A 55-year-old man experienced diplopia and ophthalmoplegia and was admitted to our hospital 3 days after the onset of the double vision. He had a history of hypertension for more than 20 years. His highest blood pressure was 180/104 mmHg. Neurologic examination and cover test showed exotropia of the left eye, alternating exotropia, and bilateral internuclear ophthalmoplegia with impaired convergence. Vertical saccades and smooth pursuit of the left eye were also limited (see Supplementary Video). Pupillary, levator function, and bilateral abducent nucleus were normal. No other positive signs of the nervous system were found in physical examination. Besides, no abnormalities were found after liver and kidney function checks, blood tests, and the coagulation markers detection. Moreover, no abnormality was found in the levels of hepatitis B surface antigen (HbsAg), hepatitis B core antibody (HbcAb), hepatitis Be antigen (HBeAg), anti-hepatitis B e antibody (anti-HBe), anti-hepatitis B core antibody (anti-HBc), anti-hepatitis C virus (anti-HCV), anti-human immunodeficiency virus (anti-HIV), anti-treponema pallidum (anti-TP) antibody, anti-streptolysin O (ASO), rheumatoid factor (RF), C-reactive protein (CRP), and the autoantibodies. The lumbar puncture showed that the pressure was about 120 mmH2O, and the cerebrospinal fluid (CSF) analysis was normal. Consequently, the patient underwent an MRI scan, which suggests an acute infarction in the left of the pontine tegmentum involving the left medial longitudinal fasciculus (MLF) (Figure 1). The patient was finally diagnosed with pons infarction.
FIGURE 1
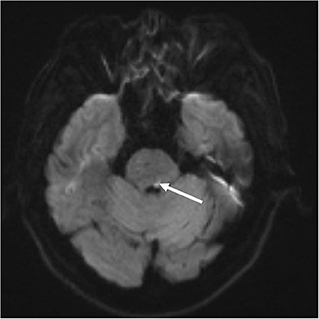
Figure 1. Brain MRI: Diffusion-weighted images reveal a focal ischemic stroke in the dorsal pons (arrows).
The patient received anticoagulation and anti-platelet aggregation therapy. There was no stroke recurrence, and diplopia returned to a healthy level after the patient's discharge from the hospital 6 months.
DiscussionWall-eyed bilateral internuclear ophthalmoplegia is a syndrome that involves bilateral adduction deficits, bilateral abducting nystagmus, and a large angle exotropia in primary gaze (Sharpe et al., 1974). WEBINO is mainly caused by cerebrovascular disorders (CVD), multiple sclerosis, neurodegenerative disorders, and infections (Sakamoto et al., 2012). WEBINO syndrome caused by CVD has been reported by several studies (Chen and Lin, 2007). Studies have shown that the disease is often associated with brainstem ischemia and hydrocephalus, immunotherapy of tumors, and diseases such as multiple sclerosis. This study summarized 39 case reports, including 42 WEBINO patients (Inocencio and Ballecer, 1985; Lana et al., 1990; Fay and Strominger, 1999; Korkmaz et al., 2002; Ozer et al., 2005; Chen and Lin, 2007; Kim et al., 2008; Matsumoto et al., 2008, 2019; Ushio et al., 2008; Jacob et al., 2010; Sierra-Hidalgo et al., 2010; Shinoda et al., 2011; Beh and Frohman, 2012; Jadhav and Prasad, 2012; Sakamoto et al., 2012; Bar et al., 2014; Chakravarthi et al., 2014; de Mora et al., 2014; Mathis et al., 2014; Muralidhar et al., 2014; Nakajima et al., 2014; Toufeeq and Dave, 2014; Agarwal et al., 2015; Ljevak et al., 2015; Man et al., 2015; de Souza et al., 2017; Sajjadi et al., 2017; Zou and Chen, 2017; Keereman et al., 2018; Papageorgiou et al., 2018; Im et al., 2020; Vázquez-Justes et al., 2020; Yazdi et al., 2020; Ansari et al., 2021; Jo et al., 2021; Petrik et al., 2021; Sinha et al., 2021; Wako et al., 2022). The age range of the patients was 12–85 years; 26 were male (61.9%), 15 were female (35.7%), and the gender of one was unknown. In the analysis of the clinical data of neuro-ophthalmological signs in WEBINO patients, 37 (88.1%) cases of exotropia in the first eye-position, 38 (90.5%) cases of bilateral intraocular disorders, 22 (52.4%) cases of convergence barrier, six (14.3%) cases of blepharoptosis, 18 (42.9%) cases of vertical gaze disorder, six (14.3%) cases of vertical nystagmus, eight (19.0%) cases of pupillary anomalies, and two (4.8%) cases of reversed dip. Among the studies, the lesion site summary showed that 28 (66.7%) cases occurred in the midbrain, 14 (33.3%) in the pons, nine (21.4%) in both the midbrain and the pons, and one (2.4%) in the brainstem. Among the causes of morbidity in WEBINO patients, 26 (61.9%) had cardiovascular and cerebrovascular diseases, ten (23.8%) neurological diseases, three (7.1%) infectious diseases, two (4.8%) tumor-related diseases, one (2.4%) alcohol overdose, and one (2.4%) drug-immune reaction. More details are shown in Table 1.
