A scar results from tissue regeneration following an injury to the dermis. It can be elevated or depressed with altered skin texture, vascularity, and/or pigmentation with loss of adnexal structures. Histologically, it shows altered, dense fibrous tissue replacing the normal dermal components.1
Varying morphologies of scars have been described, such as linear, round, atrophic, cigarette paper-like, hypertrophic, or keloidal. The term varioliform scars, also termed pock-like scars and vermiculate scars, is often used to describe shallow, depressed, and sharply demarcated scars mimicking smallpox scars.1 Several dermatological disorders present with varioliform scars [Table 1]. We have attempted to classify, review the aetiology and provide a clinical approach to a patient with varioliform scars.
Table 1: Dermatological disorders with varioliform scars
S. No 1. Infectious disordersChickenpox
Smallpox
Papulonecrotic tuberculid
Secondary syphilis – pustular syphilis & lues maligna
2. Inflammatory disordersAcne necrotica
Lupus miliaris disseminatus faciei
3. Perforating disordersReactive perforating collagenosis
Generalised perforating granuloma annulare
4. Photosensitive disordersHydroa vacciniforme
Cutaneous porphyrias
5. Lymphoproliferative disordersPityriasis lichenoides et varioliformis acuta
Lymphomatoid papulosis
Hydroa vacciniforme like T-cell lymphoma
6. GenodermatosesDeposition disorder:
Lipoid proteinosis
Disorders with follicular keratosis:
Keratosis follicularis spinulosa decalvans
Ulerythema ophryogenes
Atrophoderma vermiculatum
7. OthersDegos disease
Degos-like lesions associated with connective tissue disorders
Atrophia maculosa varioliformis cutis
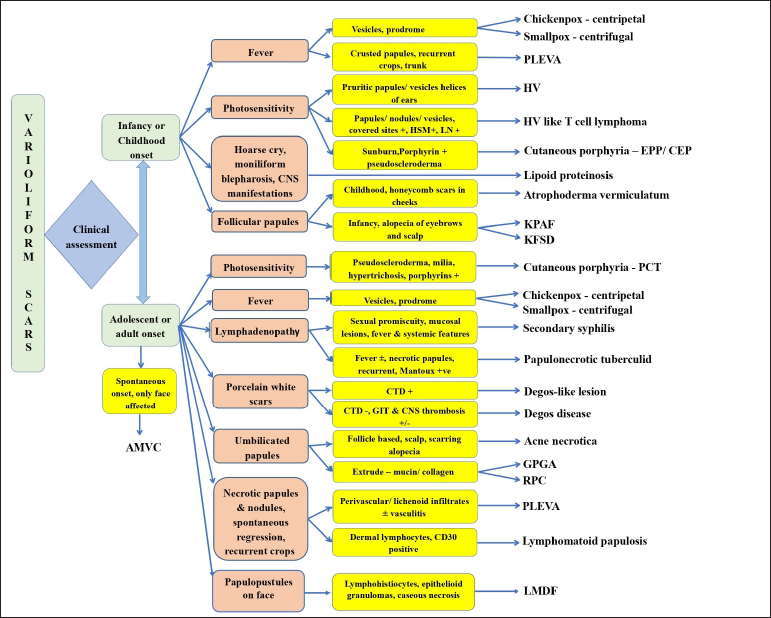
Varioliform scars can be broadly classified into two groups based on their distribution:
A brief review of various disorders are included under each subtype, along with their distinguishing features.
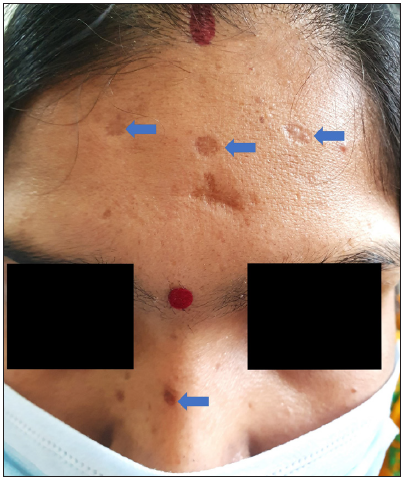
Disorders producing generalised skin lesions Chickenpox/VaricellaInfection with the varicella zoster virus (VZV) results in chickenpox, commonly affecting children. It presents with fever and self-limiting skin rash. The rash is polymorphic, which starts as macules and rapidly progresses to papules, followed by vesicles. Lesional crusting is observed in centripetal distribution, which resolve with hyperpigmentation with or without varioliform scars [Figure 1]. Sometimes mucosal ulcers can occur.2 Demonstration of multinucleated giant cells using a Tzanck smear is diagnostic.3
Export to PPT
SmallpoxSmallpox, caused by the Variola virus, was eradicated globally in 1980. It affected children and adolescents with a high fatality rate. It is common to come across survivors with typical varioliform scars on the face. The disease presented with a sudden onset of influenza-like symptoms and a monomorphic rash with centrifugal distribution. Lesions progressed from macules to papules to vesicles to pustules that formed scabs, leaving behind depressed scars [Figure 2].4

