CLINICAL STUDIES / ETUDES CLINIQUES
FACTORS INFLUENCING SURGICAL OUTCOMES OF CAUDA EQUINA SYNDROME IN TOGO
FACTEURS PREDICTIFS DES RESULTATS CHIRURGICAUX DU SYNDROME DE LA QUEUE DE CHEVAL AU TOGO
ABSTRACT
Introduction
Cauda equina syndrome is an emergency whose treatment is almost exclusively surgery. The surgical results are variously appreciated in the literature. In Africa, in addition to the scarcity of data, many parameters influence the evolution. The aim of this study is to try to find factors influencing surgical outcomes of cauda equina syndrome in Togo.
Material and methods
This was a descriptive retrospective study from 2012 to 2021 including 56 patients operated for cauda equina syndrome in the neurosurgery department of CHU Sylvanus Olympio in Lomé. The neurological recovery was assessed 6 and 12 months according age, sex, symptoms duration, initial neurological status using multi-variable analysis (R logiciel) to determine predictors. Two-sided p values < 0.05 were considered statistically significant.
Results
The mean age of the patients was 49.7 years with a male predominance (sex ratio of 2.3). The onset was sudden in 26.8%. All patients had motor and sensory disorders, and 92.8% genito-sphincter disorders. The syndrome was complete in 48.2%. The mean evolution time was 12.7 days. The main etiology was degenerative. Majority of patients was operated on within one week of admission (96.4%). The average hospital stay was 25.8 days. At 12 months, the results were good in 23.2% and satisfactory in 39.3%. There was a statistically significant difference between complete and incomplete syndrome concerning neurological outcomes (p= 0.000). Furthermore, traumatic cases recovered better than others (p= 0.04). The recovery was independent to the duration of signs as well as for sex and age (p= 0.8).
Conclusion
The main factors influencing neurological recovery are the completeness or not of the syndrome and its etiology. We noted also that, despite long delays, the surgical outcomes were good overall.
Keywords: Cauda equina syndrome – Risk factors- Surgery Outcomes – Togo.
RESUME
Introduction
Le syndrome de la queue de cheval est une urgence dont le traitement est presque exclusivement chirurgical. Les résultats chirurgicaux sont diversement appréciés dans la littérature. En Afrique, outre la rareté des données, de nombreux paramètres influencent l’évolution. Le but de cette étude était de déterminer les facteurs influençant les résultats chirurgicaux du syndrome de la queue de cheval au Togo.
Matériel et méthodes
Il s’agissait d’une étude rétrospective descriptive et analytique de 2012 à 2021 incluant 56 patients opérés d’un syndrome de la queue de cheval dans le service de neurochirurgie du CHU Sylvanus Olympio à Lomé. La récupération neurologique a été évaluée à 6 et 12 mois selon l’âge, le sexe, la durée des symptômes, l’état neurologique initial à l’aide d’une analyse multivariée (R logiciel) pour déterminer les facteurs prédictifs. Les valeurs p bilatérales < 0,05 ont été considérées comme statistiquement significatives.
Résultats
L’âge moyen des patients était de 49,7 ans avec une prédominance masculine (sex ratio de 2,3). Le début a été brutal dans 26,8 %. Tous les patients présentaient des troubles moteurs et sensitifs, et 92,8 % des troubles génito-sphinctériens. Le syndrome était complet dans 48,2 %. La durée moyenne d’évolution était de 12,7 jours. L’étiologie principale était dégénérative. La majorité des patients ont été opérés dans la semaine suivant leur admission (96,4 %). La durée moyenne d’hospitalisation était de 25,8 jours. A 12 mois, les résultats étaient bons dans 23,2% et satisfaisants dans 39,3%. Il y avait une différence statistiquement significative entre le syndrome complet et incomplet concernant les résultats neurologiques (p = 0,000). Les cas traumatiques ont également mieux récupéré que les autres (p = 0,04). La récupération était indépendante de la durée des signes ainsi que du sexe et de l’âge (p = 0,8).
Conclusion
Les principaux facteurs influençant la récupération neurologique sont la complétude ou non du syndrome et son étiologie. Nous avons également noté que malgré de longs délais, nos résultats chirurgicaux sont globalement bons.
