Chronic Obstructive Pulmonary Disease (COPD) and asthma are two prevalent respiratory diseases that significantly affect patients’ respiratory function and quality of life. Inhaled medications include long-acting beta2-agonists (LABA), long-acting muscarinic antagonists (LAMA), and inhaled glucocorticoids (ICS). This combination of drugs can act in concert through different mechanisms to improve respiratory symptoms, reduce the risk of exacerbations, and improve patients’ quality of life. In recent years, the research progress of inhaler triple therapy (LABA + LAMA + ICS) as an essential treatment for COPD and asthma has attracted much attention.
GOLD 2024 indicates triple therapy (LABA + LAMA + ICS) for patients at high risk for acute exacerbation of COPD who are poorly controlled on duo therapy (LABA + LAMA/LABA + ICS) or have eosinophils ≥300/ul (GOLD Report, 2024). The risk of acute exacerbation, risk of hospitalization, and risk of death were significantly lower in the triple therapy group of COPD patients compared with the duo therapy group (Martinez et al., 2021; Lipson et al., 2018; Lipson et al., 2020). Although there was an increased risk of pneumonia, triple therapy had a better benefit-risk ratio (Lee et al., 2019; Dransfield et al., 2021). GINA 2024 states that inhaler triple therapy may be considered for adult patients whose disease is not controlled with low to moderate doses of ICS and LABA (Reports, 2024). Studies have found that asthma patients in the triple therapy group exerted better results in improving lung function and reducing the number of acute exacerbations compared to the duo therapy group (Lee et al., 2021; Virchow et al., 2019). Several studies involving China, Spain, and the United Kingdom have shown that triple therapy is more cost-effective than single- or two-drug therapy (Zhou et al., 2021; Paly et al., 2022; Kendall et al., 2023). Patient compliance was improved with the application of a single inhaler compared to multi-inhaler triple therapy (Mannino et al., 2022).
Budesonide/Glycopyrronium/Formoterol Fumarate (BUD/GLY/FOR) and Fluticasone Furoate/Umeclidinium/Vilanterol (FF/UMEC/VI) are the two most common single-inhaler triple therapy. Regarding timing, FF/UMEC/VI was approved to begin marketing in the United States in September 2017 (FDA, 2017), followed by the European Union and China. BUD/GLY/FOR has been available in the U.S. since July 2020 (FDA, 2020) and has since been launched in Japan, China, and the European Union. Two meta-analyses suggest that BUD/GLY/FOR is comparable to other triple inhalations regarding acute exacerbations of COPD and improvement in lung function (Ferguson et al., 2020; Rogliani et al., 2022). Another study found FF/UMEC/VI superior to other triple-therapies for annual acute exacerbations and symptoms of COPD (Ismaila et al., 2022). There are few randomized controlled studies of BUD/GLY/FOR in the treatment of asthma, and even fewer studies comparing the efficacy of BUD/GLY/FOR with FF/UMEC/VI.
Similarly, there is a paucity of studies on BUD/GLY/FOR versus FF/UMEC/VI adverse drug events (AEs), and our study focused on exploring and comparing the AEs of the two drugs. Although clinical trials are essential in identifying drug AEs, certain AEs are not easily detected, thus affecting drug efficacy and patient prognosis (Feagins et al., 2019). This study’s purpose was to determine the AEs related to FF/UMEC/VI and BUD/GLY/FOR through the U.S. Food and Drug Administration’s (FDA) Adverse Event Reporting System (FAERS) to provide real-world evidence of potential AEs for single-inhaler triple therapy.
MethodsData sourcesWe performed this real-world pharmacovigilance study based on FAERS. The FAERS database is an FDA adverse event reporting system that includes information on AE and drug medication errors (Sakaeda et al., 2013). The source of data for the FAERS database is primarily reports from within the United States, but also includes some international reports from multinational companies. FAERS is updated quarterly, and AE report data comes from physicians, consumers, or forms submitted by drug manufacturers (Matera et al., 2024). When an AE occurs, the appropriate person (e.g., physician or patient) submits a report to FAERS. When submitting a report, the patient may choose to remain anonymous or provide limited information. The database’s high sample size and broad range of AE reports make it the best way to explore rare AEs (Silberstein et al., 2023).
We downloaded the American Standard Code for Information Interchange (ASCII) reporting files for drugs in the FAERS. Considering the time to market of the drug and the number of AEs, we download the BUD/GLY/FOR reporting files for Q3 2020 through Q3 2024 and the FF/UMEC/VI reporting files for Q1 2018 through Q3 2024. The data were processed using R4.2.3.
