The vestibular nerve transmits self-motion and orientation information from the vestibular end organs (the semicircular canals, saccule, and utricle) to the brainstem, cerebellum, and cerebral cortices. This transmission is crucial for oculomotor and postural control, as well as spatial orientation. Additionally, branches of the vestibular nerve project to the mastoid region behind the ear. It is possible to stimulate the vestibular system by applying a low-intensity electric current to the vestibular nerve. This is typically accomplished by placing electrodes on the mastoids and delivering transcutaneous current to local vestibular afferents. This noninvasive form of stimulation is known as Galvanic Vestibular Stimulation (GVS), named after Luigi Galvani who used electric current to evoke frog muscle contractions (Galvani, 1953; Dlugaiczyk et al., 2019). It has been used for its various diagnostic and therapeutic capabilities as well as to investigate vestibular physiology. For example, it can induce a complex whole-body response of oculomotor and balance reflexes, which vary greatly depending on the waveform and other stimulation parameters.
While much of the research on GVS in humans has been restricted to non-invasive methods due to ethical and practical considerations, substantial invasive studies on animals have provided deeper insights into the mechanistic effects of GVS. Johann Purkinje first noted in 1820 that passing electric current through the human head led to balance and equilibrium disturbances (Purkinje, 1820). Later, Josef Breuer attributed these effects to the galvanic stimulation of the vestibular system, observing distinct head movements resulting from the stimulation of individual semicircular canals (SCCs) in birds (Breuer, 1874). Many years later, Chapman et al. (2019) applied targeted GVS to rat SCC nerves and found higher concentrations of c-Fos protein in the contralateral medial vestibular nucleus. These findings by Breuer and Chapman et al. suggest that GVS stimulates the SCC rather than the otoliths. On the other hand, Holstein et al. (2012) applied low-frequency sinusoidal GVS (0.02–0.04 Hz) to rats and found c-Fos protein in the nuclei of otolith-driven neurons, indicating that GVS serves as an otolithic stimulus. To resolve this inconsistency, Kwan et al. (2019) conducted a study in which they inserted recording electrodes into the vestibular nerves of rhesus macaques to measure the activity of individual afferents. Their findings demonstrated that both otolith and SCC afferents are activated by sinusoidal GVS. These results suggest that GVS does not replicate natural head motion as closely as may have been previously assumed, as regular head rotations typically do not stimulate both otoliths and SCC simultaneously.
Nguyen et al. (2021) investigated the effects of GVS on mice following unilateral labyrinthectomy. They found that 1 Hz sinusoidal GVS at 0.1 mA accelerated the recovery of spatial memory and locomotor function in these mice, indicating a potential therapeutic benefit of GVS in vestibular dysfunction. In another study, Sabzevar et al. (2023) applied GVS to rats in direct current (DC) pulses at the minimum intensity that induced eye movement and discovered electrophysiological signals in the tail of the striatum, a recently discovered sensory region, suggesting that vestibular projections also extend into this area. These studies highlight the potential of GVS to influence not only vestibular functions, but also broader neural circuits involved in spatial memory and sensory processing.
The complexity of vestibular signaling and the effects of GVS contribute to significant variability in observed outcomes, which depend on factors such as waveform, anatomical location of stimulation, and other selected parameters.
The mechanisms of suprathreshold and subthreshold are presumably different. Suprathreshold GVS, delivered in either DC or sine waveform, modulates the firing rates of vestibular afferent neurons in a manner that is directly proportional to the applied current, as demonstrated in neural recordings from non-human primates (Kwan et al., 2019; Forbes et al., 2023). This neural activation is subsequently transmitted to the vestibular nuclei in the brainstem, where it mediates a complex whole-body response involving balance reflexes. These reflexes are influenced by various factors, including the head and body’s orientation and position, the specific task being performed, and the sensory input received from other sensory modalities (Fitzpatrick and Day, 2004). In response to this perception, oculomotor and postural responses are triggered directed toward the anodal current (Fitzpatrick and Day, 2004).
Conversely, subthreshold GVS when delivered as a noisy waveform (nGVS) is thought to act by inciting stochastic resonance, increasing the discharge and resting state activity of vestibular afferents, thereby improving neural activation “information transfer” even at intensities that do not cause gross motor activity (Wuehr et al., 2016b). Behavioral responses have been observed that are consistent with this hypothesized mechanism, such as reduced vestibular perceptual thresholds with moderate amplitudes of nGVS (Galvan-Garza et al., 2018), and improvements in balance in both healthy (e.g., Keywan et al., 2018) and diseased populations (e.g., Fujimoto et al., 2018). However, to our knowledge, no studies have quantified vestibular afferent neuron firing rates during nGVS application in non-human primates, as has been done with suprathreshold DC or sine GVS (Kwan et al., 2019; Forbes et al., 2023).
Electrode positioning strongly impacts the induced current flow pattern and electric field at the vestibular organs of interest (Thomas et al., 2020; Truong et al., 2024). This consideration is critical as current flow is believed to modulate the firing rate of vestibular hair cells that is ultimately relayed to the vestibular nuclei in the brainstem (Wardman and Fitzpatrick, 2002). Functional MRI has revealed that bilateral GVS stimulates the temporoparietal junction, central sulcus, anterior interior intraparietal sulcus, and premotor regions of the frontal lobe (Lobel et al., 1999).
Consequently, it is crucial to establish stimulation parameters tailored to the desired application to ensure accuracy and reproducibility. To identify the optimal waveform parameters, we conducted a systematic review of clinical trials on GVS according to the PRISMA guidelines (Page et al., 2021) and extracted stimulation parameters relevant to each application. While GVS is employed both as a diagnostic tool (Dlugaiczyk et al., 2019) and as a method to enhance or modulate balance in healthy individuals (e.g., Wuehr et al., 2016a; Brunyé et al., 2024), this review specifically concentrates on its therapeutic applications. Additionally, although other forms of vestibular stimulation, such as thermal (e.g., caloric) and invasive techniques, are worthy of consideration, our focus is on conventional, non-invasive GVS.
2 MethodsWe conducted a literature search of the PubMed and Embase databases for clinical trials with the keyword “galvanic vestibular stimulation” up to July 1, 2024. We included research articles, letters, and case studies, but excluded literature reviews and abstracts. A research team member screened each result and removed duplicates, studies that used GVS solely for diagnostic or screening purposes, and studies that applied GVS simply to enhance functions in healthy subjects rather than to treat a specific symptom or disorder. We segmented the remaining results into three groups: (1) GVS for treating impaired postural control, (2) GVS for post-stroke patients, and (3) GVS for other clinical applications. We extracted the stimulation parameters of each study as well as the study design and number of diseased patients in each arm. We only report that a study was double-blind when the authors mention that the investigators were blinded to the treatment conditions. Otherwise, we assume that blinded studies were only single-blind.
The stimulation parameters included electrode montage, waveform, frequency, intensity, sham procedure, stimulation length, number of sessions, and inter-session interval as follows:
2.1 Electrode montageElectrode montage describes the anatomical positions of the electrodes as well as the polarity pattern of the electrodes. Most commonly, GVS is delivered through one electrode on each mastoid, a montage known as “bilateral-bipolar” (Figure 1A). Some studies have examined alternative electrode montages or additional electrodes at locations such as the forehead or temples (e.g., Cevette et al., 2012; Aoyama et al., 2017; Figures 1B,C).
