Urologists have accumulated experience in percutaneous nephrolithotomy (PCNL), and PCNL equipment has undergone vast development. Accordingly, the application of PCNL technology, which has become the preferred treatment for kidney stones ≥2 cm or complex urinary stones, has spread internationally (1–3). The PCNL process primarily comprises three operative steps, namely, puncture, tract dilation, and stone fragmentation. Despite being a minimally invasive surgical procedure, renal vessel damage during any of these steps can result in postoperative bleeding, which is the most prevalent complication of PCNL. It can usually be controlled via conservative methods (4).
For patients who encounter severe postoperative bleeding after PCNL and do not respond to conservative treatments, transcatheter angioembolization (TAE) stands as an effective and safe alternative with the success rate as high as 90%–100% (5–8). Patients who suffer from severe postoperative bleeding after PCNL often experience arterial injury. However, thus far, no systematic classification of renal vascular injuries has been conducted. Li et al. classified post-PCNL renal arterial injuries into three types: pseudoaneurysm (PA), arteriovenous fistula (AVF), and arterial lacerations (6). Choi et al. categorized arterial injuries as extravasation, PA, and AVF (7). Yang et al. classified post-PCNL vascular injuries as PA, AVF, and bleeding spot (8). Venkateswarlu et al. classified postoperative bleeding as PA, AVF, or active bleeding (9). Kervancioglu et al. divided postoperative bleeding into PA, AVF, arteriocaliceal fistula (ACF) (10). This retrospective study analyzed the clinical characteristics of TAE patients in our center over a 14 year period, systematically analyzed the types of vascular injuries, and compared the differences in the clinical characteristics of various injury types.
Methods Study population and designA retrospective analysis was conducted on 52 patients who underwent renal arteriography (RA) examination after severe postoperative bleeding following PCNL from April 2009 to December 2023. Among these patients, 38 had positive RA findings and underwent TAE. The specific clinical processing procedure is shown in Figure 1. Clinical data, including gender, age, BMI, TAE interval, hemoglobin (Hb) decrease, bleeding type, preoperative urine routine and urine culture results, preoperative hydronephrosis (11), operation time, stone size, preoperative creatinine (Cr) level, number of tracts, tract size, and baseline diseases, were summarized. The types of vascular injuries in these patients were analyzed, and the relationships between vascular injury types and clinical characteristics were summarized. Inclusion criterion was ① all patients who underwent RA examination after PCNL. Exclusion criteria were ① patients with negative RA findings; and ② patients lacking follow-up data after surgery.
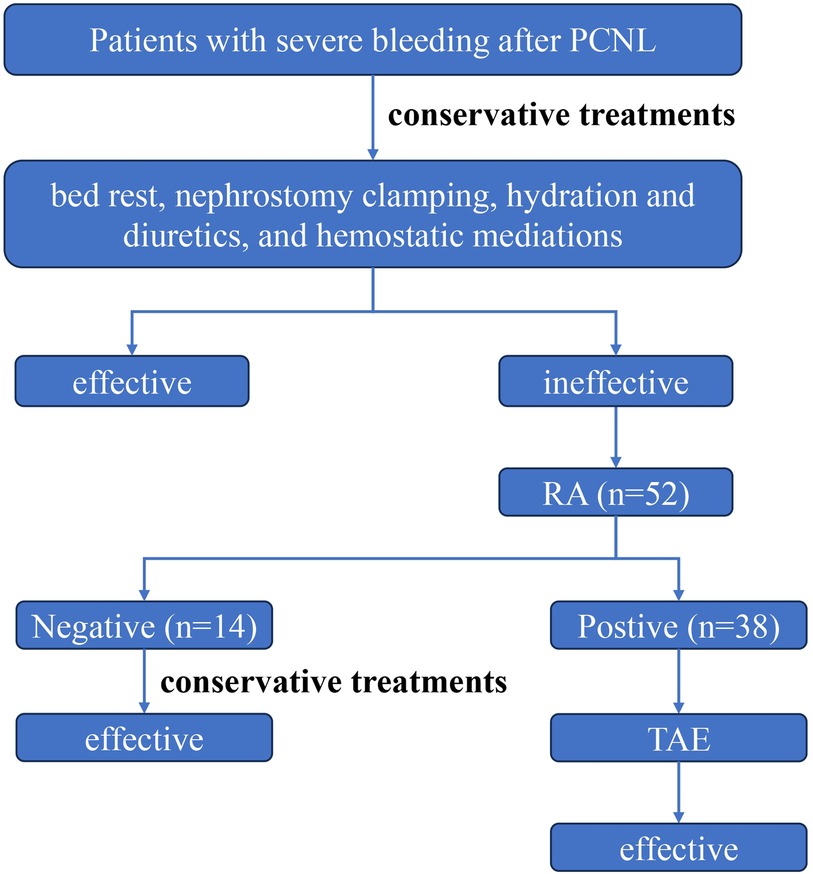
Figure 1. The clinical management flowchart for patients with severe bleeding after PCNL. Patients with severe bleeding after PCNL are initially treated by conservative measures. If conservative treatment is ineffective, a RA examination is recommended. If the RA is negative, conservative management continues; if the RA is positive, the patient undergoes TAE treatment.