Data extraction and analysisRemove duplicate items from the report. The latest report was retained for information with the same caseid number in the DEMO table. The Medex_UIMA_1.8.3 system standardized drug names to extract reports with BUD/GLY/FOR as the primary drug and reports with FF/UMEC/VI as the primary drug. The specific names of the medications screened are shown in Supplementary Tables S1, S2.
The Medical Dictionary of Regulatory Activities (MedDRA-v24) is a detailed collection of standardized medical terminology used to harmonize medication AEs (Sharma and Kumar, 2022; Javed and Kumar, 2024). The hierarchical structure of MedDRA consists of Low-Level Term (LLT), Preferred Term (PT), High-Level Term (HLT), Higher-Level Group Term (HLGT), and Systems and Organs Classification (SOC) (Brown, 2003). We coded and categorized the signals using the most commonly used PTs and SOCs.
Disproportionality analysis is a method to address the presence of asymmetry in pharmacovigilance analysis (van Puijenbroek et al., 2002). We used three types of disproportionality analyses, including reported odds ratio (ROR), proportional reporting ratio (PRR), and Bayesian confidence propagation neural network (BCPNN). ROR and PRR show better specificity for detecting early adverse reaction signals, whereas BCPNN has a more vital ability to detect rare signals (Singh, 2015; Zou et al., 2024). All of the above algorithms are based on a 2 × 2 list of columns (Table 1), while the formulas and thresholds for the three methods are shown in Table 2.
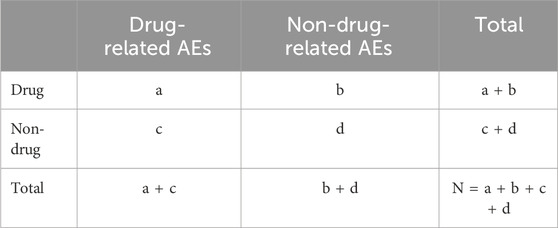
Table 1. Four grid table.
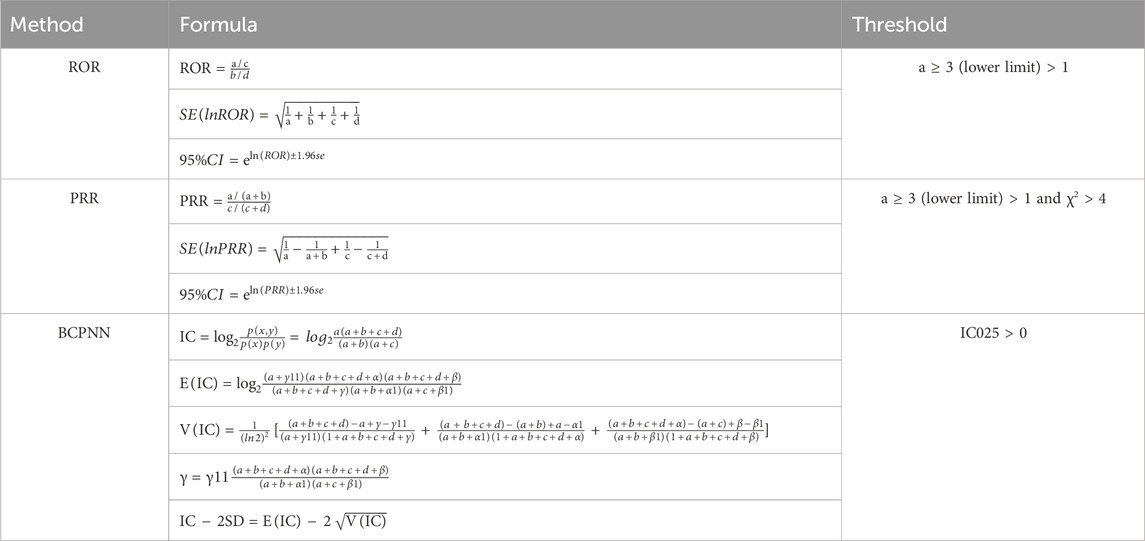
Table 2. ROR, PRR, and BCPNN methods, formulas, and thresholds.
First, after removing duplicates from the data, we extracted adverse events regarding BUD/GLY/FOR and FF/UMEC/VI. We then plotted line graphs based on the number of AEs for both drugs with each quarter. We calculated the number of AEs, PRR, ROR, and IC values for BUD/GLY/ for or FF/UMEC/VI under each system based on system organ classification (SOC).
Then, at the preferred term (PT) level, we listed adverse events for both drugs in order of the number of adverse events. We classified “device use issue,” “wrong technique in product usage process,” and “product use issue” as “device use issue” to see the incidence of device use problems for both drugs. We also conducted subgroup analyses at the PT and SOC levels based on age, gender, and reporting countries subgroups.