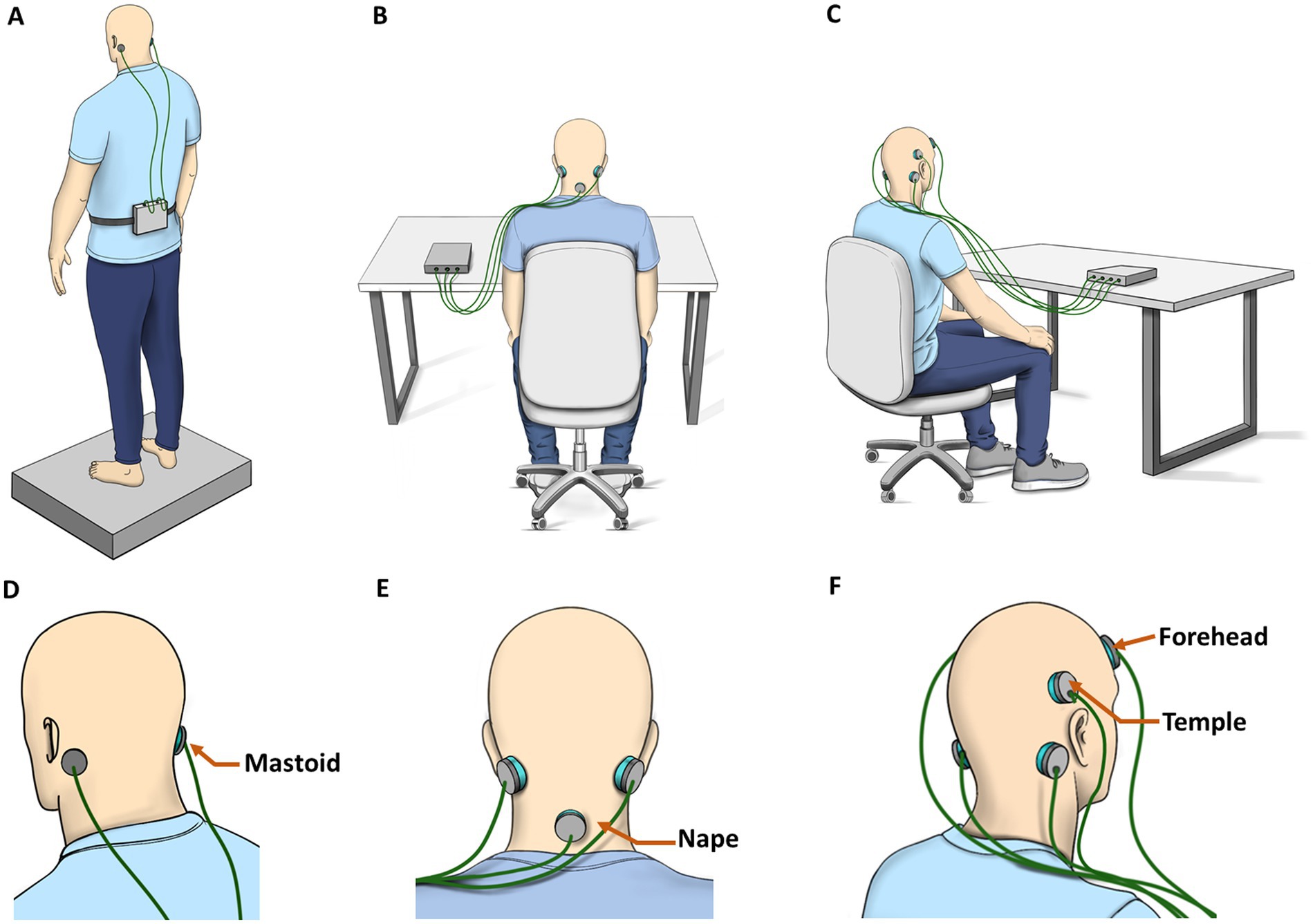
Figure 1. GVS administration and electrode montage. (A) Bilateral-Bipolar is the most common. It is often delivered while the subject stands on a force plate. (B,C) Multichannel setups are tested more frequently for motion sickness and cybersickness applications by placing additional electrodes on the back of the neck, temples, or forehead. (D–F) Corresponding expanded images indicating electrode locations tested in the literature.
2.2 WaveformWaveform is the shape of the electric current function. It is independent of amplitude or time. Different waveforms of GVS have different physiological effects and are therefore used for different applications. The most commonly used GVS waveforms are DC, sinusoidal, and stochastic noisy white noise. Figure 2 presents visual representations of these parameters as simplified electrical waveforms.
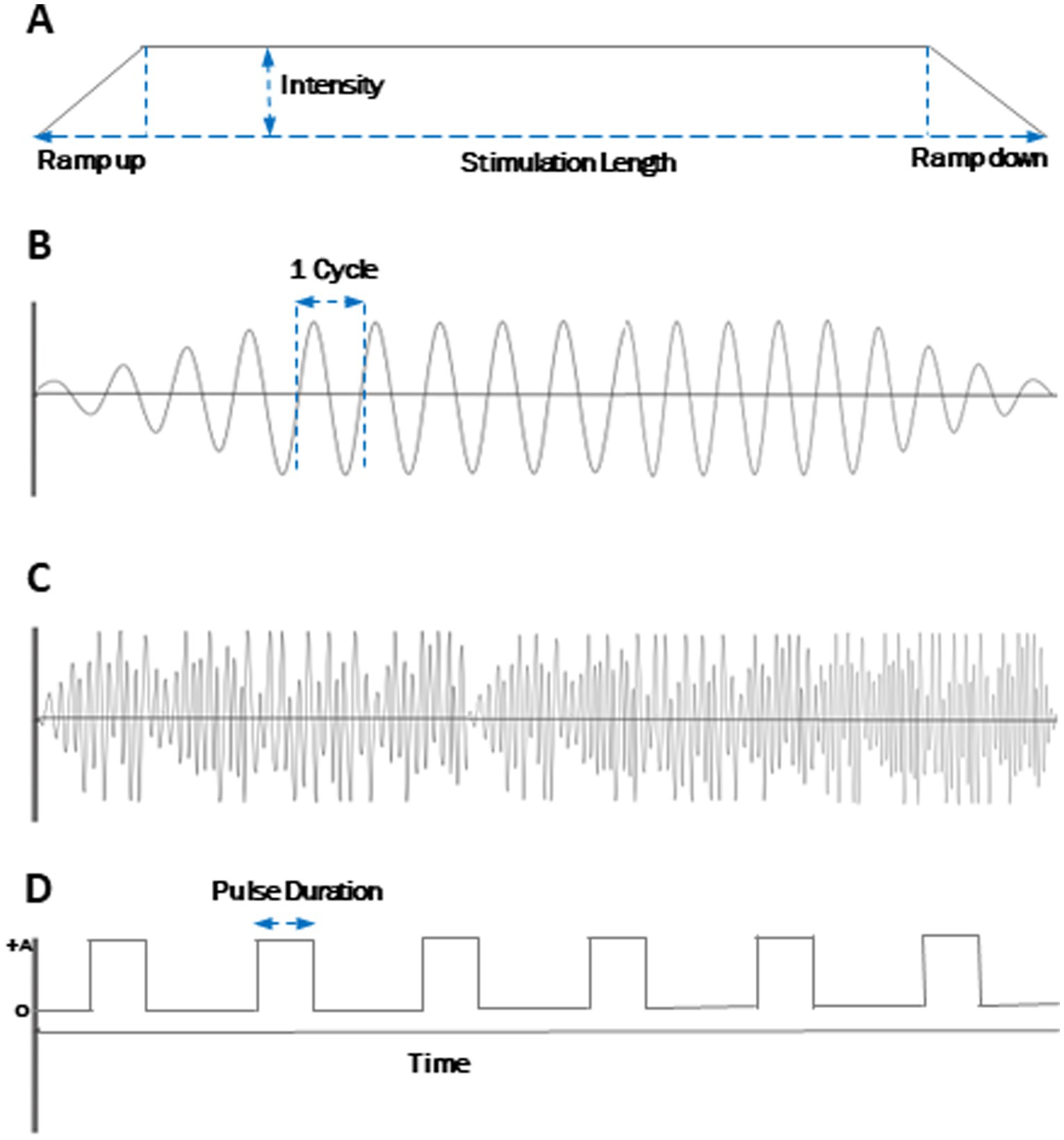
Figure 2. Electrical waveform parameters for GVS. (A) Direct Current (DC). (B) Sinusoidal. (C) Noisy. (D) DC pulses. Frequency is the number of cycles per second. Stimulation is generally ramped up and ramped down at the beginning and the end of the session to prevent cutaneous discomfort. An exemplary noise waveform is shown here and does not specifically differentiate from different implementations (white noise, random noise, etc.) Similarly, the DC pulse shown is exemplary and may or may not be offset from the 0 line.
2.2.1 Direct currentDepending on the polarity and intensity, DC causes an immediate and sustained change in the firing rate of the neurons (Bindman et al., 1964). Sometimes, GVS in a DC waveform is applied as a train of short pulses. When this is the case, we mention the time duration of each pulse (i.e., pulse width), if reported by the authors. Figure 2D illustrates DC pulses and the definition of pulse duration.
