One-lung ventilation (OLV) has become a widely used ventilatory method for clinical anesthesia in cardiothoracic surgery. It is particularly important for the smooth conduct of procedures, such as lung resection under thoracoscopy and radical esophageal cancer surgery. Lung isolation not only prevents contamination of the healthy lung by secretions or purulent blood from the diseased lung, but also prevents collapse of the operated lung, reduces interference with the surgical field, facilitates surgical manipulation, and reduces mechanical injury to the non-resected lung. However, OLV is a non-physiological ventilatory method that can lead to a sudden decrease in the ventilation/perfusion ratio in the non-ventilated lung, resulting in hypoxemia and triggering hypoxic pulmonary vasoconstriction, thereby worsening ischemia in the collapsed lung. During the ischemia of the collapsed lung, the alveolar-capillary barrier can be disrupted, stimulating the release of a large number of pro-inflammatory mediators such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) from alveolar macrophages. This leads to an increase in inflammatory cytokine levels, a decrease in nitric oxide metabolites, an increase in pulmonary capillary permeability, and, ultimately, lung edema, resulting in worsening of lung injury (1–3). Following reventilation of the collapsed lung and reperfusion of the ischemic area, large amounts of reactive oxygen species (ROS) and inflammatory mediators are released, leading to oxidative stress damage and inflammatory responses and resulting in lung ischemia-reperfusion injury (4).
Remimazolam is an ultrashort-acting benzodiazepine sedative. It has the advantages of fast onset, rapid recovery, minimal respiratory and circulatory system suppression, and a low potential for accumulation after long-term use (5). It is currently widely used in painless endoscopy, sedation diagnosis, treatment in intensive care units, and sedation of patients under general anesthesia. Remimazolam primarily acts on gamma-aminobutyric acid (GABA) A receptors. GABA inhibits ROS generation and enhances the antioxidant system, thereby reducing cell apoptosis (6). The GABA signaling pathway also participates in airway inflammatory reactions and inhibits the production of inflammatory factors (7). However, whether remimazolam effectively suppresses oxidative stress and inflammatory reactions has not yet been confirmed. Particularly, there is limited research on the lung-protective effects of remimazolam in patients undergoing thoracic surgery for OLV. Thus, this study aimed to explore the protective effects of remimazolam against oxidative stress and inflammatory injury in patients with OLV undergoing thoracic surgery.
2 Materials and methods 2.1 Study design and patientsThis was a randomized controlled trial, study was approved by the First Affiliated Hospital of Harbin Medical University Ethics Committee (approval number: 202231) and was conducted according to the tenets of the Declaration of Helsinki. Informed consent was obtained from all patients or their family members.
The calculation basis and formula of sample size are n=2σ2(tα+tβ)2(μ1−μ2)2. According to the formula n = 44. The sample size of the two groups was respectively 44 cases. The total sample size was 88 cases. A total of 88 patients with lung tumors who underwent elective thoracoscopic lobectomy under general anesthesia with OLV between March 2022 and December 2022 at the First Affiliated Hospital of Harbin Medical University were selected. The patients were randomly divided into two groups using the random number table method: an experimental group (R group) and a control group (Con group), with 44 patients per group (n = 44). The inclusion criteria were as follows: (1) undergoing elective thoracoscopic surgery with OLV under general anesthesia; (2) age 18–65 years; (3) American Society of Anesthesiologist (ASA) classification grade I–II; (4) cardiac function grade I–II; (5) no significant cardiovascular, pulmonary, hepatic, renal, or other important organ diseases. The exclusion criteria were as follows: (1) severe cardiac, pulmonary, hepatic, or renal dysfunction; (2) immune, endocrine, nervous, or mental system diseases; (3) forced expiratory volume in 1 s <50% in pulmonary function tests; (4) preoperative respiratory tract and pulmonary infections; and (5) history of long-term sedative and analgesic drug use. Data on patient characteristics, including sex, age, height, weight, ASA classification, diagnosis, and medical history, were collected from patient case history.
