Palliative care involves managing symptoms, including pain, that arise from diseases and recognising that life and death are natural processes. The aim is not to hasten or delay death but to offer support to enable patients to live as actively as possible and to help families overcome challenges when caring for patients and during bereavement.[1] Nurses have the responsibility of evaluating and treating symptoms arising from illnesses and treatment, in addition to assessing a patient’s condition and changes that occur. A comprehensive and individualised assessment of the patient is required to plan and provide optimal palliative care.[2] It is imperative that the assessment is carried out accurately and completely, as any shortcomings may ultimately affect the precision of the nursing interventions planned, and, as a result, inaccurate assessments were made regarding the patient’s health.[3]
Palliative care nursing seeks to enhance the quality of life of patients and their families by preventing and alleviating patient suffering. Nurses must appreciate the singularity of palliative care nursing to recognise a patient’s needs.[4] Nursing staff are responsible for addressing patient issues through nursing care plans that encompass all aspects, including physical, psychosocial, emotional, and spiritual well-being. To equip nurses to handle patients with severe and potentially fatal illnesses, it is imperative that a suitable educational programme is in place. This curriculum should encompass palliative care concepts, the advancement of palliative care, palliative evaluation, and techniques for managing patients with life-threatening and serious conditions.[5] Healthcare professionals, particularly nursing students, require a sufficient education to provide palliative care competently. This education can be achieved through both formal and informal training. According to recent research conducted in Norway by Valen et al.,[6] nursing students lack readiness to provide palliative care. Gelegjamts et al.[7] found that nursing students often lack sufficient preparation when providing palliative care services. To adequately equip nursing students with the knowledge and skills needed for such care, there is a need for a quality curriculum and learning resources such as textbooks that provide standardised and culturally sensitive experiences in palliative care for patients. This statement aligns with the findings of Zhou et al.,[8], who highlighted the importance of considering the varied cultural backgrounds of individuals when providing palliative care.
A suitable assessment is essential to enhance the standard of nursing care provided to patients. Nursing students can contribute to palliative nursing care for patients, including assessing their condition. Despite the challenges nursing students encounter while conducting assessments, there has been little exploration of their experiences regarding the performance of comprehensive assessments. Therefore, what constitutes the most effective assessment form that is efficient and enables students to conduct palliative assessments for patients needs further exploration. The researchers in this study aimed to investigate students’ experiences in conducting palliative assessments using the provided form in the field of palliative nursing in hospital settings. Both facilitating and hindering factors in the use of existing assessment forms were identified. This information will be beneficial for nurses, academics, and students in drafting appropriate forms to aid clinicians in conducting palliative assessments of patients.
The purpose of this study was to explore the experiences of nursing students in conducting palliative assessments for patients in an Indonesian hospital setting. The generic question this research sought to address is, ‘How do students conduct palliative assessments for patients during a clinical practice term in a hospital?’
MATERIALS AND METHODS Study design and participantsThe first researcher in this study (Titan Ligita) was a qualitative researcher who viewed the existence of phenomena that occur naturally. The human experience is meaningful and valuable. The experience is also influenced by many aspects and other people. This phenomenological study involved eight participating nursing students who were purposefully selected according to the inclusion criterion of involvement in palliative care nursing during their clinical placement in a hospital in West Kalimantan. These undergraduate nursing students had previously taken a course in end-of-life and palliative care. One of the research team members who interviewed the participants involved in providing the course. To minimise the bias, another researcher who has never been involved in the course was involved in the process of data analysis and interpretation.
Data collectionIn initial data collection, we first involved six participants. Then, during the analytical process, we interviewed two more participants and reached data saturation. For the purpose of data validation, we conducted member checking by interviewing two participants who had been interviewed previously. Consequently, the research conducted 10 interviews. The interviews were conducted at a university. Data collection took place between July and August 2023 after obtaining approval from the human research committee of the University T (Number 3480/UN22.9/PG/2023).