At the PT level, we also showed the signal strength of each AE, sorted by IC effect size. We excluded two types of PTs, medication-related illnesses and equipment use problems, focusing on the top 10 AEs in terms of signal intensity for each medication and one AE, pneumonia (the AE we were interested in). In addition, PTs present outside the drug leaflets were also analyzed and compared. In addition, we summarized time-scan plots of safety signals reflecting trends in drug-AE pairings based on IC value. Stable associations between drugs and AEs were demonstrated when the IC values for each year in the time-scan plots were greater than zero. PTs with at least 2 years of data were selected for analysis.
ResultsDescriptive characteristicsFigure 1 shows the screening process for the two drug AEs. First, 10276831 AE reports (2020Q3-2024Q3) and 6099615 AE reports (2018Q1-2024Q3) were collected from the FAERS database, respectively. After removing duplicate records, 5378 AE reports and 16,355 AEs were collected for BUD/GLY/FOR, and 19,578 AE reports and 39,110 AEs were collected for FF/UMEC/VI. Figure 2 shows the change in peaks per AE report, with FF/UMEC/VI having the highest percentage of AE reports in 2022 Q3 (1106,6.76%) and BUD/GLY/FOR having the highest number of AE reports in 2024 Q3 (643, 11.96%).
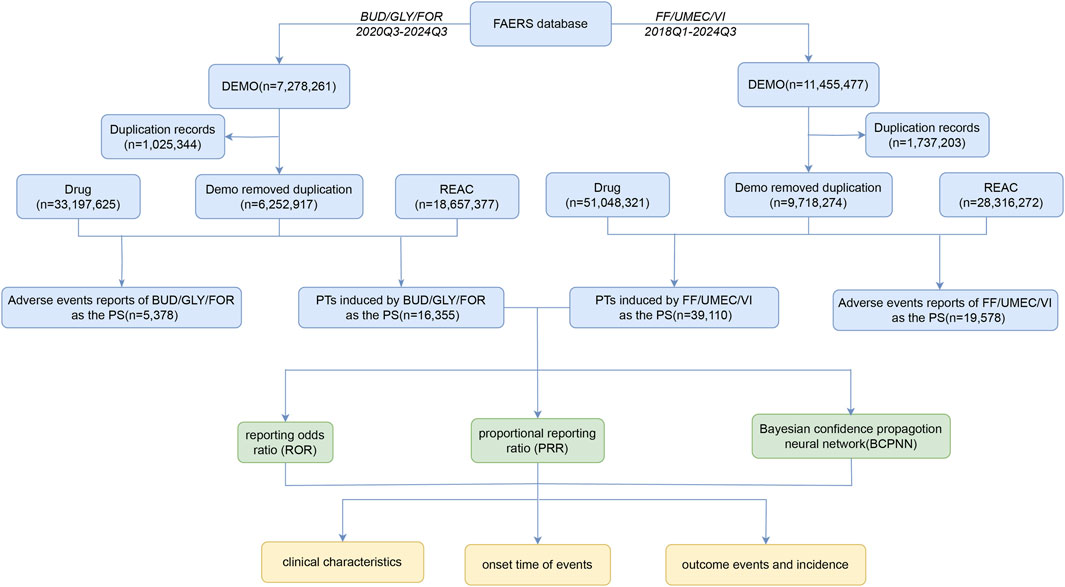
Figure 1. Flowchart of the study.
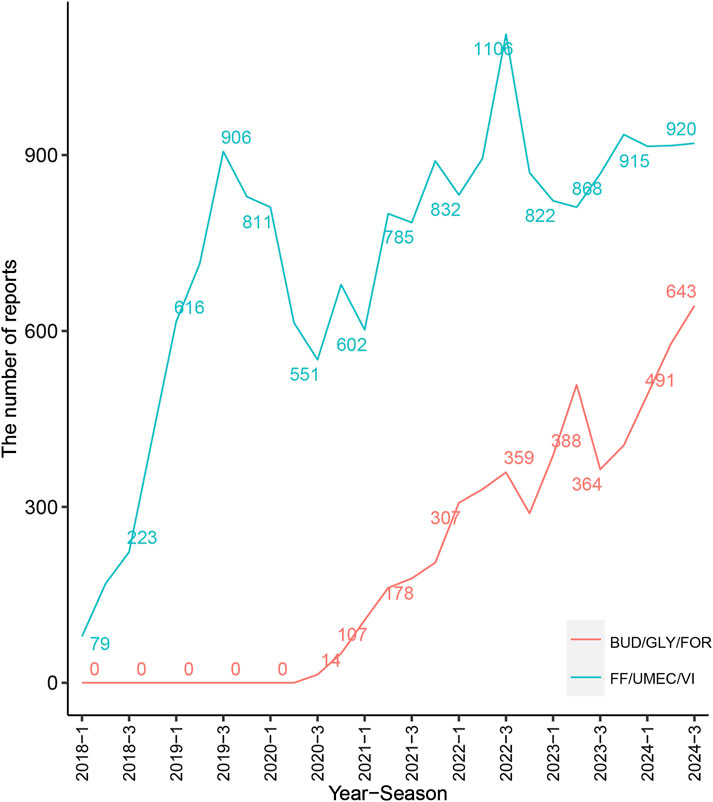
Figure 2. Number of reported cases of BUD/GLY/FOR and FF/UMEC/VI.
