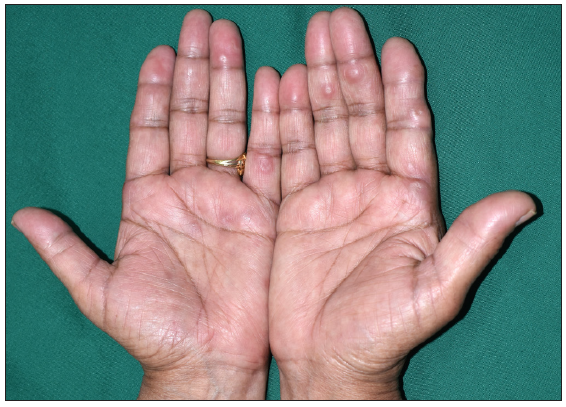
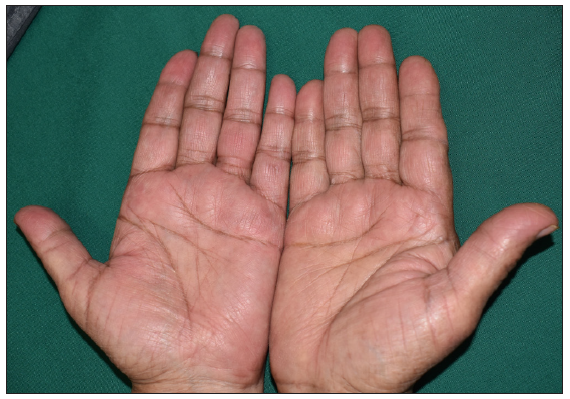
A 67-year-old woman presented to us with a 1-year history of asymptomatic skin-coloured nodules on bilateral hands and feet. The skin lesions first developed on the dorsum of hands and feet and gradually progressed to involve the palms, soles, and elbows over the next few months. She also reported mild pain affecting the small joints of her hands but denied joint swelling or morning stiffness. Her past medical history was significant for Raynaud’s phenomenon for many years and idiopathic thrombocytopenic purpura successfully treated 3 years back. Examination showed brownish, firm, mildly tender nodules and nodulo-plaques (2–3 cm in size) on the hands, predominantly around the inter-phalangeal and carpo-metacarpal joints, feet, and elbows [Figure 1a], and tender umbilicated papules on palms and soles [Figure 1b].

Export to PPT
Export to PPT
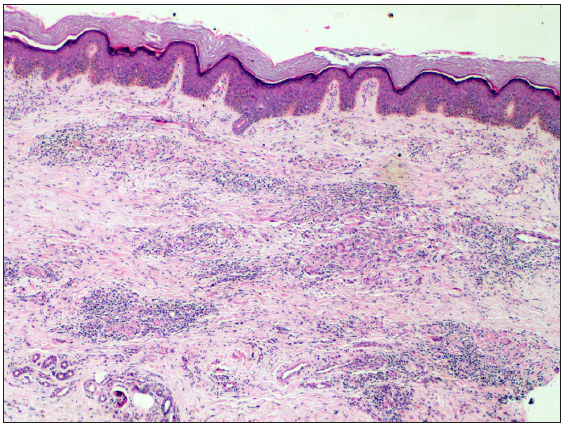
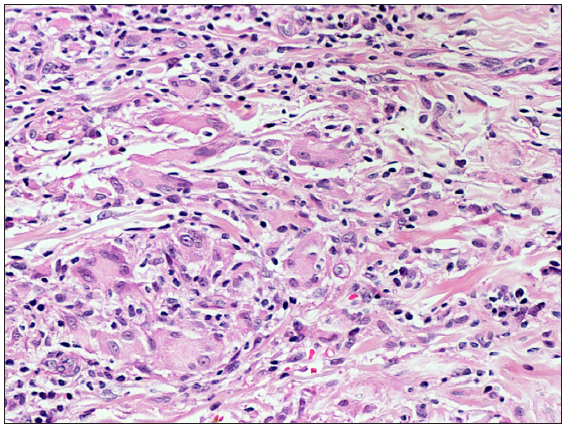
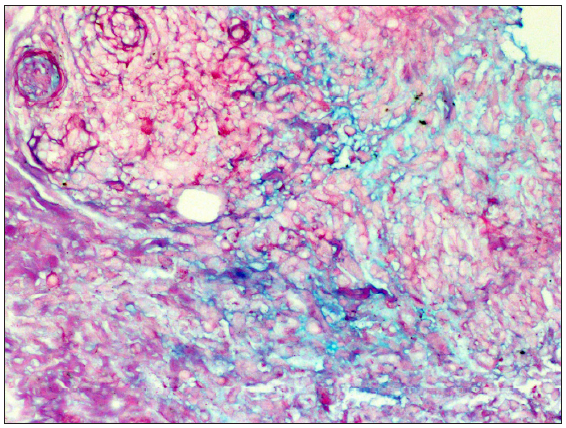
Histopathology of the hand nodule as well as the palmar papule showed perivascular and interstitial dermal infiltrate composed predominantly of histiocytes and lymphocytes along with a few small collections of epitheloid histiocytes and multinucleated giant cells [Figures 2a and 2b]. Alcian blue stain highlighted the excess dermal mucin deposition [Figure 2c]. Her blood investigations were significant for mildly elevated C-reactive protein (12.5 mg/dL; normal range <1.0 mg/dL) and antinuclear antibody titre of 1:80. Rheumatoid factor was negative. Radiographs of bilateral hands and feet were unremarkable.
Export to PPT
Export to PPT
Export to PPT
QuestionWhat is your diagnosis?
AnswerDiagnosis: Granuloma annulare
Oral dapsone (100 mg/day) and naproxen (500 mg/day) produced significant improvement in skin lesions and joint pain in 1 month. At 3 months, all the lesions on the hands and feet had completely subsided [Figures 3a and 3b], while the nodules around elbows had flattened significantly.

Export to PPT
Export to PPT
DiscussionTypical clinical variants of granuloma annulare include localised, generalised, subcutaneous or deep, perforating, and patch type.1 Barzilai et al. described a juxta-articular variant of deep granuloma annulare in a series of 14 women with erythematous-violaceous or skin-coloured nodules located mainly around the small joints of hands. Because of their clinical and histological resemblance to rheumatoid nodules, these were termed as ‘pseudorheumatoid nodules’.2 In addition, there are a few reports of granuloma annulare presenting as painful papules on the palms and soles as well which show the classical palisading or interstitial infiltrate and mucin deposition on histopathology. This appears to be a clinically distinct variant of granuloma annulare characterised by acute-onset of painful lesions on hands and feet and often associated with constitutional features.3
Our patient had juxta-articular as well as palmoplantar tender papules and nodules, along with arthralgias. In addition to granuloma annulare, differential diagnoses of juxta-articular and palmar nodules associated with arthralgias include rheumatoid nodules, erythema elevatum diutinum, and palisaded and neutrophilic granulomatous dermatitis. However, the absence of palisading necrobiotic granulomas, neutrophilic dermal infiltrate, and vessel wall damage on histopathology excluded these possibilities.4-6 Another entity, interstitial granulomatous dermatitis with arthritis can resemble granuloma annulare histologically and is associated with arthralgias, but the skin lesions are present on the trunk and flexures.7
To conclude, a possibility of granuloma annulare should be considered in patients presenting with tender juxta-articular and acral nodules. Clinical diagnosis may be missed because of its rarity and a strong clinico-pathological correlation is required to arrive at the correct diagnosis.
留言 (0)