Dear Editor,
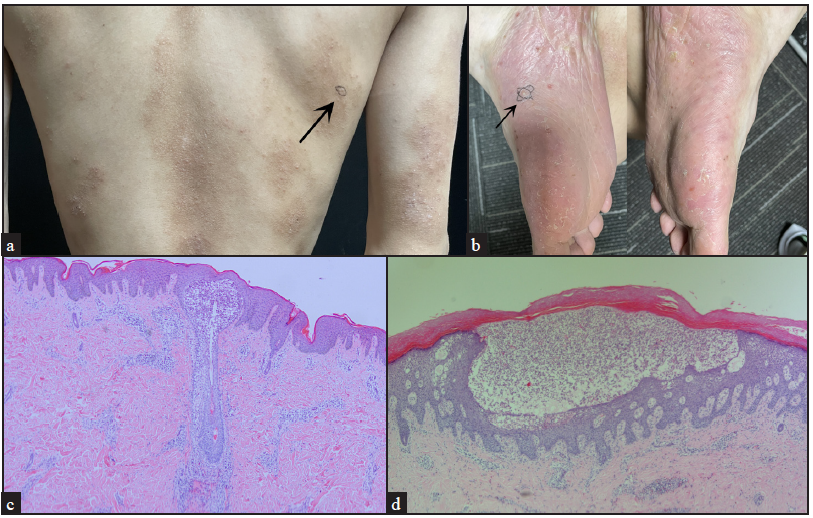
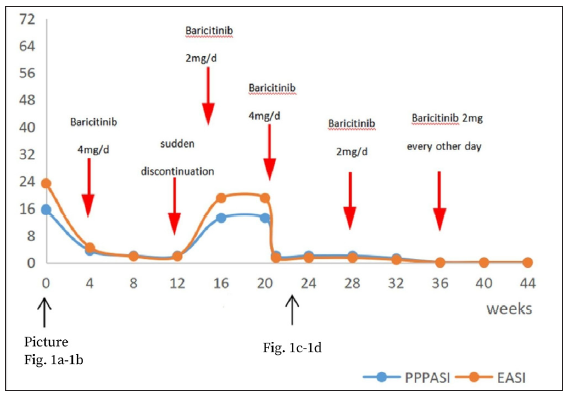
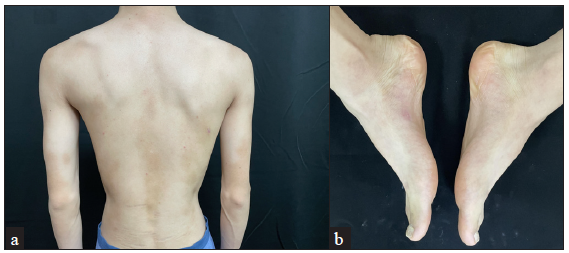
A 20-year-old man presented with generalised erythema with pruritus for the last five years. He also had recurrent pustules and erythema on the soles for two years. Previous therapies with topical corticosteroids, antihistamines, and traditional Chinese medicine were ineffective. The patient had a history of allergic rhinitis. There was no family history of psoriasis, and systemic symptoms were unremarkable. Physical examination revealed scattered edematous erythematous papules on the face, dull erythematous patches containing clustered papules with localised lichenification on the trunk and limbs, and multiple pustules on large erythemato-squamous patches on the soles [Figures 1a, 1b]. He had no joint pain or fever. Laboratory tests showed an elevated eosinophil count (0.8 ×109/L) and IgE level (99 kU/L). Histology from the back showed hyperkeratosis, parakeratosis, focal mild interspinous oedema, few eosinophils and lymphocytes surrounding superficial dermal blood vessels and hair follicles, with infiltration of neutrophils and eosinophils in the infundibulum [Figure 1c]. Histology from the right foot showed hyperkeratosis, mild acanthosis, intraepidermal pustules with numerous neutrophils, perivascular eosinophils, and lymphocyte infiltration in the dermis below the pustules [Figure 1d]. The patient was diagnosed with palmoplantar pustulosis (PPP) and atopic dermatitis (AD). He was treated with oral baricitinib 4 mg/d, and the lesions resolved four weeks later. After another three months, the dose was tapered to 2 mg/d. During the following two months, he discontinued baricitinib for one week and experienced a relapse. Then, the dose was increased back to 2 mg/d and continued for four weeks, but there was no improvement [Figure 2]. When it was further increased to 4 mg/d, the rash resolved within one week [Figures 3a, 3b]. The rash did not recur during the following two months. Then, baricitinib was tapered to 2 mg/d and 2 mg every other day for the next two months. No new skin lesions emerged, and all laboratory findings were within the normal limits.
Export to PPT
Export to PPT
Export to PPT
Palmoplantar pustulosis (PPP) is a chronic pustular dermatitis facilitated by T helper 1 (Th 1) cytokine production. AD is a persistent inflammatory skin disease; its acute phase is mainly mediated by Th2, and the Th2-Th1 switch promotes disease chronicity.1 PPP and AD were once considered two opposite poles of the Th cell-mediated inflammation. The Th1/Th2 imbalance maybe the main immunological mechanism underlying PPP and AD.2
The patient’s diagnosis of AD was clear. However, plantar lesions must be distinguished from palmoplantar pustular psoriasis (PPPP). Yamamoto considered PPP to be a distinct entity from PPPP.3 PPPP presents as well-circumscribed keratotic erythematous plaques with few pustules, not confined to the palms and soles. The dorsal surfaces of the hands and feet may also be involved, and patients usually develop plaque psoriasis elsewhere. Our patient was characterised by multiple sterile pustules over an erythematous and oedematous background on the soles, with no psoriasis-like lesions elsewhere on the body and no family history of psoriasis. Therefore, a diagnosis of PPP was made.
Traditional treatments have undesirable side effects, and biologics targeting specific cytokines are used to treat only one disease. Baricitinib, an oral Janus kinase (JAK) inhibitor, effectively targets JAK1 and JAK2, inhibiting downstream cytokine production and Th-cell differentiation by impeding the JAK-STAT signalling pathway. The course of our patient hints at a rapid response and long term efficacy of baricitinib in treating PPP and AD, but its dose must be reduced gradually. This is consistent with the findings from phase II4, phase III5 trials and a long-term double-blind extension study6 of baricitinib in the treatment of AD. Currently, there have been no reports of the use of baricitinib in the treatment of PPP. However, Koumaki et al.7 have previously reported palmoplantar pustulosis eruption caused by baricitinib. Our study is distinct from the former and contributes to further exploration of the pathways involved in the effect of baricitinib on PPP. In conclusion, baricitinib could be a novel alternative for patients suffering from PPP with AD.
留言 (0)