ProcedureRA and TAE are common procedures done for diagnosis and treatment of renal hemorrhage, and thus, only a brief summary is provided in this article. Patients with severe postoperative bleeding after the implementation of failed conservative methods, including bed rest, diuretics and hydration, nephrostomy clamping, and hemostatic mediations, were subjected to RA examination. The procedure was accomplished by interventional radiologists using digital subtraction angiography equipment. Local anesthesia was administered, and percutaneous vascular access was established in the right or left femoral artery. The Seldinger technique was used to position a 4–5 French guiding sheath introducer. The renal artery was accessed via renal angiography with the use of a Cobra catheter. The type, size, and location of renal vascular injury were determined through selective arterial angiography. TAE was conducted based on the findings of RA examination. In the case of negative RA findings, patients returned to the ward for continued conservative treatment. Positive RA findings prompted transcatheter embolization, which was performed using platinum microcoils, N-butyl cyanoacrylate, particles, or Spongostan, depending on the type and severity of vascular injury. Embolization was followed by repeat angiography to confirm hemostasis and exclude complications.
Observation indicatorsThe following data on TAE patients were recorded and analyzed: gender, age, BMI, TAE interval, Hb decrease, bleeding type, preoperative urine routine and urine culture results, preoperative hydronephrosis (11), operation time, stone size, preoperative Cr level, number of tracts, tract size, and baseline diseases (hypertension, diabetes, history of previous ipsilateral PCNL or ureterotomy, and renal insufficiency). The operation time spanned from ureteral catheter placement to suturing and fixation of the nephrostomy tube or suturing of the percutaneous renal tract.
Based on the literature, bleeding types were classified as follows: sudden onset, intermittent, and continuous slow (6, 12). Given the lack of specific definitions for these classifications, the following conditions were considered: sudden onset bleeding type refers to the sudden drop in Hb levels after surgery or bladder obstruction due to sudden bleeding or continuous drainage of bright-red blood from the nephrostomy tube; intermittent bleeding type refers to intermittent gross hematuria and an intermittent decrease in Hb levels; and continuous slow bleeding indicates the persistent drainage of dark red or pale red blood in urine or from the nephrostomy tube, with a slow, continuous decrease in Hb levels.
Statistical analysisStatistical analysis was accomplished using SPSS 20.0. As the number of included patients is relatively low, continuous data are presented as median (interquartile range) and were analyzed via Kruskal–Wallis H(K) test. post hoc test for pairwise comparisons was adjusted by Bonferroni method. Categorical data are presented as percentages and were analyzed using chi-square test. Statistical significance was considered at a p-value less than 0.05.
Results General clinical data of patientsTable 1 summarizes the clinical characteristics of the 38 TAE patients included in the study. After TAE treatment, bleeding was successfully controlled in all patients. These patients included 32 males and 6 females with a mean age of 51.50 (18.25) years, mean BMI of 24.05 (5.06) kg/m2, mean TAE interval of 5.00 (6.25) days, average Hb decrease of 44.50 (24.50) g/L, average operation time of 90.50 (54.50) min, mean stone size of 41.00 (39.50) mm, preoperative urine routine white blood cell count of 158 (840), Cr level of 77.55 (24.15) μmol/L, mean tract number of 1 (0.25), and tract size of F20(6) (Table 1). According to the different clinical bleeding types, continuous slow bleeding was the main bleeding type among the TAE patients (19 patients), followed by sudden onset (15 patients), and intermittent (4 patients) bleeding.
