Lumbar disc herniation is a common spinal surgical disease, especially in elderly population, with low back pain and sciatica being its main clinical symptoms (1, 2). Although it usually responds favorably to conservative treatment, surgical decompression is necessary in a small percentage of them. For patients with unilateral disc herniation, microscopic surgery is a common choice to minimize the damage (3, 4), but microscopic or endoscopic minimally invasive approaches may not be suitable for all cases. Studies have suggested that minimally invasive techniques may not be effective enough to achieve satisfactory outcomes in Carragee type II and IV hernias, which are more prone to recurrent disc herniation and segmental instability (5, 6). Clinical evidence shows that decompression surgery such as lumbar discectomy and vertebral fusion can improve low back pain and sciatica (7, 8). For patients with unilateral disc herniation, the less trauma surgery such as transforaminal lumbar interbody fusion (TLIF) can also improve both lower back pain and sciatica and most patients can achieve good results, but there are still some patients who are not satisfied with the surgical results (9).
The purpose of performing lumbar surgery is to alleviate the pain of the patients and achieve satisfactory therapeutic effects. Satisfaction or dissatisfaction are both subjective feelings experienced by patients. However, the factors that lead to dissatisfaction among patients undergoing transforaminal lumbar interbody fusion surgery are not yet known. In view of this, the objective of this study is to investigate the factors contributing to patients' dissatisfaction following TLIF surgery, in order to offer valuable insights to clinicians.
Materials and methods PatientsWe conducted a retrospective analysis of 625 patients who received TLIF from March 2018 to December 2021. Informed consent was obtained from each patient, and the study was approved by the ethics review board of our hospital and acquired a unique identification number for research registration (the research registration number is 20241111).
The inclusion criteria consisted of patients who: (1) were aged 18 years or older, (2) presence of mechanical back and unilateral radicular leg pain caused by lumbar disc herniation, (3) failure of conservative treatment to alleviate the radicular pain, (4) confirmation of lumbar disc herniation through magnetic resonance imaging (MRI) findings, and (5) follow up to study endpoint. Exclusion criteria were: (1) Other severe spinal diseases such as spinal tumors, spinal tuberculosis, and pyogenic spinal infections, (2) spinal mechanical instability, such as lumbar spondylolisthesis or segmental instability, (3) unwillingness to participate in the study, and (4) lumbar spine surgery history.
Surgical techniqueAfter general anesthesia, the patient is placed in a prone position with the abdomen suspended to reduce intra-abdominal pressure, thereby reducing bleeding from the venous plexus in the spinal canal during decompression operations. A midline incision on the lower back should be made, cutting through the skin and subcutaneous tissue. Then, the paraspinal muscles should be carefully removed from under the periosteum to reveal the vertebral plate and facet joints. Pedicle screws were placed, and then the lower articular process of one side of the upper vertebral body and the upper articular process of the lower vertebral body was bitten off by the vertebral plate clamp. When removing the ligamentum flavum, the dural sac is protected by the nerve peeler to prevent tearing the dura mater. The deep ligamentum flavum was removed and the lateral recess was decompressed. Then the hypertrophic ligamentum flavum and residual joint capsule were removed from the intervertebral foramen and lateral recess.
Expose the intervertebral disc from the intervertebral foramen area. Use a sharp knife to cut through the fibrous ring on the surface of the intervertebral disc. Use nucleus pulposus forceps to remove degenerated nucleus pulposus tissue from the intervertebral disc. Scrape off the upper and lower cartilage endplates and determine the type of intervertebral fusion cage. Wash the intervertebral space with sterile physiological saline, implant autologous bone, allogeneic bone fragments, and fusion cage and ensure the presence of bone tissue around the fusion cage. Place the appropriate length of the bowl rod and bending, and place the screw tail cap. Cover the surface of the dural sac with gelatin sponge. Place drainage tube and suture the layers.
Clinical indexesThis study includes the collection of clinical indicators from the cases and follow-up results at 2 years after surgery. These include age, gender, osteoporosis, body mass index (BMI), painful limbs, hypertension, diabetes, occupation, lesion segment (multi segment, high-level segment), preoperative pain time, operation time, intraoperative blood loss, postoperative wound drainage, wound infection, deep vein thrombosis (DVT), preoperative visual analog scale (VAS)-back, postoperative VAS-back, postoperative rehabilitation training, complication, feel depression 2 years after discectomy, symptom recurrence and level of satisfaction.
