Palliative care (PC) is defined by the World Health Organization (WHO) as ‘an approach that improves the quality of life of patients and their families who are facing problems associated with a life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial, or spiritual.’[1]
The ageing population phenomenon and the growing prevalence of non-communicable diseases are responsible for a strong global demand for PC.[2,3] Globally, it is estimated that each year, over 56.8 million people need a PC.[4] Most of them (67.1%) are adults over the age of 50, and at least 7% are children.[4] Yet, non-communicable diseases account for nearly 69% of adult needs.[4]
However, PC is less developed in most countries of the world.[4] Apart from North America, Europe, and Australia, access to quality PC remains very limited, although 76% of the needs are in low- and middle-income countries.[4]
Indeed, the extant literature has identified a range of barriers limiting access to PC services, including a lack of trained PC healthcare professionals.[5] Advanced practice registered nurses (APRNs) are essential PC providers and members of the interdisciplinary PC team.[6]
In 2020, the International Council of Nurses (ICN) highlighted advanced practice nurse (APN) as a generalist or specialist nurse who, through further higher education (at least a master’s degree), has acquired the skills necessary for advanced nursing practice (ANP) in which the nurse will be authorised to practice.[7]
The training of APNs is implemented in the country. In 2013, the universitarisation of health sciences was carried out in Morocco through the Higher Institute of Health Sciences (HIHS), providing a comprehensive bachelor’smaster’s-doctorate training cycle in health sciences.[8]Subsequently, in 2016, the HIHS accredited a master’s degree program in advanced healthcare practice. Furthermore, in 2022, the Higher Institute of Nursing Professions and Health Techniques introduced a master’s degree specifically focused on advanced practice in oncology and PC.[9] Themaster’s cycle comprises a 2-year training program leading to certification in advanced practice in health sciences. This certification is available for both professionals and students who hold a bachelor’s degree in nursing sciences.
Internationally, ANP is needed as a policy recommendation to expand the quality of care[10], and the roles of APNs are expanding as there is an increased need for specialist nursing care at an advanced practice level.[11] Nationally, there is an increased demand for nurses qualified in PC and a lack of legislation governing the role of APNs in PC, which requires a consolidation of the role so that it is accepted by the public to avoid overlap between the roles of the different professionals.
ObjectivesThis article aims to achieve the following objectives:
To outline the background of ANP in PC, its interest, and training needs
To put forward recommendations for its establishment in the Moroccan healthcare system.
