Generalised pustular psoriasis (GPP) is a chronic, multisystemic, autoinflammatory disease with predominant cutaneous manifestations characterised by recurrent episodes of widespread, macroscopic aseptic pustules, with a highly unpredictable, heterogeneous and unstable clinical course.1,2 A typical GPP flare is characterised by an acute onset of widespread, inflamed skin studded with multiple sterile pustules of variable size, and is usually associated with systemic symptoms.3,4 GPP flares may occur de novo or triggered by factors such as infections, pregnancy and medications.3
Disease flares during the course of GPP are potentially life-threatening if left untreated, with a risk of multiple complications such as secondary bacterial infection, acute renal and liver damage, acute respiratory distress syndrome and cardiovascular aseptic shock.4,5 Mortality rate directly attributable to GPP or its associated treatment is reported to be 2–16%.6–11 Most common comorbidities in patients with GPP are arthritis, hypertension, depression, diabetes, asthma and thyroid dysfunction.12,13
Globally, treatment guidelines for GPP are evolving.14 However, currently there are no guidelines for the management of GPP in India. Varying ethnic, socio-economic and demographic factors necessitate the development of Indian guidelines/consensus. We therefore aimed to develop an Indian expert consensus addressing these unmet needs in the diagnosis and treatment of GPP.
Materials and Methods Study designThe objective of this Delphi panel study was to achieve consensus on six key domains of GPP: burden of GPP; diagnosis; severity assessment; investigations; treatment initiation, monitoring and escalation; and special populations.
MethodologyTwelve experts in the field of psoriasis agreed to participate in this consensus-building exercise. These experts are from various locations in India, and together provide a representation of all four zones – north, east, west and south – of India. Each of the experts (a) has an experience in the field of dermatology of more than 20 years, (b) has managed multiple patients of GPP, (c) works in a hospital-based (±office-based) setting with a facility to admit patients with GPP and (d) has an interest around psoriasis, as reflected by his/her publications. Based on discussions with each expert, Arun Dahiya & Tomson Toms identified problem areas related to the diagnosis and management of GPP, for which current evidence is absent or limited, and finalised topics/statements, removing duplicates and merging similar topics. This led to a total of 19 statements, which were then reconfirmed with the experts and classified under six domains. Consensus on these topics was assessed using the modified Delphi method, a well-established consensus technique for diseases in which clinical evidence might be insufficient. In round one, each expert was asked to opine on every statement by expressing his/her agreement/disagreement on a Google form (i.e., an asynchronous approach to consensus development). Experts were able to provide additional comments as freetext. Consensus was said to be reached when ≥80% of experts agreed to a statement. After round one, feedback (anonymised responses) was shared with all experts. Statements that reached consensus (i.e. ≥80% agreement) were not revised. Where consensus was not reached, statements were revised and the process of round one was repeated. In case stability in responses was reached (i.e. no change in response in two consecutive rounds), the Delphi iterations were closed.
ResultsAfter two rounds, consensus was reached for 17 statements (89%) [see summary in Table 1]. Wherever applicable, clarifications or additional comments by experts have been provided to make the consensus document more informative.
Table 1: Summary of all the statements on which consensus was or was not achieved.
