suggests that an IV-to-Oral switching where this is practical is associated with improved clinical and economic outcomes (83, 84).
Another key concern is the high consumption of “Watch” category antibiotics in our study at 72.1%, indicating an appreciable divergence from the recent UNGA target of up to 70% consumption of “Access” antibiotics (60). However, such a non-judicious antibiotic use could be impeded by preferring ASP interventions, particularly formulary restriction or prior authorization of antibiotics (85, 86). Our findings are consistent with multifarious studies reporting inappropriate and high Watch category usage in various countries and worldwide (59, 64, 87–90). In contrast, South African studies (68, 91) reported 55.9%–70.2% antibiotic prescriptions from the Access category. Ceftriaxone was the most commonly used antibiotic in our study (37.2%), which is similar to other studies in Pakistan (25.8%) (56) as well as Ethiopia (30.4%) (76), and Uganda (50.6%) (92). Moreover, a point prevalence survey in 69 countries by Pauwels et al. concluded that Ceftriaxone is the most prescribed drug globally, predominantly used against pneumonia, with total prescriptions accounting for 20% (87).
Overuse of ceftriaxone has substantially contributed to its growing resistance against gram-negative pathogens (Klebsiella pneumoniae and E. Coli) in the pediatric population (50), which needs to be addressed going forward. Recently, a pharmacist-led educational intervention in one of the secondary care hospital in Pakistan showed an improvement in the knowledge, attitude, and practices of healthcare workers regarding the rational use of antibiotics and concluded that continuous educational programs could foster strong adherence to ASP guidelines (93). Such programs should be reciprocated to other facilities to generate strong compliance with ASP and curtail the threat of growing AMR.
The present study is not absolved of limitations. Although the study is multi-centric, we prefer not to generalize the results to Pakistan, as repeated PPS from all the provinces is a more balanced approach towards identifying trends affecting prescribing determinants. The study may not fully capture the influence of seasonal fluctuations on different diseases and use of antibiotics. The present study noted fewer antibiotic prescriptions in surgical prophylaxis as the survey day was “surgical OT day”; most of the patients were present in the operating room. Moreover, owing to the minimal reporting of antibiotic indications on patient notes, it was not possible to judge the appropriateness of the prescribed antibiotic. However, in conjunction with the existing literature, our study provides useful information regarding the state of antibiotic use in pediatrics and identifies areas of improvement and ASP implementation. Based on the findings, healthcare facilities can enhance guideline adherence and rationalize prescribing practices, contributing to better patient outcomes and reduced AMR in resource-limited settings.
ConclusionThis study reported a high prevalence of antibiotic use in pediatric patients. The use of the Watch category antibiotics was high, presenting a divergence from the target set by the WHO's AWaRe Classification. Although the AWaRe framework acts as a tool to instigate ASP, the practice of antibiotic use noted in our study highlights a clear deviation. Strong measures should be taken to ensure adherence to this tool. Moreover, the high empirical use of antibiotics highlights the lack of a microbiological laboratory infrastructure. It is time for ASP to be strengthened within hospital facilities to curb rising AMR and protect antibiotics for future use.