Dear Editor,
Trichostasis spinulosa is an under-recognised disorder affecting the hair follicles or pilosebaceous unit, characterised by black, spiny, keratotic follicular plugs with tufts of hair. It typically occurs on the mid-face, especially the nose and upper arms. However, occurrences over the scalp, lower eyelids, breasts, and axillae have also been reported.1 It may sometimes coexist with other dermatological conditions such as intradermal melanocytic naevi, collagenomas, and syringomas.2 Here, we describe a case of secondary trichostasis spinulosa within a chest keloid.
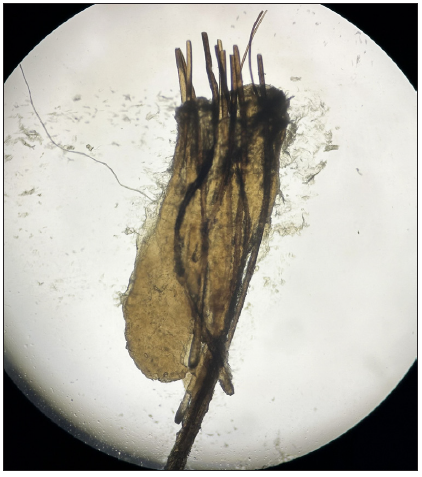
A 48-year-old male presented to us for the treatment of a 3-year-old keloid over his right chest. He had received multiple intralesional triamcinolone acetonide injections over the past year without much improvement. On examination, apart from the keloid, multiple brown–black keratotic papules were noticed incidentally at the periphery of the keloid [Figure 1]. Dermoscopy of these papules revealed hair tufts emerging from small pits and comedo-like structures [Figure 2]. A potassium hydroxide (10% KOH) mount of expressed follicular plug revealed a bundle of short and stout hair surrounded by a keratinous sheath [Figure 3]. Based on these findings, the black papules were diagnosed as secondary trichostasis spinulosa in a keloid. The patient was counselled about the benign nature of the disease and offered laser hair reduction. Given the asymptomatic lesions, the patient opted out of any trichostasis spinulosa–specific treatment. The keloid was planned to be treated with cryotherapy and silicone gel sheet applications.

Export to PPT

Export to PPT
Export to PPT
Trichostasis spinulosa is a disorder of hair follicles characterised by the successive production and retention of vellus telogen club hair from a single hair matrix within a dilated hair follicle. The asymptomatic nature of this disorder often makes it an unrecognised and underreported entity. However, few cases may be associated with pruritus and erythema.3 There are two clinical variants: the classical variant, which presents as asymptomatic comedo-like lesions on the nose in elderly individuals, and the pruritic variant, which presents as multiple itchy follicular papules on the trunk and extremities in adults.1
The precise cause of trichostasis spinulosa remains unclear. It is hypothesized that various external factors, such as ultraviolet radiation, dust, oils, heat, and topical minoxidil, may contribute to follicular damage. Systemic conditions such as chronic kidney disease and congenital follicular dysplasia have also been linked to the disorder. Several theories have been proposed to explain its pathogenesis, including a halt in hair shedding, infundibular hyperkeratosis, and an abnormal angle between the isthmus and infundibulum. The involvement of Malassezia and Propionibacterium has been suggested as well.1–3 Nakamura et al. hypothesised that excessive collagen production, in their case of collagenoma, may block the follicular infundibulum and play a role in the development of trichostasis spinulosa.2 The collagen production in keloids is significantly higher than in normal scars, and the keloidal matrix lacks elastin, hyaluronic acid, and dermatopontin, resulting in rigidity and reduced elasticity.4,5 These changes in the microenvironment of hair follicles within keloids could lead to follicular dilation and increased risk of trichostasis spinulosa. Additionally, the widespread upregulation of involucrin expression in keloids may induce follicular hyperkeratosis, and the loss of the arrector pili muscle could result in an altered angle between the isthmus and infundibulum, causing retention of shed telogen hairs.5,6
Pilonidal sinuses are not uncommon within keloids and are often complicated by recurrent purulent discharge. Similar to trichostasis spinulosa, the pilonidal sinus also has tufts of trapped, shed telogen hair, which can be extracted manually.7 However, unlike trichostasis spinulosa, hairs in the pilonidal sinus are outside the follicular canal and, therefore, elicit recurrent inflammatory episodes. Trichostasis spinulosa is characterised by polytrichia (>5 hairs emerging from a follicular ostium), a finding also seen in pili multigemini, tufted folliculitis, and other cicatricial alopecias.1 However, as the anagen hair is involved in these disorders, the hair tuft cannot be expressed manually.
Treatment approaches encompass the use of topical keratolytics, emollients, erythromycin gel, and topical and oral retinoids. Additionally, hydroactive adhesive tapes are employed. For effective results and minimal recurrence, laser hair reduction through the application of an 800 nm diode laser and a long-pulsed 755 nm alexandrite laser has shown benefit.1–3
To conclude, we report a novel observation of trichostasis spinulosa within a keloid. It is important to distinguish this benign and likely incidental finding from other conditions.
留言 (0)