Worldwide, every year, an estimated 56.8 million people need palliative care. Only 14% of needed people globally receive palliative care needed.[1] Of 20 million patients with a life-threatening illness around the world, only 3 million patients receive palliative care services. The World Health Organization (WHO) has undertaken several measures to improve and provide palliative care services in the healthcare systems of low-middle-income countries. However, these measures have faced various hindrances during its implementation.[2,3] The need for palliative care will continue to grow worldwide as a result of an increase in the aging population and the increasing burden of non-communicable diseases and some communicable diseases. The number of deaths due to noncommunicable diseases in 2019 accounts for 74% of all deaths. By 2040, it is estimated that 75–88% of palliative patients could benefit from palliative care.[4] In India, around 7 million people may need palliative care.[5] Various initiatives like the national programme for palliative care were launched by the government as a part of ‘Mission Flexipool’ under the National Health Mission to improve the quality-of-care service delivery.[6]
Community-based palliative careIn Tamil Nadu and Puducherry, though there are many studies on palliative care services. Studies on home-based palliative care are limited. Our college provides palliative care services for sick people and the needy through field practice in urban as well as rural settings of the Villupuram district of Tamil Nadu. We have enrolled a list of palliative care patients from the villages under the service area of our college by healthcare providers through house-to-house visits. Each patient has a case sheet which comprises the clinical condition as well as their treatment and follow-up. Palliative care visit is scheduled monthly, once with two follow-up visits per patient, and we cover a maximum of 10 km per visit. We cover patients who are less compliant with medication and care, and priority is given to these patients. Totally 37 palliative care patients were covered in both the Urban Health Training Centre (UHTC) and Rural Health Training Centre (RHTC). Prior intimation is given to healthcare providers regarding the next day’s visit and to prepare for the visit. As a part of the community-based palliative care program, the monthly training program is conducted to train the healthcare providers (Junior residents, auxiliary nurse and midwife [ANM] and Medical social workers [MSWs]) on topics definition of palliative care, who needs palliative care, where to approach for palliative care, types of care for palliative care patient and counselling services for family members. All the palliative care patients were provided care for bed sores, diabetic foot ulcers, wound cleaning and dressing, treatment for minor ailments such as fever and cough and treatment of comorbidities such as diabetes mellitus and hypertension. Provision of multi-vitamin tablets, urine bags, catheter, dressing material, etc.; provision of rehabilitation services through NGOs and physiotherapy for palliative care patients.
Especially in COVID times, identification of COVID cases and treatment given. Referral services for severe cases to tertiary hospitals and provision of raw ingredients for cooking were also given to palliative care patients. The service is provided by a group of healthcare providers such as postgraduate/medical officers, Junior Residents, ANMs, and MSWs. Identifying gaps in palliative service is a requirement for developing end-of-life care in non-palliative care settings, which have not been explored adequately. Hence, it is needed to know how patients at the end-of-life stage are cared for from the healthcare provider’s point of view. Our college has been providing community-based palliative care since 2009. Initially, the palliative care program was started in collaboration with the Institute of Palliative Medicine (IPM), Calicut. As a part of the evaluation of community-based palliative care programs, this study was conducted to explore the difficulties faced by healthcare providers.