Mots clés : Syndrome de la queue de cheval – Facteurs prédictifs chirurgicaux – Togo.
INTRODUCTION
The cauda equina syndrome (CES), characterized in its complete form by paraplegia, sphincter disorders, and saddle anesthesia is relatively rare. Its annual incidence is 5 to 10 cases per 1 million. It’s responsible of important long-term morbidity, why requiring urgent therapeutic measures (3,10,15,22,30). The treatment is based almost exclusively on surgery, which results are variously assessed in the international literature (7,8,17,29). The predictor’s factors influencing outcomes are controversial (14). In Africa, the specificities as long delays of treatment, the lack of all therapeutic modalities and the patients follow up difficulties are greatly influencing the results (26,29). This motivated the current study to try to find factors influencing surgical outcomes of CES in Togo.
MATERIAL AND METHODS
This was a descriptive retrospective study from 2012 to 2021 including all patients operated for cauda equina syndrome in the neurosurgery department of the CHU Sylvanus Olympio in Lomé. CES was defined as the partial or total association of the following 3 disorders: – Motor disorders: total or partial deficit affecting at least one of the roots below L1; – Perineal sensation impairment: hypoesthesia or anesthesia; – Genito-sphincter disorders: urinary and faecal incontinence, urinary emergency, incomplete urination, urinary retention, erectile disorder for men.
The complete syndrome was defined as association of paraplegia, saddle anesthesia, and anal and/or urinary incontinence. In addition to those disorders, CES must be confirmed by the compression of nerve roots of cauda equina with imaging.
We assessed surgical outcomes over 2 periods of time: short term (6 months postoperative) and middle term (12 months postoperative). The parameters were based on motor, sphincter and sensory recovery; each of them can be total, partial or null. The results were: – Good: when the recovery of each of the 03 functions was total; – Satisfactory: sphincter control associated with motor recovery more than 3; – Bad: in the other cases.
Multi-variable analysis (R logiciel) was used to determine predictors. The factors assessed concerning neurological recovery were age, sex, symptoms duration, etiologies and initial neurological status. Two-sided p values < 0.05 were considered statistically significant
RESULTS
A total of 56 patients were operated for CES during the study period. The average age was 49.7 years (18 to 79 years) with male predominance (sex ratio of 2.3). The onset was sudden in 26.8%, rapidly progressive (< 15 days) in 50% and progressive (> 15 days) in 23.2%. Patients presented clinical history of lumboradiculalgia in 51.8% with radicular claudication in 23.2%. All the patients had motor and sensory disorders and 92.8% genito-sphincter disorders (Table I). The symdrome was complete in 48.2%. The average time for progression of the syndrome before diagnosis was 12.7 days. Only 8.9% of patients consulted within 2 days of cauda equina syndrome onset. CT scan (48.2%) and MRI (82.1%) found mainly degenerative causes as the etiology of the syndrome (Table II).
Two patients had been operated on within 24 hours and the majority within a week after admission (96.4%). We did after laminectomy, 19 discectomies, 17 osteosyntheses and 08 tumor resections including 3 total removals (neurinomas). Radiation therapy was performed for a case of chordoma, Chemotherapy for plasmacytoma and anti-tuberculosis. The mean length stay was 25.8 days. Functional rehabilitation was daily during hospitalization and after discharge, only 24 patients (42.9%) honored it. In the medium term, surgical outcomes on neurological recovery were satisfactory, especially for incomplete forms. The difference between the 2 forms was statistically significant for good and satisfactory results (p= 0.000). The recovery was also better for traumatic CES comparative to other etiology (p=0.04). The recovery was independent to the duration of evolution (Figure 1) as well as for sex (p=0.8) and age (p=0.8). (Table III).