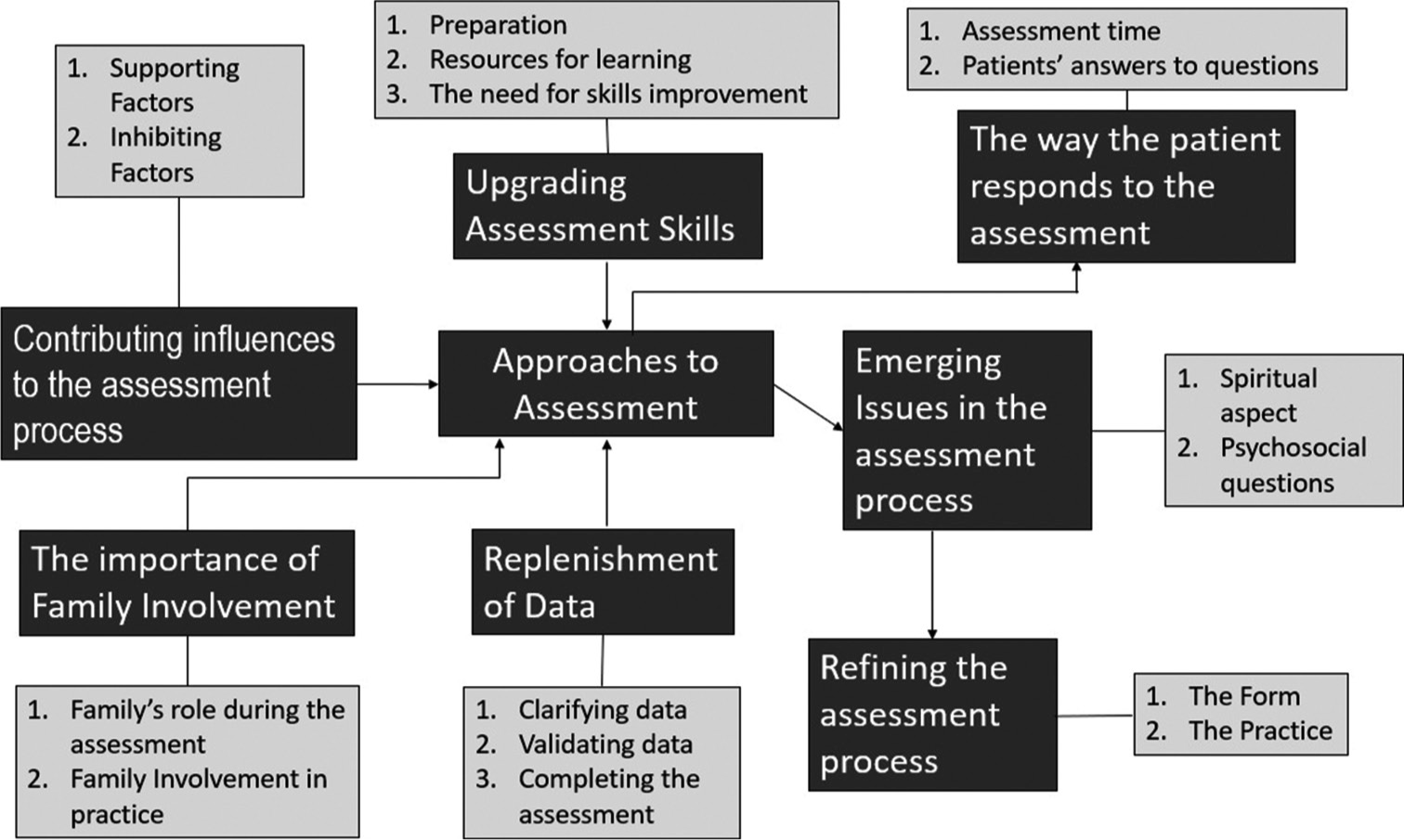
Data analysisThe data gathered were analysed using the interpretative phenomenological approach of Eatough et al.,[9] which involves eight essential steps. We first transcribed the interview recordings verbatim. The transcriptions were read several times. To assist in the analytical process, a concept map was also created. This map depicted the assessment of palliative care from the perspective of nursing students [Figure 1]. In this figure, black colors indicate the main themes of the study findings while the gray colors represent the sub-themes. Member checking involved two previous participants and two upcoming participants who had not been interviewed. In the member-checking process, they were presented with a narrative account of the student’s experiences, accompanied by a concept map to aid comprehension. The researchers subsequently solicited feedback on the interim findings. The results of this second round of data collection and analysis served to reinforce the conclusions of the initial investigation. The process of data analysis was undertaken by an academic nurse with a doctorate in nursing and one academic nurse with a master’s degree in nursing.