2.2 Surgical protocolNone of the patients were taking any medications preoperatively. After entering the operating room, a radial artery puncture and catheter placement were performed under local anesthesia. Routine monitoring included invasive arterial pressure, electrocardiography, pulse oxygen saturation, end-tidal carbon dioxide pressure, airway resistance, and bispectral index values. In this study, the dosage of remimazolam during the induction and maintenance of general anesthesia was determined in accordance with the instructions. Meanwhile, a pre-experiment was conducted to ensure that patients' blood pressure, heart rate and blood oxygen were stable during the induction and maintenance of general anesthesia, and there was no delay in the awakening time. The study indicates that 0.2 mg/kg of remimazolam used for anesthesia induction and maintenance during general anesthesia is safe and effective, with fewer adverse effects than propofol (8).
During anesthesia induction, the anesthesiologist in the experimental group gave remimazolam at a dose of 0.2 mg/kg intravenous injection, whereas the control group received an equal volume of normal saline using the same method. Both groups were then administered propofol (1–2 mg/kg), rocuronium (1–2 mg/kg), and sufentanil (0.2–0.4 μg/kg). This was followed by double-lumen endotracheal intubation after 4 min using a fiberoptic bronchoscope to adjust the position of the double-lumen tube, which was then connected to the anesthesia machine. The tidal volume was set at 8 ml/kg, and the respiratory rate was set at 12–15 breaths per minute, with an inspiratory-to-expiratory ratio of 1:2. End-tidal carbon dioxide pressure was maintained at 30–40 mmHg. During anesthesia maintenance, the anesthesiologist in the experimental group gave remimazolam at a dose of 0.2 mg/kg/h intravenous injection, whereas the control group received an equivalent volume of normal saline intravenously. Both groups received sevoflurane inhalation continuously, and intermittent intravenous injections of rocuronium (0.2–0.3 mg/kg) and sufentanil were given as needed. The bispectral index values were maintained between 40 and 60 during surgery, and hemodynamic stability was ensured during OLV, with a maintenance of at least 20% above baseline values. Oxygen saturation was maintained above 90%, and airway pressure was maintained below 40 cmH2O. After surgery, the endotracheal tube was removed once the patient regained consciousness and recovered spontaneous breathing, and the patient was transferred to the post-anesthesia care unit (PACU).
2.3 Observation indicatorsThe average arterial pressure, heart rate, oxygen saturation, and respiratory rate were recorded at four time points: immediately upon entering the operating room (T1), immediately after tracheal intubation (T2), immediately after skin incision (T3), and immediately after the completion of surgery (T4). The levels of oxidative stress markers, superoxide dismutase (SOD) and glutathione peroxidase (GSH-Px), as well as inflammatory cytokine markers TNF-α and IL-6, were determined using enzyme-linked immunosorbent assay (ELISA) on arterial blood samples (3 ml) collected at T1 and T4. The dosages of sufentanil and propofol, duration of surgery, time to awakening, duration of stay in the PACU, and postoperative complications such as nausea, vomiting, and agitation were recorded.
2.4 Statistical analysisAll statistical analyses were performed using SPSS software (version 25.0). Data are presented as mean ± standard deviation. The Shapiro–Wilk normality test was used to assess normality, and Levene's test was applied to evaluate the homogeneity of variance. For comparisons between the two groups, an independent sample t-test was used for data that met the assumptions of normality and homogeneity of variance, whereas a corrected Welch t-test was employed for data that conformed to normality but not homogeneity of variance. When the data do not conform to normality, the Mann–Whitney U test was used. For count data between two groups, the χ test was applied. Repetitive data were analyzed using repeated measures of variance. To ensure the accuracy of the comparisons, the Bonferroni correction was applied to adjust for the potential bias resulting from multiple comparisons. The level of statistical significance was set at P < 0.05.
3 Results 3.1 Patient characteristicsThe R group had a mean age of 53.41 ± 8.61 years, and the average height and weight were 164.89 ± 6.62 cm and 64.64 ± 11.96 kg, respectively. There were 16 men and 28 women. With respect to diagnosis, the R group included 35 patients with lung adenocarcinoma and 9 patients with lung nodules. There were 7 and 37 patients with segmentectomy and pulmonary lobectomy, respectively. The ASA classification was II and III in 28 and 16 patients, respectively. The mean duration of surgery was 234.89 ± 44.53 min. Meanwhile, the Con group had a mean age of 56.09 ± 8.03 years, and the average height and weight were 166.91 ± 7.36 cm and 69.20 ± 10.98 kg, respectively. There were 21 men and 23 women, and 37 and 7 patients had lung adenocarcinoma and lung nodules, respectively. There were 8 and 36 patients with segmentectomy and pulmonary lobectomy, respectively. A total of 27 and 17 patients had American Society of Anesthesiologists (ASA) classifications II and III, respectively. The mean duration of surgery was 217.72 ± 57.39 min. Age, sex, height, weight, clinical diagnosis (lung adenocarcinoma and pulmonary nodules), ASA classification, and surgical duration were not significantly different between the two groups (P > 0.05). Further details are listed in Table 1.