Export to PPT
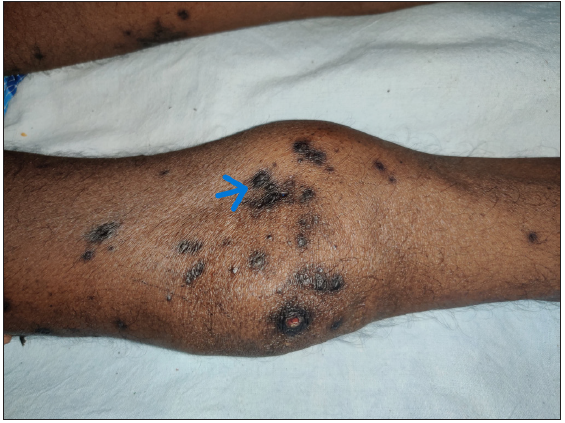
Papulonecrotic tuberculid (PNT)PNT is a cutaneous hypersensitivity response to Mycobacterium tuberculosis due to hematogenous spread. It is predominantly seen in young adults as a chronic, recurrent eruption of asymptomatic dusky erythematous necrotising papules with central ulceration and crust that resolve with varioliform scars. The patients usually lack constitutional symptoms. Common sites of predilection include extensor aspects of extremities, the trunk, face, and very rarely the glans penis. A positive Mantoux test, present or past history of tuberculosis, failure to detect mycobacteria from the skin lesions, healing of lesions with varioliform scars, and disease remission with antitubercular therapy are the clues to confirm the diagnosis.5
Secondary SyphilisPustular syphilis (lues maligna/malignant syphilis) is a rare form of secondary syphilis (<2%), commonly seen in HIV patients, which can result in varioliform scarring.6 It presents with acute-onset widespread, pustulo-ulcerative lesions associated with constitutional symptoms and generalised lymphadenopathy.7 Deep dermal tenderness can be elicited on the rash with a pinhead, termed Buschke-Ollendorff sign.8 The VDRL titre is usually high in these patients.6 Histopathology is characterised by obliterative endarteritis.7
Reactive perforating collagenosis (RPC)RPC is identified by the extrusion of altered collagen through the epidermis. Familial RPC often presents at an early age without any systemic association. Acquired RPC may occur in association with diabetes mellitus, chronic kidney disease, hypothyroidism, lymphoma and hyperparathyroidism. It is characterised by pruritic erythematous papules and nodules with a central adherent keratotic plug present over the trunk, the upper, and lower limbs. Removal of the crust exposes a crateriform pit. These lesions resolve with or without treatment with varioliform scars [Figure 3]. Differential diagnoses include other perforating disorders like elastosis perforans serpiginosa, perforating folliculitis, and Kyrle’s disease.9
Export to PPT
Generalised perforating granuloma annulare (GPGA)GPGA is a rare subtype of granuloma annulare characterised by discrete, umbilicated papules extruding mucoid material from the centre. The lesions occur in crops over the extremities and trunk. The etiology includes insect bites, viral infection, trauma, ultraviolet radiation, diabetes mellitus, and thyroiditis. Histopathology shows histiocytic granulomas surrounding necrobiotic collagen with mucin deposition, epithelioid histiocytes, and multinucleate giant with transepidermal elimination of degenerated collagen and mucin.10,11
Pityriasis lichenoides et varioliformis acuta (PLEVA)PLEVA is a rare, benign lymphoproliferative disorder that commonly affects children. Fever and lymphadenopathy are usually present. Cutaneous manifestations include the abrupt onset of recurrent crops of itchy or asymptomatic, spontaneously regressing erythematous to purpuric papules that form crusts, ulcers, vesicles, or pustules involving the trunk and flexural surface of the extremities and heal with varioliform scars.12
Lymphomatoid papulosisIt is a non-aggressive CD30+ cutaneous T-cell lymphoma characterised by recurrent episodes of asymptomatic or slightly itchy, self-resolving papulonodular lesions with or without necrosis. The skin lesions tend to involve the trunk and limbs and resolve with atrophic scars. These patients may develop haematological malignancies subsequently.13
Hydroa vacciniforme-like T-cell lymphomaIt is a rare subgroup of EBV-associated T-cell lymphoma from childhood, common in darker skin types. It presents with facial edema and recurrent outbreaks of pruritic or painful, infiltrated, and erythematous papules and nodules, vesicles, necrotizing ulcers and crusts that resolve with varioliform scars. In contrast to hydroa vacciniforme, these lesions can occur on sun-protected sites. Patients have associated fever, lymphadenopathy, and hepatosplenomegaly. Mosquito bite hypersensitivity, chronic EBV infection, and hemophagocytic lymphohistiocytosis are the other associations.14
Lipoid proteinosisLipoid proteinosis or Urbach–Weithe disease is a rare autosomal recessive genetic disorder. Lesions occur secondary to the deposition of amorphous hyaline material in different body parts due to a mutation in the ECM1 gene. It presents in early infancy with hoarseness of voice due to the vocal cord infiltration, followed by recurrent hemorrhagic vesicles, bullae, macules, papules, and skin-coloured nodules, which resolve with pock-like scars [Figure 4]. Woody tongue, thickened lingual frenulum, xerostomia, macroglossia, moniliform blepharitis, and nail dystrophy are seen. The respiratory system, upper gastrointestinal tract, and central nervous system may be involved.15