Export to PPT
RESULTSEight main themes were generated: Upgrading assessment skills, Contributing influences in the assessment process, The way the patient responds to the assessment, Replenishment of data, The importance of family involvement, Emerging issues in the assessment process, Approaches to assessment, and Refining the assessment process.
Upgrading assessment skillsTo enhance assessment proficiency, students must prepare, utilise pertinent learning materials, and engage in practice exercises to become familiar with assessment methods. They can access research papers, participate in peer discussions, and watch educational videos through diverse media. In addition, reflecting on prior practice experience, including learning from fellow students who have worked on palliative care assessments, can aid in improving skills. Before beginning an assessment, students undertake various preparations, including mental preparation, gathering the necessary materials, and acquainting themselves with the assessment form. These may involve discussions with peers and healthcare professionals. For students to enhance their assessment skills, they must discuss the results of the assessment with supervisors and peers. Furthermore, students should practise reviewing in class to become more accustomed to assessment questions and avoid difficulty in comprehending them. Participant 3 and participant 6 remarked:
For knowledge preparation before clinical placement, I read and discuss with friends so that there is no miscommunication. So, the preparation is communication in the group or directly during shift changes, such as whether there are questions that will be repeated. Then I read medical records to see from the perspective of the previous nurse. (P6)
Contributing influences in the assessment processThere are supportive factors that can assist in conducting the assessment. The students were given material during their classes by their lecturers, and their fellow students reminded them of the assessment questions that had to be completed. An individual’s confidence and understanding can positively influence the execution of their assessment of a patient. A patient’s unstable condition presents an inhibiting factor for assessment, necessitating a specialised strategy for conducting a palliative assessment. Moreover, conducting an inappropriate assessment may affect the collected data, which is not yet comprehensive:
Things that can hinder the assessment process, for example, when I felt that the patient’s gestures showed they were too tired to respond or answer, so I just had to shorten it (the assessment). When I was about to do the assessment and saw that the patient was still resting, I postponed it. The family plays an important role by paying attention to the patient’s condition because palliative patients need support. (P3)
The way the patient responds to the assessmentA patient’s responses to questions may be adversely influenced by factors such as their health status and the evaluation schedule. Furthermore, the interactional style of the examiner can influence the provided answers. The answers provided by patients tend to be short or simplistic despite open-ended interrogations being employed. There are certain questions that students might have difficulty posing to patients, which can affect their patient’s willingness to disclose pertinent information. Assessing a patient’s condition can be challenging, depending on their willingness to disclose information and their response during assessment. Students in this study emphasised that the patient’s current state should be considered in the assessment process, as the following students’ experiences illustrate:
There are patients who, when being asked a question, they answer it briefly. Especially if we give a choice of answers, the patient will answer briefly (Even if asked an open question), and the patient also answers (briefly). For example, regarding the question of the source of pain, ‘Where does it hurt mum? Is it in the head?’, ‘Yes’. (P2)
Replenishment of dataWhen completing data assessments, nursing students perform two key tasks: Data clarification and data validation. Data clarification involves verifying data with other group members. If a student struggles with this task, they can complete the assessment during patient care activities. Data validation is conducted by observing the patient’s condition over the course of several days of treatment and by directly asking the patient for information. If the data remains incomplete, students perform additional assessments during patient care and cross-check information with medical records. Regarding student group assessments, tasks are divided according to the practice schedule for review, and assessment data are then combined and adjusted to the required form. This is essential to ensure a complete and accurate assessment. Several nursing students expressed their efforts in this regard in the following statements:
For data shortages in the assessment, I usually go back to the patient when we are doing other activities, such as checking vital signs, in which we have a conversation and collect the information that is currently lacking. Furthermore, I can ask the nurse or look at the patient’s medical record again. (P1)