MATERIALS AND METHODS Study designThe present study was conducted to identify and summarise the current knowledge on APNs and their role in PC at an international level by studying the impact of this role on outcomes and the training needed to acquire the necessary skills.
This review was carried out according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guideline, Edition 2020.[12]
Inclusion and exclusion criteriaThe inclusion criteria were: (1) studies published between 2012 and 2022; (2) studies written in English; (3) studies published in the field of nursing.
The exclusion criteria were conference abstracts, pathways, letters, textbooks, and studies that do not mention the contribution of the APN ANP in the field of PC.
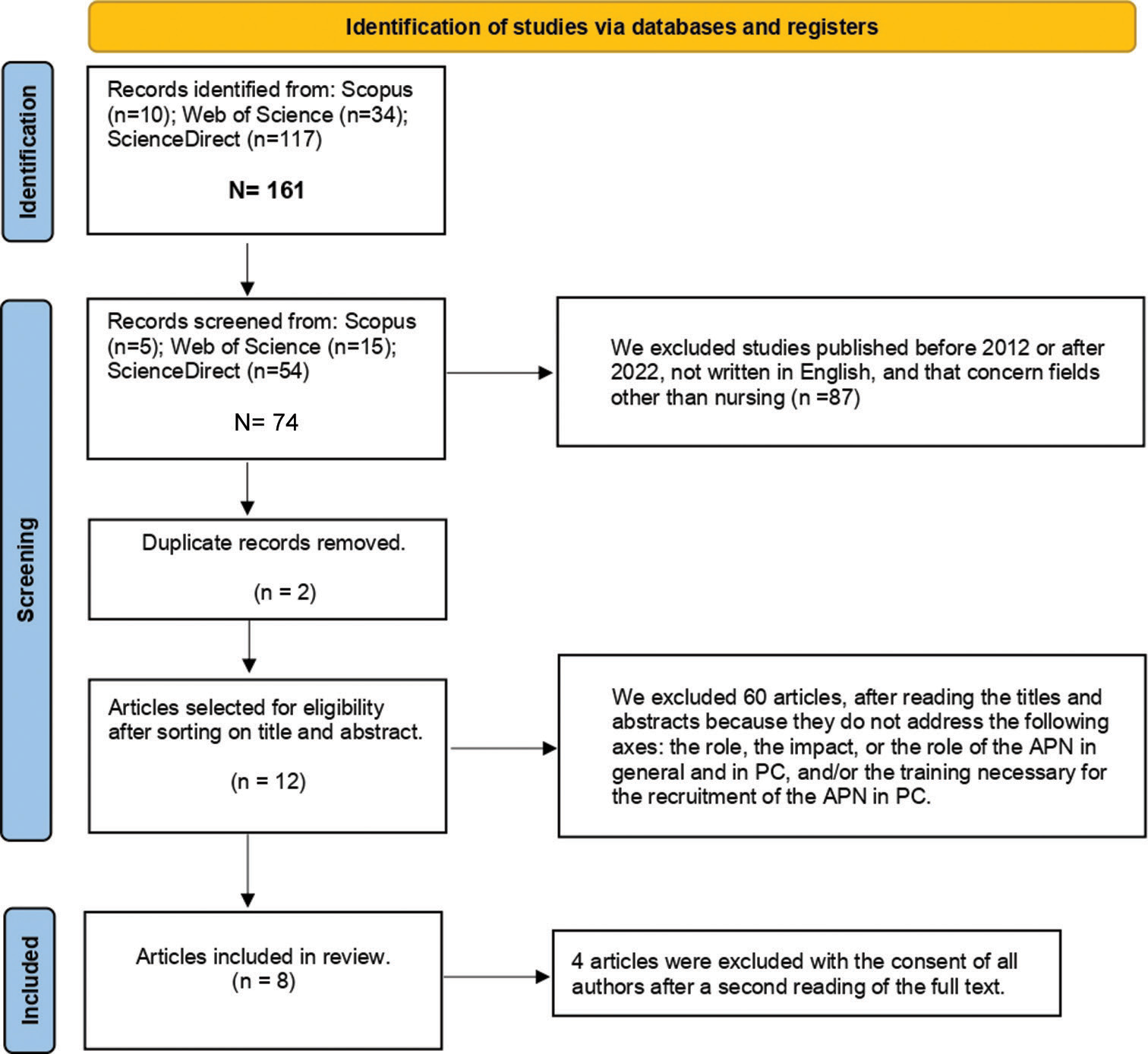
Literature search and strategyRelevant studies were searched using online scientific databases available through IMIST/CNRST, including Scopus, Web of Science, and ScienceDirect, published between 2012 and 2022. The full process, illustrated in Figure 1 (flow diagram), was conducted from 10 to 27 July 2023.
Export to PPT
The keywords used during the search were: ‘Advanced nursing practice’ and ‘palliative care,’ attached by the logical Boolean connector ‘AND.’
The flow diagram Figure 1 shows the sorting process. The recording through database searching was n = 161 (Scopus = 10; Web of Science = 34; ScienceDirect = 117). Seventy-four studies were found to be potentially relevant following the screening. Sixty-two studies did not meet the inclusion criteria, and 12 articles were identified from the title and the abstract screening. Finally, eight relevant studies were included in this review after a second reading to refine eligibility after mobilising the AGREE II tool.[13]
Data extractionThe following three biases were assessed to eliminate the risk of data gathering, namely selection bias (to avoid a random selection of studies, this review defined inclusion and exclusion criteria), detection bias (to ensure that the study is exhaustive and that all the relevant studies were identified, this review attempted to obtain information from the various databases available) and interpretation bias (to guarantee an objective interpretation, reading committee with five members were involved in the evaluation and synthesis of the studies).
Moreover, at the final step of the selection process, the quality analysis was assessed using the AGREE II tool developed by Brouwers et al., updated in 2016,[13] for greater accuracy and neutrality and to ensure the final selection. This grid contains 23 items, grouped into six areas, which were evaluated for each study selected, scope and purpose, stakeholder involvement, the rigour of development, clarity of presentation, applicability, and editorial independence. All items are assessed using a Likert scale from 1 (Strongly disagree) to 7 (Strongly agree).
RESULTS Article selectionAs shown in the flow diagram, eight articles were selected from 161 articles. The characteristics of the selected studies with the details: Title, author(s), year publication, aim, material and methods, and relevant notes are summarised in Table 1.