Operational definition Palliative carePalliative care is an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial, or spiritual.[1]
Palliative care patientsPalliative care patients include patients with cancer, human immunodeficiency virus/acquired immunodeficiency syndrome, dementia, progressive neurological disorders such as Parkinson’s disease, multiple sclerosis, motor neuron disease, stroke, and paralysis; progressive systemic diseases such as chronic obstructive pulmonary disease, and interstitial lung disease and heart diseases, liver and kidney dysfunctions due to various causes, debility of old age and other degenerative disorders.[7]
MATERIALS AND METHODS Study setting and periodThe present study was done in the Department of Community Medicine, Sri Manakula Vinayagar Medical College and Hospital, Puducherry, a tertiary care teaching hospital in South India. Data collection was done between the period of January 2023 and March 2023 (3 months). Our healthcare providers have been providing community-based palliative care for the past 15 years and provide care through different seasons of the year. Our healthcare providers were trained and qualified in palliative care. Both of our MSWs have completed a fellowship in palliative care at the IPM WHO Collaborating Centre for Community Participation in Palliative Care and Long-term Care, Kozhikode, Kerala. Comprehensive palliative care is provided by a group of healthcare providers such as staff nurse, ANMs, MSWs, Junior Residents and Medical officers; which addresses physical, social, psychological, psychosocial and spiritual problems for patients. Community palliative care was provided for all the villages around our peripheral institution which is the RHTC as well as UHTC which is situated at Thiruvennainallur and Villupuram, respectively. In UHTC, there are around 17 palliative care patients who are non-ambulant (1), cancer patients (1), old age patients and bedridden (1), mental retardation (3) and central nervous system (CNS)-related disorders or disease (12). While in RHTC, 20 palliative care patients are non-ambulant (3), bedridden and old age (2), CNS-related disorder or disease (14), and