2.2.2 SinusoidalSinusoidal GVS induces sensations and vestibulo-ocular reflexes that resemble those elicited by head rotations (Kim et al., 2011; Gensberger et al., 2016). However, GVS does not perfectly replicate natural head movements, as it likely stimulates both the SCC and the otolith organs (Kwan et al., 2019), whereas natural head motion typically does not. In rare instances, a combination of sine waves of different frequencies are combined into a single stimulation waveform, known as multisine (Kazemi et al., 2021; Lee et al., 2021a; Liu et al., 2021).
2.2.3 NoisyProducing stochastic resonance by applying band-limited nGVS is assumed to reduce the firing threshold of vestibular irregular afferent neurons boosting weak physiological signals from the vestibular apparatus (Nooristani et al., 2021; Eder et al., 2022; Wuehr et al., 2023).
2.3 FrequencyFrequency is a measure of the rate of oscillatory fluctuations of a waveform. While DC frequency is zero, sinusoidal current is typically applied at a specified frequency (i.e., the sine wave frequency) and nGVS is typically delivered within a defined frequency spectrum that encompasses all frequencies within the specified range (e.g., a bandwidth of 0.01 to 2.0 Hz). The electric current delivered varies across frequencies within this range.
2.4 IntensityCurrent intensity is a measure of the amplitude, or strength, of the electric current. Given the weak nature of current applied in GVS, this is typically reported in milliampere (mA) units. While some studies have used a fixed intensity across all subjects, individualized current intensity (determined pre-trial) is also used. Sometimes, this was done to ensure that the current intensity was below the subject’s sensory threshold (either cutaneous or vestibular) so as not to compromise subject blinding. In other studies, it was done to determine the highest or most optimal current level based on previous literature without surpassing limits of safety and tolerability. We also report the mean and standard deviation of the threshold when provided by the paper. For sine and noisy waveforms where the intensity fluctuates, we report the maximum intensity.
2.5 ShamSome studies compare the effects of real GVS to sham (i.e., placebo) stimulation. We report whether studies used a sham comparison and how it was implemented.
2.6 Stimulation lengthStimulation length is the duration that stimulation is delivered during a single session. A longer stimulation length is generally believed to have a greater effect. We note that some studies only report that stimulation was delivered throughout the duration of a task, but do not report the time duration of the task. In these cases, we report that stimulation length was not specified.
2.7 Number of sessionsThe number of sessions is the total number of stimulation sessions delivered. The importance of the number of sessions is that it considers the effect of cumulative dosage (Thompson et al., 2021).
2.8 Inter-session intervalInter-session interval is the time duration between stimulation sessions. Sometimes stimulation was delivered while subjects performed tasks where there was a break between each task to avoid potential after-effects. In may be unclear how long the breaks were between stimulations. It then becomes important for the reader to carefully track the full methodology to retrieve the exact timing. In studies that involved multiple successive trials, some of the trials could have active stimulation while others were shams. As a result, inter-session interval is sometimes not straightforward to comprehend and could imply the time duration between trains of stimulation pulses or the interval between a group of trials. When the session is repeated multiple times in a day (e.g., Fujimoto et al., 2016), this ambiguity may lead to further confusion. In this study, we sought to make this distinction clear as well as the specified number of hours and/or days between stimulation sessions. In summary, besides the ambiguity in interpreting length of stimulation session and inter-session intervals in some studies, other parameters are reported in precise terms. The parameters we listed above serve as a basis to systematically compare across the studies included in this review.
3 ResultsOur search returned a total of 239 results. We then removed 92 duplicates, 88 articles that did not meet the inclusion criteria, and 2 papers that were not available (Figure 3). Among the remaining 57 publications, four of them were secondary analyses of other studies. This left us with 53 independent studies discussed below.
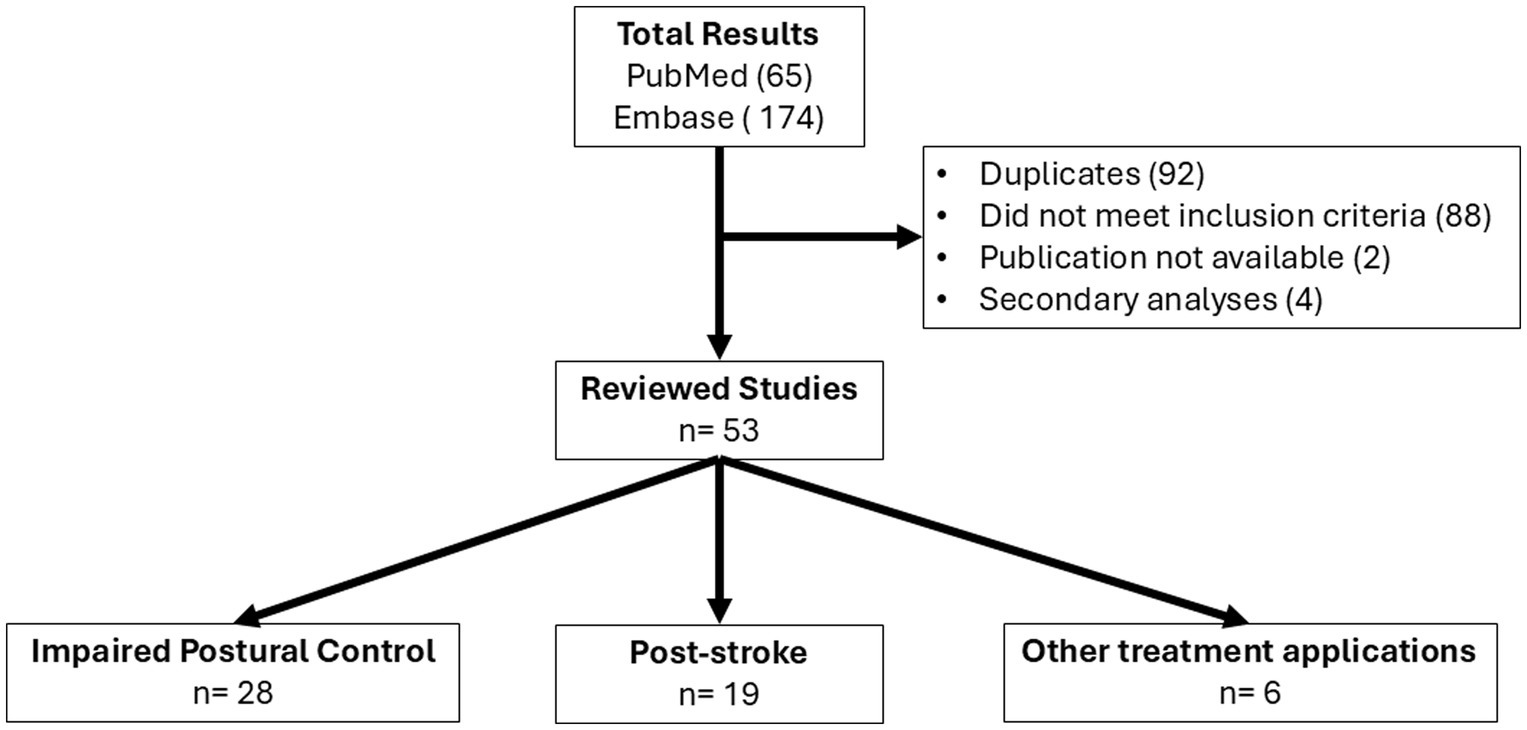
Figure 3. Flow of study selection procedure.
3.1 GVS for impaired postural controlImpaired upright postural control often arises from disruptions in the sensory information that governs motor skills, as well as the body’s awareness of its position in relation to its surroundings and spatial orientation. Such disturbances can be attributed to disorders of the vestibular system, which may result from factors such as head injury, viral infections, and various genetic and environmental influences. Common symptoms of vestibular system pathology include loss of balance, vertigo, dizziness, blurred vision, nausea, lack of coordination, vomiting, unsteady gait, and muscle aches (Thompson and Amedee, 2009; Pérez-Fernández and Ramos-Macías, 2023).