There was a specific time to do the assessment (for example, to clarify the pain the patient felt). I asked first if the patient was willing to be interviewed because I was worried about disturbing their rest time; then during the vital signs examination activity, I made sure to clarify whether there was still an increase in pain. (P6)
The importance of family involvementDuring patient assessments, students value the participation of the patient’s family and their important role in the assessment process. When asking questions that needed to be kept simple because of the patient’s condition, students focused on the assessment queries. Families helped translate patient responses into Indonesian and provided information additional to the patient’s answers. The family contributed by adding clarity to the patient’s answers. They also offered suggestions regarding activities that the patient could undertake and provided insights into the patient’s condition at home. A family-oriented approach is essential during assessment, particularly for patients who are heavily reliant on their families. This is illustrated by participant 5 and participant 2:
When conducting the assessment, the family also helped to validate; when the patient answered, the family helped to explain about the beginning of the patient experiencing this disease. (P5)
Emerging issues in the assessment processVarious issues emerged during assessments, particularly surrounding questions about the patient’s religious practices while in the hospital. Patients predominantly responded by stating that they pray, which limited the ability of students to delve further into the prayer ritual because the patients did not explain in detail their religious rituals. Furthermore, students struggled to discuss social aspects because of the use of a language that was challenging for the general public to comprehend, which required students to seek synonyms with identical meanings. On occasion, individuals replied impolitely to inquiries from the students regarding these psychosocial facets. Emerging issues were highlighted by the students:
Questions related to spiritual aspects are rather difficult to understand, so they are difficult to ask. The language used in the questions in the assessment form is quite easy, but it became difficult for me when I asked the patient these questions. Therefore, it is necessary to include training to improve skills in asking questions. (P7)
Approaches to assessmentDuring the assessment, students implemented strategies to address any issues that may arise. They ensured cultural sensitivity by adapting their language when interacting with patients to facilitate better understanding. If the patient and student shared the same culture, such as speaking the same regional language, the assessment process tended to be smoother. During an assessment, students considered the patient’s environment and conditions while paying attention to the effects of the surroundings on their psychosocial well-being. They carefully framed their questions and observed the patient’s condition to ensure an appropriate duration for the assessment. If the patient’s condition permitted, the questioning continued. In terms of spiritual assessment, students commonly enabled their peers to enquire about spirituality to avoid any misunderstandings. Moreover, students carried out assessments by observing patients participating in worship rituals while under hospital care. Students experienced the following situations with patients:
I didn’t really emphasize the cultural aspects of the assessment, especially the language used when asking questions. I can use Indonesian with patients, but when the patient has limited Indonesian, for example, only speaking Malay, I asked my fellow students who speak the same language to help with the assessment questions. (P2)
Refining the assessment processStudents felt that there was a need for improvements in the assessment process to promote ease and practicality for students in reviewing. These included improvements during practice and preparation as well as improvements to the assessment form. According to the students, the duration of practice in the field needs to be increased. Furthermore, there needs to be a demonstration in class before students undertake the practical programme in the field so that students are accustomed to asking questions according to the assessment form. The current assessment form is complete and well-designed, but some aspects should be rectified; in particular, the questions should be simpler, especially those relating to spiritual and psychosocial aspects. As students have different levels of understanding of the assessment form, it is necessary to explain ambiguous questions in language that is easy to understand, including foreign languages in the assessment form. The foreign language used in the form needs to be translated into Bahasa Indonesia. Two participants described the need for improvement in the assessment:
Cultural questions need to be asked because usually, people look at their illnesses from a cultural point of view. Then, in conducting the assessment, it is important to as much as possible use language that is more easily understood by other cultures. (P10)
DISCUSSION Upgrading assessment skillsThe students recognised the importance of improving their palliative care assessment skills, including the need to prepare before conducting patient assessments. They engaged in discussions with their peers and healthcare professionals regarding their challenges. Although this study did not investigate student attitudes toward caring for endof-life patients, it is recommended that their knowledge and attitudes in this regard are aligned and reinforced.[10] Muliira et al.[10] discovered that the attitudes of the respondents in their study were not aligned with their limited knowledge. Their lack of knowledge included an inability to comprehend patients’ symptoms, such as delirium, cancer pain, and dyspnoea, as well as an inability to recognise the side effects of opioids. The course content should prioritise incorporating palliative care principles to boost students’ comprehension of symptom control, psychological and spiritual care, and pain management.[11] Although pain management is often covered in courses, other symptom management and nonpharmacological approaches receive inadequate attention. Moreover, teaching about palliative care emergencies, as well as ethical and legal dilemmas, is often lacking.[12] A thorough understanding of fundamental concepts is imperative for nursing students. Inadequate knowledge may arise because of deficiencies in the curriculum, such as in its design and implementation, nursing educators, or the pedagogical practices employed in nursing student education.[10]
Contributing influences in the assessment processThe researchers in this study found that assessing patients with unstable conditions posed a challenge and required a particular approach to conducting an accurate palliative assessment. Incorrect assessments may lead to incomplete data collection. Many students lack an understanding of the role of palliative care in non-pain symptom management.[13] Therefore, it is crucial that students receive sufficient training in accurate symptom assessment. Nursing students participate in various clinical placements that involve individuals who require palliative and end-of-life care across hospital and community-based environments.[12] Students of nursing must capitalise on the opportunities that arise in these settings to enhance their education.
The way the patient responds to the assessmentThe present investigation examined whether the students acknowledged that the patients’ answers to inquiries were affected by their physical state. In the palliative care field, it is important for students to learn strategies for interacting with patients who have various health conditions. The provision of a course on palliative care enables students to improve their ability to communicate with patients and their families, as well as understand patients who may be emotionally or behaviourally unstable.[14] It assists in developing the necessary skills for compassionate and effective care in a challenging setting.
Replenishment of dataIn the present study, students recommended that their training includes classroom demonstrations to better prepare them for palliative care practice, including gaining familiarity with the tools and forms used for palliative care assessments. As students had varying understandings of the tool, further explanations were requested regarding specific questions, such as those relating to spiritual and psychological aspects. Because of the scarcity of specialist providers for clinical placements in palliative care, it is recommended to enhance students’ learning. The pedagogical approach involves lecturers’ role-playing, along with supervised experience and simulation. The curriculum covers a range of topics, including coping, bereavement, and palliative care philosophy, to varying extents.[12] In one study, nursing students had a low level of understanding of palliative care, including the principles and philosophy behind it, as well as pain and symptom management and psychological and spiritual care.[11] However, some students do recognise the importance of palliative care and the significance of receiving palliative education.[15] Nonetheless, their ability to provide adequate palliative care may be deficient as evidenced by insufficient knowledge and preparation in this field, as well as inadequate symptom assessment abilities, as highlighted by Sadhu et al.[16]
The importance of family involvementFamily involvement was acknowledged by the participants in this study. Effective palliative care learning necessitates student participation in care, the cultivation of amicable relationships with patients and family carers, and the nurturing of internal factors conducive to practical learning.[6] Delivering palliative care is an emotionally arduous task, and novices can feel unpracticed and unsure of themselves. Accordingly, when faced with intricate patient situations in the presence of their respective families, nursing students are inclined to defer to expert nurses who can bestow the necessary assistance.