cancer patients (1). Home care visits improve compliance as the patients are treated in their comfort zone (home/doorsteps). Among the palliative care patients, 60–70% of patients were compliant while the non-compliance comprises 30–40%. Non – compliance patients were visited once in 2 weeks while patients with good compliance were visited monthly once.
Study design and study participantsParticipatory research action (PRA) techniques, one of the qualitative research methods, consist of a cobweb diagram, social mapping, seasonal calendar, force field analysis, Venn diagram, pairwise ranking, etc. Systematic technique is also a qualitative research method comprised of free listing combined with pile sorting, Delphi technique, etc. We decided to follow both PRA techniques as well as Systematic techniques in this study. The study was conducted among Junior Residents (6), ANMs (4), and MSWs (2) who were trained in providing home-based palliative care for the patients.
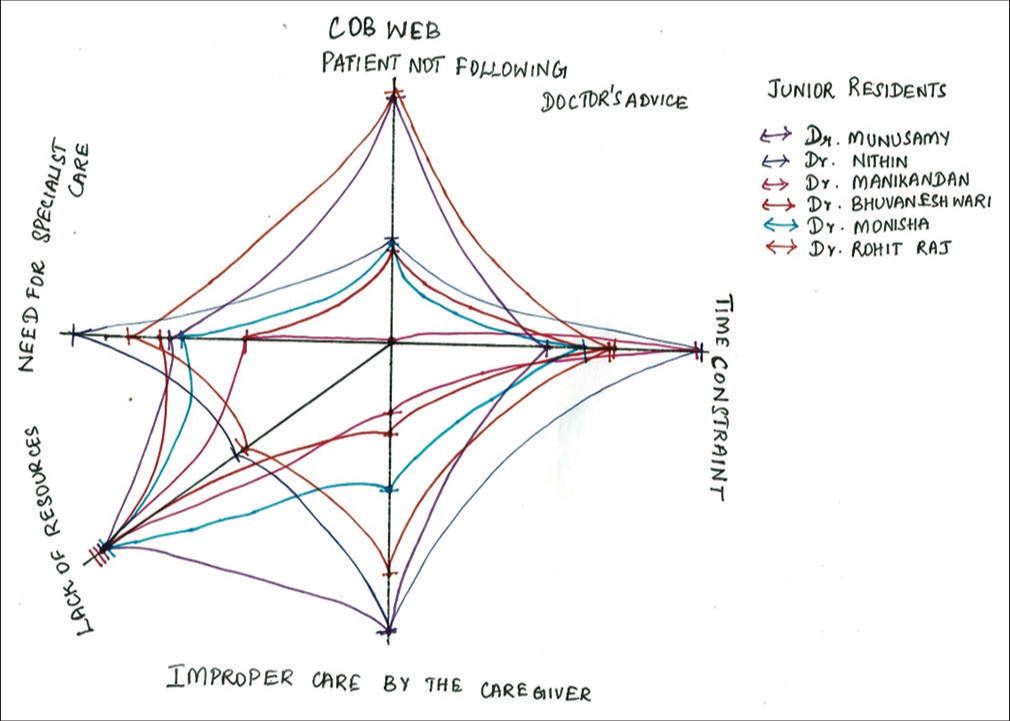
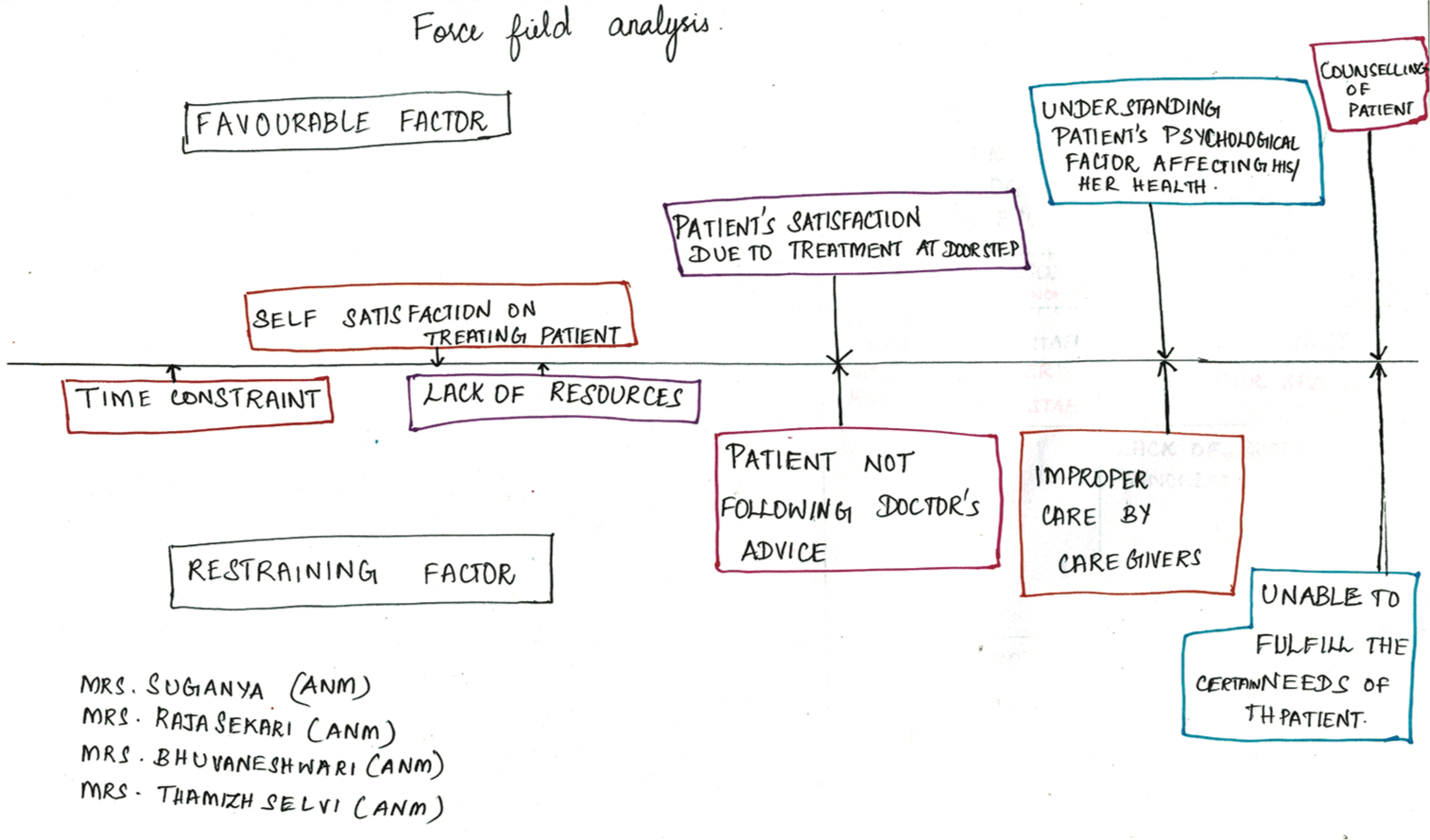
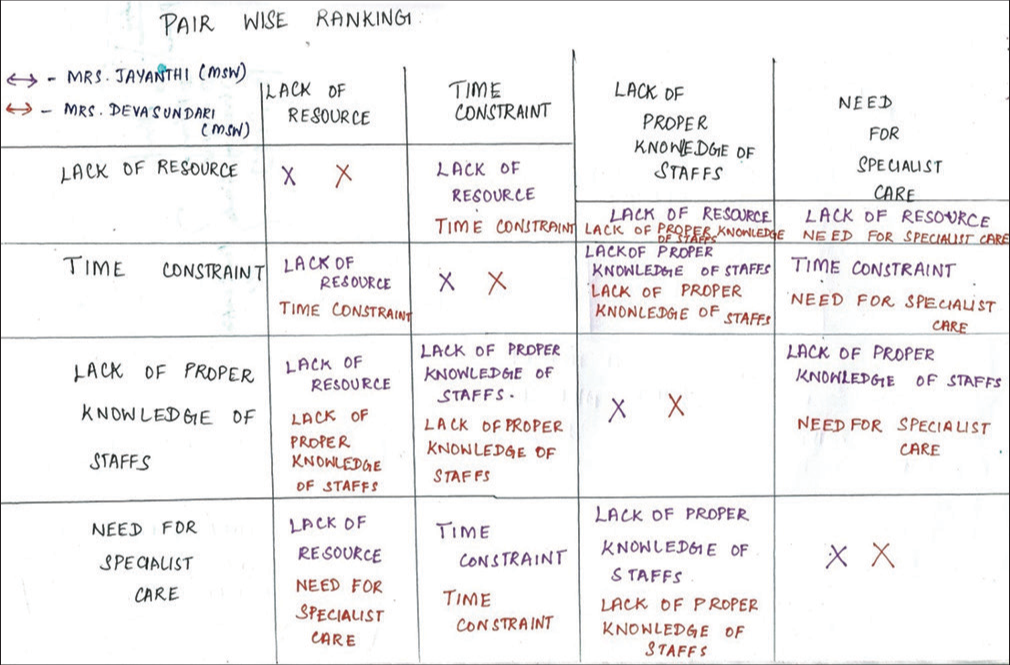
Data collection and procedureInitially, participants were sensitised to PRA techniques. Later, participants were divided for each PRA technique. Faculty and postgraduates trained in qualitative research methods have done the technique after obtaining informed consent from the participants. The technique was conducted in UHTC and RHTC centres, respectively, for around 3 months from January to March 2023 and the technique was conducted for 40 min per PRA technique. The cobweb diagram is one of the PRA techniques conducted among 6 Junior Residents in RHTC and UHTC, respectively, during their postings. Junior Residents expressed the difficulties faced by them during the palliative care visit and those difficulties were enlisted and then plotted to form a cobweb. Force field analysis, a PRA technique carried out among 4 ANMs who were working in RHTC. The driving force and restraining force were derived and plotted with the data collected from ANMs. Pairwise ranking is another PRA technique conducted among 2 MSWs at UHTC and RHTC, respectively, data collected from MSWs