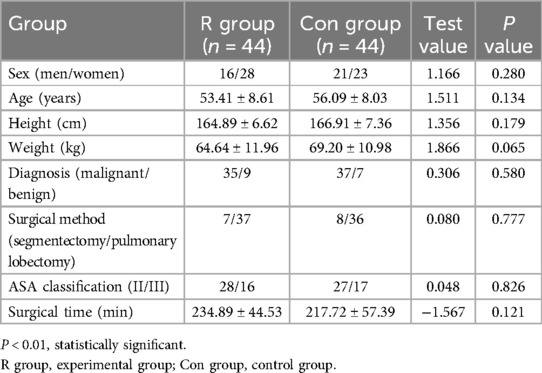
Table 1. Comparison of patient characteristics between the two groups.
3.2 Comparison of oxidative stress response between the two groupsThere were no significant between-group differences in preoperative levels of SOD and GSH-Px (P > 0.05). However, postoperative SOD and GSH-Px levels were significantly higher in the R group than those in the Con group (P < 0.01). In the R group, the SOD and GSH-Px levels were significantly decreased after surgery than that before surgery (P < 0.01). Similarly, the SOD and GSH-Px levels were also significantly decreased after surgery in the Con group (P < 0.01). Further details are shown in Tables 2, 3 and in Figures 1, 2.
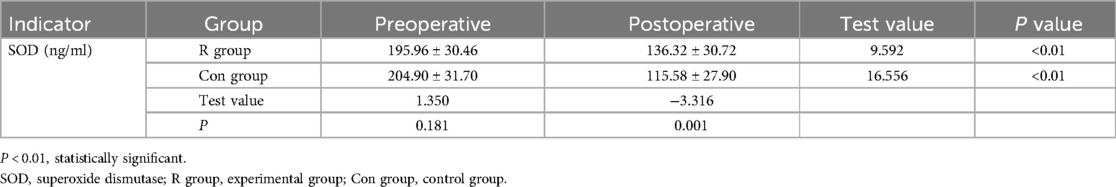
Table 2. Comparison of SOD levels between the two groups.
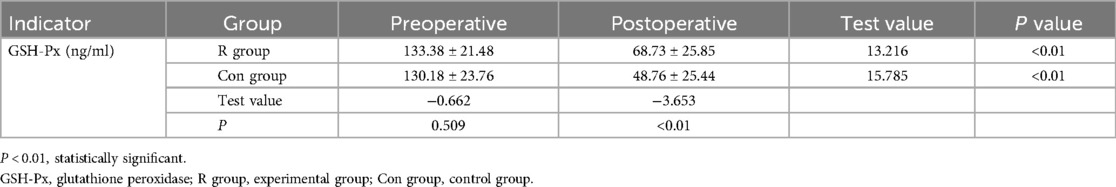
Table 3. Comparison of GSH-Px levels between the two groups.
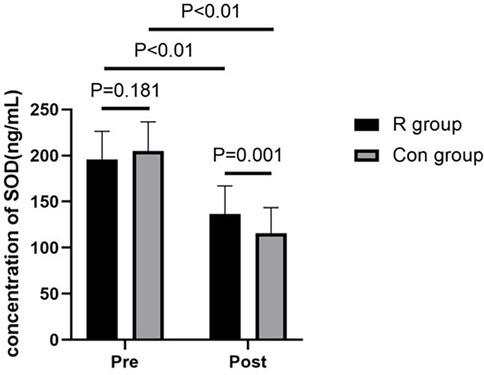
Figure 1. Comparison of SOD levels between the two groups of patients. P < 0.01, statistically significant. SOD, superoxide dismutase; R group, experimental group; Con group, control group.