TABLE 1
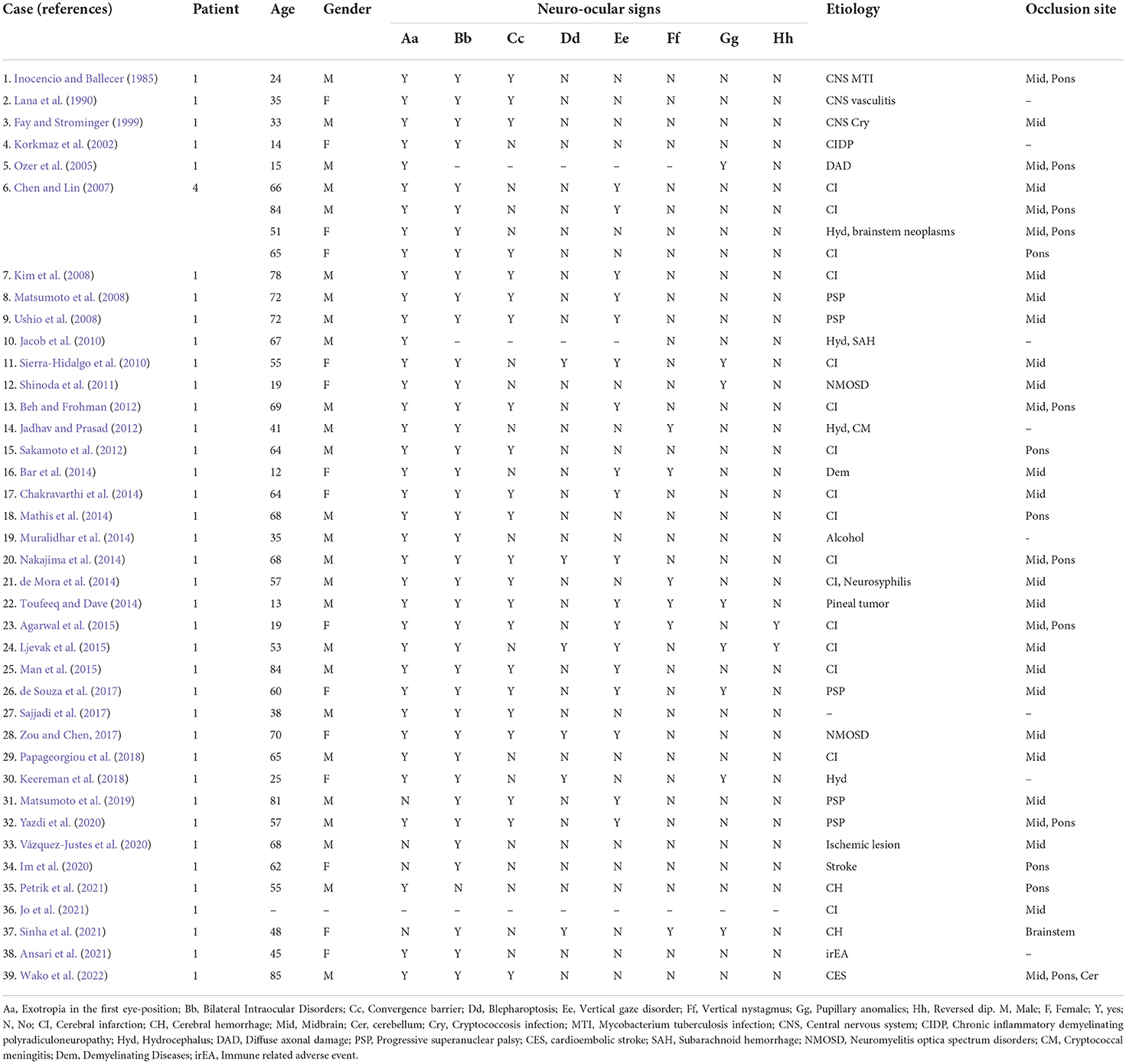
Table 1. Analysis of clinical data of WEBINO patients.