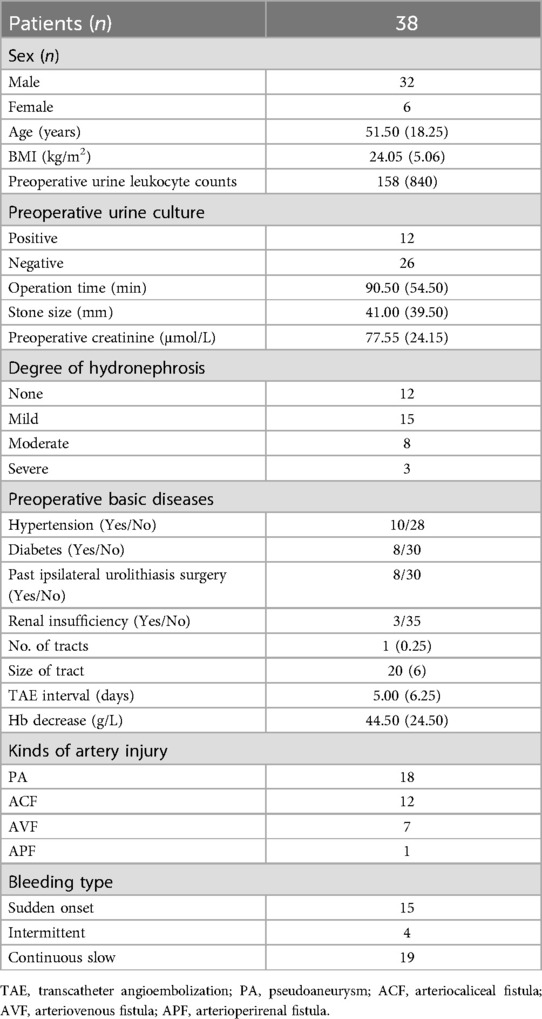
Table 1. Clinical characteristics of TAE patients.
The TAE interval ranged from the first post-PCNL day to the day of TAE. Hb decrease referred to the decrease in Hb from post-PCNL day to the day of RA. Based on the equivalence of one unit of red blood cells or whole blood to 1 g/dl Hb, the changes in Hb were corrected for patients who received blood transfusion prior to TAE (6).
Classification and characteristics of artery injury patients after PCNLThe types of vascular injuries among the 38 TAE patients were classified into four categories based on angiographic images and clinical bleeding characteristics: 18 cases of PA (Figure 2A), 12 cases of ACF (Figure 2B), 7 cases of AVF (Figure 2C), and 1 case of arterioperirenal fistula (APF) (Figure 2D). Given that only one patient with APF was included in the study, this patient was excluded from the statistical analysis. Only the clinical characteristics of patients with PA, ACF, and AVF were analyzed. Continuous data including age, BMI, urine leukocyte counts, stone size, Cr, TAE interval, Hb decrease, operation time, No. of tracts, and size of tract were analyzed via Kruskal–Wallis H(K) test. Categorical data including gender, urine culture, hydronephrosis, hypertension, diabetes, previous surgery, renal insufficiency, and bleeding type were analyzed using chi-square test. No statistically significant differences were observed among the three groups of patients in terms of gender, age, BMI, TAE interval, Hb decrease, operation time, stone size, preoperative urine routine white blood cell count, Cr level, and baseline disease status, such as hypertension, diabetes, history of previous surgeries, or renal insufficiency. The only parameter showing a statistically significant difference was the number of tracts (P = 0.032) (Table 2). And the post hoc test for pairwise comparisons of the number of tracts indicated the ACF group had more tracts than AVF group (Table 2).

Figure 2. Different types of artery injury after PCNL. (A) Left renal RA suggesting that PA is the most common type of vascular injury after PCNL. (B) Left RA showing the extravasation of contrast agent and indicating vascular injury. The patient had severe hematuria and was clinically classified as ACF. (C) RA revealing the contrast agents found in the renal veins early during angiography, which implies AVF. (D) Left kidney RA revealing the extravasation of contrast agent to the perirenal area with the inferior kidney compressed. The patients often showed decreased Hb with no evident gross hematuria, and imageological examinations usually suggest perirenal hematoma. This type of artery injury was APF.