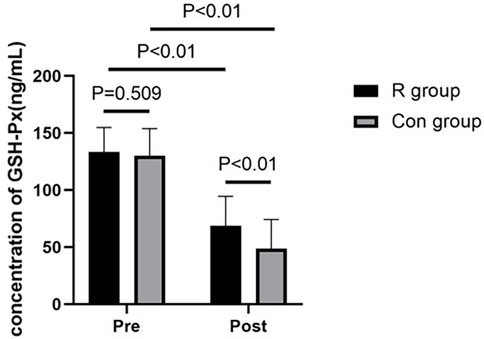
Figure 2. Comparison of GSH-Px levels between the two groups of patients. P < 0.01, statistically significant. GSH-Px, glutathione peroxidase; R group, experimental group; Con group, control group.
3.3 Comparison of serum TNF-α and Il-6 levels between the two groupsThe preoperative TNF-α and IL-6 levels were not significantly different between the R and Con groups (P > 0.05). However, postoperative TNF-α and IL-6 levels were significantly lower in the R group than in the Con group (P < 0.01). The TNF-α and IL-6 levels were significantly increased after surgery in both the R group (P < 0.01) and the Con group (P < 0.01). Further details are shown in Tables 4, 5 and in Figures 3, 4.
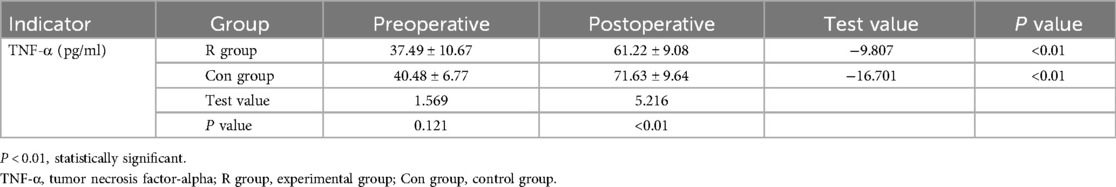
Table 4. Comparison of TNF-α levels between the two groups of patients.
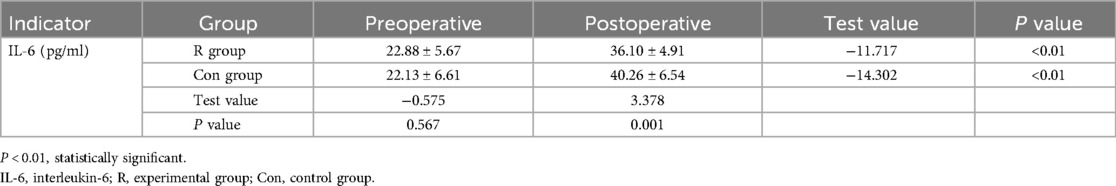
Table 5. Comparison of IL-6 levels between the two groups.
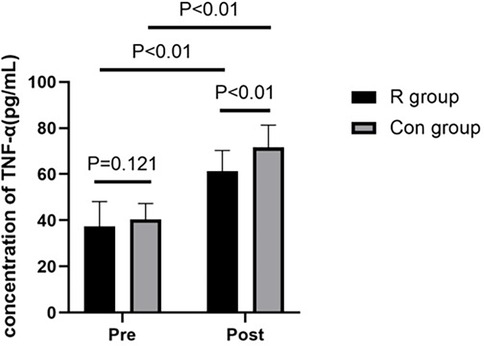
Figure 3. Comparison of TNF-α levels between the two groups of patients. P < 0.01 has statistical significance. TNF-α, tumor necrosis factor-alpha; R group, experimental group; Con group, control group.
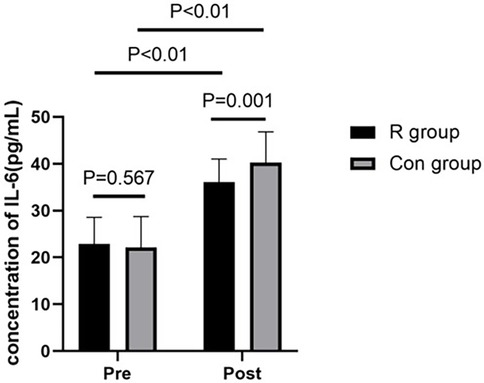
Figure 4. Comparison of IL-6 levels between the two groups of patients. P < 0.01, statistically significant. IL-6, interleukin-6; R, experimental group; Con, control group.