Osteoporosis was diagnosed with the aid of x-ray or computerized tomography (CT) findings. In continuous variables, except for age and BMI, all other variables are defined by median as their high and low values. Obesity was defined as having a BMI of no less than 28. Advanced age is defined as the patient's age not less than 60 years old. Patients were divided into mental workers and manual workers according to their occupation. The patients, who undertook a small amount of manual labor and worked mainly indoor, were regarded as mental workers. The patients, who undertook a large amount of manual labor and worked mainly outdoor, were regarded as manual workers. The level of patient satisfaction with the treatment outcome was determined using the patient satisfaction index (PSI) (10). A PSI of 1 or 2 is considered satisfactory, while a PSI of 3 or 4 is considered unsatisfactory. DVT records did not include cases of lower extremity intermuscular thrombosis because this type of thrombosis was classified as a peripheral variant of DVT and essentially limited to the venous plexus of soleus and gastrocnemius. Studies have shown that lower extremity venous intermuscular thrombosis has almost no impact on patients (11). Postoperative rehabilitation training starts on the second day after surgery and lasts until three months after surgery and it is mainly for lumbar core muscle training. The Zung Self-Rating Depression Scale (ZSRDS) (12), a 20-item self-administrated questionnaire, was used to measure the severity of depressive symptoms. ZSRDS consists of 10 express negative experience and 10 express positive experience. The ZSRDS scores on the test range from 25 through 100. An ZSRDS score = 50 suggests clinically significant symptoms with the following three levels of severity ratings: score 25–49 response normal; score 50–59 response mild to moderate; score 60–69 response moderate to severe; and score no less than 70 responses severe (13, 14). Symptom recurrence is a result discussed by the group of expert and manifests as lower back pain and sciatica caused by lumbar disc herniation either on the opposite side of the initial treatment site or in adjacent segments.
Follow up and end pointFollow up of patients after discharge is necessary. Generally, patients are scheduled for regular follow-up examinations at one month, three months, six months, one year and two years after surgery. However, it is important to note that if patients experience sudden situations such as significant back pain and lower limb neuralgia, they can come for diagnosis at any time. This study would have two endpoints. One is that during a 2-year period, the patient experienced severe back pain and lower limb neuralgia again and after being diagnosed with symptom recurrence through MRI examination, the time and VAS-back were recorded. The other is 2 years after surgery, at this point, all patients except those who have already completed the study would be evaluated.
StatisticsThis study is based on binary logistic regression analysis to calculate the minimum sample size required. In this study, stepwise binary logistic regression was applied to eliminate confounding factors, and patient dissatisfaction level was used as the dependent variable for comparative analysis. The chi square test was used for univariate analysis, and variables with p ≤ 0.05 were separately subjected to binary logistic regression analysis to exclude confounding variables with p > 0.05. Then, the remaining variables were included in the binary logistic regression model with dissatisfaction level as the dependent variable. For each variable, we calculated the odds ratio (OR) of its 95% confidence interval (CI). In the chi-square test and multivariate logistic regression model, except for age and BMI, all the other continuous variables were defined by the median. All statistical analyses were done using SPSS software version 27.0 (SPSS, Inc., Chicago, IL, USA).
Result General informationAccording to the sample size calculation formula, the minimum sample size required for this study is 323, which is much smaller than the actual sample size in this study. A total of 660 patients were included in the study. Of these, 24 patients with spinal mechanical instability and 11 who refused the second evaluation were excluded. Finally, 625 patients who met the inclusion criteria from March 2018 to December 2021 were included in this study. Among them, there were 296 male patients (47.4%) and 329 female patients (52.6%). The average age and BMI were 54.9 years old and 26.48 kg/m2, respectively. According to PSI, patients are divided into two groups, 529 patients (84.6%) in satisfied group showing 1 or 2 stage in PSI and 96 patients (15.4%) in dissatisfied group showing 3 or 4 stage in PSI (Table 1).