Consensus level (%) Statements on which consensus was achieved GPP is clinically, pathophysiologically and genetically distinct from plaque psoriasis. GPP is primarily driven by the IL-36 pathway in contrast to plaque psoriasis which is primarily driven by IL-17/23. 100 Indian data on GPP is scarce. However, the incidence/prevalence is very low and GPP is considered to be a rare disease. 83 Added to the clinical diagnosis, presence of markers of systemic inflammation, such as fever, fatigue, myalgia, elevated CRP levels and leukocytosis, increases diagnostic certainty. 100 Added to the clinical diagnosis, skin biopsy (showing presence of neutrophilic subcorneal pustules and other characteristic features of GPP) increases diagnostic certainty. 100 Added to the clinical diagnosis, a history of repeated episodes of flare-ups of disease increases diagnostic certainty. 100 Generalised Pustular Psoriasis Physician Global Assessment is recommended to be assessed in clinical practice to assess the severity of flares of GPP. 100 Impact of GPP on QoL can be assessed using tools such as Dermatology Life Quality Index (DLQI), Pain visual analogue scale (Pain VAS) and Psoriasis Symptom Scale (PSS). 100 The routine laboratory investigations recommended in most cases of flares of GPP include CBC (complete blood counts), ESR (erythrocyte sedimentation rate), CRP (C-reactive protein), LFT (liver function tests), RFT (renal function tests) and urine analysis. 83 Skin biopsy is recommended in all suspected GPP patients. 92 Optional/additional investigations in select cases are: (a) Screening for infections such as tuberculosis, hepatitis B, hepatitis C and HIV and (b) Genetic testing to identify potential causative mutations in suspected patients. 100 In most patients with acute flare of GPP, the primary goal of therapy is rapid and sustained clearance of pustules. 100 While various drugs are currently used in the management of GPP flares, their safety and efficacy are yet to be adequately established. 100 Biologics should be considered as treatment escalation in (a) Patients with refractory flare that is intractable to systemic non-biologics or (b) Patients who are intolerant or have contraindications to systemic non-biologics. 100 Biologics may be considered over non-biologics as initial therapy, if two of the following three criteria are met: (a) Patients with a flare affecting ≥5% of the body surface area (BSA), (b) Patients with GPPGA total score ≥3, (c) Patients with significant impact on psychological/social function (e.g. DLQI ≥ 10) 92 It is recommended that outpatients or inpatients after discharge should be followed up on a weekly basis until resolution of flare. 83 The following drugs can be used in pregnant women – cyclosporine, corticosteroids, infliximab. 92 Treatment of GPP flares in children is in line with that of adults and should be based on risk-benefit assessment. 100 Statements on which consensus was not achieved GPP can be diagnosed clinically in a patient presenting with acute, primary, generalized and macroscopically visible pustules on non-acral skin. 75 Treatment escalation should be considered if a patient doesn’t achieve minimal improvement as defined by decrease in GPPGA total score by at least 1 point in 7–10 days. 42 Domain 1: Burden of GPPGPP was first described by Leopold von Zumbusch in 1910 as a severe form of psoriasis.2 However, it is now recognised as clinically, pathophysiologically and genetically distinct from plaque psoriasis.2
Traditionally, psoriasis comprised of both erythrosquamous and pustular lesions. These are distinct both clinically and histologically. More than 50% of patients with GPP can have concurrent or a previous history of plaque psoriasis.4 This may lead to an assumption that primary pustular conditions (e.g. GPP) are part of the psoriasis spectrum. However, primary pustules do not form part of the psoriasis spectrum except when pustules arise within or at the edge of plaques, and this should not be considered pustular psoriasis. In contrast,pustules are the primary lesions in GPP.15
GPP is an autoinflammatory pustular neutrophilic disease with a predominant involvement of innate immunity characterised by sterile inflammation without pathogenic autoantibodies or autoreactive T lymphocytes, whereas plaque psoriasis shows involvement of both innate and adaptive immunity and is an autoimmune disease.16 GPP is primarily driven by the IL-36 pathway while plaque psoriasis is driven by the TNF-α/IL-23/IL-17/IL-22 axis.17,18
GPP is rare and studies show a wide degree of regional variability in prevalence: 0.02 per 10,000 in France, 0.07–0.09 per 10,000 in Brazil, 0.15 per 10,000 in Sweden, 0.2 per 10,000 in Japan, 0.9 per 10,000 in the USA, 1.1 per 10,000 in South Korea and 1.4 per 10,000 in Germany.12,14,19 In India, however, there is limited published data on the prevalence of GPP.20
Statements1.
GPP is clinically, pathophysiologically and genetically distinct from plaque psoriasis. GPP is primarily driven by the IL-36 pathway in contrast to plaque psoriasis which is primarily driven by IL-17/23.
Agreement level: 12/12 (100%)
2.
Indian data on GPP is scarce. However, the incidence/prevalence is very low and GPP is considered to be a rare disease.