3.4 Comparison of vital signs at different time points between the two groupsSystolic blood pressure, diastolic blood pressure, and heart rate at T1, T3, and T4 were not significantly different between the R and Con groups (all P > 0.05). At T2, the R group had significantly higher systolic blood pressure, diastolic blood pressure, and heart rate than the Con group (P < 0.01, Table 6).

Table 6. Comparison of vital signs at different time points between the two groups.
3.5 Comparison of awakening time and PACU time between the two groupsThere were no significant differences in postoperative recovery time and PACU time between the R and Con groups (P > 0.05, Table 7).
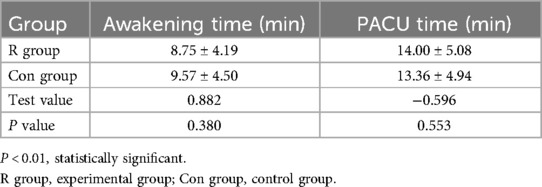
Table 7. Comparison of awakening time and PACU time between the two groups.
3.6 Comparison of incidence of adverse reactions between the two groupsThere was no significant difference in the incidence of postoperative adverse reactions, including nausea and vomiting, respiratory depression, hypotension, and agitation, between the R and Con groups (P > 0.05; Table 8).
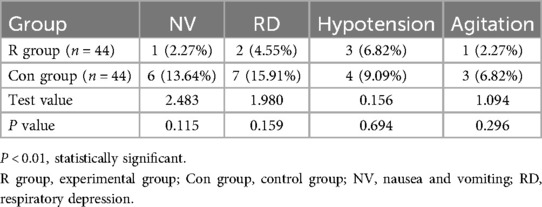
Table 8. Comparison of the incidence of adverse reactions between the two groups.
4 DiscussionThis study found that low-dose (0.2 mg/kg) remimazolam to maintain general anesthesia in patients undergoing OLV can increase the levels of SOD and GSH-Px and decrease the levels of TNF-α and IL-6 in patients undergoing lobectomy with OLV in thoracic surgery. These effects may exert a protective benefit against oxidative stress and inflammatory response damage in patients undergoing OLV, providing clinical evidence to inform decision-making in their management. To our best knowledge, this study is the first to investigate the effect of remimazolam on the oxidative stress response in patients undergoing thoracic surgery with OLV and the first study to show that the use of low-dose remimazolam for the maintenance of general anesthesia can increase the levels of SOD and GSH-Px and reduce oxidative stress reactions in these patients.
OLV is a specialized anesthetic technique widely used in thoracic surgery, including lung resection, esophageal cancer, and thoracic aortic aneurysms, due to its better exposure and reduced damage. It relies on mechanical ventilation with a double-lumen endotracheal tube, ventilating one lung while the other collapses. This ensures surgical field exposure and facilitates procedures. However, OLV can cause ventilation/perfusion mismatch, lung injury, ischemia-reperfusion injury, oxidative stress, alveolar and vascular disruption, inflammation, and severe complications (9). Postoperative mortality after thoracic surgery is mainly due to acute lung injury and acute respiratory distress syndrome, with a 40% mortality rate for the latter (10). The pathophysiological mechanism of lung injury during OLV mainly involves ischemia-reperfusion injury (11), particularly in the non-ventilated lung upon re-ventilation and re-expansion at surgery's end due to hypoxia (12). ROS are released early in ischemia-reperfusion (4), while antioxidants like SOD and GSH-Px become depleted, reducing ROS clearance (13). This leads to nuclear and mitochondrial damage, lipid peroxidation, and apoptosis. ROS also induce inflammatory factors like TNF-α and IL-1β (14), activating neutrophils and causing an oxidative stress response in the lungs.