Table 1: The characteristics of the articles obtained.
Title Author (s) Publication year Material and methods Aim (s) Consensus points Role of the APN in PC.[15] George 2016 Short report containing a literature review. Explore the context ofthe APN, its importance, and its significant role in PC through a review ofthe literature. The report deals with the definition of PC and the APN, as well as the role of the APN in PC and the training required for this profile. PC advanced practice nursing in Israel: Bridging creation and implementation.[16] Collett et al. 2020 Document analysis and key informant interviews. Explore the development of the role of the APRN in other specialties based on the description of the development of the APRN in PC in Israel. The article discusses the definition of PC, the definition of the APN, their role in PC, the training required, and the limitations and recommendations of the profession. A framework for integrating oncology PC in DNP education.[17] Fennimore et al. 2018 Organisation of a 2-day course with the support of the National Cancer Institute. Improving the integration of PC in oncology into the DNP program through the development of a training program by PC experts and qualified DNP teachers. The role of APRNs in PC, as well as training challenges and recommendations related to the practice of this profession, was determined. A review of advanced practice nursing in the United States, Canada, Australia and Hong Kong SAR, China.[18] Parker and Hill 2017 Review Discuss and give an overview of the role of the APN, based on topics identified by the China nursing network the countries and regions highlighted in the title. The review covers the background of the APN, its scope, its role in PC, and the prospects/recommendations for the preparation of training, prescribing and the accreditation system. The review also noted the importance of a performance evaluation system and legislative requirements in the light of local conditions. The impact of ANP role on adult patients with cancer: A quantitative systematic review.[19] Alotaibi and Al Anizi 2020 Quantitative systematic review and thematic analysis Recognise how ANPs contribute to oncology care. This review identifies the definition of the APN, its role in PC, and the limits encountered when the APN was introduced. Integration of APPs into the Israeli healthcare system.[20] Aaron and Andrews 2016 Integrative Review In order to promote the status of APPs in Israel as a solution to the shortage of medical and paramedical staff, the authors have described the factors and obstacles favouring the implementation ofAPPs at international level, based on the recognition ofAPPs, their roles, and the necessary education, while analysing their impact on the safety and quality ofthe care provided. The review revealed the definition of the APN (APPs), its contributions and the advantages of its interventions, its skills, its training and underlined the need for the APN in PC. The hospice and PC APRN workforce: Results of a national survey.[25] Pawlow et al. 2018 An online survey distributed nationally. Describe the contributions of APRNs in PC, the obstacles to their practice, and their training needs. The study shed light on the effects of APNs and highlighted their contributions to PC. It also addressed the future efforts that need to be provided on the educational, regulatory and professional sides, to develop the APNs workforce in PC. An APN coordinated multidisciplinary intervention for patients with late-stage cancer: A cluster randomised trial.[30] McCorkle et al. 2015 A cluster randomised controlled trial. Assess, at the clinical level, the effects of an intervention provided by a multidisciplinary team coordinated by APNs for patients newly diagnosed with late-stage cancer by studying the results obtained from the interventions. The study highlighted the contribution of the interventions provided by the multidisciplinary teams coordinated by the APNS on the quality of patients’ lives. The impact of the role of the APN in PC was also mentioned, as was the need for a PC module in training.The studies selected were published in English between 2015 and 2020 and addressed the objective of the study.
