Dear Editor,
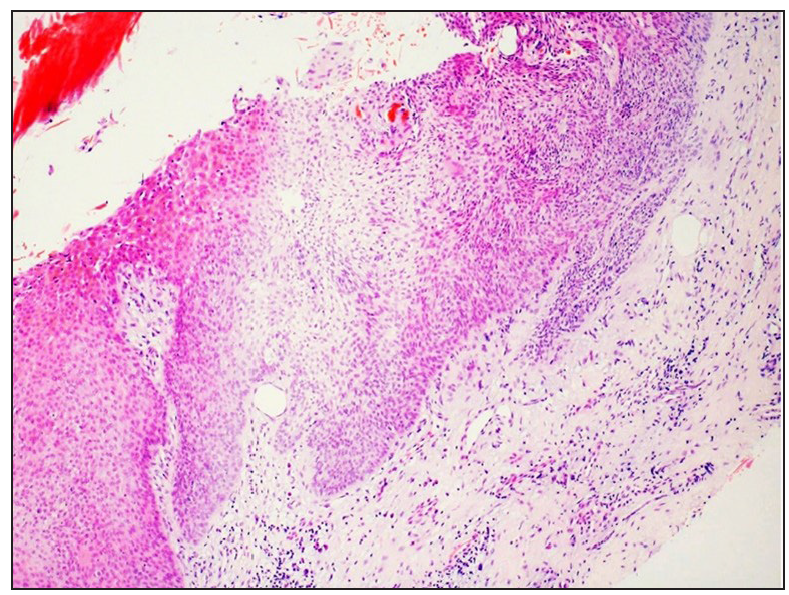
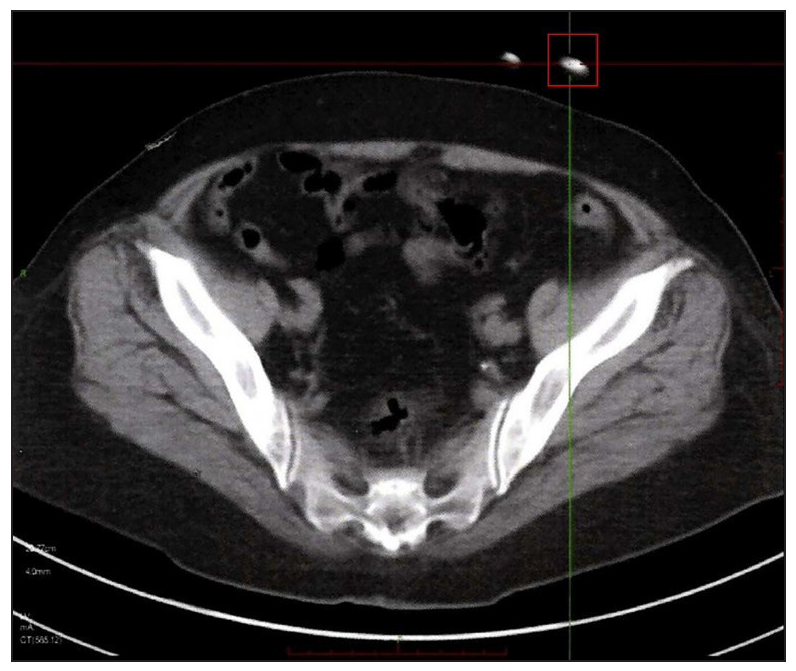
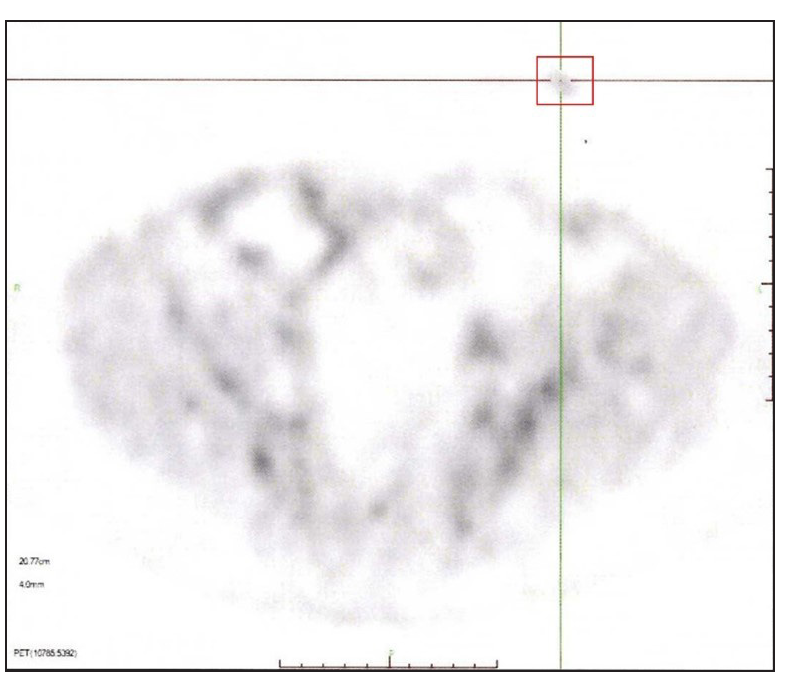
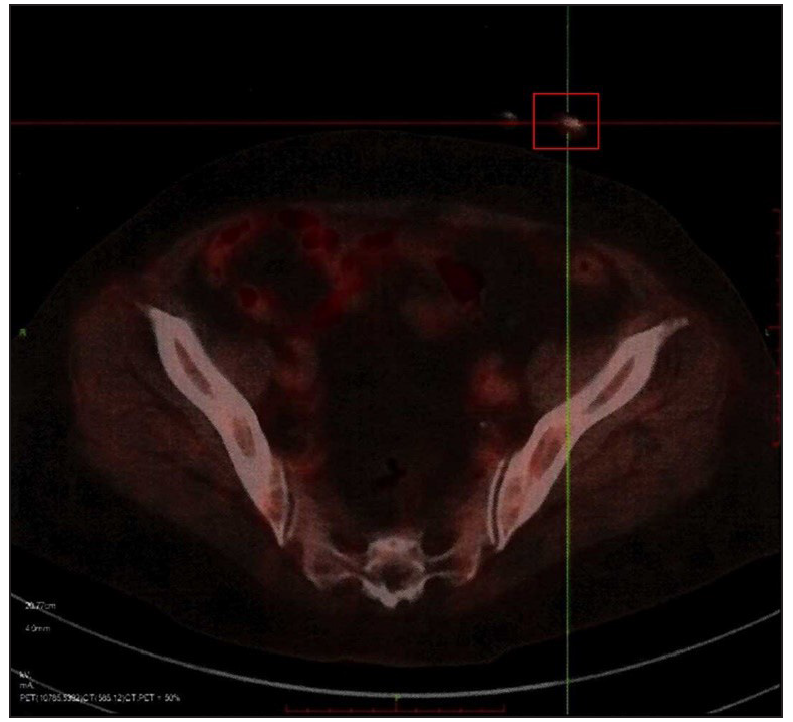
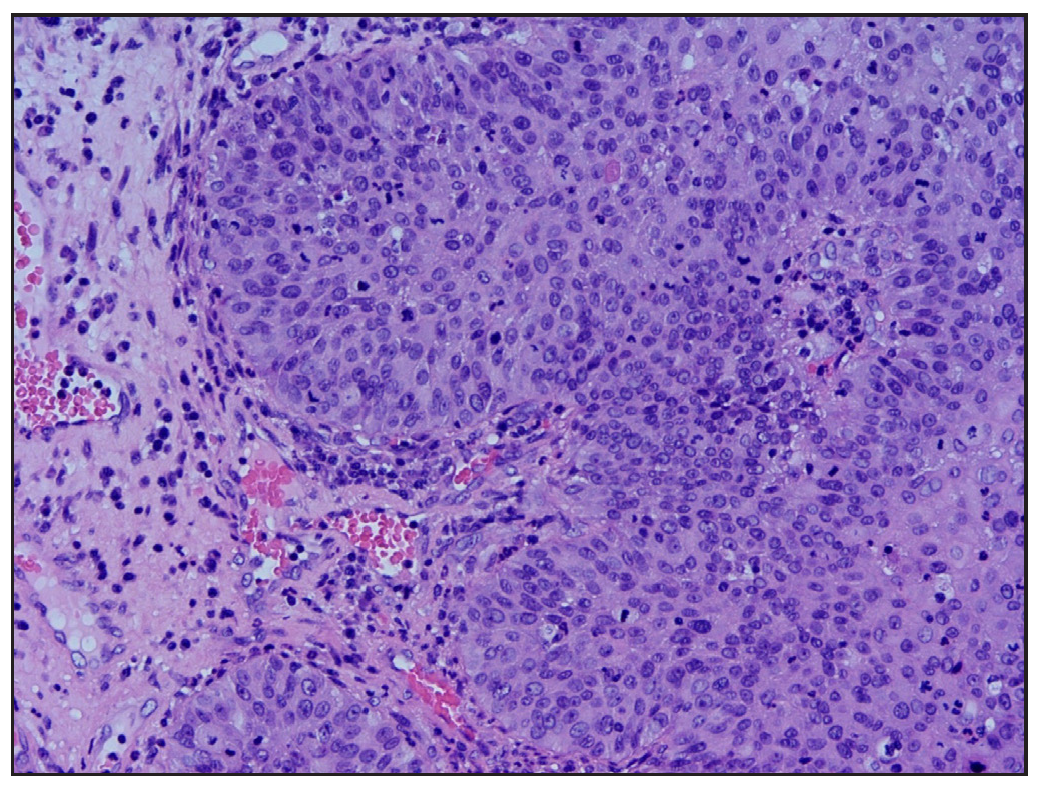
Subungual squamous cell carcinoma (Subungual SCC) is a rare neoplasm of the skin. Diagnosis of subungual SCC is often challenging given the resemblance to other common nail diseases, such as paronychia, onychomycosis, and papilloma. Herein, we report the case of a 62-year-old woman with a 3-year history of indolent subungual bleeding from the right ring finger. Similar symptoms had also been present 10 years ago affecting the same nail. A lymph node biopsy of the right axillary and supraclavicular lymph nodes confirmed a diagnosis of squamous cell carcinoma (SCC) of epithelial origin. She received chemotherapy which led to a temporary improvement in the subungual lesion followed by a recurrence for which the patient was referred to us 3 years ago. At the presentation, there was an irregular scaly plaque affecting the hyponychium of the right ring finger with occasional bleeding, accompanied by a localised thick yellow nail plate [Figure 1a]. Dermoscopy in the polarised mode revealed a pink, translucent structureless area, a nail plate with free edge thickening, a fuzzy lesion edge, and subungual bleeding accompanied by white scales and yellow keratinous crusts [Figure 1b]. A nail bed biopsy showed dyskeratotic cells, atypical keratinocytes, and