Agreement level: 10/12 (83%)
Additional comments:
In the absence of adequate data on incidence/prevalence of GPP in the Indian population, two authors did not comment on the rarity of the disease. However, both opined that as compared to the prevalence of plaque psoriasis, GPP is very infrequent in clinical practice.
Domain 2: DiagnosisGPP should be suspected in any patient with acute onset erythema and pustulosis.15,21 Diagnosis of GPP presents a clinical challenge due to the rarity of the disease and the absence of consistent diagnostic criteria.3,22
GPP is most common in the fourth decade of life and has a female preponderance.22 The clinical presentation is heterogeneous. Many patients experience GPP in three phases over several years – an initial pre-pustular phase, first widespread flare and a post-flare chronic phase.5 The initial pre-pustular phase may last for several years, in which many patients may experience psoriatic lesions. The next phase is marked by acute onset, widespread sterile pustules and inflamed skin. In the post-flare/chronic phase, it is common to have persisting skin symptoms. Relapse of flares is observed in most patients.10
Readers can refer to the European Rare and Severe Psoriasis Expert Network (ERASPEN) and the Japanese Dermatological Association (JDA) criteria for diagnosis of GPP.15,23 The most important diagnosis to exclude is acute generalised exanthematous pustulosis (AGEP), a severe and acute pustular condition most often triggered by medications. Typically, acute generalised exanthematous pustulosis has a rapid onset, shorter course of illness, no recurrence pattern and no personal or family history of plaque psoriasis. Resolution of acute generalised exanthematous pustulosis is often spontaneous and usually seen within 15 days of withdrawal of the causative agent.21,24,25 Other differential diagnoses include annular pustular psoriasis, localised forms of pustular psoriasis (e.g. palmoplantar pustulosis, acrodermatitis continua of Hallopeau), pemphigus foliaceus, immunoglobulin A(IgA) pemphigus and subcorneal pustular dermatosis.22
Statements3.
GPP can be diagnosed clinically in a patient presenting with acute, primary, generalised and macroscopically visible pustules on non-acral skin.
Agreement level: 9/12 (75%)
Additional comments: Pustules on an erythematous base, lakes of pus and peripheral scaling (which appears after a few days as a result of healing of pustules) are other characteristics. Bedside gram stain of smears from pustules helps in ruling out bacterial infection.
Disagreement: 3/12 experts mentioned that a confident diagnosis of GPP cannot be made solely on clinical examination.
4.
Added to the clinical diagnosis, the presence of markers of systemic inflammation, such as fever, fatigue, myalgia, elevated C-Reactive Protein (CRP) levels and leucocytosis increases diagnostic certainty.
Agreement level: 12/12 (100%)
5.
Added to the clinical diagnosis, biopsy (showing presence of neutrophilic subcorneal pustules and other characteristic features of GPP) increases diagnostic certainty.
Agreement level: 12/12 (100%)
6.
Added to the clinical diagnosis, history of repeated episodes of flare-ups of disease increases diagnostic certainty.
Agreement level: 12/12 (100%)
Domain 3: Assessment of severityPhysician Global Assessment (PGA) and Psoriasis Area and Severity Index (PASI) are clinical outcome measures widely used in plaque psoriasis to assess disease severity and response to treatment objectively.18 To improve the validity of these measures in GPP, the induration component in the above outcome measures was replaced with a pustular component, to develop the Generalised Pustular Psoriasis Physician Global Assessment (GPPGA) and the Generalised Pustular Psoriasis Area and Severity Index (GPPASI) respectively , which were externally validated.26, 27
GPP interferes in activities of daily living such as exercise, attending important life events and socialising, thus severely impacting the quality of life(QoL).5,28,29 A study among 102 patients with acute GPP reported a mean Dermatology Life Quality Index (DLQI) score of 12.4 during a follow-up visit (i.e. non-flare period), indicating severe impairment even in the post-flare chronic phase.10 Hence, assessment of clinical severity alone is inadequate to evaluate the burden of GPP, and patient-reported outcome measures can be used to assess the impact on QoL.27
Statements7.
GPPGA is recommended to be assessed in clinical practice to assess the severity of flares of GPP.
Agreement level: 12/12 (100%)
8.