After reviewing the selected publications, the results were summarised in the following areas:
Definition PC nursingPC has been recognised worldwide as a range of care offered to patients with life-limiting illnesses.[14,15] PC is specialised care aimed at relieving spiritual, emotional, physical, and social distress.[16,17]
George cited the WHO’s call for PC to join the medical specialty with an essential interdisciplinary nature.[15] He emphasised that PC is ‘an approach that improves the quality of life by treating the pain and physical, psychological and emotional symptoms of patients with life-threatening illnesses.’[15,17]
APNAPNs are independent nurses who make diagnoses and can interpret them, intervene, and issue prescriptions.[15,16] Moreover, Parker and Hill cited in 2017 that the specialisation of care provided by APNs is linked to that of medical settings. They add that the following tasks are approved for APNs: Guiding patients through the treatment process, assessment, prognosis, diagnosis, and prescribing medication.[18] In 2020, Alotaïbi and Al Anizi highlighted that Health Education England defines APNs as health professionals who have acquired the skills necessary to take on expanded roles.[19] In this respect, APNs are able to develop leadership in the provision of care and the training of nurses to improve health outcomes.[16]
According to the ICN and the International Federation of Nurse Anaesthetists cited by Aaron and Andrews, there are four options for the APN profession, including Certified Registered Nurse Anaesthetist, Certified Nurse Midwife, Clinical Nurse Specialist, and Nurse Practitioner (NP).[20] Indeed, In the US, the term APRN refers to one of the four recognised professions mentioned above.[18]
In the studies selected, NPs represented the most highly regarded profession. These nurses have the skills needed to contribute to initiatives and the ability to develop care protocols and innovate assessment approaches based on evidence gathered that can improve nursing practice.[18]
However, definitions of APN differ from one practice setting to another.[16,21] The legitimacy of the roles requires coherent definitions of the profession based on those adopted and accepted worldwide, with reference to the needs of the population and local health systems.[18]
Role and contribution of the APN in PCThe care provided by APNs has been proven to be effective, safe, and of high quality.[22-25] The demand for APNs has recognised an increase in their clinical expertise, leadership, and effectiveness as leaders of change on the health side and as a part of nurses’ careers.[18,26]
APNs are necessary care providers in interdisciplinary teams working in PC departments.[17,18,25] One of the areas in which the APN’s contribution is sought is oncology.[19] APNs play an important role in all phases of the cancer treatment process, they contribute to the PC.[19,15]
PC experts claim that APNs play an effective role in the care of patients with life-limiting illnesses.[6,25,27] Due to their knowledge of pharmacology psychology and their in-depth clinical skills,[15] APNs can meet the needs of patients and their families by promoting a positive death.[15,28] Besides, a study conducted by Schenker et al., in 2015 revealed that the PC provided by APNs was feasible and acceptable to the patients.[29,30]
Alotaïbi and Al Anizi cited that Bakitas et al., in 2019, have determined the roles of APNs in PC, namely communication and counselling with patients and their families, pain and accompanying symptoms management, advanced care offer, quality of life development and improving patient’s end-of-life experiences.[19,31] It was mentioned by McCorkle et al. that APNs facilitate the management of patients with advanced cancers by helping them to understand their disease and by offering PC integrated into complete cancer treatment to potentially prolong their life expectancy.[30]
Moreover, it was also highlighted that APNs have the necessary skills for anxiety relief and managing patients’ symptoms, which reduces the number of visits [19], and have leadership skills that allow them to work as administrators, specialists, clinical consultants, and researchers.[15,32]
To this end, APNs, in particular NPs, will increasingly take on active and efficient roles in primary and specialist PCs.[17] Then, APNs have skills that encompass the responsibilities of several workforces[15,33], and they can provide training in best PC practice by collaborating with other care contributors.[15,17]
PC-based training for APNsIn all fields, APNs must have at least a Master’s degree.[15,17-20] According to Health Education England, by 2020, APNs should be trained to master’s level, providing them with the knowledge and skills to take on expanded and defined roles.[19]
Whereas it was concluded that training should be specialised in a particular field, such as geriatrics PCs.[15] The American Society of Clinical Oncology recommended that healthcare programmes should include PCs.[30] However, if nurses are already practising as APNs, they can obtain a post-master’s certificate in PC offered by institutes or universities.[15,34]
Actually, nurses need to be trained to take on more complex care responsibilities.[18] To achieve this, university programme managers need to consolidate the basic nursing training programmes and recruit highly qualified teachers.[18] These programmes must be based on well-defined competencies for the role and the diploma.[18,35] A master’s programme based on the 3Ps (Physiology, Pathophysiology, and Pharmacology) was mentioned by Parker and Hill in 2017.[18] This programme focuses on the acquisition of the following skills: Planning, critical thinking, informatics, leadership, evidence-based practice, and evaluation.[18]
Furthermore, nurses can enrol in postgraduate training in a specialised field and complete a minimum of 500 h to obtain a license to practice in the US.[16,35] The same point was raised by George, who added that the training should be carried out in the year preceding the recruitment exam.[15]
As for Israel, it required 350 hours of didactic training and 400 hours of clinical training. The academic programme requires one year’s training at a state-recognised nursing school and 400 hours of internship in clinical practice supervised by a physician.[16]
Limits and recommendationsThe studies have identified a lack of clarity in the APN profession. Collett et al. noted that there is a need for a clear definition of the roles accorded to APNs and the authority of their practice since there are healthcare staff who are unaware of the qualifications of APNs and how to generate integration flows in the work departments.[16] In addition, Alotaibi and Al Anizi reported that this lack concerns the differences between hospital services and even the variations in context in each country.[11,19]
Furthermore, studies have mentioned the obstacles of the regulations governing the profession. Pawlow et al. highlighted that although the authorities have made efforts to improve legislation, restrictive regulations hinder the implementation of the scope of practice of APNs.[25] It concerns the power to prescribe and bill for homecare services and the independence linked to supervision by physicians.[25] However, Parker and Hill have determined that the legitimacy of this profile requires the acceptance of all those concerned,[18] and Collett et al. have proposed a consolidation of knowledge,[16,36] which can be increased by creating organisations that advocate the introduction of APNs and the increased use of this profile.[11,16,37] Indeed, the determination of a national definition is needed and must refer to internationally accepted definitions, mentioned in coherent documents that encompass all the data concerning the scope of practice of APNs.[18]
DISCUSSIONThe following key concepts were obtained through the relevant studies selected: The definition of PC and APN, its role in PC, the training required for this cadre in general and for PC practice, and recommendations/limitations to be considered when implementing this profession.