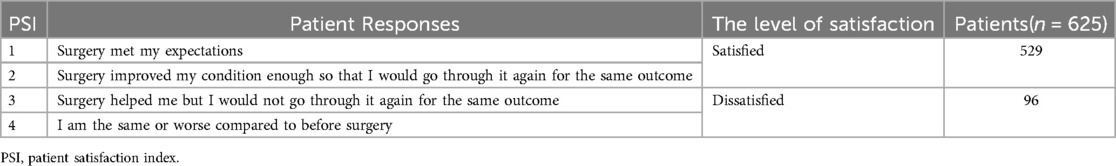
Table 1. Patient satisfaction index (PSI).
Univariate analysis of factors related to postoperative patient dissatisfactionAt baseline, there was no difference between the two groups in gender, age, occupation, hypertension, diabetes, painful limbs and preoperative VAS-back. Compared to satisfied patients, the dissatisfied patients had longer preoperative pain time and higher BMI (Table 2). For the collected clinical information, there was no difference between the two groups in terms of surgical segment (including high and multiple segments), surgical time, wound drainage volume, and postoperative thrombosis. Compared to satisfied patients, dissatisfied patients had higher postoperative VAS-back, intraoperative bleeding volume, incidence of depression and symptom recurrence rate (Table 3).
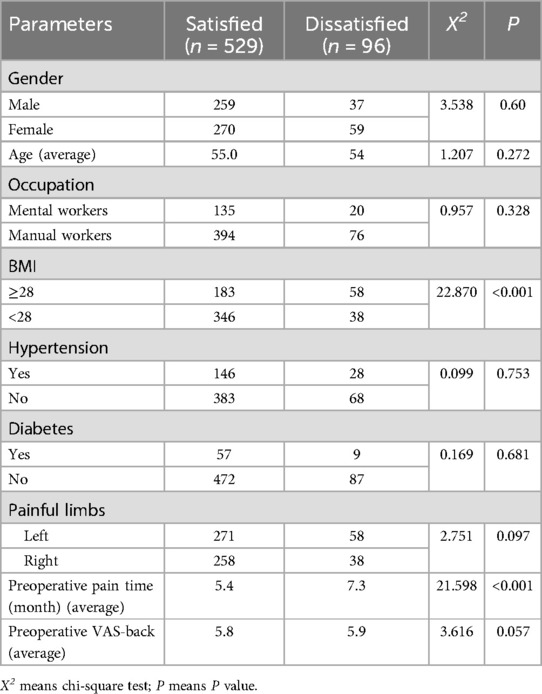
Table 2. Basic information of 625 patients.
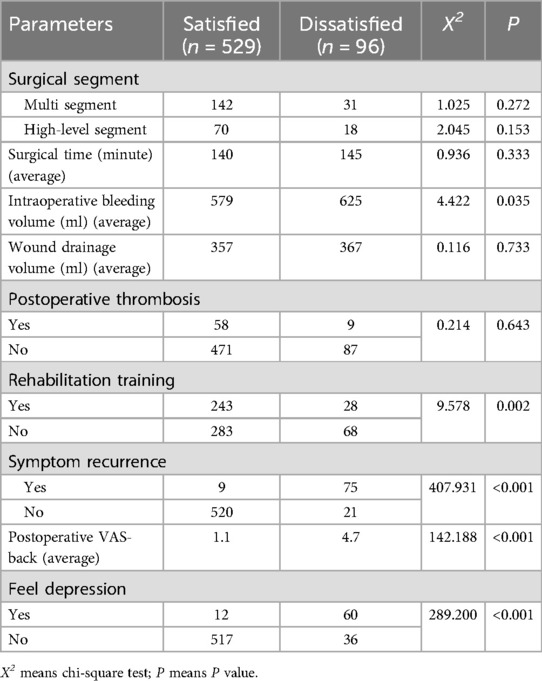
Table 3. Surgical related information and 2-year follow-up after surgery of 625 patients.
Handling of confounding factorsPerform binary logistic regression analysis separately with postoperative dissatisfaction level as the dependent variable for the following factors: BMI, preoperative pain duration, intraoperative bleeding volume, postoperative VAS-back, feel depression, postoperative rehabilitation training and symptom recurrence. When comparing the above factors with postoperative dissatisfaction levels, no confounding factors were found, and they all had statistical significance. Table 4 showed detailed data for excluding confounding factors.