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Ethical clearance for the study was obtained from the Human Ethics Division of the Department of Pharmacy Practice at the Faculty of Pharmacy, Bahauddin Zakariya University, Multan (Ref: BZU-FOPDPP-2446). Permission to conduct the study within the selected hospitals was also granted by their respective management teams. To ensure confidentiality, all patient data were anonymized at the time of collection. Unique, non-identifiable survey numbers generated by the Global-PPS software were used to maintain the anonymity of the data. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributionsSS: Conceptualization, Data curation, Writing – original draft. ZS: Conceptualization, Writing – original draft, Methodology, Project administration, Supervision, Writing – review & editing. SA: Conceptualization, Writing – review & editing. MQ: Methodology, Writing – review & editing. AR: Data curation, Writing – review & editing. SH: Methodology, Writing – original draft. BR: Project administration, Writing – review & editing, Funding acquisition. BG: Formal Analysis, Writing – original draft, Supervision.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Research Supporting Project, King Saud University, Riyadh, Saudi Arabia, (RSP2024R378) which provided funding for this work.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Wang CH, Hsieh YH, Powers ZM, Kao CY. Defeating antibiotic-resistant bacteria: exploring alternative therapies for a post-antibiotic era. Int J Mol Sci. (2020) 21(3):1–18. doi: 10.3390/ijms21031061
Crossref Full Text | Google Scholar
2. Abbott IJ, Peel TN, Cairns KA, Stewardson AJ. Antibiotic management of urinary tract infections in the post-antibiotic era: a narrative review highlighting diagnostic and antimicrobial stewardship. Clin Microbiol Infect. (2023) 29(10):1254–66. doi: 10.1016/j.cmi.2022.05.016
PubMed Abstract | Crossref Full Text | Google Scholar
3. Dhingra S, Rahman NAA, Peile E, Rahman M, Sartelli M, Hassali MA, et al. Microbial resistance movements: an overview of global public health threats posed by antimicrobial resistance, and how best to counter. Front Public Health. (2020) 8:535668. doi: 10.3389/fpubh.2020.535668
PubMed Abstract | Crossref Full Text | Google Scholar
4. Uddin TM, Chakraborty AJ, Khusro A, Zidan BRM, Mitra S, Emran TB, et al. Antibiotic resistance in microbes: history, mechanisms, therapeutic strategies and future prospects. J Infect Public Health. (2021) 14(12):1750–66. doi: 10.1016/j.jiph.2021.10.020
PubMed Abstract | Crossref Full Text | Google Scholar
5. Sartorius B, Gray AP, Weaver ND, Aguilar GR, Swetschinski LR, Ikuta KS, et al. The burden of bacterial antimicrobial resistance in the WHO African region in 2019: a cross-country systematic analysis. Lancet Glob Health. (2024) 12(2):e201–16. doi: 10.1016/S2214-109X(23)00539-9
PubMed Abstract | Crossref Full Text | Google Scholar
6. Naghavi M, Vollset SE, Ikuta KS, Swetschinski LR, Gray AP, Wool EE, et al. Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050. Lancet. (2024) 404(10459):1199–226. doi: 10.1016/S0140-6736(24)01867-1
PubMed Abstract | Crossref Full Text | Google Scholar
7. Poudel AN, Zhu S, Cooper N, Little P, Tarrant C, Hickman M, et al. The economic burden of antibiotic resistance: a systematic review and meta-analysis. PLoS One. (2023) 18(5):e0285170. doi: 10.1371/journal.pone.0285170
PubMed Abstract | Crossref Full Text | Google Scholar
9. Browne AJ, Chipeta MG, Haines-Woodhouse G, Kumaran EP, Hamadani BHK, Zaraa S, et al. Global antibiotic consumption and usage in humans, 2000–18: a spatial modelling study. Lancet Planet Health. (2021) 5(12):e893–904. doi: 10.1016/S2542-5196(21)00280-1
PubMed Abstract | Crossref Full Text | Google Scholar
12. Duong QA, Pittet LF, Curtis N, Zimmermann P. Antibiotic exposure and adverse long-term health outcomes in children: a systematic review and meta-analysis. J Infect. (2022) 85(3):213–300. doi: 10.1016/j.jinf.2022.01.005