an irregularly thickened epithelium [Figure 1c]. Positron emission tomography- computed tomography (PET-CT) showed no visceral malignancy and a positive uptake in the right ring finger [Figures 2a–2d]. The lesion was excised by distal digit amputation. The pathologic evaluation was diagnostic of SCC with axillary metastases [Figure 3].

Export to PPT

Export to PPT
Export to PPT
Export to PPT
Export to PPT
Export to PPT

Export to PPT
Export to PPT
Subungual bleeding could be caused by trauma, dermatoses, tumour, vasculitis, drug reactions, or infectious diseases.1 Traumatic subungual bleeding usually presents as black discoloration located distally in most patients; however, lesions are more red and more proximal in patients with systemic diseases.1 Subungual SCC should be suspected in patients with long-term recurrent nail disease that does not respond to treatment. In this case, the patient presented with long-term recurrent indolent subungual bleeding, and there was no history of trauma. Dermoscopy and biopsy are indicated at the earliest possible once this suspicion arises. There are no diagnostic criteria for dermoscopic characterisation of subungual SCC. Common dermoscopic features include a pink background, translucent structureless areas, white scales, and dotted or irregular vessels.2 Our patient showed most of these features except vascular structures. Subungual SCC’s are generally considered low-grade malignancies with a low propensity to metastasize. However, there are usually delays in the diagnosis, which results in delayed treatment.3 Huang et al.4 reported a patient who presented with metastatic SCC in the left groin 3 years following his first diagnosis of a subungual SCC presenting on his left fifth toe. Dalle et al.5 reported a median delay in diagnosis of subungual SCC to be 24.5 months. One of the 35 patients in this series died from lung metastases.
Though there are currently no established treatment guidelines for subungual SCC, it is generally accepted that most can be successfully treated with surgical excision.3 When there is no involvement of the distal phalangeal bone, Mohs surgery and wide surgical excision can be performed whereas amputation of the distal phalanx or disarticulation of the involved digit is often indicated for invasive disease.3 Metastatic tumours, in addition, require block dissection of the regional lymph nodes, postoperative irradiation of the draining lymph nodes, and systemic chemotherapy.6 Kelly et al.7 suggested that early management of metastatic disease with complete lymphadenectomy or radiation is strongly recommended. This was the treatment plan followed in our patient too.
This case illustrates the significance of a thorough history and physical examination to allow early and accurate diagnosis of subungual SCC for a better prognostic outcome. Furthermore, although it metastasises rarely, physicians must be aware of this possibility.
留言 (0)