Here we reported a single case of a patient with atypical WEBINO with unilateral exotropia (Supplementary Video) as the main clinical manifestation. The dissociated abducting nystagmus, impaired convergence, and supranuclear vertical gaze palsy implied a lesion of bilateral MLF. Yet, most of the infarcts in the left median dorsal pons cause unilateral, not bilateral, lesion of MLF (Gossman, 2006). The mechanism for the atypical clinical presentation in this patient may be due to the proximity of the unilateral lesion to the midline resulting in bilateral MLF lesions combined with converging fiber involvement resulting in WEBINO. Still, the causal pathophysiology remains unclear and disputed.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statementThe studies involving human participants were reviewed and approved by the Ethics Committee of Harrison International Peace Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributionsJH and TW organized and proofread the writing of the manuscript. DC and TW wrote the manuscript draft. All authors contributed to the article and approved the submitted version.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2022.974645/full#supplementary-material
ReferencesAnsari, J., Mohmmed, Y. E., Ghazal-Aswad, S., Ansari, H., Akhter, S. M., Hadid, O. H., et al. (2021). Rare case of chemotherapy-refractory metastatic vaginal squamous cell carcinoma with complete response to concurrent pembrolizumab and radiotherapy-case report and literature review. Gynecol. Oncol. Rep. 38:100878. doi: 10.1016/j.gore.2021.100878
PubMed Abstract | CrossRef Full Text | Google Scholar
Bar, A., Urbine, J., Bahora, Y., Berkenstock, M., Vodzak, J., Guruprasad, H., et al. (2014). 12-year-old African American girl with subacute bilateral ophthalmoplegia. In: Seminars in Pediatric Neurology (Philadelphia, PA: Elsevier), 173–176.
PubMed Abstract | Google Scholar
Chen, C. M., and Lin, S. H. (2007). Wall-eyed bilateral internuclear ophthalmoplegia from lesions at different levels in the brainstem. J. Neuroophthalmol. 27, 9–15. doi: 10.1097/WNO.0b013e3180334e8d
PubMed Abstract | CrossRef Full Text | Google Scholar
de Mora, M. R. C., Moreno, G. R., and Contreras, M. E. (2014). Webino syndrome caused by meningovascular syphilis. a rare entity with an unexpected cause. Arch Soc Esp Oftalmol. 89, 199–202. doi: 10.1016/j.oftale.2014.07.001
PubMed Abstract | CrossRef Full Text | Google Scholar
de Souza, L. C., Resende, E. D. P. F., Magalhães, D., Teixeira, A. L., and Gomez, R. S. (2017). Wall-eyed bilateral internuclear ophtalmoplegia (WEBINO) in a patient with Richardson's syndrome-Progressive supranuclear palsy. Parkinsonism Relat. Disord. 41, 121–123. doi: 10.1016/j.parkreldis.2017.05.006
PubMed Abstract | CrossRef Full Text | Google Scholar
Fay, P. M., and Strominger, M. B. (1999). Wall-eyed bilateral internuclear ophthalmoplegia in central nervous system cryptococcosis. J. Neuroophthalmol. 19, 131–135. doi: 10.1097/00041327-199906000-00052
PubMed Abstract | CrossRef Full Text | Google Scholar
Gossman, M. (2006). Stroke: Pathophysiology, Diagnosis and Management. Philadelphia, PA: LWW.
Im, K., Ju, H., Lee, M., and Roh, H. A. (2020). Case report of wall-eyed bilateral internuclear ophthalmoplegia with bilateral facial Palsy. J. Stroke Cerebrovasc. Dis. 29, 105–139. doi: 10.1016/j.jstrokecerebrovasdis.2020.105139
PubMed Abstract | CrossRef Full Text | Google Scholar
Inocencio, F. P., and Ballecer, R. (1985). Tuberculosis granuloma in the midbrain causing wall-eyed bilateral internuclear ophthalmoplegia (Webino). J. Clin. Neuroophthalmol. 5, 31–35.