PubMed Abstract | Crossref Full Text | Google Scholar
15. Bamford A, Masini T, Williams P, Sharland M, Gigante V, Dixit D, et al. Tackling the threat of antimicrobial resistance in neonates and children: outcomes from the first WHO-convened paediatric drug optimisation exercise for antibiotics. Lancet Child Adolesc Health. (2024) 8(6):456–66. doi: 10.1016/S2352-4642(24)00048-8
PubMed Abstract | Crossref Full Text | Google Scholar
18. Romandini A, Pani A, Schenardi PA, Pattarino GA, De Giacomo C, Scaglione F. Antibiotic resistance in pediatric infections: global emerging threats, predicting the near future. Antibiotics. (2021) 10(4):1–12. doi: 10.3390/antibiotics10040393
Crossref Full Text | Google Scholar
20. Munkholm L, Rubin O. The global governance of antimicrobial resistance: a cross-country study of alignment between the global action plan and national action plans. Global Health. (2020) 16:1–11. doi: 10.1186/s12992-020-00639-3
PubMed Abstract | Crossref Full Text | Google Scholar
21. Godman B, Egwuenu A, Wesangula E, Schellack N, Kalungia AC, Tiroyakgosi C, et al. Tackling antimicrobial resistance across sub-Saharan Africa: current challenges and implications for the future. Expert Opin Drug Saf. (2022) 21(8):1089–111. doi: 10.1080/14740338.2022.2106368
PubMed Abstract | Crossref Full Text | Google Scholar
22. Willemsen A, Reid S, Assefa Y. A review of national action plans on antimicrobial resistance: strengths and weaknesses. Antimicrob Resist Infect Control. (2022) 11(1):90. doi: 10.1186/s13756-022-01130-x
PubMed Abstract | Crossref Full Text | Google Scholar
23. Saleem Z, Godman B, Azhar F, Kalungia AC, Fadare J, Opanga S, et al. Progress on the national action plan of Pakistan on antimicrobial resistance (AMR): a narrative review and the implications. Expert Rev Anti Infect Ther. (2022) 20(1):71–93. doi: 10.1080/14787210.2021.1935238
PubMed Abstract | Crossref Full Text | Google Scholar
24. Ashley EA, Recht J, Chua A, Dance D, Dhorda M, Thomas NV, et al. An inventory of supranational antimicrobial resistance surveillance networks involving low- and middle-income countries since 2000. J Antimicrob Chemother. (2018) 73(7):1737–49. doi: 10.1093/jac/dky026
PubMed Abstract | Crossref Full Text | Google Scholar
25. World Health Organization. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report: 2022. Geneva: World Health Organization (2022).
26. Pallett SJ, Charani E, Hawkins L, Mazzella A, Anton-Vazquez V, Banerjee R, et al. National action plans for antimicrobial resistance and variations in surveillance data platforms. Bull World Health Organ. (2023) 101(8):501. doi: 10.2471/BLT.22.289403
PubMed Abstract | Crossref Full Text | Google Scholar
27. Sharland M, Gandra S, Huttner B, Moja L, Moja L, Pulcini C, et al. Encouraging AWaRe-ness and discouraging inappropriate antibiotic use—the new 2019 essential medicines list becomes a global antibiotic stewardship tool. Lancet Infect Dis. (2019) 19(12):1278–80. doi: 10.1016/S1473-3099(19)30532-8
PubMed Abstract | Crossref Full Text | Google Scholar
28. Sharland M, Pulcini C, Harbarth S, Zeng M, Gandra S, Mathur S, et al. Classifying antibiotics in the WHO essential medicines list for optimal use—be AWaRe. Lancet Infect Dis. (2018) 18(1):18–20. doi: 10.1016/S1473-3099(17)30724-7
PubMed Abstract | Crossref Full Text | Google Scholar
29. Tao W, Ivanovska V, Schweickert B, Muller A. Proxy indicators for antibiotic consumption; surveillance needed to control antimicrobial resistance. Bull World Health Organ. (2019) 97(1):3–3A. doi: 10.2471/BLT.18.227348
PubMed Abstract | Crossref Full Text | Google Scholar