Impact of GPP on QoL can be assessed using tools such as DLQI, Pain visual analogue scale (Pain VAS) and Psoriasis Symptom Scale (PSS).
Agreement level: 12/12 (100%)
Additional comments: Of the 12 experts,eight preferred DLQI, two preferred pain VAS and two preferred PSS as their first choice.
Domain 4: InvestigationsInvestigations are done to confirm diagnosis, assess severity/inflammation, assess involvement of other organs or to assess if certain medicines can be administered to a particular patient. Usual investigations include complete blood counts (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), liver function tests (LFT), renal function tests (RFT), urinalysis, blood chemistry, blood culture, gram staining of smear from pustules and skin biopsy.22,23,30
Among patients with the first flare of GPP, a skin biopsy may be done to confirm the diagnosis. Kogoj’s spongiform pustules in histopathology are a distinct finding. Other features include parakeratosis, hyperkeratosis, and elongated rete ridges.21,22
Screening for tuberculosis, hepatitis B, hepatitis C and human immunodeficiency virus (HIV) may be needed before initiating certain therapies.31
Loss of function mutations in the IL-36 receptor antagonist gene (IL36RN) associated with GPP were first identified in 2011. The frequency of this mutation in GPP patients ranges from 23% to 37%.4,5 Other mutations associated with GPP occur in CARD14, AP1S3, TNIP1, SERPINA3, and MPO genes.32 It is noted that patients with these mutations have increased disease severity, an earlier age of onset, and an increased risk of systemic inflammation.17 Importantly, these mutations are distinct to GPP and are not reported in patients with plaque psoriasis.33
Whether such mutations influence therapeutic responses hasn’t been wellstudied. Successful treatment with ustekinumab, IL-17A antagonists and spesolimab has been reported in patient subgroups with and without IL36RN mutations.34
Statements9.
The routine laboratory investigations recommended in most cases of flares of GPP include CBC, ESR, CRP, LFT, RFT, and urine analysis.
Agreement level: 10/12 (83%)
Additional comments:
A few experts opined that additional investigations e.g., serum calcium to look for hypocalcaemia, serum procalcitonin to assess risk of sepsis, ultrasonography (USG) of the abdomen to rule out cholangitis and blood culture to identify potential pathogens should be performed routinely in suspected cases.
10.
Skin biopsy is recommended in all suspected GPP patients.
Agreement level: 11/12 (92%)
Disagreement:
One expert opined that biopsy is required only in select cases when diagnosis is not clear and is not recommended for all patients with suspected GPP.
11.
Optional/additional investigations in select cases are:
Screening for infections such as tuberculosis, hepatitis B, hepatitis C and HIV.
Genetic testing to identify potential causative mutations in suspected patients.
Agreement level: 12/12 (100%)
Clarification: Screening for infections such as tuberculosis, hepatitis B, hepatitis C and HIV may not be required in all patients, but is mandatory before initiating immunosuppressants/biologics. Genetic testing for potential causative mutations is not commonly available and is not necessary, but can be sought, especially if there are ‘clusters’ of cases in a family.
Domain 5: Treatment initiation, monitoring and escalationRapid control of skin symptoms, control of systemic inflammation and preventing complications are the immediate therapeutic goals during an acute flare.35
Treatment initiationAvailable data for a majority of treatment options originate mainly from case reports and a few small open-label, single-arm studies.4,17
Although some studies describe positive clinical outcomes, data are limited by small sample size, single-arm open-label study design, potential publication bias and limited generalizability. Additionally, it is important to note that these studies assessed patients with chronic GPP and not in acute flares.4 Differences in the reporting and use of varying non-standardised measures to assess therapeutic efficacy make it difficult to assess the evidence from these studies.17
Conventional therapies are not approved specifically for the treatment of patients with GPP.4 While some patients may respond to these therapies, the response is often partial and delayed.36 Recently, spesolimab has been approved for the management of flares of GPP in various countries, including India.37 The approval is based on the results of Effisayil 1 trial, which is one of the largest placebo-controlled trials in patients with flares of GPP.