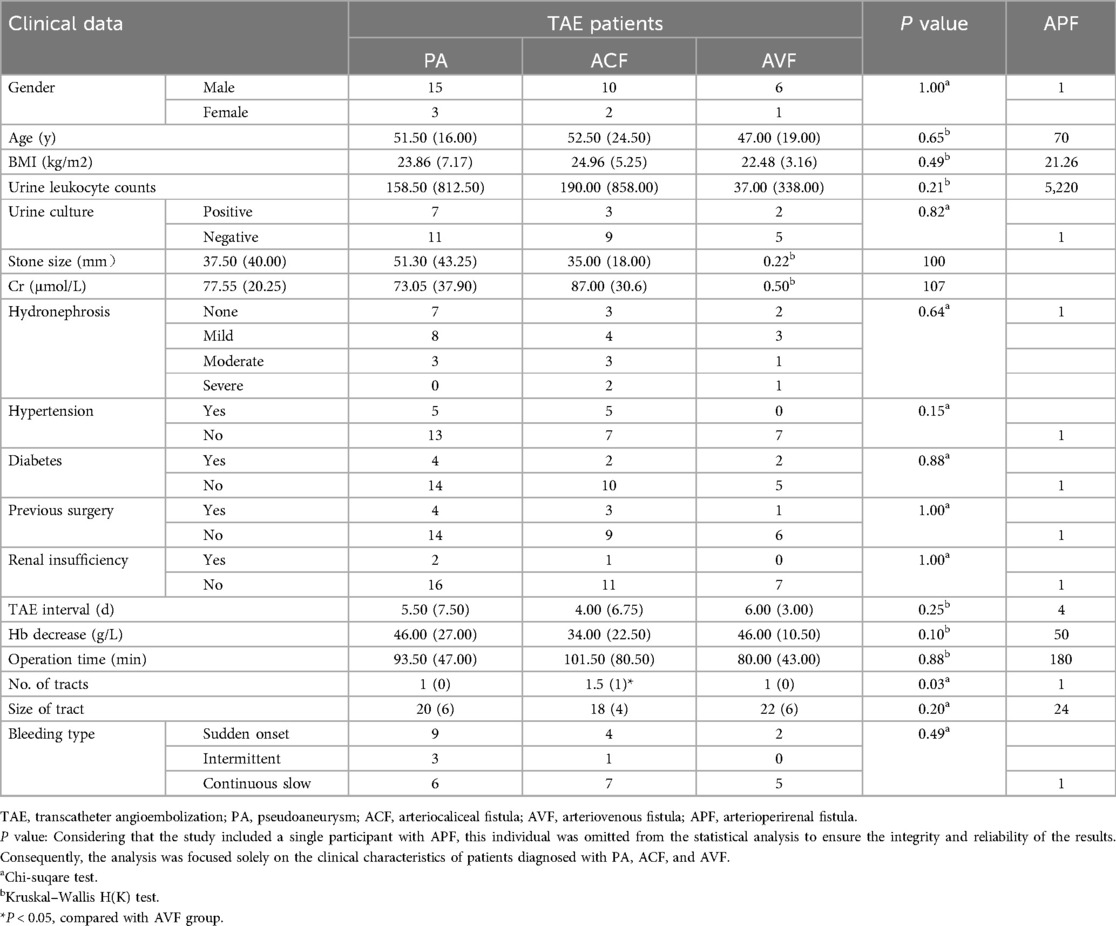
Table 2. The comparison of clinical data among different kinds of artery injury patients treated with TAE.
DiscussionRetrospective analysis of 14 years of single-center data showed that TAE effectively controlled all severe postoperative bleeding after PCNL of patients who received ineffective conservative treatments, with a mean postoperative TAE interval of 5.00 (6.25) days and a mean Hb decrease of 44.50 (24.50) g/L. All patients requiring TAE after PCNL suffered from arterial injuries. Previous studies lacked a standardized classification for post-PCNL vascular injuries. Past reports also described other types of injuries, namely, PA, AVF, arterial lacerations, extravasation, bleeding spot, active bleeding, and ACF, with PA and AVF being the most commonly mentioned (6–10).