were derived and plotted. The interview guide/questionnaire for the PRA technique includes what are the enabling or driving factors in providing palliative care services and the restraining forces or challenges faced during palliative care services, especially home visits. We conducted the Delphi technique among a panel of six experts involved in providing palliative care services from all over Puducherry. Mail communications were sent to the experts to suggest solutions for the challenges faced during home care visits.
Ethical issuesInformed consent was obtained from the participants before conducting the study.
Analysis and interpretationIn the techniques, open-ended questions were asked of the participants. The interview was audio recorded and key points were noted down separately for each PRA technique. The interview was translated into English. The manual content analysis was done on transcription prepared from the discussion of PRA. The qualitative data were effectively captured using this PRA technique. Transcription of qualitative data was done using Atlas ti, version 5.0 software. The statements evolved from all Cobweb, force field analysis and pairwise ranking were grouped. The codes were by the information from the direct statements which are double quoted. These codes were grouped into categories.
RESULTSDifficulties faced by Junior Residents were derived and plotted based on priorities and joined to form a cobweb, as shown in Figure 1. Difficulties were time constraints; lack of resources such as medications for other complaints and transport facilities; need for specialist care and non-adherence to medical advice like a patient not following the advice properly.
Export to PPT
For time constraints, a Junior Resident said, ‘Time to visit a patient was less, we have to hurry and return very soon, and the number of visits per month is also inadequate for each patient.’ Lack of resources was another difficulty faced by other Junior Residents. ‘Medications for other complaints such as anti-epileptic tablets, some antidiabetic drugs, and insulin injections were not available, and transport facilities were also not available on scheduled time.’