Remimazolam acts on GABA receptors, especially the GABA-A receptor, with high affinity, increasing the frequency of chloride ion channel opening and enhancing the effects of GABA, thereby producing sedative or hypnotic effects (15). GABA can scavenge reactive intermediates produced during lipid peroxidation and readily react with malondialdehyde under physiological conditions, thereby reducing the malondialdehyde reaction, increasing the activity of SOD and GSH-Px, inhibiting the production of ROS, and enhancing the antioxidant system, ultimately reducing cell apoptosis (6). The current study found that SOD and GSH-Px levels were significantly lower postoperatively than that preoperatively in both the R and Con groups, indicating that OLV induced an oxidative stress response in the body. SOD scavenges superoxide anion radicals, whereas GSH-Px promotes the reduction of peroxides. These are important antioxidant enzymes in the body that play a crucial role in the balance between oxidation and antioxidation. In the current study, postoperative serum levels of SOD and GSH-Px were significantly higher in the R group than in the Con group. This indicates that remimazolam attenuates the oxidative stress response in the body and has a protective effect on the lungs. This evidence provides a new direction for the use of remimazolam under general anesthesia.
OLV can lead to a series of pathological and physiological changes that disrupt the alveolar-capillary barrier. It can also stimulate the release of large amounts of pro-inflammatory mediators from alveolar macrophages (1–3). TNF-α and IL-8 are the most important inflammatory mediators in alveolar macrophages and neutrophils. They are mainly involved in immune response and inflammatory response. They are produced by alveolar macrophages; are increased under trauma, inflammation, and other stresses; and can induce the production of other factors such as IL-6. Therefore, the levels of TNF-α, IL-6, and IL-8 can reflect the severity of the inflammatory response caused by surgical stress. Remimazolam is a GABA receptor agonist, and its effect on GABA-A receptors is dose-dependent. At low doses, it has anxiolytic effects, and the sedative and hypnotic effects predominate as the dose increases (6). GABA and its receptors are widely expressed in the airway epithelium and lung tissues and are involved in the pathological processes of respiratory diseases, such as asthma (16), clearance of lung fluid, and airway inflammatory responses (17). The GABA system plays an important role in the regulation of pulmonary fluid balance, and activation of this system significantly increases the rate of lung fluid clearance, improving acute lung injury (18, 19).
The results of the current study showed that compared to preoperative levels, postoperative TNF-α and IL-6 levels were significantly increased in both the R group and Con group. This indicated that OLV surgery can induce the release of a large amount of inflammatory factors in the body. Postoperative TNF-α and IL-6 levels were significantly lower in the R group than in the Con group, demonstrating that remimazolam can reduce the release of inflammatory factors in the body, providing better protection for the lungs, it may be helpful to the prognosis of the operation. However, this study only studied the effect of remimazolam on the inflammatory response after single lung ventilation, and did not explore its long-term effect on the postoperative inflammatory response. Remimazolam improved neurological function and reduced cerebral damage after ischemia/reperfusion, suggesting protection via inhibiting inflammatory factors (20). Septic mice given remimazolam showed higher survival and lower inflammatory mediators compared to controls, indicating its protective effect in sepsis (21). In elderly cancer patients, remimazolam alleviated inflammation and reduced early postoperative cognitive dysfunction (22).
Activation of the GABA receptor by remimazolam leads to the influx of chloride ions into the cell, subsequently reducing excitability and inhibiting neuronal electrical activity, thereby producing a sedative effect (23). The current study found no significant differences in blood pressure and heart rate between the Con group and R group at T1, T3, and T4, except at T2 where the R group had higher values. This suggests remimazolam's mild effect on circulation and safety in OLV patients. This is consistent with the findings of other researchers. In cardiac valve replacement surgery, remimazolam resulted in lower hemodynamic fluctuations, hypotension, and norepinephrine usage compared to propofol (24).
In out study, no significant differences in awakening time and PACU stay were found between the R group and Con group in OLV patients. This phenomenon has also been observed in other studies. For gastroscopy patients, remimazolam's sedative efficacy was comparable to propofol, with faster alert recovery in the remimazolam group. These results confirm remimazolam's safety and effectiveness, without adverse effects on awakening or prognosis (25). Low-dose remimazolam as an auxiliary anesthetic may explain the absence of differences. Postoperative adverse reactions were similar between groups, supporting remimazolam's safety for anesthesia maintenance in OLV patients. Another study found remimazolam non-inferior to propofol for anesthesia induction and maintenance, with significantly fewer adverse reactions in the remimazolam group, indicating good tolerability (26).