31. Saleem Z, Hassali MA, Godman B, Versporten A, Hashmi FK, Saeed H, et al. Point prevalence surveys of antimicrobial use: a systematic review and the implications. Expert Rev Anti Infect Ther. (2020) 18(9):897–910. doi: 10.1080/14787210.2020.1767593
PubMed Abstract | Crossref Full Text | Google Scholar
32. Versporten A, Zarb P, Caniaux I, Gros MF, Drapier N, Miller M, et al. Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: results of an internet-based global point prevalence survey. Lancet Glob Health. (2018) 6(6):e619–29. doi: 10.1016/S2214-109X(18)30186-4
PubMed Abstract | Crossref Full Text | Google Scholar
33. Vandael E, Latour K, Goossens H, Magerman K, Drapier N, Catry B, et al. Point prevalence survey of antimicrobial use and healthcare-associated infections in Belgian acute care hospitals: results of the global-PPS and ECDC-PPS 2017. Antimicrob Resist Infect Control. (2020) 9(1):13. doi: 10.1186/s13756-019-0663-7
PubMed Abstract | Crossref Full Text | Google Scholar
34. Karanika S, Paudel S, Grigoras C, Kalbasi A, Mylonakis E. Systematic review and meta-analysis of clinical and economic outcomes from the implementation of hospital-based antimicrobial stewardship programs. Antimicrob Agents Chemother. (2016) 60(8):4840–52. doi: 10.1128/AAC.00825-16
PubMed Abstract | Crossref Full Text | Google Scholar
35. Lee CF, Cowling BJ, Feng S, Aso H, Wu P, Fukuda K, et al. Impact of antibiotic stewardship programmes in Asia: a systematic review and meta-analysis. J Antimicrob Chemother. (2018) 73(4):844–51. doi: 10.1093/jac/dkx492
PubMed Abstract | Crossref Full Text | Google Scholar
36. Nathwani D, Varghese D, Stephens J, Ansari W, Martin S, Charbonneau C. Value of hospital antimicrobial stewardship programs [ASPs]: a systematic review. Antimicrob Resist Infect Control. (2019) 8(1):35. doi: 10.1186/s13756-019-0471-0
PubMed Abstract | Crossref Full Text | Google Scholar
37. Otieno PA, Campbell S, Maley S, Obinju Arunga T, Otieno Okumu M. A systematic review of pharmacist-led antimicrobial stewardship programs in sub-Saharan Africa. Int J Clin Pract. (2022) 2022(1):3639943. doi: 10.1155/2022/3639943
PubMed Abstract | Crossref Full Text | Google Scholar
38. Cox JA, Vlieghe E, Mendelson M, Wertheim H, Ndegwa L, Villegas MV, et al. Antibiotic stewardship in low-and middle-income countries: the same but different? Clin Microbiol Infect. (2017) 23(11):812–8. doi: 10.1016/j.cmi.2017.07.010
PubMed Abstract | Crossref Full Text | Google Scholar
39. Kiggundu R, Lusaya E, Seni J, Waswa JP, Kakooza F, Tjipura D, et al. Identifying and addressing challenges to antimicrobial use surveillance in the human health sector in low- and middle-income countries: experiences and lessons learned from Tanzania and Uganda. Antimicrob Resist Infect Control. (2023) 12(1):9. doi: 10.1186/s13756-023-01213-3
PubMed Abstract | Crossref Full Text | Google Scholar
40. Harun MGD, Sumon SA, Hasan I, Akther FM, Islam MS, Anwar MMU. Barriers, facilitators, perceptions and impact of interventions in implementing antimicrobial stewardship programs in hospitals of low-middle and middle countries: a scoping review. Antimicrob Resist Infect Control. (2024) 13(1):8. doi: 10.1186/s13756-024-01369-6
PubMed Abstract | Crossref Full Text | Google Scholar
41. WHO. Antimicrobial stewardship programmes in health-care facilities in low-and middle-income countries: a WHO practical toolkit. (2019).
42. Di Pentima MC, Chan S, Hossain J. Benefits of a pediatric antimicrobial stewardship program at a children’s hospital. Pediatrics. (2011) 128(6):1062–70. doi: 10.1542/peds.2010-3589
PubMed Abstract | Crossref Full Text | Google Scholar
43. Donà D, Barbieri E, Daverio M, Lundin R, Giaquinto C, Zaoutis T, et al. Implementation and impact of pediatric antimicrobial stewardship programs: a systematic scoping review. Antimicrob Resist Infect Control. (2020) 9(1):3. doi: 10.1186/s13756-019-0659-3
留言 (0)