In addition to these factors, aging contributes to progressive functional decline that increasingly compromises balance. The natural loss of muscle mass (sarcopenia), along with neurological and psychiatric disorders, vestibular impairments, certain medications, and cardiovascular disease, can exacerbate balance deficits among older adults. These balance disorders represent a significant risk factor for falls, which are a major public health concern, as they account for the leading cause of accidental death in individuals over the age of 60 (Gaspar and Lapão, 2021).
Impaired postural control can also be the result of neurodegenerative disorders such as Parkinson’s Disease (PD), an incurable chronic neurological disorder characterized by the degeneration of nerve cells in the substantia nigra. Symptoms of PD include postural imbalance, tremors, rigidity, bradykinesia (slowness of movement), and stiffness of limbs (Hodgson et al., 2021).
The peripheral vestibular system, along with its associated brain regions, plays a critical role in the collection and integration of vestibular signals. Consequently, modulation of the vestibular system presents a promising approach for addressing postural control deficits in humans. GVS is particularly advantageous due to its minimal and transient side effects, making it suitable for repetitive treatments and compatible with concurrent tasks, such as rehabilitation therapy (Volkening et al., 2016). Moreover, recent studies have revealed that GVS delivered in a noisy waveform can induce neurochemical changes in key regions, including the substantia nigra and the parvocellular medial vestibular nucleus, both of which are implicated in PD (Lee et al., 2021b). This suggests that GVS may not only aid in improving postural control but also influence underlying neurophysiological mechanisms related to PD.
Various stimulation parameters of GVS have been used to improve impaired postural control in persons with vestibular disorders, elderly adults, and in patients with neurodegenerative disorders. We present parameters of each study in Table 1. Table 2 serves as a summary providing the most commonly utilized parameters across GVS studies for impaired postural control as well as the full range of parameters.
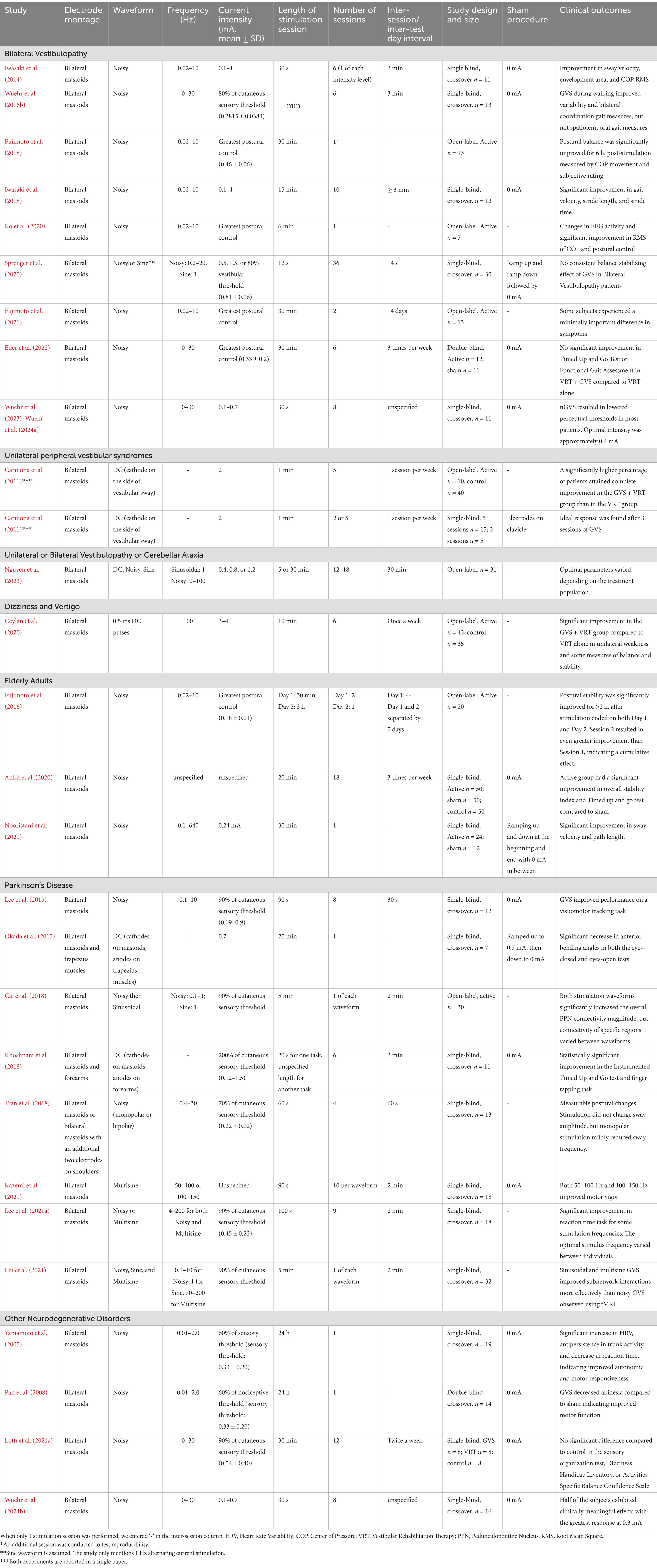
Table 1. GVS stimulation parameters for improving postural control in various populations and reported clinical outcomes.
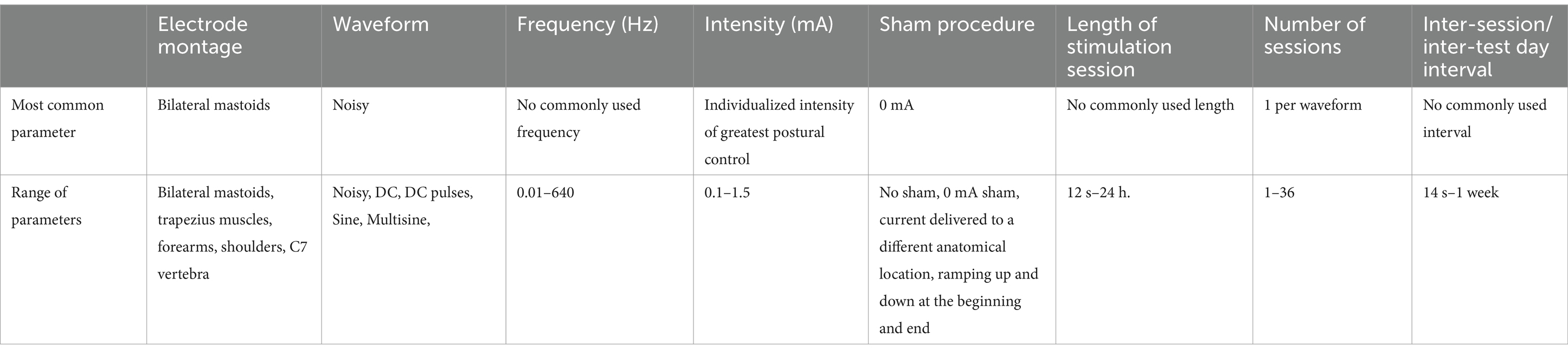
Table 2. Most common parameters and range of parameters used for improving postural control.
3.1.1 Electrode montage, waveform, and frequencyFor impaired postural control, the objective of GVS is to compensate for dysfunctional vestibular function by enhancing the sensory input to the vestibular system. This is typically achieved by delivering a noisy waveform to the vestibular afferents that project to the mastoid region. This stimulation lowers the neural firing threshold, thereby amplifying weak physiological signals. This method has been applied across various populations with impaired postural control, resulting in notable improvements in autonomic and motor functions in patients with neurodegenerative disorders (Yamamoto et al., 2005; Pan et al., 2008; Khoshnam et al., 2018; Lee et al., 2021a), as well as enhanced postural stability in elderly adults (Fujimoto et al., 2016; Nooristani et al., 2021) and individuals with bilateral vestibulopathy (Iwasaki et al., 2014; Fujimoto et al., 2018; Wuehr et al., 2016b; Iwasaki et al., 2018; Ko et al., 2020; Fujimoto et al., 2021). Notably, Fujimoto et al. (2016) reported that elderly participants experienced improved postural stability several hours after stimulation had ceased. The bilateral-bipolar montage was the predominant configuration used by the majority of studies evaluated in this review, indicating it as the preferred montage choice.