The limitations of this study include its small sample size and the single-center design, which limit the representativeness of the research findings. In the future, we will conduct a large sample multi-center randomized controlled trial. The study only used the enzyme-linked immunosorbent assay method to detect the levels of SOD, GSH-Px, TNF-α, and IL-6, and the experimental methods were relatively simple. This study focused only on clinical experiments and did not investigate the mechanism of action of remimazolam. The mechanism of remimazolam can be studied in the future.
In summary, low-dose remimazolam can enhance SOD and GSH-Px levels while reducing TNF-α and IL-6 levels, thereby preventing oxidative stress and inflammatory response damage. Additionally, it does not compromise hemodynamic stability, recovery time, or PACU duration, and exhibits fewer adverse reactions. Therefore, low-dose remimazolam can provide lung-protective effects for patients undergoing OLV during the induction and maintenance of general anesthesia.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statementThe studies involving humans were approved by the First Affiliated Hospital of Harbin Medical University Ethics Committee (approval number: 202231). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. The manuscript presents research on animals that do not require ethical approval for their study.
Author contributionsSL: Data curation, Investigation, Writing – review & editing. SS: Conceptualization, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. DW: Conceptualization, Investigation, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This project was funded by the Zhongguancun Precision Medicine Foundation of China. Fund number is 320.21.2022.02.17.
AcknowledgmentsThe authors would like to thank all of the trial participants. They would also like to thank all of the doctors, nurses and research departments who collaborated in this study.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AbbreviationsASA, American Society of Anesthesiologist; GABA, gamma-aminobutyric acid; GSH-Px, glutathione peroxidase; IL-6, interleukin-6; OLV, One-lung ventilation; PACU, post-anesthesia care unit; ROS, reactive oxygen species; SOD, superoxide dismutase; TNF, tumor necrosis factor-alpha.
References2. Kozian A, Schilling T, Freden F, Fredén F, Maripuu E, Röcken C, et al. One-lung ventilation induces hyperperfusion and alveolar damage in the ventilated lung: an experimental study. Br J Anaesth. (2008) 100(4):549–59. doi: 10.1093/bja/aen021
PubMed Abstract | Crossref Full Text | Google Scholar
4. Zhu Z, Shi Z, Xie C, Gong W, Hu Z, Peng Y. A novel mechanism of gamma-aminobutyric acid(GABA) protecting human umbilical vein endothelial cells (HUVECs) against H2O2-induced oxidative injury. Comp Biochem Physiol C. (2019) 21(7):68–75. doi: 10.1016/j.cbpc.2018.11.018
Crossref Full Text | Google Scholar
5. Oka S, Satomi H, Sekino R, Taguchi K, Kajiwara M, Oi Y, et al. Sedation outcomes for remimazolam, a new benzodiazepine. Oral Sci. (2021) 63(3):209–11. doi: 10.2334/josnusd.21-0051
PubMed Abstract | Crossref Full Text | Google Scholar
7. Munroe ME, Businga TR, Kline JN, Bishop GA. Anti-inflammatory effects of the neurotransmitter agonist honokiol in a mouse model of allergic asthma. J Immunol. (2010) 185(9):5586–97. doi: 10.4049/jimmunol.1000630
PubMed Abstract | Crossref Full Text | Google Scholar
8. Dai G, Pel L, Duan F, Liao M, Zhang Y, Zhu M, et al. Safety and efficacy of remimazolam compared with propofol in induction of general anesthesia. Mnerva Anestesiol. (2021) 87(10):1073–9. doi: 10.23736/S0375-9393.21.15517-8
PubMed Abstract | Crossref Full Text | Google Scholar