Another Junior Resident said, ‘Though we treat the patient properly and on time. The patient fails to follow the advice given to them. Thus, their condition doesn’t improve or even worsens’.
A Junior Resident stressed the need for specialist care, ‘Few patients needed care from certain specialities such as in case of cataract, corneal ulcers and chronic otitis media, which should be attained by the respective specialities.’
Force field analysis to explore the driving force and restraining forces for palliative care was derived from ANM and plotted, as shown in Figures 2 and 3. It includes favourable factors such as self-satisfaction with treating the patient, patient satisfaction like treatment at the doorstep, understanding the patient’s psychological or social factors affecting their health, skill development, and counselling of the patient. The restraining factors of the healthcare providers in providing palliative care services are time constraints, lack of resources, patient not following the advice properly ,improper care by caregivers and unable to fulfill certain needs of the patient. Psychosocial as well as spiritual factors were found to be a hindrance to proper compliance of the patients.
Export to PPT
Export to PPT
One of the ANMs stated, ‘I was feeling satisfied that we were able to treat the patient symptomatically and improve the patient’s condition, and also patient was happy as they received treatment at their doorstep, a mutual benefit which made me actively involved in providing palliative care.’ Similarly, she said, ‘I felt that we need to increase the number of visits per month and also spend some more time with the palliative patient.’ Patients welcomed us with open arms and were eager as they did not have to travel far for treatment. Home care visits improve compliance as the patients are treated within their comfort zone (home/doorsteps).
Pairwise scoring/ranking was done for MSWs by plotting the issues faced in palliative care as rows and columns, as shown in Figure 4. The difficulties found were time constraints, lack of resources, lack of proper knowledge of staff, and need for specialist care.
Export to PPT
An MSW (participant) said that ‘Time spent for each patient was not adequate and the vehicle was not available as scheduled time.’ Based on the findings, the difficulties were derived as codes and plotted [Table 1], and the overall conceptual framework of the PRA techniques used was depicted in Figure 5.
Table 1: Barriers faced by healthcare providers during home visits.
Barriers I felt that we needed to increase the number of visits per month and also spend some more time with the palliative patient. Time constraint Medications for other complaints such as anti-epileptic tablets, some antidiabetic drugs and insulin injections were not available and transport facilities were not available on scheduled time. Lack of resource Although we treat the patient properly and on time. The patient fails to follow the advice given to them. Thus, their condition does not improve or even worsens. Non-adherence to treatment Some of the staff need proper training in palliative care Training on palliative care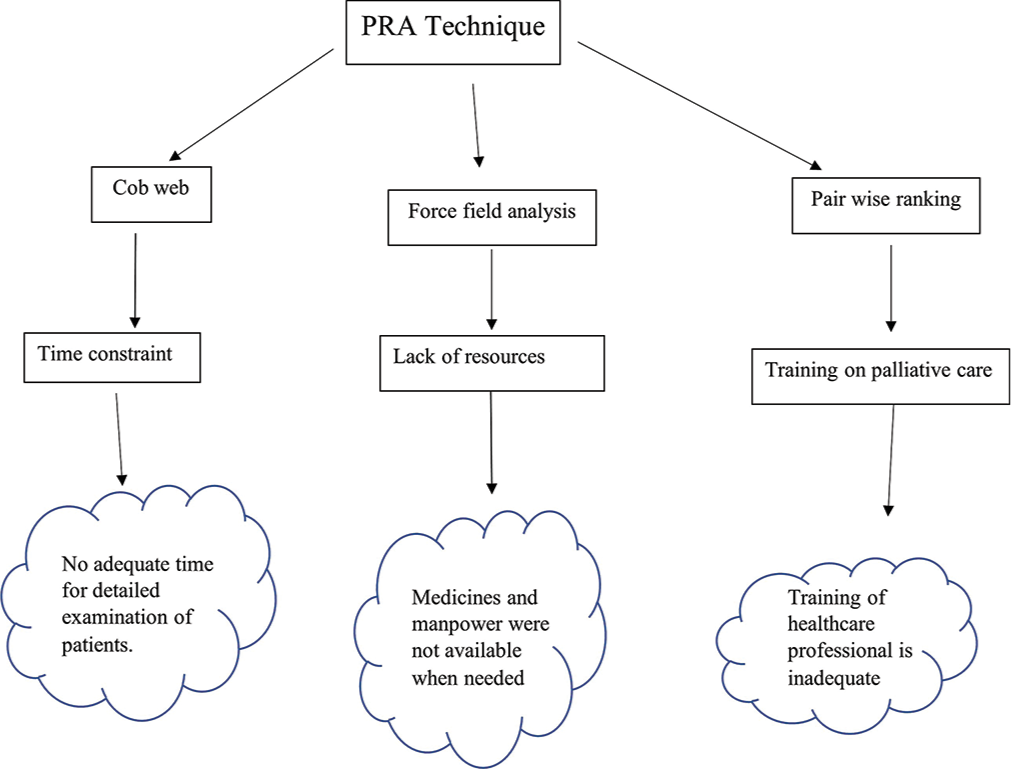
Export to PPT
The experts have arrived at a consensus regarding possible potential solutions that they were properly planning to reduce time constraints, more intense counselling of patients on adherence to treatment and care, and increase the frequency of hands-on training for newly joined staff and junior residents to overcome the practical difficulties in wound care and dressing and assessing the vitals. Arrangements of monthly special camps for those who are in need of specialist care.