DISCUSSION
CES is characterized by several sign making its definition difficult (1,2,7). Whatever the form, it is a surgical emergency. Early surgery upon diagnosis is an important parameter for neurological recovery; the ideal time, although controversial, would be surgery within 24-48 hours after onset, if not as soon as possible (5,13,20,32). As our patients were operated late, there was no difference in neurological recovery between according operating times. On the other hand, we noted a significant difference between the complete or not CES in the evolution in favor of the incomplete forms as also underlined by several authors (7,11,31,33). The other parameters influencing neurological recovery are the duration of the syndrome, etiology, age, sex and functional rehabilitation (16,19). Regarding the etiology, the post-traumatic causes would have a better neurological recovery than the others (12,31). We noticed it in our series. Our operative findings may could explain this fact: we noted in all cases of post-traumatic cauda equina syndrome, a dural rupture. The existence of this rupture would reduce the intrathecal pressure, but would also facilitate the mobility and spreading of the rootlets in the available intracanal space, resulting less stress on them. This is reflected in a mostly incomplete syndrome, resulting in better post-surgical recovery. This mechanism would not occur in cauda equina syndrome due to herniated disc in which the dura being intact, generates by compression, a significant intrathecal hydrodynamic pressure damaging on the rootlets (9,20,21,24,25,28).
Age does not seem to influence neurological recovery as found in our series (19). But we believe that it could be if we choose the right comparison groups. Indeed, we believe that the presence of degenerative lesions with chronic vascular alterations could slow down recovery compared to the subjects free of these lesions.
Although it was demonstrated no recovery difference between the 2 sexes; in the long term, some authors have found that women have more urinary incontinence than men, solely due to the anatomical specificity of the sphincters of the 2 sexes (19).
Concerning disease duration, it has been shown that the slow evolution augurs better neurological recovery, especially because it mostly giving an incomplete CES (6,11,19,27). The complete CES which often reflects a total interruption of the nerve impulse (anatomical or functional) is most often correlated with a sudden onset. It is in this case a rapid decompression is very important before occurrence of irreversible ischemia, because the Wallerian degeneration that follows compromises neurological recovery after surgery.
The role of physiotherapy is well established (18). Our results could be better if there were intensive rehabilitation centers; because only 43% of outpatients were able to perform 3 weekly physiotherapies during the follow-up period. However, our results may probably evolve favorably in the long term, as neurological improvements occurred later than 4 years (4).
CONCLUSION
This study reflected like many others the difficulty to identify the prognostic factors of CES even some of them are reaching a consensus such as the initial neurological status and the etiology. The speed of management, even though controversial, is also beneficial for the patient first to avoid to complete his syndrome but also to avoid irreversible ischemia of the root vessels which definitively compromises neurological recovery. We noted also that, despite long delays, our surgical outcomes are overall good.
Tables
Table I: Signs of cauda equina syndrome at admission.