MonitoringClinical disease outcome measures (e.g. GPPGA) and markers of systemic inflammation can be used to evaluate treatment response.38
Treatment escalationPhysicians usually wait from a few days to one or two weeks to assess response to therapy. In case response is considered inadequate, treatment is escalated with an increase in the dose of ongoing medication, addition of other therapies or switching to an alternative therapy.31,38
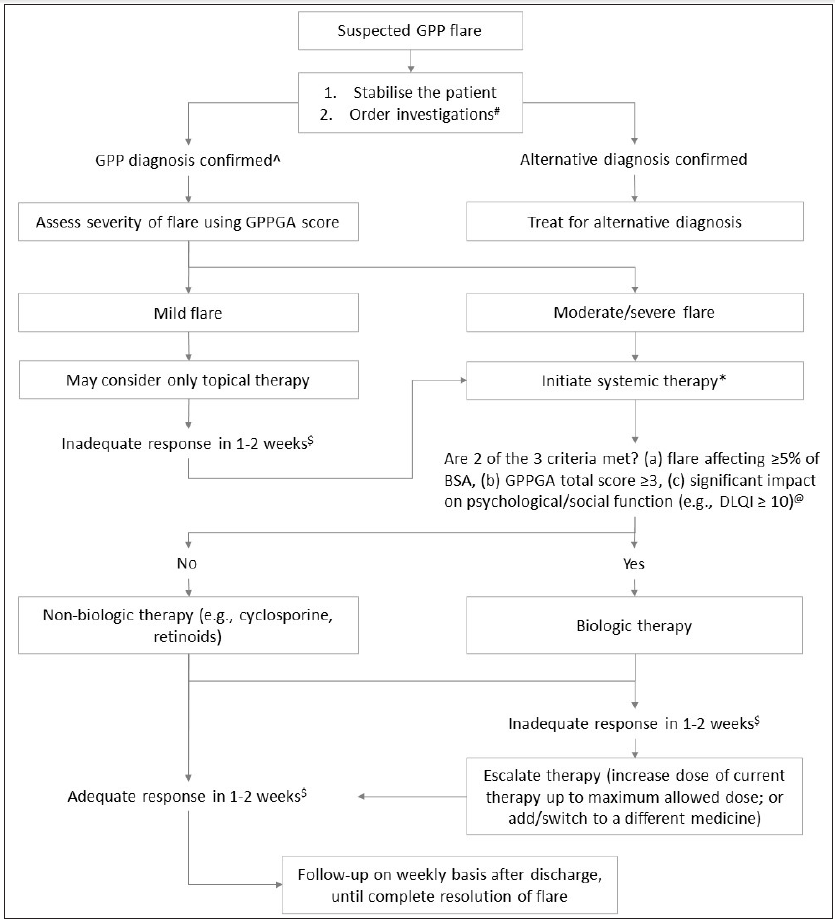
Treatment algorithmSystemic therapy should be initiated in patients with moderate/severe disease and in mild cases where topical therapy is ineffective.4 Various medicines that may be tried include retinoids, cyclosporine, TNF inhibitors, and biologics used for plaque psoriasis. Spesolimab has been recently approved for the management of flares of GPP in adult patients, and adds to the treatment armamentarium. Systemic corticosteroids should only be used in severe/life-threatening cases and only for a few days, considering the risks associated with steroids, including triggering a flare upon withdrawal.4 Standard protocol for tapering corticosteroids should be followed.
Supportive measures include maintenance of fluid and electrolyte balance, thermoregulation, monitoring for infections and other complications and treatment of symptoms such as pain/fever.23
Based on the consensus, we have suggested an algorithm for the management of flares of GPP [see Figure 1].
Export to PPT
Statements12.
In most patients with acute flare of GPP, the primary goal of therapy is rapid and sustained clearance of pustules.
Agreement level: 12/12 (100%)
13.
While various drugs are currently used in the management of GPP flares, their safety and efficacy are yet to be adequately established.
Agreement level: 12/12 (100%)
Additional comments:
A few experts commented that there is reasonable clinical experience with use of certain agents (e.g. cyclosporine, acitretin, methotrexate) in GPP, although published literature on their safety and efficacy is limited.