Emerging issues in the assessment processIn this study, cultural sensitivity was investigated, with a focus on using language that patients could readily understand. If communication problems arose, students sought assistance from colleagues with a similar cultural background to the patient. Brooks et al.[17] identified a scarcity of information on how clinicians evaluate patients and their families in palliative and end-of-life care, particularly with respect to culturally specific needs, such as spiritual needs. However, like in the current study, Brooks et al.[17] identified a range of options for spiritual care, including translation services and cultural background matching during the assessment process to address differences in values. Communication with patients with different languages or backgrounds has been identified as a primary obstacle for nurses, and to address this challenge, nurses should improve their communication techniques when discussing sensitive topics with patients.[18] Cicolini et al.[19] emphasised the importance of training for nurses to enhance their cultural competency. This will ensure that nurses can act as role models for nursing students in acquiring this competency. Training nurses, including student nurses, in history-taking skills and disease management would be advantageous when considering cultural sensitivity.[18]
Approaches to assessmentThe exploration of students in this study highlighted that the duration of their clinical placement was insufficient and failed to adhere to the ideal time frame. Therefore, a longer period is required to acquire relevant clinical experience in palliative care in an Indonesian context. In general, formal teaching in this area is delivered through seminars and tutorials.[12] Nursing students who opt for palliative and end-of-life care as their subject are constrained by restricted clinical placements, impeding their learning opportunities. Challenges in enhancing education in this area emerge from inadequate teaching time and insufficient clinical placements with palliative care providers, as noted by Heath et al.[12] They stated that as nursing students progress through their training, they encounter various clinical placements, including hospital and community-based settings, where individuals with palliative and end-of-life care needs may be present. To improve future nursing professionals’ levels of palliative care knowledge and skills, training programmes should include strategies that facilitate palliative care knowledge and skill acquisition. For instance, the researchers in Oman, engaged in interdisciplinary palliative care education and training, are deliberating over strategies for the development and assessment of palliative care adoption in all nursing programmes throughout the country.[10]
Refining the assessment processPalliative care assessment is a crucial element of the nursing process as it facilitates a thorough understanding of patients’ needs. It is imperative to avoid any unnecessary delays in this stage of the nursing process. Utilising an established assessment form can enable nurses and nursing students to conduct palliative care assessments effectively. The palliative assessment form for nursing students includes an evaluation of the bodily system and a review of the nine primary symptoms commonly found in patients: pain, shortness of breath, nausea, anxiety, anorexia, depression, fatigue, drowsiness, and worsening condition. It also entails an inquiry into psychosocial and spiritual considerations. Khraisat et al.[11] highlighted the inadequacy of the current palliative nursing education in a Middle Eastern country provided in the curriculum, indicating an urgent need for the integration of palliative care nursing education into nursing programmes. With the escalating demand for palliative care in the future, nursing students must receive an education emphasising interprofessional collaboration to address endof-life care while considering patients’ rights and interests.[15] It is crucial for nurses to engage in reflection and learning to understand the advantages of collaboration when managing complex situations.[20]
This research study was limited by the selection of participants from one university in the province of West Kalimantan. To enhance conceptual transferability at a nationwide level, it is recommended that further research should be conducted with a larger and more representative sample of nursing students from other universities in more than one province. An additional constraint of the present investigation is that it was conducted solely in one location, meaning that the researchers cannot extrapolate definitive conclusions based solely on this study.
ImplicationsThe study’s outcomes provide valuable insights for enhancing the quality of education and nursing practice services, primarily in carrying out palliative assessments for patients suffering from severe or life-threatening ailments. The findings furnish updated information on the requirements and experiences of students in performing palliative assessments in a user-friendly assessment format.
This study sought to explore the experiences, challenges, and barriers faced by nursing students when undertaking palliative care assessments. Furthermore, the study investigated supportive interventions used by these students during such assessments. The findings of this research offer valuable insights for academic nurses and nurse practitioners seeking to recommend appropriate palliative assessments based on the signs and symptoms observed and experienced by patients. Eventually, a custom evaluation instrument could be designed for individuals nearing the end of their life.
CONCLUSIONThrough conducting an interpretive phenomenology analysis, data were generated to explore the factors that influence student experiences during palliative care assessments. The findings indicate that further practice is required for students to enhance their skills. This study has heightened nursing students’ awareness of the necessity to improve their assessment abilities and the forms they use. It was discovered that familiarising oneself with assessment tools through classroom simulations before commencing clinical placement was advantageous for students. The present investigation suggests that there should be an increased emphasis on educational establishments developing a suitable curriculum in palliative care that meets the requirement to enhance the quality of palliative care in the future.
留言 (0)