Repartition n % Motor disorders Paraplegia 27 48,2 Paraparesis 24 42,9 Root deficits 5 8,9 Sensory disorders Saddle anesthesia 28 50 Root hypoesthesia 17 30,4 Perineal hypoesthesia 11 19,6 Genito-sphincter disorders Urinary / anal incontinence 27 48,2 Emergency micturition. 13 23,2 Erectile disorders ⃰ 12 21,4⃰ for male (39)
Table II: cauda equina syndrome etiologies
Repartition n % Degenerative disease 37 66 Lombal stenosis / lombolisthesis 19 33,9 Disc hernia 18 32,1 Tumors 09 16,1 Neurinoma 3 5,4 Ependymoma 3 5,4 Plasmocytoma 2 3,5 Chordoma 1 1,8 Traumatic 6 10,7 Infections 4 7,1 Pott disease 4 7,1
Table III: surgical outcomes according different factors
Short term Middle term Satisfactory n(%) Bad n(%) Lost n(%) Good n(%) Satisfactory n(%) Bad n(%) Lost n(%) Incomplete CES (29)1 24 (42.8) 4 (7.1) 1 (1.8) 9 (16.1) 17 (30.3) 0 3 (5.4) Complet CES (27)1 4 (7.1) 21(37.5) 2 (3.6) 4 (7.1) 5 (8.9) 12 (21.4) 6 (10.7) p=0.000 p=0.15 p=0.002 ≤ 40 years old (14)2 8 (14.3) 5 (8.9) 1 (1.8) 6 (10.7) 3 (5.3) 3 (5.3) 2 (3.6) ≥40 years old (42)2 20 (35.7) 20 (35.7) 2 (3.6) 7 (12.5) 19 (33.9) 9 (16.1) 7 (12.5) p=0.5 p=0.04 p=0.11 Male (39)3 22 (39.3) 15 (26.8) 2 (3.6) 9 (16.1) 15 (26.8) 9 (16.1) 6 (10.7) Female (17)3 6 (10.7) 10 (17.8) 1 (1.8) 4 (7.1) 7 (12.5) 3 (5.3) 3 (5.3) p=0.14 p=0.9 p=0.8 Traumatic CES (6)4 6 (10.7) 0 0 4 (7.1) 2 (3.6) 0 0 Others CES (50)4 22 (39.3) 25 (44.6) 3 (5.4) 9 (16.1) 20 (35.7) 12 (21.4) 9 (16.1) p=0.01 p=0.008 p=0.7 Global 28 (50) 25 (44.6) 3 (5.4) 13 (23.2) 22 (39.3) 12 (21.4) 9 (16.1)1 The recovery is better (good and satisfactory results) for incomplete CES (p=0.000)
2 The recovery is independent concerning age (p=0.8)
3 The recovery is independent concerning gender (p=0.8)
4 The recovery is better (good and satisfactory results) for traumatic CES (p=0.04)
Figure
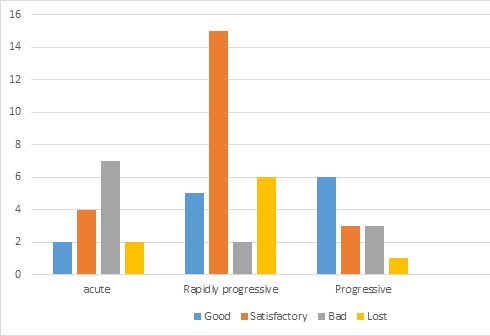
Figure 1 : Patients outcomes according to onset mode
REFERENCES
BALASUBRAMANIAN K, KALSI P, GREENOUGH CG, SEETHARAM Reliability of clinical assessment in diagnosing cauda equina syndrome. Br J Neurosurg. 2010;24:383–6. BELL D, COLLIE D, STATHAM P. Cauda equina syndrome: what is the correlation between clinical assessment and MRI scanning? Br J Neurosurg. 2007;21:201–3 CHAN AM, XU LL, PELZER NR, GRAGNANIELLO Timing of surgical intervention in cauda equina syndrome: a systematic critical review. World Neurosurg. 2014;81(3-4):640-50. CHANG HS, NAKAGAWA H, MIZUNO J. Lumbar herniated disc presenting with cauda equina syndrome long term follow-up of four cases. Surg Neurol. 2000;53:100–5. DELONG WB, POLISSAR N, NERADILEK B. Timing of surgery in cauda equine syndrome with urinary retention: meta-anlysis of observation studies. J Neursurg Spine. 2008;8(4):305–20. DOMEN PM, HOFMAN PA, VAN SANTBRINK. Predictive value of clinical characteristics in patients with suspected cauda equina syndrome. Eur J Neurol. 2009;16:416–9. FRASER S. Cauda equina syndrome: a literature review of its definition and clinical presentation. Arch Phys Med Rehabil. 2009;90(11):1964–8. FUSO FA, DIAS AL, LETAIF OB, CRISTANTE AF, MARCON RM, DE BARROS TE. Epidemiological study of cauda equina syndrome. Acta Ortop Bras. 2013;21(3):159-62. GELFAN S, TARLOV JM. Physiology of spinal cord, nerve root and peripheral nerve compression. Am J Physiol. 1956;185:217–29. GITELMAN A, HISHMEH S, MORELLI BN, JOSEPH SA, CASDEN A, KUFLIK P, NEUWIRTH M, STEPHEN M. Cauda equina syndrome: a comprehensive review. Am J Orthop. 2008;37(11):556-62. GLEAVE JRW, MACFARLANE R. Cauda equina syndrome, what is the relationship between timing of surgery and outcome. Br J Neurosurg. 