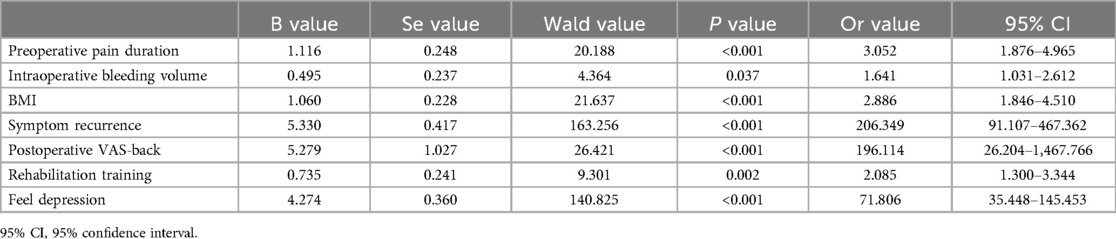
Table 4. Individual logistic regression analysis excludes confounding factors.
Factors of patient dissatisfaction after discectomy identified by multivariate analysisThe following variables were included as input into the multivariate model: BMI, preoperative pain duration, intraoperative bleeding volume, postoperative VAS-back, feel depression, rehabilitation training and symptom recurrence. When included in a multivariate logistic regression model, BMI, preoperative pain duration, rehabilitation training, feel depression and symptom recurrence were independently associated with patient dissatisfaction 2 years after discectomy (Table 5).
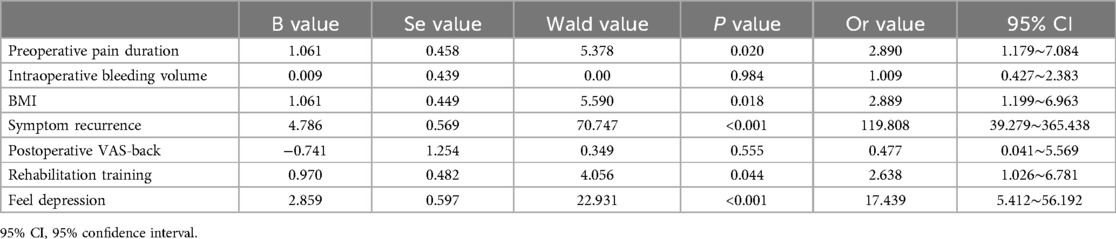
Table 5. Factors of patient dissatisfaction after discectomy identified by multivariate analysis.
DiscussionIn this study, a total of 625 patients with lumbar disc herniation treated with TLIF were investigated. Most patients were satisfied with the results of discectomy and fusion surgery, and would undergo surgery again. However, there are still 96 patients (15.4%) who are dissatisfied, and there is sufficient evidence to suggest that we should identify preoperative and postoperative factors that affect patients' level of satisfaction, in order to maximize the therapeutic benefits for patients. This study shows that obesity, preoperative pain lasting more than three months, feel depression and recurrence of symptoms are four independent factors affecting patients' dissatisfaction. While postoperative rehabilitation training for three months is a protective factor. Therefore, in the treatment of lumbar disc herniation with TLIF, it is important to pay close attention to these factors to improve the recovery effect.
This study shows that obesity is considered to be an independent factor for dissatisfaction in patients undergoing TLIF surgery. Obesity is often a negative factor for patients after surgery, which may be related to the following two aspects. First of all, compared with normal weight controls, obese patients experience an increase in intervertebral disc pressure during most daily activities, leading to accelerated intervertebral disc degeneration (15, 16), and studies have shown than obesity is associated with adjacent segment degeneration after lumbar fusion for degenerative lumbar disease (17). The degeneration of adjacent segments will lead to a series of new problems, such as symptom recurrence (18), thereby reducing the psychological expectations of obese patients. Moreover, obesity frequently hampers the overall activity levels of postoperative patients, leading to decreased mobility and potentially diminishing the surgical outcome. However, obesity should not be considered a contraindication for patients undergoing surgery, and for the improvement of back pain in patients, obesity is comparable to non-obese patients. Therefore, preoperative conversations with obese patients are necessary.