In this study, we classified the types of vascular injuries into PA, ACF, AVF, and APF (Figure 2). PA is defined as a vascular injury where surrounding connective tissue forms an imaging characteristic similar to an aneurysm (6, 13, 14). AVF occurs when the artery and vein are involved in the injury, which leads to early arterial blood entering the vein (6, 13, 14). ACF refers to an arterial injury connected to the collecting system (10). APF includes an arterial injury connected to the renal capsule. This type of injury has not been previously reported but may be associated with compression of the renal capsule following bleeding. The patients typically present with a decrease in Hb level, accompanied with back pain and a relatively clear urine color. In addition, imaging examinations often reveal massive retroperitoneal hematoma.
In this study, the types of bleeding included 18 cases of PA, 12 cases of ACF, 7 cases of AVF, and 1 case of APF. A retrospective analysis by Li et al. revealed that among 137 patients with positive RA findings, PA, AVF, and arterial laceration accounted for 47.9%, 19.4%, and 16%, respectively (6). The proportions of PA and AVF in our study were consistent with those reported in previous research, suggesting that PA is the main type of vascular injury after PCNL.
Performing RA on patients with severe postoperative bleeding after PCNL did not necessarily indicate that the renal artery was the sole site of injury. Postoperative bleeding may result from damage of any artery during PCNL access or stone fragmentation. Figure 3 illustrates a patient with RA positivity who experienced severe bleeding after PCNL in this study. The patient had intermittent postoperative bleeding, and conservative treatment was ineffective, leading to the RA examination. However, RA examination revealed no abnormalities in the renal artery or accessory renal arteries but detected PA in the lumbar artery. The bleeding ceased following embolization. Consequently, when performing an RA examination, it is important to consider not only the renal artery but also potential injuries to the accessory renal arteries, lumbar arteries, renal capsular artery, and intercostal arteries (7, 15–17).
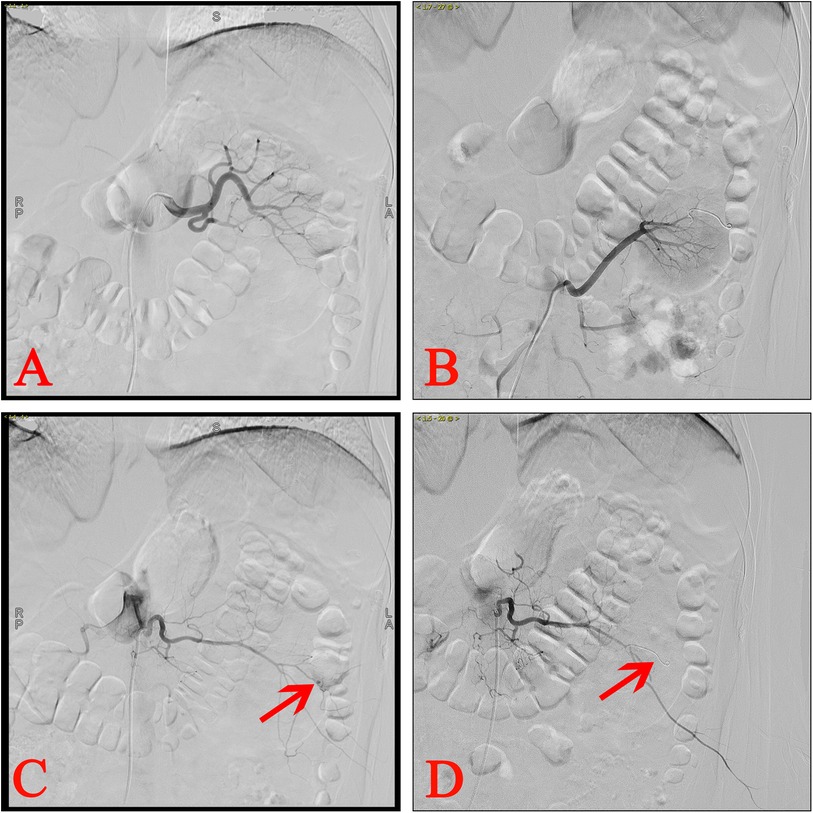
Figure 3. Ra of a patient with lumbar artery injury after PCNL. (A) Left RA showing no abnormalities. (B) Left accessory RA revealing no abnormalities. (C) Lumbar arteriography suggested PA. (D) The PA was successfully embolized.