2002;16(4):325–8. HARROP JS, HUNT GE, VACCARO AR. Conus medullaris and cauda equine syndrome as a result of traumatic injuries: management principles. J Neurosurg Neurosurg Focus. 2004;16:19–23. KOHLESS SS, KOHLES DA, KARP AP, ERLICH VM, POLISSAR Time-dependent surgical outcomes following cauda equina syndrome diagnosis: comments on a meta-analysis. Spine (Phila Pa 1976). 2004;29(11):1281–7. KONIG A, AMELUNG L, DANNE M, MEIER U, LEMCKE J. Do we know the outcome predictors for cauda equine syndrome (CES)? A retrospective, single-center analysis of 60 patients with CES with a suggestion for a new score to measure severity of symptoms. Eur Spine J. 2017; 26 :2565–72. KORSE NS, JACOBS WC, ELZEVIER HW, VLEGGEERT-LANKAMP Complaints of micturition, defecation and sexual function in cauda equina syndrome due to lumbar disk herniation: a systematic review. Eur Spine J. 2013;22(5):1019-29. KORSE NS, PIJPERS JA, VAN ZWET E, ELZEVIER HW, VLEGGEERT-LANKAMP CLA. Cauda Equina Syndrome: presentation, outcome, and predictors with focus on micturition, defecation, and sexual dysfunction. Eur Spine J. 2017;26:894–904. LONG B, KOYFMAN A, GOTTLIEB Evaluation and management of cauda equina syndrome in the emergency department. Am J Emerg Med. 2020;38(1):143-8. MAHMOUD H, QANNAM H, ZBOGAR D, MORTENSON B. Spinal cord injury rehabilitation in Riyadh, Saudi Arabia: time to rehabilitation admission, length of stay and functional independence. Spinal Cord. 2017;55: 09–14. MCCARTHY MJH, AYLOTT CEW, GREVITT MP, HEGARTY Cauda equina syndrome: factors affecting long-term functional and sphincteric outcome. Spine. 2007;32:207–16. NASCONE JW, LAUERMAN WC, WIESEL SW. Cauda equina syndrome: is it a surgical emergency? Orthop J. 1999;12:73–6. OLMARKER K, RYDEVIK B, HOLM S, BAGGE Effects of experimental, graded compression on blood flow in spinal nerve roots: a vital microscopic study on porcine cauda equina. J Orthop Res. 1989;7:817–23. ORENDACOVA J, CIZKOVA D, KAFKA J, LUKÁCOVÁ N, MARSALA M, SULLA I, MARSALA J, KATSUBE Cauda equina syndrome. Proq Neurobiol. 2001;64(6):613-37. RINKAEWKAN P, KUPTNIRATSAIKUL V. The effectiveness of inpatients rehabilitation for spinal cord patients in Siriraj hospital. Spinal Cord. 2015; 53:591–7. RYDEVIK BL, BROWN MB, LUNDBORG G. Pathoanatomy and pathophysiology of nerve root compression. 1984;9:7–15. RYDEVIK BL, MYERS RR, POWELL HC. Pressure increase in the dorsal root ganglion following mechanical compression. 1989;14:574–6. SARKAR S. Outcome of Cauda Equina Syndrome When Presenting Late in Developing Countries. J Am Coll Surg. 2020;231(4,Suppl 2):39‑40. SEKIGUCHI M, KIKUCHI S, MYERS RR. Experimental spinal stenosis: relationship between degree of cauda equina compression, neuropathology, and pain. Spine. 2004;29:1105–11. SHARPLESS SK. Susceptibility of spinal roots to compression block: NIH Workshop. In: GOLDSTEIN M, ed. The Research Status of Spinal Manipulative Therapy NINCDS Monograph No. 15]. 1975:155–61. SRIKANDARAJAH N, WILBY M, CLARK S, NOBLE A, WILLIAMSON P, MARSON Outcomes Reported After Surgery for Cauda Equina Syndrome: A Systematic Literature Review. Spine (Phila Pa 1976). 2018; 43(17):E1005-E13. TAMBURELLI FC, GENTITIEMPO M, LOGROSCINO CA.Cauda equina syndrome and spine manipulation:case report and review of the literature. Eur Spine J.2011;20(1):S128-31. THONGTRANGANI, LE H, PARK J, KIM Cauda equina syndrome in patients with low lumbar fractures. Neurosurg Focus. 2004;16(6):6. TODD NV Cauda equine syndrome: the timing of surgery probably does influence outcome. Br J Neurosurg. 2005;19(4):301–6. TODD NV, DICKSON RA. Standards of care in cauda equina syndrome. Br J Neurosurg. 2016;30(5):518–22.
留言 (0)