Previous studies have not provided sufficient evidence to demonstrate the relationship between duration of preoperative symptoms and postoperative satisfaction for patients undergoing TLIF surgery. In this study, we found that preoperative symptom duration lasting no less than six months was an independent risk factor for postoperative dissatisfaction. As the preoperative symptom duration increased, the patient 's dissatisfaction increased. On the one hand, the longer duration of preoperative symptoms is related to the longer duration of nerve root compression, which may lead to irreversible damage to the nerve root (19). On the other hand, after the first symptoms appear, patients usually choose conservative treatment. In China, most patients consider the cost issue and surgery is usually considered as the last option for treatment, with high expectations. However, after undergoing surgical treatment, some patients did not achieve the expected surgical outcome. It is still uncertain whether a preoperative symptom duration of 6 months can be used as a standard timeline for surgical efficacy. Previous studies have shown that patients with preoperative symptom duration less than three months achieved better results one year after surgery, and predicted that the rate of re-operation increased with the prolongation of preoperative symptom duration (20). Other studies have also reported that patients with preoperative symptoms lasting longer than one year had adverse outcomes, whether it was in the early or middle and late postoperative period (21). Patients who undergo early surgery are more likely to benefit more than patients with prolonged symptoms.
The ZSRDS is a 20-item questionnaire with well-established reliability and validity (22). Postoperative depression measured by the ZSRDS is another factor of dissatisfaction after TLIF. The association between preoperative depression and postoperative outcomes was demonstrated in previous studies, that is, preoperative depression reduces patients' level of satisfaction (23, 24). However, we found that postoperative depression also affects patients' level of satisfaction in this study. On the one hand, compared to preoperative depression, which is influenced by prolonged pain and high surgical costs, postoperative depression largely depends on the effectiveness of the surgery, indirectly reflecting the impact of psychological states such as feeling depressed on postoperative satisfaction. On the other hand, patients with depression may be more sensitive to postoperative pain, which may further reduce postoperative satisfaction (25). For patients undergoing TLIF, changes in postoperative depression have a more significant impact on satisfaction than preoperative depression (25). It is necessary to understand the expectations of these patients and fully provide them with emotional support and physical therapy to improve their overall satisfaction. Therefore, it is necessary to conduct preoperative visits by anesthesiologists and strengthening preoperative education, anxiety and depression can be detected early and intervened in a timely manner, which can reduce postoperative pain and cognitive dysfunction. The clinical doctors should inform patients of the surgical effect to avoid unrealistic expectations and alleviate surgical anxiety. Postoperative appropriate medication should be used to stabilize the patient's emotions and eliminate adverse reactions such as tension, fear, and anxiety caused by various surgeries. During postoperative follow-up, appropriate communication should be given to the patient. If symptoms are found, a psychologist should be consulted and medication should be used for treatment.
Another factor that affects postoperative dissatisfaction of patients is symptom recurrence, which often requires secondary surgery, which brings additional physical and psychological trauma to patients. It is reported that the incidence of recurrent lumbar disc herniation is 5%–15% (26, 27). This study showed that 84 (13.4%) of the 625 patients who received TLIF for lumbar disc herniation symptom recurrence. Among these recurrent patients, the majority were not satisfied with the results two years after surgery, while 9 patients (10.7%) still showed their satisfaction. We found that among the 9 patients who were satisfied, two patients had obvious obesity, five patients had long preoperative pain, and two patients had high preoperative VAS-back. Although the symptoms recurred after surgery, the pain was still relieved. The above patients were satisfied with the preoperative full communication and underwent secondary surgery. Unfortunately, this study did not conduct further follow-up. The recurrence of symptoms in patients treated with TLIF for lumbar disc herniation can occur either on the opposite side of the initial treatment site or in adjacent segments. Symptoms recurrence is the most common cause of unsatisfactory surgical treatment in patients with lumbar disc herniation (26, 28). Good preoperative communication can enable patients to fully understand the evolution of the disease, reduce the fear of the disease, and increase the level of postoperative satisfaction.