DISCUSSIONWorldwide, several studies have been conducted to assess the challenges in the provision of palliative care services. In this study, we found out the various difficulties faced by the healthcare providers of palliative care while providing care to palliative patients. The healthcare providers face a lot of difficulties like inadequate time to visit a patient; non-availability of transport or vehicle; patient not following doctor’s advice; need to address other complaints of the patient; some staff needed proper training; caretaker needs counselling in taking proper care over the patient and unable to fulfil the needs of the patient. These factors cause hindrances in providing proper care to palliative patients. These difficulties need to be looked at to improve the quality of providing palliative care to palliative care patients. Similarly, a study was conducted in low-middle-income countries to assess barriers and challenges in the provision of palliative care. In the study, the same issues, like lack of resources, which are one of the hindrances in providing palliative care in low-middle income countries, were found. It also denoted improper infrastructure and financial constraints being factors that prevent the delivery of proper palliative care in low-middle-income countries.[2] In many low-middle-income countries, palliative care services are not available, which leads to many challenges, such as the significant gap between demand and supply of services, lack of resources, limited infrastructure, as well as manpower and finances. A similar study was conducted in South India to evaluate the training program on palliative care developed for Junior Residents. The study denoted that palliative care provided was inadequate, thus creating a healthcare provider needing proper training.[8] A study conducted in the Eastern Mediterranean Region found that the caregivers did not provide or adhere to the advice given by the healthcare providers. Moreover, there was limited availability of medications such as anti-epileptics, antipsychotic drugs, insulin injections, few antihypertensive and antidiabetic drugs for providing to palliative care patients.[9] A study in the USA focused on challenges to integrating palliative care; in the study, they formed the barriers into three domains such as education domain, implementation domain and policy domain. These reflected the lack of resources and inadequate training of the healthcare professionals.[10] During the COVID pandemic, there were many difficulties in delivering palliative care, scarcity of data on palliative care needs and interventions given during crises, challenges of care delivery, particularly due to improper pain relief resources and inadequate guidelines for it, a lack of uniformity on the ethics of providing, limitation of palliative care as part of humanitarian healthcare response and the importance of contextually appropriate care. Palliative care has become a significant approach to improving the quality of life of these patients. The necessity for better communication with healthcare providers was also reported in some studies. Spending time and conversing the important issues with patients have been identified as the family’s needs.[11-14] There were many lacunae in these studies and these studies were done mostly in developed and urban areas. Our study has filled these lacunae by covering most of the difficulties faced by healthcare providers who provide care to palliative care patients, especially in a rural setting of Tamil Nadu in Villupuram district.
CONCLUSIONIt helped to identify the various difficulties faced by healthcare providers and to plan for solutions in future palliative home care visits. Specialist care in case of cataracts, corneal ulcers, and chronic otitis media needs to be addressed. Scheduling of frequency of specialist visits needs to be planned prior.
LimitationThe palliative care barriers on three levels: individual level, family level, and community level were not covered fully.
留言 (0)