First, as for the PC definition, PC is a range of care offered to patients with a life-limiting illness. It consists of pain relief, symptom management, and emotional, social, and psychological support for patients and their families.[15-17]
Second, concerning the APN, S/He is a nurse who has acquired the knowledge and skills necessary to practise in an advanced field of expertise through at least a master’s degree.[15,18-20] APNs mobilise skills in service management, resource management, the provision of primary and advanced safe care, and leadership to improve the quality of care and access to healthcare services.[15-20,30] They can diagnose, prescribe, refer, bill, and act autonomously, as well as train and invest in health programmes, thanks to their in-depth knowledge.[15-20,30]
In addition, studies have shown the role of the APN in PC. They can work in a multidisciplinary team in a variety of services, and it has been shown in several studies that they can have a positive impact on PC services, given their knowledge, technical skills, and soft skills in psychology, psychopathology, and pharmacology.[15-20,30] In fact, it was recommended that PC training should be integrated into the training programmes of APNs.[15-17,30]
However, according to some selected studies, it was mentioned a few limitations that hinder the implementation of the profession. In particular, the definition must be well-defined according to the local context while respecting the recognised international guidelines.[16,18] Second, there is a lack of clarity of legislation governing this field of practice and a lack of knowledge amongst other providers about ANP and the remit intended for APNs,[16,18,19,25] which leads to authoritarian supervision of physicians and independence of practice.
Limitations and strengths of the studyThis study has some limitations that should be mentioned. In particular, the absence of studies dealing with ANP in the Moroccan context. In addition, the concepts of ‘APN’ and ‘PC’ are emerging in the national context.
However, this study is the first of its kind in Morocco, combining these two concepts to attract the attention of decision-makers, given that this profession is a solution to the shortage of nursing staff in this speciality.
Recommendations and implicationsWe recommend that the study be generalised by modifying the filters used in the first instance (year of publication, search field, the field of practice of the APN) to identify the contribution of APNs as a solution to the shortage of medical staff, which represents a major public health challenge.
As for the implications, the study approves that the implementation of the APN in the national health system is possible given the maintenance of training through the universitarisation of nursing care in the master’s degree, recognised internationally as a necessary degree for the training of APNs.
In addition, one of the departments recognising a shortage of staff and requiring a multidisciplinary team to manage patients is the PC department. The APN combines the skills of several professionals, making it the most appropriate solution for this shortage. It has been proven that the APN offers a polyvalent and high-quality range of care, given the technical and non-technical skills it possesses. This will be reflected in the quality-cost ratio.
CONCLUSIONThe integration of APNs has been introduced in numerous countries as a strategic response to public health challenges due to the notable advantages they bring to care provision. Within the realm of PC, APNs have demonstrated their significant impact by imposing specialised knowledge and expertise to effectively address the needs of patients with life-limiting illnesses and offer support to their families. This specialised knowledge is acquired through rigorous university training that aligns with the standards of the healthcare sector and academic programs. Nonetheless, the continued advancement of this profession necessitates well-defined legislation and heightened visibility amongst other healthcare providers, stakeholders, and patients.
留言 (0)