Postoperative rehabilitation exercise is the last factor affecting patient satisfaction in this study. Rehabilitation exercise is a protective factor, and patients who undergo rehabilitation exercise after surgery are more likely to achieve satisfactory surgical results. Postoperative rehabilitation training can effectively relieve pain and improve quality of life, and early rehabilitation training could enhance results in terms of pain and disability without an enhanced risk of complications (29, 30). However, in practical clinical work, rehabilitation exercise is often overlooked, even though both clinical doctors and patients know the effectiveness of rehabilitation exercise. In this study, we will inform patients in detail about the importance of postoperative rehabilitation exercise after surgery, but only 43.36% (271/625) patients persisted in exercising every day until 3 months after surgery. The effect of rehabilitation exercise is slow and firm (31), and rehabilitation training can improve muscle and tissue tolerance, avoiding slow recovery caused by muscle atrophy (29). Therefore, postoperative functional exercise is needed to strengthen the waist muscles, alleviate patient pain, and improve patient satisfaction.
There are several limitations in our research. Firstly, satisfaction is the subjective reaction of patients to clinical results, which is related with many variables and may result in selection bias. Secondly, this study is a retrospective single center study, which is still a valuable research method despite limitations such as limited the ability to establish causal relationships, recall bias, and limited generalizability of results. This article can provide clues and hypotheses for future research through reasonable design and rigorous analysis. Meanwhile, future research should consider conducting a multicenter prospective study with a larger sample size to validate our results. Finally, considering that precise osseointegration of the vertebral body and ideal recovery period of neurological function can be achieved 2 years after surgery, which can lead an accurate result. Therefore, this study only recorded detailed data of patients 2 years after surgery, and due to the limitations of retrospective analysis, detailed data of patients who underwent secondary surgery 3 months, 6 months, 1 year, and 2 years after surgery were not recorded in a timely manner.
ConclusionThis study indicates that 84.6% of patients are satisfied with TLIF treatment for lumbar disc herniation, but there are still some patients who are dissatisfied. And obesity, preoperative pain duration lasting no less than 6 months, feel depression and symptom recurrence are connected with postoperative patients' dissatisfaction. While postoperative rehabilitation training for three months is a protective factor. Adequate preoperative and postoperative communication is necessary for patients with these risk factors.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statementEthical approval was provided by the ethics committees of the Third Affiliated Hospital of Hebei Medical University Ethics Committee and obtained the unique identification number of research registration (the research registration number is 20241111). Each patient signed a written informed consent form.
Author contributionsLY: Data curation, Formal Analysis, Software, Validation, Writing – original draft. ZG: Data curation, Formal Analysis, Writing – original draft. YQ: Data curation, Formal Analysis, Writing – review & editing. JG: Formal Analysis, Writing – review & editing, Data curation. JL: Data curation, Formal Analysis, Writing – review & editing. WW: Conceptualization, Formal Analysis, Supervision, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was sponsored by Grants from Natural Science Foundation of Hebei Province (H2021206139).