Export to PPT
Degos diseaseOtherwise known as ‘malignant atrophic papulosis’ is an occlusive arteriopathy involving small vessels of the dermis and sometimes of the gastrointestinal tract and central nervous system. Characteristic skin lesions are porcelain white papules with central atrophy with a surrounding rim of erythema. The gastrointestinal, renal, cardiopulmonary, central, and peripheral nervous systems can be affected (classical subtype) with up to 50% fatality rate. Isolated cutaneous disease has a benign course. Pathognomonic cutaneous lesions and histopathology showing a wedge-shaped region of necrosis with thrombotic arterial occlusion without any vasculitis are important pointers to making a diagnosis.16,17
Degos-like lesionDegos-like lesions reportedly occur in connective tissue diseases like dermatomyositis, systemic lupus erythematosus, and scleroderma as non-specific manifestations. The occurrence of these lesions is associated with the risk of systemic vasculopathy, which warrants screening and intervention.18
Disorders producing localised skin lesions Acne necroticaAcne necrotica is an uncommon disorder presenting with chronic recurrent crops of pruritic and/or inflammatory papulonodular lesions that rapidly necrotise and resolve with scarring. It occurs as crops of erythematous follicular papules or pustules which develop central umbilication and necrosis, in adults with a head and neck preponderance, healing with pitted varioliform scars and cicatricial alopecia [Figure 5]. The disease has no relation to acne vulgaris [Figure 6] and is a possible variant of pyoderma.19