9. Marret E, Cinotti R, Berard L, Piriou V, Jobard J, Barrucand B, et al. Protective ventilation during anaesthesia reduces major postoperative complications after lung cancer surgery: a double-blind randomised controlled trial. Eur J Anaesthesiol. (2018) 35(10):727–35. doi: 10.1097/EJA.0000000000000804
PubMed Abstract | Crossref Full Text | Google Scholar
10. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. (2016) 315(8):788–800. doi: 10.1001/jama.2016.0291
PubMed Abstract | Crossref Full Text | Google Scholar
11. Lohser J, Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg. (2015) 121(2):302–18. doi: 10.1213/ANE.0000000000000808
PubMed Abstract | Crossref Full Text | Google Scholar
13. Caldeira DEdS, Souza MEJ, Gomes MCJ, Picinato MANC, Fina CF, Feres O, et al. Effects of hyperbaric oxygen (HBO), as pre-conditioning in liver of rats submitted to periodic liver ischemia/reperfusion. Acta Cir Bras. (2013) 28(1):66–71. doi: 10.1590/S0102-86502013001300013
PubMed Abstract | Crossref Full Text | Google Scholar
14. Lapenna D, Ciofani G, Pierdomenico SD, Giamberardino MA, Cuccurullo F. Reaction conditions affecting the relationship between thiobarbituric acid reactivity and lipid peroxides in human plasma. Free Radic Biol Med. (2001) 31(3):331–5. doi: 10.1016/S0891-5849(01)00584-6
PubMed Abstract | Crossref Full Text | Google Scholar
16. Xiang Y-Y, Wang S, Liu M, Hirota JA, Li J, Ju W, et al. A GABAergic system in airway epithelium is essential for mucus overproduction in asthma. Nat Med. (2007) 13(7):862–7. doi: 10.1038/nm1604
PubMed Abstract | Crossref Full Text | Google Scholar
18. Zhu T, Zhang W, Wang DX, Huang NW, Bo H, Deng W, et al. Rosuvastatin attenuates mucus secretion in a murine model of chronic asthma by inhibiting the gamma-aminobutyric acid type A receptor. Chin Med J (Engl). (2012) 125(8):1457–64.22613653
PubMed Abstract | Google Scholar
19. Chintagari NR, Lin L. GABA receptor ameliorates ventilator-induced lung injury in rats by improving alveolar fluid clearance. Crit Care. (2011) 16(2):1–9. doi: 10.1186/cc11298
Crossref Full Text | Google Scholar
20. Shi M, Chen J, Liu T, Dai W, Zhou Z, Chen L, et al. Protective effects of remima-zolam on cerebral ischemia/reperfusion injury in rats by inhibit-ing of NLRP3 inflammasome-dependent pyroptosis. Drug Des Devel Ther. (2022) 16:413–23. doi: 10.2147/DDDT.S344240
PubMed Abstract | Crossref Full Text | Google Scholar
21. Liu X, Lin S, Zhong Y, Shen J, Zhang X, Luo S, et al. Remimazolam protects against LPS-induced endotoxicity improving survival of endotoxemia mice. Front Pharmacol. (2021) 11(12):739603. doi: 10.3389/fphar.2021.739603
Crossref Full Text | Google Scholar
22. Liao YQ, Min J, Wu ZX, Hu Z. Comparison of the effects of remimazolam and dexmedetomidine on early postoperative cognitive function in elderly patients with gastric cancere. Front Aging Neurosci. (2023) 6(15):1123089. doi: 10.3389/fnagi.2023.1123089
Crossref Full Text | Google Scholar
23. Jacob TC, Moss SJ, Jurd R. GABA(A) receptor trafficking and its role in the dynamic modulation of neuronal inhibition. Nat Rev Neurosci. (2008) 9(5):331–43. doi: 10.1038/nrn2370
PubMed Abstract | Crossref Full Text | Google Scholar
24. Liu TX, Lai T, Chen J, Lu Y, He F, Chen Y, et al. Effect of remimazolam induction on hem-odynamics in patients undergoing valve replacement surgery: a randomized, double-blind, controlled trial. Pharmacol Res Perspect. (2021) 9(5):851–7. doi: 10.1002/prp2.851
Crossref Full Text | Google Scholar
25. Chen S, Yuan T, Zhang J, Bai H, Tian M, Pan C, et al. Remimazolam tosi-late in upper gas-trointestinal endoscopy: a multi-center, randomized, non-inferiority, phase III trial. J Gastroenterol Hepatol. (2021) 36(2):474–81. doi: 10.1111/jgh.15188
PubMed Abstract | Crossref Full Text | Google Scholar
26. Doi M, Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. (2020) 34(4):543–53. doi: 10.1007/s00540-020-02788-6
留言 (0)