AcknowledgmentsOur tribute also goes to Ruixue Diao, an English teacher in Hebei Medical University, for her help in carefully editing the grammar, spelling and punctuation of our manuscript.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References2. Zhao YF, Tian BW, Ma QS, Zhang M. Evaluation of the efficacy and safety of percutaneous transforaminal endoscopic discectomy for multi-segmental lumbar disc herniation. Pak J Med Sci. (2023) 39(6):1626–30. doi: 10.12669/pjms.39.6.3399
PubMed Abstract | Crossref Full Text | Google Scholar
3. Choi KC, Kim JS, Park CK. Percutaneous endoscopic lumbar discectomy as an alternative to open lumbar microdiscectomy for large lumbar disc herniation. Pain Physician. (2016) 19(2):E291–300. doi: 10.36076/ppj/2016.19.E291
PubMed Abstract | Crossref Full Text | Google Scholar
4. Ruan W, Feng F, Liu Z, Xie J, Cai L, Ping A. Comparison of percutaneous endoscopic lumbar discectomy versus open lumbar microdiscectomy for lumbar disc herniation: a meta-analysis. Int J Surg. (2016) 31:86–92. doi: 10.1016/j.ijsu.2016.05.061
PubMed Abstract | Crossref Full Text | Google Scholar
5. Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. (2003) 85(1):102–8. doi: 10.2106/00004623-200301000-00016
PubMed Abstract | Crossref Full Text | Google Scholar
6. Ozer AF, Keskin F, Oktenoglu T, Suzer T, Ataker Y, Gomleksiz C, et al. A novel approach to the surgical treatment of lumbar disc herniations: indications of simple discectomy and posterior transpedicular dynamic stabilization based on carragee classification. Adv Orthop. (2013) 2013:270565. doi: 10.1155/2013/270565
PubMed Abstract | Crossref Full Text | Google Scholar
7. Akeda K, Hasegawa T, Togo Y, Watanabe K, Kawaguchi K, Yamada J, et al. Quantitative analysis of lumbar disc bulging in patients with lumbar spinal stenosis: implication for surgical outcomes of decompression surgery. J Clin Med. (2023) 12(19):6172. doi: 10.3390/jcm12196172
PubMed Abstract | Crossref Full Text | Google Scholar
8. Awadalla AM, Aljulayfi AS, Alrowaili AR, Souror H, Alowid F, Mahdi AMM, et al. Management of lumbar disc herniation: a systematic review. Cureus. (2023) 15(10):e47908. doi: 10.7759/cureus.47908
PubMed Abstract | Crossref Full Text | Google Scholar
9. Loubeyre J, Ferrero E, Jmal MM, Guigui P, Khalifé M. Surgical treatment of degenerative lumbar spondylolisthesis: effect of TLIF and slip reduction on sagittal alignment. Orthop Traumatol Surg Res. (2023) 109(6):103541. doi: 10.1016/j.otsr.2022.103541
PubMed Abstract | Crossref Full Text | Google Scholar
10. Slosar PJ, Reynolds JB, Schofferman J, Goldthwaite N, White AH, Keaney D. Patient satisfaction after circumferential lumbar fusion. Spine. (2000) 25(6):722–6. doi: 10.1097/00007632-200003150-00012
PubMed Abstract | Crossref Full Text | Google Scholar
11. Barco S, Corti M, Trinchero A, Picchi C, Ambaglio C, Konstantinides SV, et al. Survival and recurrent venous thromboembolism in patients with first proximal or isolated distal deep vein thrombosis and no pulmonary embolism. J Thromb Haemostasis. (2017) 15(7):1436–42. doi: 10.1111/jth.13713
PubMed Abstract | Crossref Full Text | Google Scholar
15. Wang F, Chen K, Lin Q, Ma Y, Huang H, Wang C, et al. Earlier or heavier spinal loading is more likely to lead to recurrent lumbar disc herniation after percutaneous endoscopic lumbar discectomy. J Orthop Surg Res. (2022) 17(1):356. doi: 10.1186/s13018-022-03242-x
PubMed Abstract | Crossref Full Text | Google Scholar
16. Ren G, Liu L, Zhang P, Xie Z, Wang P, Zhang W, et al. Machine learning predicts recurrent lumbar disc herniation following percutaneous endoscopic lumbar discectomy. Global Spine J. (2024) 14(1):146–52. doi: 10.1177/21925682221097650
PubMed Abstract | Crossref Full Text | Google Scholar
17. Wang T, Ding W. Risk factors for adjacent segment degeneration after posterior lumbar fusion surgery in treatment for degenerative lumbar disorders: a meta-analysis. J Orthop Surg Res. (2020) 15(1):582. doi: 10.1186/s13018-020-02032-7
PubMed Abstract | Crossref Full Text | Google Scholar
18. Staszkiewicz R, Ulasavets U, Dobosz P, Drewniak S, Niewiadomska E, Grabarek BO. Assessment of quality of life, pain level and disability outcomes after lumbar discectomy. Sci Rep. (2023) 13(1):6009. doi: 10.1038/s41598-023-33267-z