The type of clinical bleeding detected in patients with TAE remains controversial. Li et al. retrospectively observed intermittent bleeding (46.5%) as the main type of TAE (6). The retrospective research of Ran et al. revealed sudden onset bleeding (52.9%) as the main type (12), whereas in the present study, continuous slow bleeding (50%) was the main type. Hence, to further gain insights into the clinical characteristics of patients with various types of vascular injuries, we conducted a comparative analysis of their clinical characteristics to provide guidance for interventional physicians during TAE. In this retrospective analysis, the types of vascular injuries were classified into four categories. Subgroup analysis (PA, ACF, and AVF) revealed no statistically significant differences in patient age, BMI, operation time, stone size, preoperative baseline disease status, bleeding type, etc. However, statistically significant difference was observed only in the number of tracts, suggesting that this parameter may be a predictor of different vascular injuries in TAE patients.
Currently, there is no research discussing the types of renal artery injuries in patients with severe bleeding after PCNL. However, regardless of the different type of vascular injury, TAE has been proven to be an effective method for treating severe bleeding after PCNL (6, 7, 9, 10, 13). Understanding different types of vascular injuries may assist interventional radiologists in performing RA examinations and in selecting embolic materials during TAE. In addition, although this study found that the number of tracts might be a factor in predicting the type of vascular injury, the mechanism between the two has not been clarified and requires further research.
Limitations of this study: The retrospective design of this study may introduce potential bias in the results. Conducting a prospective randomized controlled trial for patients with severe postoperative bleeding following PCNL is challenging due to the significant psychological burden it places on both surgeons and patients. Additionally, the study included only one case of APF, which was insufficient for statistical analysis despite its notable clinical characteristics. Further research with larger sample sizes is needed to enhance the validity of these findings.
ConclusionThis retrospective analysis revealed that TAE effectively controlled severe postoperative bleeding after PCNL. The types of vascular injuries in TAE patients were classified as PA, ACF, AVF, or APF. Further analysis revealed the number of tracts as a possible predictor of the different types of vascular injuries in TAE patients.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Ethics Committee of the First Affiliated Hospital with Nanjing Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributionsXM: Writing – original draft, Writing – review & editing. RC: Writing – original draft. YH: Writing – original draft. ZW: Writing – review & editing. NS: Writing – review & editing. WY: Writing – review & editing. RS: Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was funded by Jiangsu Province Capability Improvement Project through Science, Technology and Education (No. ZDXK202219).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Ruhayel Y, Tepeler A, Dabestani S, MacLennan S, Petřík A, Sarica K, et al. Tract sizes in miniaturized percutaneous nephrolithotomy: a systematic review from the European association of urology urolithiasis guidelines panel. Eur Urol. (2017) 72:220–35. doi: 10.1016/j.eururo.2017.01.046
PubMed Abstract | Crossref Full Text | Google Scholar
2. Akdogan N, Deger M, Yilmaz IO, Borekoglu A, Yucel SP, Izol V, et al. Is percutaneous nephrolithotomy effective and safe in infants younger than 2 years old? Comparison of mini standard percutaneous nephrolithotomy. J Pediatr Urol. (2023) 14:S1477–5131(23)00558–2. doi: 10.1016/j.jpurol.2023.12.004
Crossref Full Text | Google Scholar
3. De Stefano V, Castellani D, Somani BK, Giulioni C, Cormio A, Galosi AB, et al. Suction in percutaneous nephrolithotripsy: evolution, development, and outcomes from experimental and clinical studies. Results from a systematic review. Eur Urol Focus. (2023) 11:S2405-4569(23)00152-9. doi: 10.1016/j.euf.2023.06.010