PubMed Abstract | Google Scholar
Jacob, J. T., Burns, J. A., Dupont, S. A., Lanzino, G., and Wijdicks, E. F. (2010). Wall-eyed bilateral internuclear ophthalmoplegia after ruptured aneurysm. Arch. Neurol. 67, 636–637. doi: 10.1001/archneurol.2010.60
PubMed Abstract | CrossRef Full Text | Google Scholar
Jo, Y. -S., Hong, J. Y., Kim, S. Y., and Na, S. -J. (2021). Wall-Eyed Bilateral Internuclear Ophthalmoplegia (WEBINO) in a patient with a unilateral midbrain infarction. Neurologist 26, 153–155. doi: 10.1097/NRL.0000000000000332
PubMed Abstract | CrossRef Full Text | Google Scholar
Keereman, V., Platteau, E., Crevits, L., and Algoed, L. (2018). Wall-eyed bilateral internuclear ophthalmoplegia (WEBINO) in a patient with idiopathic intracranial hypertension. Neurologist 23, 157–159. doi: 10.1097/NRL.0000000000000192
PubMed Abstract | CrossRef Full Text | Google Scholar
Kim, J., Jeong, S. -H., Oh, Y -M., Yang, Y. S., and Kim, S. (2008). Teaching NeuroImage: Wall-eyed bilateral internuclear ophthalmoplegia (WEBINO) from midbrain infarction. Neurology 70:e35. doi: 10.1212/01.wnl.0000299904.48116.cf
PubMed Abstract | CrossRef Full Text | Google Scholar
Korkmaz, A., Topaloglu, H., and Kansu, T. (2002). Wall eyed bilateral internuclear ophthalmoplegia in chronic inflammatory demyelinating polyneuropathy. Eur. J. Neurol. 9, 691–692. doi: 10.1046/j.1468-1331.2002.00447_5.x
PubMed Abstract | CrossRef Full Text | Google Scholar
Lana, M. A., Moreira, P. R. R., and Neves, L. B. (1990). Wall-eyed bilateral internuclear ophthalmoplegia (Webino syndrome) and myelopathy in pyoderma gangrenosum. Arq. Neuropsiquiatr. 48, 497–501. doi: 10.1590/S0004-282X1990000400016
PubMed Abstract | CrossRef Full Text | Google Scholar
Ljevak, J., Mišmaš, A., Poljaković, Z., and Habek, M. (2015). Bilateral ptosis with wall-eyed bilateral internuclear ophthalmoplegia and vertical gaze paralysis. Neurol. Sci. 36, 473–475. doi: 10.1007/s10072-014-1838-x
PubMed Abstract | CrossRef Full Text | Google Scholar
Man, B. L., Chi, M. S., and Fu, Y. P. (2015). Wall-eyed bilateral internuclear ophthalmoplaegia (WEBINO) from a paramedian mesencephalic infarct. Case Rep. 2015:bcr2014207240. doi: 10.1136/bcr-2014-207240
PubMed Abstract | CrossRef Full Text | Google Scholar
Mathis, T., Ducray, F., Tilikete, C., Vighetto, A., and Biotti, D. (2014). Pontine infarction responsible for wall-eyed bilateral internuclear ophthalmoplegia syndrome. Neurol. Clin. Pract. 4, 524–525. doi: 10.1212/CPJ.0000000000000063
PubMed Abstract | CrossRef Full Text | Google Scholar
Matsumoto, H., Inaba, T., Kakumoto, T., Miyano, R., Uchio, N., Sakurai, Y., et al. (2019). Progressive supranuclear palsy with wall-eyed bilateral internuclear ophthalmoplegia syndrome: authors' second case. Case Rep. Neurol. 11, 205–208. doi: 10.1159/000501394
PubMed Abstract | CrossRef Full Text | Google Scholar
Matsumoto, H., Ohminami, S., Goto, J., and Tsuji, S. (2008). Progressive supranuclear palsy with walleyed bilateral internuclear ophthalmoplegia syndrome. Arch. Neurol. 65, 827–829. doi: 10.1001/archneur.65.6.827
PubMed Abstract | CrossRef Full Text | Google Scholar
Muralidhar, R., Chandrasekhar, C., Ramamurthy, D., and Kanthappan, P. (2014). WEBINO after binge drinking. J. Pediatr. Ophthalmol. Strabismus 51, 256–256. doi: 10.3928/01913913-20140604-04
PubMed Abstract | CrossRef Full Text | Google Scholar
Nakajima, N., Ueda, M., and Katayama, Y. (2014). Brainstem infarction with wall-eyed bilateral internuclear ophthalmoplegia syndrome and vertical one-and-a-half syndrome. J. Stroke Cerebrovasc. Dis. 23, e291–e293. doi: 10.1016/j.jstrokecerebrovasdis.2013.11.012
PubMed Abstract | CrossRef Full Text | Google Scholar
Ozer, F., Mutlu, A., Meral, H., Kansu, T., and Carsancakli, B. (2005). Wall-eyed bilateral internuclear ophtalmoplegia presenting as monocular alternating nystagmus: a non-epileptic phenomenon in a case of diffuse axonal injury. Epilept. Disord. 7, 53–56.