An alternative, less commonly used stimulation setup involves applying DC through two cathodal electrodes placed on the mastoids and two anodal electrodes positioned on the trapezius muscles (Okada et al., 2015) or forearms (Khoshnam et al., 2018). This electrode configuration allows for the stimulation of vestibular nerves on both sides simultaneously with anodal current, which is not feasible with bilateral-bipolar stimulation. Reports indicate that this method can improve anterior bending posture and other motor symptoms in patients with PD (Okada et al., 2015; Khoshnam et al., 2018).
When addressing peripheral vestibular syndromes, the aim shifts to stimulating the very sensory system that is known to be damaged. In cases where the peripheral disorder is unilateral, DC is delivered with the anodal electrode on the contralateral side of the impairment to counteract the patient’s mediolateral sway. Consequently, Carmona et al. (2011) applied DC stimulation in conjunction with vestibular rehabilitation therapy (VRT) to patients with unilateral peripheral vestibular syndromes, positioning the anodal electrode on the contralateral side of the impairment.
Frequency is not applicable for DC stimulation but is a major consideration in noisy GVS protocols. There is variability, however, with respect to the actual administration of the noisy waveforms, with spectral content varying from close to 0 Hz to low 10s or sometimes even up to 640 Hz. As discussed in a review by McLaren et al. (2023) the choices of different frequencies are supported by various rationales related to the physiology of vestibular organs or the central nervous system. Body sway typically occurs within a frequency range of 0.02–10 Hz (Assländer et al., 2021; Lajoie et al., 2021), whereas normal head motion during walking is found in the 0–2 Hz range (Hirasaki et al., 1999). Conversely, a frequency range of 0–30 Hz has been identified as effective for stimulating vestibular hair cells and is regarded as the natural frequency of the vestibular system (Mulavara et al., 2011; Goel et al., 2015; Mulavara et al., 2015; Dlugaiczyk et al., 2019). Alternatively, some studies have used a frequency range of 0 to 640 Hz, as this range has been shown to activate cortical neurons (Terney et al., 2008), suggesting its potential for effective GVS outcomes. Also, due to this ability to stimulate cortical activity, this frequency range is commonly employed in tES devices, which are widely utilized in GVS research. Therefore, in these instances, the choice of frequency band may simply be due to the available setting on the stimulator.
Given that most studies report beneficial outcomes, it may be inferred that precise tuning of frequency content is less critical than otherwise assumed. However, the broad frequency ranges often employed might result in suboptimal application, suggesting that effects could be further enhanced with more targeted and precise frequency settings.
3.1.2 Intensity and sham controlSome investigators have delivered stimulation just below the subject’s sensory threshold (Lee et al., 2021a; Liu et al., 2021; Lotfi et al., 2021a), to enable blinding for controlled studies. This way the subjects would not know whether they received active or sham stimulation. Other studies delivered stimulation at the subject’s optimal intensity to maximize stimulation benefit (Fujimoto et al., 2016; Fujimoto et al., 2018; Ko et al., 2020). For example, Fujimoto et al. (2016) used a dosage titration technique before each experimental session by measuring three parameters during various current intensities: the mean velocity, envelopment area, and the root mean square of the center of pressure (COP) movement in the XY plane. They identified the optimal intensity of noisy GVS as the intensity which improved all these parameters simultaneously during the stimulus compared with baseline. Notably though, Eder et al. (2022) performed the same optimization technique on the same population and combined the stimulation with vestibular rehabilitation therapy (VRT). Results showed no additional effects of GVS compared to patients who received VRT alone. The authors suggest that the lack of combined effect may be due to the difference in mechanisms as low intensity GVS affects sub-threshold vestibular cues, while the VRT protocol employed in the study focused on fast head kinematics. Conversely, the aforementioned study by Carmona et al. (2011) found that patients with unilateral peripheral vestibular syndromes undergoing VRT and GVS at 2 mA intensity were more likely to recover than subjects who received VRT alone. The difference in clinical outcomes between Carmona et al. and Eder et al. may suggest that a VRT-GVS synergy is present when suprathreshold intensity is used, as opposed to when subthreshold GVS is used. Alternatively, the difference in clinical outcomes between these two studies may have been due to differences in subject population (unilateral vs. bilateral vestibular pathology) or waveform (noisy vs. DC).
Other studies delivered stimulation uniformly to all subjects at a single intensity, such as 0.4 mA, (e.g., Inukai et al., 2018) or a range of intensities, such as 0.1–0.7 mA, to test the effects of GVS at different intensities (e.g., Wuehr et al., 2023). In studies that delivered supersensory stimulation, a topical anesthetic can be applied to minimize sensation so as to improve subject blinding (Sprenger et al., 2020).
While some GVS studies were open-label without a sham control, others used a study arm that received 0 mA throughout (e.g., Kazemi et al., 2021) or a brief stimulation period where current was delivered at the beginning of the session and then ramped down without informing the subject (Okada et al., 2015; Sprenger et al., 2020; Nooristani et al., 2021), a technique often used as sham in studies on transcranial electrical stimulation (tES). Studies focusing solely on dose optimization (e.g., Nguyen et al., 2023) were less likely to utilize a sham control, as the different doses themselves served as an internal control for comparison. We note the non-ideal sham strategy in Carmona et al., 2011, where they applied stimulation to the mastoids in the active arm and off-target (clavicle) in the sham arm. While the study may have assessed blinding efficacy, it was not reported. Similarly, Khoshnam et al., 2018 reported that the sham condition was administered as “GVS off.” Given active arm delivered stimulation above the cutaneous threshold, it is unclear how blinding efficacy was maintained.
3.1.3 Stimulation sessions: length, number, and intervalMost studies have primarily examined the effects of a single galvanic vestibular stimulation (GVS) session (Yamamoto et al., 2005; Pan et al., 2008; Okada et al., 2015) or a single session of each waveform (Iwasaki et al., 2014; Liu et al., 2021). A limited number of studies have explored the cumulative effects of multiple sessions, particularly in conjunction with VRT (Carmona et al., 2011; Ceylan et al., 2020).
The duration of GVS sessions varied considerably among studies, influenced by whether the aim was to assess the immediate effects of stimulation—wherein brief stimulation suffices for testing—or to evaluate the prolonged effects resulting from extended stimulation. For instance, Inukai et al. (2018) administered only 30 s of stimulation and measured improvements in postural control among elderly adults during the stimulation. In contrast, Ankit et al. (2020) implemented 20-min sessions for the same demographic and analyzed the effects of prolonged stimulation. Studies investigating extended stimulation typically limited the duration to 20 or 30 min, adhering to safety protocols established for transcranial direct current stimulation (tDCS; Woods et al., 2016; Bikson et al., 2016).
To prevent carryover effects between sessions to effectively assess each waveform independently, studies implemented intervals between different stimulation waveforms. The intervals varied significantly, with some studies using 2-min breaks (Cai et al., 2018; Liu et al., 2021; Lee et al., 2021a) and others opting for longer breaks such as a 30-min interval (Nguyen et al., 2023). When investigating cumulative effects through repeated doses, studies typically adopted regimens that included treatments administered once, twice, or three times per week (Carmona et al., 2011; Ankit et al., 2020; Ceylan et al., 2020; Lotfi et al., 2021a; Eder et al., 2022).
3.2 GVS for spatial orientation in stroke patientsRecent medical advancements have increased the percentage of stroke survivors. However, the survivors are left to cope with the psychological, functional, physical, and social effects of stroke. A common lasting effect of both ischemic and hemorrhagic stroke is an impairment in the ability to integrate visual, somatosensory, and vestibular information (Saeys et al., 2018; Barra et al., 2010; Utz et al., 2011a). This often results in a misperception of verticality as indicated by deviations in the patients’ subjective visual vertical (SVV; Utz et al., 2011b; Oppenländer et al., 2015a). The inability to integrate these channels also shifts the center of gravity towards the paretic side, impairing postural balance to the extent that sitting or standing can become impossible (Volkening et al., 2016), aside from postural difficulties arising from muscle weakness. Patients will also often actively push with the non-affected extremities towards the paretic side and exhibit resistance to passive correction, a condition called pusher behavior (Volkening et al., 2016). Difficulty in integrating various sensory channels post-stroke also often results in spatial neglect (Barra et al., 2010; Utz et al., 2011b), which is the impairment in detecting or responding to sensory stimuli in contralesional space (Heilman et al., 2000). Patients often show left-sided spatial neglect after damage to the right hemisphere (Volkening et al., 2016). When spatial neglect is present, a deviation of the egocentric reference frame towards ipsilesional space is experienced (Karnath, 1994; Vallar, 1997).