14.
Treatment escalation should be considered if a patient doesn’t achieve minimal improvement as defined by a decrease in GPPGA total score by at least 1 point in 7–10 days.
Agreement level: 5/12 (42%)
Additional comments:
‘Minimal improvement’ of 1 point in 7–10 days was considered too small an improvement by 7 out of 12 experts. Various alternatives suggested (but none reaching consensus) by experts were:
i.
Reduction in GPPGA total score by ≥1 point in 4–5 days
ii.
Reduction in GPPGA total score by ≥2 points in 7–10 days
iii.
Reduction in GPPGA pustulation subscore by ≥2 points in seven days
15.
Biologics should be considered as treatment escalation in:
a.
Patients with refractory flare that is intractable to systemic non-biologics
b.
Patients who are intolerant or have contraindications to systemic non-biologics
Agreement level: 12/12 (100%)
16.
Biologics may be considered over non-biologics as initial therapy if two of the following three criteria are met:
a.
Patients with a flare affecting ≥5% of the body surface area (BSA)
b.
Patients with GPPGA total score ≥3
c.
Patients with significant impact on psychological/social function (e.g. DLQI ≥ 10)
Agreement level: 11/12 (92%)
Additional comments:
One expert opined that biologics can also be considered as initial therapy in the context of important life events (e.g. marriage). Another expert opined that cost is an important factor while choosing biologics.
Disagreement:
One expert opined that for criterion (a), cut-off should be ≥ 10% BSA instead of ≥ 5% BSA.
17.
It is recommended that outpatients or inpatients after discharge should be followed up on a weekly basis until resolution of the flare.
Agreement level: 10/12 (83%)
Additional comments:
Experts opined that most of these patients would be hospitalised during an acute flare and would be reviewed daily.
One expert opined that weekly follow-up might not be possible for patients living at faraway places. In these cases, fortnightly follow-up may be acceptable.
Disagreement:
One expert suggested more than once a week and another suggested fortnightly follow-up frequency until resolution of flare.
Domain 6: Special populations Pregnancy and lactationTreatment of GPP in pregnant women is challenging. Acitretin and methotrexate are contraindicated, and the safety of biologics is not well established.4 Biologics may be considered with caution for severe/refractory cases, discontinuing biologics at the earliest.31,39 Many biologics (certolizumab pegol being an exception) are transferred across the placenta; the impact of this on neonatal development is not well studied.39 It is prudent to avoid live vaccines for the first six months of life in infants born to mothers who received biologictherapy beyond 16 weeks of gestation.38
Children: Evidence for various GPP therapies in children is even more limited. However, therapy can be on the lines of therapy for adults. In the absence of evidence, biologics may be considered only in severe/refractory cases.4,31
Statements18.
Following drugs can be used in pregnant women – cyclosporine, corticosteroids and infliximab.
Agreement level: 11/12 (92%)
Additional comments:
Corticosteroids can cause cleft lip/palate when administered in the first trimester. Prednisolone is considered to be safer among the corticosteroids, since it is degraded by the placenta and foetal exposure is low. Another expert added that non-fluorinated corticosteroids should be preferred in pregnancy. Biologics like infliximab, etanercept and adalimumab can be used in first and second trimesters, while certolizumab can be used in all trimesters.
19.
Treatment of GPP flares in children is in line with that of adults and should be based on risk-benefit assessment.
Agreement level: 12/12 (100%)
Additional comments:
One expert recommended involving a paediatrician in managing children with GPP.
DiscussionTo date, there has been a lack of consensus and an absence of recommendations on diagnosing and treating GPP. This paper presents a consensus-based guidance by Indian experts. We assessed 19 statements across six major domains relevant to clinicians who come across patients with GPP and achieved consensus on 17 statements.
Statements for which consensus was not reached likely indicate areas of evidence gaps. Hopefully, additional evidence will become available in the future and potentially resolve the disagreement.
ConclusionThis expert consensus provides guidance for the diagnosis and management of GPP. We believe that this consensus will provide a framework for future treatment decision-making in India.
留言 (0)