PubMed Abstract | Crossref Full Text | Google Scholar
19. Wu W, Liang J, Ru N, Zhou C, Chen J, Wu Y, et al. Microstructural changes in compressed nerve roots are consistent with clinical symptoms and symptom duration in patients with lumbar disc herniation. Spine. (2016) 41(11):E661–6. doi: 10.1097/BRS.0000000000001354
PubMed Abstract | Crossref Full Text | Google Scholar
20. Støttrup CC, Andresen AK, Carreon L, Andersen MØ. Increasing reoperation rates and inferior outcome with prolonged symptom duration in lumbar disc herniation surgery—a prospective cohort study. Spine J. (2019) 19(9):1463–9. doi: 10.1016/j.spinee.2019.04.001
Crossref Full Text | Google Scholar
21. Wu H, Hu S, Liu J, He D, Chen Q, Cheng X. Risk factors involved in the early and Medium-term poor outcomes of percutaneous endoscopic transforaminal discectomy: a single-center experience. J Pain Res. (2022) 15:2927–38. doi: 10.2147/JPR.S380946
PubMed Abstract | Crossref Full Text | Google Scholar
22. Thurber S, Snow M, Honts CR. The zung self-rating depression scale: convergent validity and diagnostic discrimination. Assessment. (2002) 9(4):401–5. doi: 10.1177/1073191102238471
PubMed Abstract | Crossref Full Text | Google Scholar
23. Levin JM, Winkelman RD, Smith GA, Tanenbaum JE, Benzel EC, Mroz TE, et al. Impact of preoperative depression on hospital consumer assessment of healthcare providers and systems survey results in a lumbar fusion population. Spine. (2017) 42(9):675–81. doi: 10.1097/BRS.0000000000002101
PubMed Abstract | Crossref Full Text | Google Scholar
24. Wang SK, Mu H, Wang P, Li XY, Kong C, Cheng JB, et al. The charlson comorbidity Index and depression are associated with satisfaction after short-segment lumbar fusion in patients 75 years and older. Front Surg. (2022) 9:991271. doi: 10.3389/fsurg.2022.991271
PubMed Abstract | Crossref Full Text | Google Scholar
25. Rahman R, Ibaseta A, Reidler JS, Andrade NS, Skolasky RL, Riley LH, et al. Changes in patients’ depression and anxiety associated with changes in patient-reported outcomes after spine surgery. J Neurosurg Spine. (2020) 32(6):871–90. doi: 10.3171/2019.11.SPINE19586
PubMed Abstract | Crossref Full Text | Google Scholar
26. Aizawa T, Ozawa H, Kusakabe T, Nakamura T, Sekiguchi A, Takahashi A, et al. Reoperation for recurrent lumbar disc herniation: a study over a 20-year period in a Japanese population. J Orthop Sci. (2012) 17(2):107–13. doi: 10.1007/s00776-011-0184-6
PubMed Abstract | Crossref Full Text | Google Scholar
27. Li Z, Yang H, Liu M, Lu M, Chu J, Hou S, et al. Clinical characteristics and risk factors of recurrent lumbar disk herniation: a retrospective analysis of three hundred twenty-one cases. Spine. (2018) 43(21):1463–9. doi: 10.1097/BRS.0000000000002655
PubMed Abstract | Crossref Full Text | Google Scholar
28. Miwa S, Yokogawa A, Kobayashi T, Nishimura T, Igarashi K, Inatani H, et al. Risk factors of recurrent lumbar disk herniation: a single center study and review of the literature. J Spinal Disord Tech. (2015) 28(5):E265–9. doi: 10.1097/BSD.0b013e31828215b3
PubMed Abstract | Crossref Full Text | Google Scholar
29. Zhu Y, Xia S, Yang W, Shi F, Ji H. Early efficacy of postoperative rehabilitation training for lumbar disc herniation. BMC Sports Sci Med Rehabil. (2023) 15(1):97. doi: 10.1186/s13102-023-00704-5
PubMed Abstract | Crossref Full Text | Google Scholar
30. Ruffilli A, Manzetti M, Cargeli A, Viroli G, Ialuna M, Traversari M, et al. Unveiling timetable for physical therapy after single-level lumbar surgery for degenerative disc disease: insights from a systematic review and meta-analysis. J Clin Med. (2024) 13(9):2553. doi: 10.3390/jcm13092553
PubMed Abstract | Crossref Full Text | Google Scholar
31. Atsidakou N, Matsi AE, Christakou A. The effectiveness of exercise program after lumbar discectomy surgery. J Clin Orthop Trauma. (2021) 16:99–105. doi: 10.1016/j.jcot.2020.12.030
留言 (0)