Through GVS activation of the vestibular cortex, the subjective vertical inclines to the anodal side, shifting the center of gravity to the anodal side as well (Oppenländer et al., 2015a). As such GVS has been investigated as a treatment mechanism for improving these symptoms in stroke patients. The parameters used are enumerated in Table 3. Table 4 serves as a summary providing the most commonly utilized parameters across GVS studies for post-stroke patients as well as the full range of parameters.
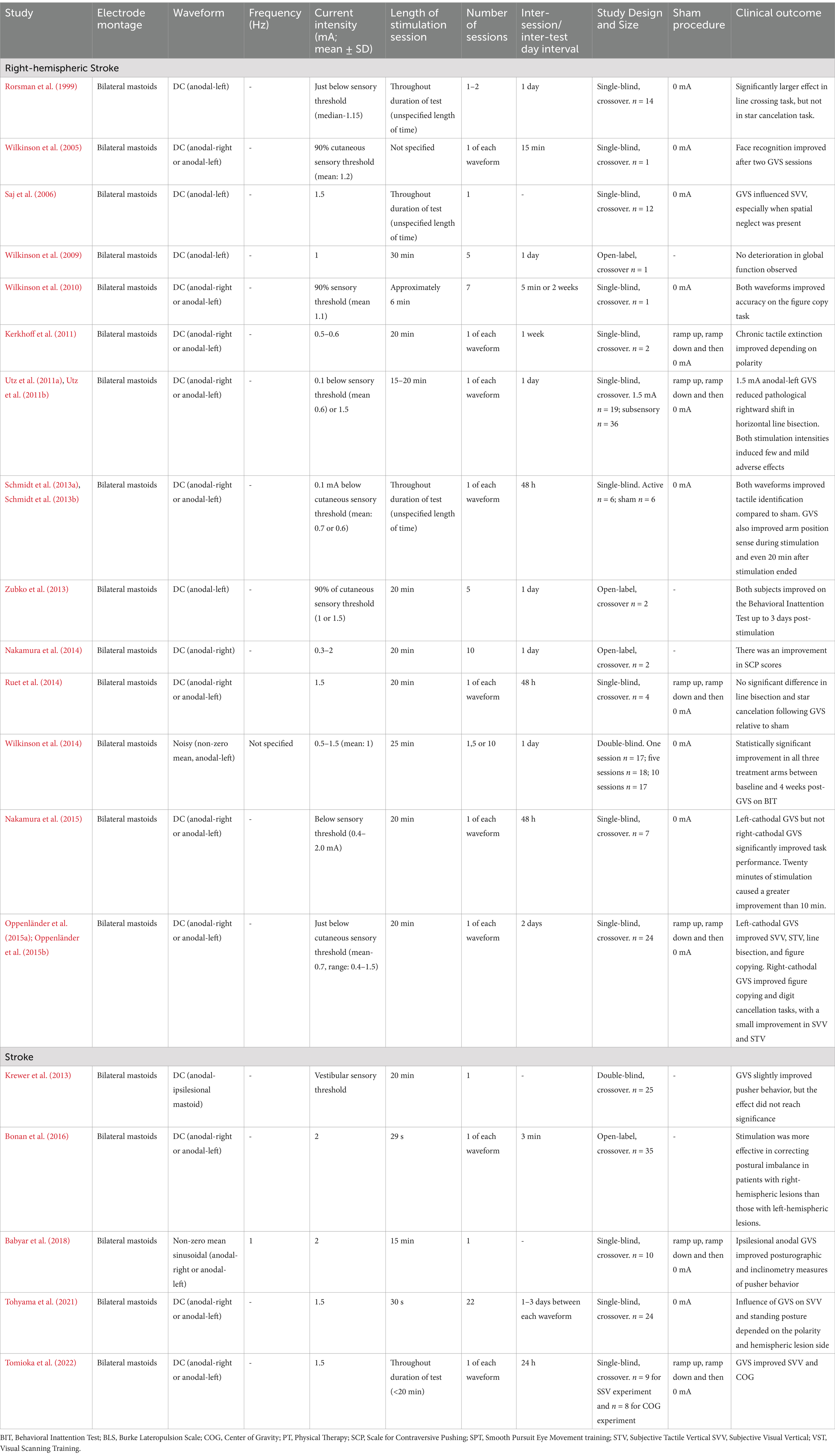
Table 3. GVS stimulation parameters for post-stroke patients and reported clinical outcomes.
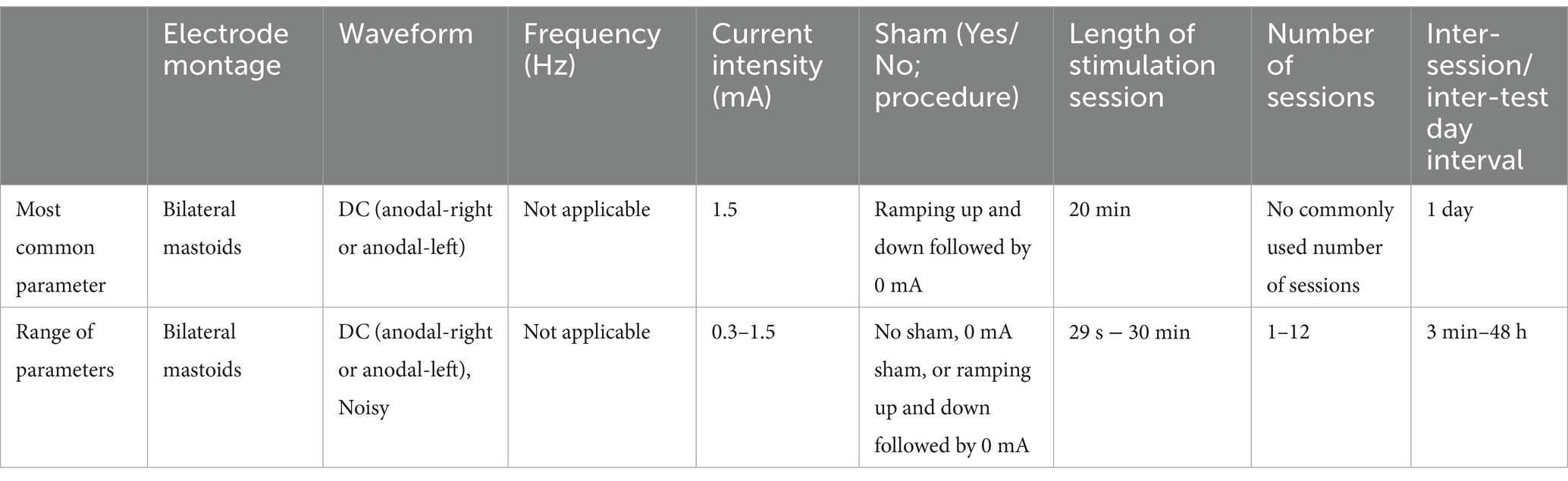
Table 4. Most common parameters and range of parameters used for post-stroke patients.
3.2.1 Electrode montage, waveform, and frequencyLike GVS for improved balance, post-stroke studies have overwhelmingly preferred the bilateral-bipolar montage. However, while GVS studies aimed at improving postural control usually employ a noisy waveform, DC stimulation has been predominantly utilized for post-stroke patients, due to its ability to shift the subjective vertical (except for Wilkinson et al., 2014 who found improvement with a non-zero noisy waveform). Consequently, frequency is generally considered irrelevant in the context of GVS for post-stroke rehabilitation.
Regarding electrode polarity, earlier studies typically positioned the anodal electrode on the contralateral side of the lesion (Rorsman et al., 1999; Saj et al., 2006; Wilkinson et al., 2009). In contrast, more recent research has investigated the effects of placing the anodal electrode on either the ipsilesional or contralesional side for comparative purposes, usually a day apart to prevent carryover effects. As anticipated, these studies have often demonstrated greater symptom improvement when the anode was positioned contralaterally (Utz et al., 2011a; Nakamura et al., 2015; Babyar et al., 2018).