PubMed Abstract | Google Scholar
Papageorgiou, E., Tsironi, E. E., Androudi, S., and Koltsidopoulos, P. (2018). Teaching video neuroimages: pulsatile proptosis and wall-eyed bilateral internuclear ophthalmoplegia. Neurology 90, e1542–e1543. doi: 10.1212/WNL.0000000000006462
PubMed Abstract | CrossRef Full Text | Google Scholar
Sakamoto, Y., Kimura, K., Iguchi, Y., Shibazaki, K., and Miki, A. A. (2012). small pontine infarct on DWI as a lesion responsible for wall-eyed bilateral internuclear ophthalmoplegia syndrome. Neurol. Sci. 33, 121–123. doi: 10.1007/s10072-011-0647-8
PubMed Abstract | CrossRef Full Text | Google Scholar
Sharpe, J. A., Rosenberg, M. A., Hoyt, W. F., and Daroff, R. B. (1974). Paralytic pontine exotropia: a sign of acute unilateral pontine gaze palsy and internuclear ophthalmoplegia. Neurology 24, 1076–1076. doi: 10.1212/WNL.24.11.1076
PubMed Abstract | CrossRef Full Text | Google Scholar
Shinoda, K., Matsushita, T., Furuta, K., Isobe, N., Yonekawa, T., Ohyagi, Y., et al. (2011). Wall-eyed bilateral internuclear ophthalmoplegia (WEBINO) syndrome in a patient with neuromyelitis optica spectrum disorder and anti-aquaporin-4 antibody. Multiple Scler. J. 17, 885–887. doi: 10.1177/1352458510391690
PubMed Abstract | CrossRef Full Text | Google Scholar
Sierra-Hidalgo, F., Moreno-Ramos, T., Villarejo, A., Martín-Gil, L., de Pablo-Fernández, E., Correas-Callero, E., et al. (2010). A variant of WEBINO syndrome after top of the basilar artery stroke. Clin. Neurol. Neurosurg. 112, 801–804. doi: 10.1016/j.clineuro.2010.06.004
PubMed Abstract | CrossRef Full Text | Google Scholar
Sinha, S., Naik, B. B., and Ghanekar, J. (2021). Wall eyed bilateral internuclear ophthalmoplegia (WEBINO) syndrome as a false localising sign in intracranial haemorrhage due to snake bite. BMJ Case Rep. 14, e244830. doi: 10.1136/bcr-2021-244830
PubMed Abstract | CrossRef Full Text | Google Scholar
Ushio, M., Iwasaki, S., Chihara, Y., and Murofushi, T. (2008). Wall-eyed bilateral internuclear ophthalmoplegia in a patient with progressive supranuclear palsy. J. Neuroophthalmol. 28, 93–96. doi: 10.1097/WNO.0b013e318175ccfe
PubMed Abstract | CrossRef Full Text | Google Scholar
Vázquez-Justes, D., Martín-Cucó, A., Gallego-Sánchez, Y., and Vicente-Pascual, M. (2020). WEBINO syndrome (wall-eyed bilateral internuclear ophthalmoplegia) secondary to ischemic stroke, about a case. Arch. Soc. Esp. Oftalmol. 95, 205–208. doi: 10.1016/j.oftale.2019.12.008
PubMed Abstract | CrossRef Full Text | Google Scholar
Wako, S., Toi, S., Mizuno, T., Nishimura, A., Ishizuka, K., Kitagawa, K. A., et al. (2022). Case of cardioembloic stroke with wall-eyed bilateral internuclear ophthalmoplegia (WEBINO) syndrome. Clin. Neurol. 62, 541–545. (2022). doi: 10.5692/clinicalneurol.cn-001701
PubMed Abstract | CrossRef Full Text | Google Scholar
Zou, Z., and Chen, W. (2017). Can Wernekink commissure syndrome and wall-eyed bilateral internuclear ophthalmoplegia be ascribed to neuromyelitis optica spectrum disorder? Neurol. Sci. 38, 2053–2055. doi: 10.1007/s10072-017-3041-3
留言 (0)