Crossref Full Text | Google Scholar
4. Zheng Z, Xu J, Li Z, Mao L, Zhang W, Ye Z, et al. Development and internal validation of a prediction model to evaluate the risk of severe hemorrhage following mini-percutaneous nephrolithotomy. World J Urol. (2023) 41:843–8. doi: 10.1007/s00345-023-04291-5
PubMed Abstract | Crossref Full Text | Google Scholar
5. Zhaohui H, Hanqi L, Xiongbing L, Caixia Z, Shawpong W, Guohua Z. Analysis of repeated renal arteriography after percutaneous nephrolithotomy. Urolithiasis. (2017) 45:495–9. doi: 10.1007/s00240-016-0936-z
PubMed Abstract | Crossref Full Text | Google Scholar
6. Li L, Zhang Y, Chen Y, Zhu KS, Chen DJ, Zeng XQ, et al. A multicentre retrospective study of transcatheter angiographic embolization in the treatment of delayed haemorrhage after percutaneous nephrolithotomy. Eur Radiol. (2015) 25:1140–7. doi: 10.1007/s00330-014-3491-4
PubMed Abstract | Crossref Full Text | Google Scholar
7. Choi MJ, Kim PH, Shin JH, Kim JW, Gwon DI, Kim JH, et al. Angiographic management of percutaneous renal procedure-related bleeding: a single-center experience. Int J Urol. (2019) 26:406–12. doi: 10.1111/iju.13891
PubMed Abstract | Crossref Full Text | Google Scholar
8. Yang BB, Liu WZ, Ying JP, Li C, Huang T, Shi JY, et al. Computed tomography angiography and three-dimensional reconstruction of renal arteries in diagnosing the bleedings after Mini-percutaneous nephrolithotomy: a single-center experience of 7 years. Urology. (2022) 169:47–51. doi: 10.1016/j.urology.2022.07.028
PubMed Abstract | Crossref Full Text | Google Scholar
9. Venkateswarlu J, Kumar MS, Babu RP, Abkari A. Endovascular management of iatrogenic renal vascular injuries complicating percutaneous nephrolithotomy: role of renal angiography and embolization; an analysis of 159 cases. Indian J Radiol Imaging. (2017) 27:293–7. doi: 10.4103/ijri.IJRI_54_17
PubMed Abstract | Crossref Full Text | Google Scholar
10. Kervancioglu S, Gelebek Yilmaz F, Erturhan S. Endovascular management of vascular complications after percutaneous nephrolithotomy. Vasa. (2014) 43:459–64. doi: 10.1024/0301-1526/a000393
PubMed Abstract | Crossref Full Text | Google Scholar
11. Ito Y, Kikuchi E, Tanaka N, Miyajima A, Mikami S, Jinzaki M, et al. Preoperative hydronephrosis grade independently predicts worse pathological outcomes in patients undergoing nephroureterectomy for upper tract urothelial carcinoma. J Urol. (2011) 185:1621–6. doi: 10.1016/j.juro.2010.12.035
PubMed Abstract | Crossref Full Text | Google Scholar
12. Ran R, Zhang R, Xie Y, Yin Z. Decreased hemoglobin as a quantifiable indicator of renal arterial embolization in post-percutaneous nephrolithotomy hemorrhage. Urolithiasis. (2021) 49:137–43. doi: 10.1007/s00240-020-01206-6
PubMed Abstract | Crossref Full Text | Google Scholar
13. Poyraz N, Balasar M, Gökmen İE, Koç O, Sönmez MG, Aydın A, et al. Clinical efficacy and safety of transcatheter embolization for vascular complications after percutaneous nephrolithotomy. Wideochir Inne Tech Maloinwazyjne. (2017) 12:403–8. doi: 10.5114/wiitm.2017.69108
PubMed Abstract | Crossref Full Text | Google Scholar
14. Tayeb MM E, Knoedler JJ, Krambeck AE, Paonessa JE, Mellon MJ, Lingeman JE. Vascular complications after percutaneous nephrolithotomy: 10 years of experience. Urology. (2015) 85:777–81. doi: 10.1016/j.urology.2014.12.044
PubMed Abstract | Crossref Full Text | Google Scholar
15. Li S, Zhang X, Zheng J, Su H. Post-percutaneous nephrolithotomy bleeding from a variant small accessory renal artery: a case report. Asian J Surg. (2023) 46:5346–8. doi: 10.1016/j.asjsur.2023.07.089
PubMed Abstract | Crossref Full Text | Google Scholar
16. Tummala V, Nanavati KI, Yrizarry JM, Scagnelli T. Lumbar artery pseudoaneurysm following percutaneous nephrolithotripsy: treatment by transcatheter embolization. Indian J Urol. (2008) 24:408–10. doi: 10.4103/0970-1591.42628
PubMed Abstract | Crossref Full Text | Google Scholar
17. Liu Q, Yang C, Lin K, Yang D. Bleeding of two lumbar arteries caused by one puncture following percutaneous nephrolithotomy: a case report. World J Clin Cases. (2020) 8:5790–4. doi: 10.12998/wjcc.v8.i22.5790
留言 (0)