3.2.2 Intensity and sham controlSimilar to studies on improving postural control, GVS for post-stroke patients is often administered at an intensity just below the cutaneous sensory threshold to ensure that subjects remain naïve to the stimulation. In other studies, a set intensity was chosen, usually between 1 and 2 mA (Saj et al., 2006; Wilkinson et al., 2009; Utz et al., 2011a, etc.).
The application of DC results in perceptible sensation (starting ~0.3 mA) around the electrode sites for the first few minutes of stimulation. Subjects generally habituate to the sensation thereafter. Therefore, for supersensory studies, blinding was often achieved by delivering a brief stimulation current to the subjects in the sham arm and slowly ramping down the stimulation without the subject realizing. This 0 mA level is maintained for the rest of the session. Due to the habituation that occurs with prolonged DC exposure, the initial sensation, along with the subsequent ramp-down phase and eventual absence of sensation in the sham group, closely mirrored the experiences of subjects receiving active stimulation. However, consistent with studies on impaired postural control, the most common sham-blinding procedure in post-stroke GVS research involves placing electrodes on the mastoids, as in active stimulation, but withholding any current delivery.
3.2.3 Stimulation sessions: length, number, and intervalSome studies tested the effect of stimulation on the performance of a specific task performed while stimulation was being delivered. In these studies, the stimulation length corresponded to the length of time it took the subject to perform the task (Rorsman et al., 1999; Saj et al., 2006; Tomioka et al., 2022; Schmidt et al., 2013a; Schmidt et al., 2013b). Other studies used the 20- or 30-min stimulation protocol (Zubko et al., 2013; Nakamura et al., 2014; Ruet et al., 2014) based on the safety protocol recommended for tDCS, as explained earlier.
Much like studies on postural control, GVS research involving post-stroke patients has largely concentrated on the effects of a single stimulation session, or in some cases, one session of each waveform spaced a day apart. Nevertheless, a subset of studies has explored the cumulative impact of repeated sessions, typically conducted with a one-day interval between each session. In both single and repeated session trials, most studies reported significant symptom improvements, with the exception of Krewer et al. (2013) and Ruet et al. (2014).
3.3 Other clinical applicationsMotion sickness remains a frequent problem in the modern day as there are more frequent forms of passive motion (i.e., car, train, airplane) that occupy a substantial portion of individuals’ everyday life (Bertolini and Straumann, 2016). The onset of motion sickness includes feelings of uneasiness, and symptoms can rapidly progress to dizziness, nausea, vomiting, and loss of appetite. Motion sickness is a considerable health concern as some individuals may undergo a physiological habituation process, whereas others require lifelong motion sickness medications for their chronic susceptibility (Gutkovich et al., 2021). Currently, the most widely accepted theory on motion sickness is explained by the sensory conflict model which occurs when there are discrepancies between the proprioceptive, vestibular, and visual senses and the brain’s expectation of sensory signals. Gutkovich et al. tested the application of GVS to sailors susceptible to motion sickness (i.e., seasickness) Participants were restrained to a rotating chair and wore goggles that entirely restricted their vision. They received sinusoidal GVS in an inverse phase to chair rotation, anode stimulation applied toward the rotation side. The sailors receiving active GVS reported a decrease in seasickness symptoms upon their following sea voyages compared to the sham group (Gutkovich et al., 2021).
Simulated (virtual) environments also cause symptoms of motion sickness stemming from the mismatch between vestibular and visual inputs (“cybersickness”; Geyer and Biggs, 2018). This mismatch is primarily attributed to the same sensory conflict theory as motion sickness experienced while in passive motion (Reason, 1978; Oman, 1982; Oman, 1990). This mismatch induces motion sickness symptoms as well as compromising the immersive experience, and thereby the effectiveness of the virtual reality (VR) experience. Two different GVS methods have been investigated for the alleviation of cybersickness symptoms: matched-GVS and noisy GVS. For the first method, Cevette et al. applied matched-GVS using a novel electrode montage—two electrodes on each mastoid as well as one on the forehead and one at the back of the neck. Using this setup, they delivered stimulation over multiple independent “channels” to induce sensations of motion in multiple different directions corresponding to the direction and magnitude of the simulated motion in VR. The direction of GVS-induced perceived rotation depended on the direction of current between each of the four electrodes. By matching vestibular cues to visual cues, the gap of visual-vestibular sensory incongruence is resolved, intending to alleviate cybersickness symptoms (Cevette et al., 2012). The second method (noisy GVS) sends zero-mean white noise to potentially facilitate sensory re-weighting. A possible explanation provided by the authors is that a noisy vestibular stimulus rapidly reduces vestibular cue reliability, causing visual self-motion cues to be up-weighted in return (Weech et al., 2020). In a similar fashion, Dilda et al. delivered a sum-of-sines (i.e., multisine) waveform to healthy volunteers and found that it trained them to up-weight non-vestibular cues, suggesting that GVS could serve as an effective pre-flight training method for preparing astronauts to manage vestibular perturbations experienced during spaceflight (Dilda et al., 2014).
Recently, GVS has been explored as a method to promote sleep (Kishi et al., 2023; Goothy and McKeown, 2021). Kishi et al. (2023) induced a rocking sensation through sinusoidal GVS current to facilitate sleep, a phenomenon similar to the findings of Bayer et al. (2011) who demonstrated that rocking helps synchronize brain waves, reinforcing endogenous sleep rhythms—much like the traditional practice of rocking infants to sleep. In 2023, the U.S. Food and Drug Administration (FDA) approved the first GVS-based device for therapeutic use: the Modius Sleep device, for treating chronic insomnia (Food and Drug Administration, 2023). However, the Modius Sleep device uses symmetrical biphasic rectangular waveforms, similar to those used in cranial electrotherapy stimulation (CES) devices, rather than the sinusoidal GVS current typically employed to induce a rocking sensation. CES devices traditionally deliver stimulation through electrodes placed on the temples, earlobes, or in the ear and are commonly used to treat conditions such as anxiety and depression (Datta et al., 2013; Brunyé et al., 2021). Given that biphasic rectangular pulses are not traditionally used in GVS, it is possible that it was selected for the Modius Sleep device to leverage CES as a predicate for securing 510(k) clearance by aligning with the established CES regulatory pathway, rather than due to its ideal properties for GVS. The stimulation parameters used for motion sickness studies as well as other treatment indications are enumerated in Table 5.