Export to PPT

Export to PPT
Hydroa vacciniformeIt is a photosensitive disorder of rare occurrence that tends to occur either in early childhood (1–7 years) or at puberty (12–16 years) with male predilection and seasonal spring or summer exacerbations. Itchy, erythematous macules occur in a bilaterally symmetrical manner on photo-exposed regions within hours of sunlight exposure, on the face and dorsum of the hands. Over the next few hours, the macules progress to form tender papules or plaques with vesicles or haemorrhagic blisters. The lesions become umbilicated with haemorrhagic crusting and heal over several weeks with permanent varioliform scars. The age of development and typical distribution serve as a diagnostic clue.14
Cutaneous PorphyriasThese are photosensitive disorders with skin lesions favouring the face and dorsa of the hands. Porphyria cutanea tarda (PCT) is the commonest type, but erythropoietic protoporphyria (EPP) is most frequent in children. An acute phototoxic reaction with burning pain, oedema and erythema overexposed sites is the main clinical feature of EPP. PCT presents mainly with blistering and fragility. Repeated sun exposure can leave a typical linear or pox-like scar and a waxy indurated skin, predominantly over the nose and dorsa of fingers. Congenital erythropoietic porphyria (CEP) is another rare subtype associated with marked photosensitivity, leading to vesico-bullous lesions, chronic ulcers, and sometimes mutilation of sun-exposed body parts, and can cause varioliform scarring [Figure 7].20

Export to PPT
Disorders with follicular keratosisAtrophoderma vermiculata (AV), keratosis pilaris atrophicans faciei (KPAF) and keratosis follicularis spinulosa decalvans (KFSD) fall within the spectrum of inherited disorders with follicular keratosis. These disorders are usually non-pruritic. AV occurs in early life and presents with erythema and follicular, keratotic papules leading to a symmetrical honeycomb-like pattern of atrophic scars on the cheeks, preauricular area, and remit by puberty [Figure 8]. It may be associated with Rombo syndrome, cardiac defects, steatocystoma multiplex, etc. KPAF presents in early infancy in boys with blond hair, with erythema and keratotic follicular papules involving the lateral one-third of the eyebrows, progressing to atrophy and alopecia, which extends to involve the cheeks and forehead. It has been associated with Noonan syndrome, woolly hair, cardiofaciocutaneousa syndrome, and Rubinstein-Taybi syndrome. KFSD also presents in infancy with redness and keratotic follicular papules on the malar area. There is associated scarring alopecia involving the scalp, thinning of axillary and pubic hair, ocular abnormalities, and palmoplantar keratoderma.21

Export to PPT
Atrophia maculosa varioliformis cutis (AMVC)AMVC is a rare idiopathic disorder that is characterised by noninflammatory macular atrophic lesions affecting adolescents and young adults. Few familial cases have been reported from India, Turkey, and China. It manifests as asymptomatic shallow, sharply delineated, linear, varioliform, or punctate scars on the face, appearing spontaneously without accompanying erythema, induration, pigmentation, or honeycomb pattern [Figure 9].22 The diagnosis is generally clinical. Association with extrahepatic biliary atresia, keratosis pilaris, and pachydermodactyly has been previously reported.22,23

Export to PPT
Lupus miliaris disseminatus faciei (LMDF)It is a rare, benign, chronic inflammatory dermatosis that presents in adulthood with eruptive, asymptomatic, papulopustular skin lesions involving the face which may resolve with pock-like scars [Figure 10]. Histologically, the collection of lymphohistiocytes and epithelioid granulomas with caseous necrosis is noted.24

Export to PPT
So, there is a wide spectrum of diseases presenting with varioliform scars. We have devised a simplified clinical approach [Figure 11] based on the age of onset, associated signs and symptoms to aid the treating physician in arriving at an early diagnosis and manage accordingly.
Export to PPT
留言 (0)