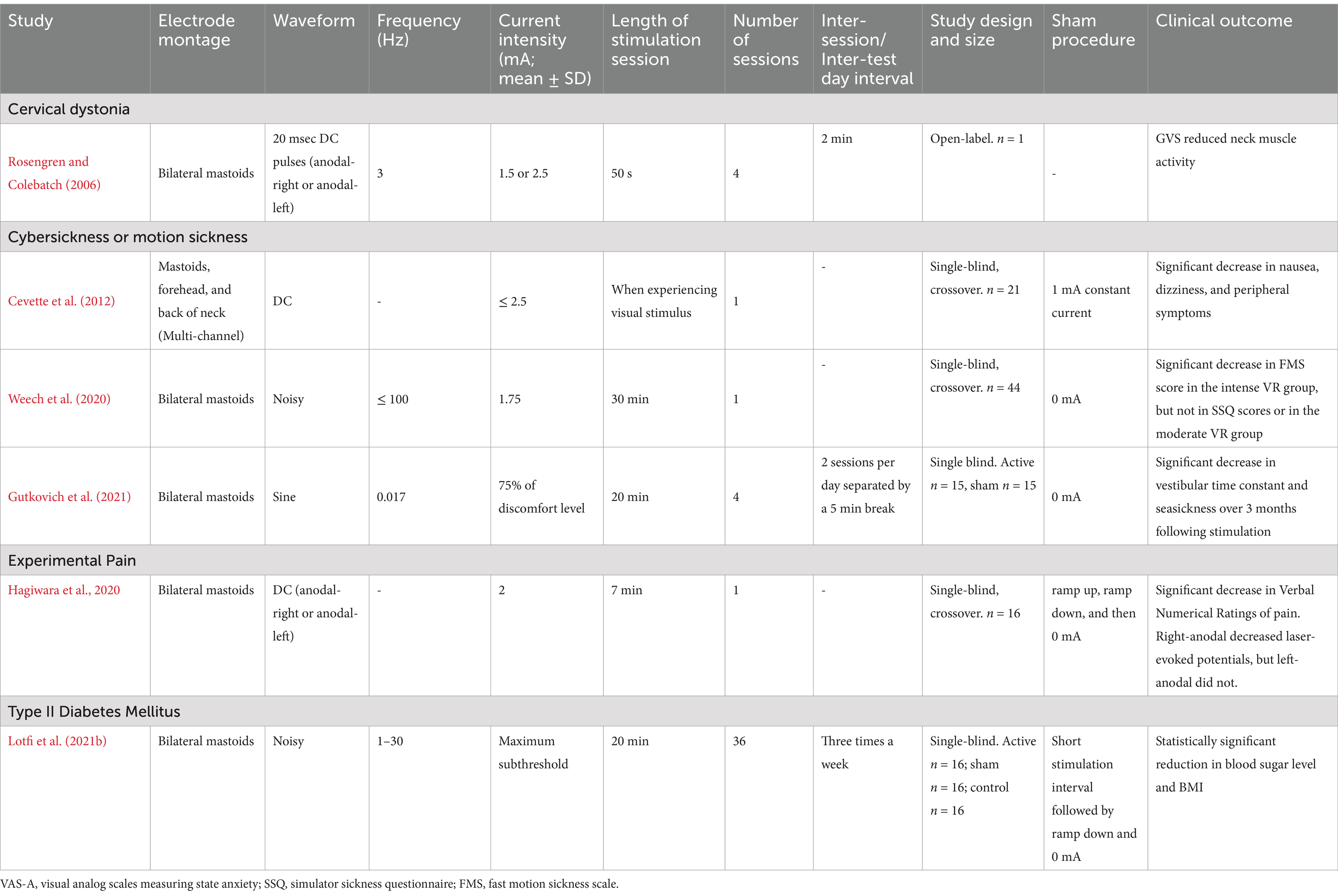
Table 5. GVS stimulation parameters investigated for other clinical applications and their clinical outcomes.
4 ConclusionThe studies discussed demonstrate that there is a notable divergence in the selection of stimulation parameters. Some parameters are widely accepted, while others remain poorly defined and require further investigation to identify the most effective settings. Studies on impaired balance usually employed noisy waveforms, driven by the beneficial effects of input noise in enhancing neural system sensitivity. This occurs through noise-enhanced responses of nonlinear systems to weak signals, a phenomenon known as stochastic resonance (Wiesenfeld and Moss, 1995). It is hypothesized that a central circuit involved in signaling movement initiation, with a pathologically elevated threshold, may benefit from noisy modulation of afferent firing rates (Pan et al., 2008). Conversely, for treating impaired verticality, studies often employed DC stimulation to counteract the misalignment (Oppenländer et al., 2015a).
With respect to current intensity, the choice has varied between choosing an individualized optimal intensity (i.e., maximizing an individual’s performance on a task), individualized subthreshold intensity, or a fixed intensity. This decision is guided by the exact outcome measure being tested and as applicable, highlights the need for personalization, as the same intensity can elicit different vestibular sensations and physiological effects in different subjects, including within the same patient population.
As expected, the choice of waveform has a bearing on the length of the stimulation session. As noisy GVS at imperceptible levels does not cause noticeable side effects in the form of oculomotor and postural responses, some studies have delivered stimulation spanning hours to an entire day. When using DC, studies have generally not exceeded the 30 min duration and inter-session duration of 1 day based on the safety criteria and protocols in place for the more thoroughly researched tDCS modality.
Repeated applications leading to cumulative and/or sustaining effects are well documented in other brain stimulation modalities (e.g., Razza et al., 2020; Black et al., 2023; Valter et al., 2024). However, most GVS studies have been limited to single session protocols. As such, there is a gap in our understanding of the long-term and cumulative effects of GVS. This highlights the need for comprehensive research to establish the appropriate treatment indication and protocol, and to examine the cumulative and long-term impacts of GVS.
In conclusion, certain GVS parameters are well-accepted for specific applications, such as the need to deliver a noisy stimulus waveform to improve postural control in Bilateral Vestibulopathy, whereas other parameters still lack consensus, such as the number of stimulation sessions necessary for improving spatial neglect in post-stroke patients. Also, a wide variety in noise frequency ranges have been used for improving postural control in subjects with vestibular disorders. While the wide range makes it difficult to determine the most effective frequency band for a given indication, it also demonstrates that a wide range of parameters are biologically active. Additional studies are therefore necessary to clarify the optimal frequency for each population and application.
GVS continues to hold significant potential for clinical utility. Furthermore, owing to low intensity current needs, GVS devices are portable and can be therefore administered across a wide variety of settings such as laboratory, clinical and home locations, mimicking protocols developed in other non-invasive brain stimulation modalities (Valter et al., 2021; Pilloni et al., 2022; Black et al., 2023). Research has also demonstrated that GVS application is even feasible in spaceflight due to its low mass and power requirements, low power usage, and minimal side effects (Putman et al., 2021; Sherman S. et al., 2023; Sherman S. O. et al., 2023). Given the safety profile, protocols can explore delivering multiple sessions over weeks and thereby expect developing clinical utility in myriad conditions. Our review serves as a suggestion for future GVS research protocols and clinical applications with respect to the choice of stimulation parameters and related considerations for specific patient populations and conditions.
Results of this review indicate that the field of GVS is still evolving, with no universally standard application guidelines. Instead, current evidence appears to be condition-dependent or patient population-specific, limiting making conclusions on an overall all-cause acceptable GVS parameter protocol, but does align more favorably with the changing clinical landscape of precision medicine practices. Nevertheless, elucidative information has surfaced from the current review that serves as the basis for early key recommendations, critical to moving the field of GVS forward. The following are those recommendations that scientists can use as reference when designing GVS research studies. First, it is essential to perform (at least one) sham condition, appropriate as a control condition for the study’s scientific objectives, and provide sufficient methodological details regarding the sham (e.g., was current applied away from the mastoids, was no current applied, were electrodes on, was the subject blinded to the GVS application, etc.). This is particularly critical for studies investigating after-effects or the longitudinal application of GVS, where there is otherwise a confound between the presence of GVS and time (which could impact learning, fatigue, boredom, etc.). We also encourage investigators, particularly for subthreshold GVS, to assess whether subjects are able to feel tingling sensations or other side effects from the GVS application, in a two-alternative forced choice test (where GVS is presented in one interval and not in the other, and the subject is required to guess which interval contained the GVS), and investigators ensure the recognition performance is no better than chance.
Second, while the literature suggests that GVS applications may require (or benefit) from personalization to each individual, this can incidentally provide investigators excessive opportunities for identifying a positive effect of GVS. For example, testing each subject with multiple amplitudes of GVS (to identify which is preferred for each individual) and then comparing each individual’s optimal amplitude to a sham condition can increase potential for false positive findings. Personalization procedures therefore need to be carefully pre-defined to ensure scientific rigor. Third, future research should aim to systematically compare multiple GVS applications (waveform, frequency, intensity, etc) in the same study for a given patient population and outcome. Nearly all prior research has only assessed one particular GVS application, requiring the field to compare across studies, performed in different laboratories, with nuanced differences in assessments, metrics, timing, and other procedures. Current, variegated approaches across studies preclude determining ‘best’ sets of GVS parameters given a specific use case. Finally, to aid in standardized GVS applications across studies, we encourage the publication of null result outcomes from GVS studies. By publishing these findings, more comparisons can be made between GVS applications that otherwise may not be noted in the literature. Further, this approach will provide advanced guidance on what GVS applications may not be useful for specific patient populations and outcomes.
Author contributionsYV: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. LV: Data curation, Formal analysis, Writing – original draft. AA: Writing – review & editing. JH: Writing – review & editing. TB: Writing – review & editing. TC: Writing – review & editing. JS: Writing – review & editing. AD: Conceptualization, Funding acquisition, Project administration, Validation, Writing – review & editing.
FundingThe author(s) declare that financial support was
留言 (0)