Table 3 shows the baseline information of the reporting population for both drug classes. Among them, the number of AE reports against FF/UMEC/VI and BUD/GLY/FOR was 9,079 (46.37%) and 2,443 (45.43%) in females, and AE reports were 6,361 (32.49%) and 1953 (36.31%) in males. In terms of age, apart from the fact that most of the data were missing, the 66–79 age group reported the highest proportion of AEs in the remaining data. Most AE reports originated from consumers (BUD/GLY/FOR, 74.17%; FF/UMEC/VI, 86.56%). In addition, the leading country for AE reporting is the United States, followed by Japan and China, and the main sources of FF/UMEC/VI reporting also involve Canada and the United Kingdom.
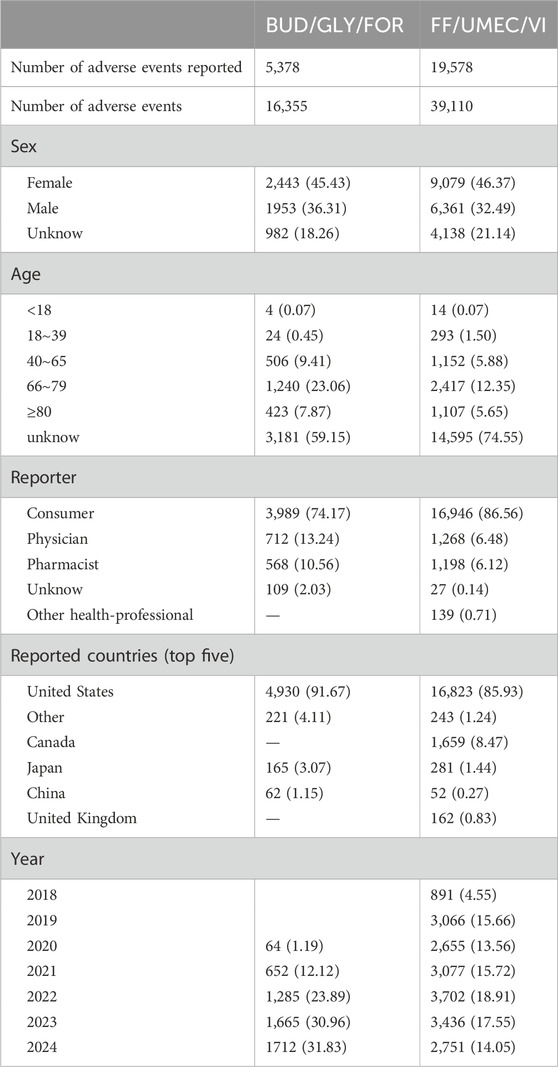
Table 3. Characterization of AE reports in BUD/GLY/FOR and FF/UMEC/VI.
Disproportionality analysesSupplementary Table S3 shows the SOCs associated with BUD/GLY/FOR and FF/UMEC/VI. “Respiratory, thoracic and mediastinal disorders (BUD/GLY/FOR: 3,246, 19.85%; FF/UMEC/VI: 8,613, 22.02%),” “Injury, poisoning and procedural complications (BUD/GLY/FOR: 5,651, 34.55%; FF/UMEC/VI: 10,073, 25.76%),” “Eye disorders (BUD/GLY/FOR: 452, 2.76%; FF/UMEC/VI: 857, 2.19%)” were the three SOCs that conformed to the study algorithms. “Ear and labyrinth disorders” in BUD/GLY/FOR (91 cases, 0.56%) and “Infections and infestations” in FF/UMEC/VI (2,669 cases, 6.82%) fit the study algorithms. In addition, Supplementary Table S4 shows the number of AEs grouped by sex, age, and reporting countries at the SOC level.
Supplementary Table S5 shows that at the PT level, sorted by the number of AEs, we extracted a total of 882 PTs in both drugs. In addition to drug-related diseases, the number of signals of device misuse is very high. The results revealed that a higher percentage of patients had “device use issues” with BUD/GLY/FOR (2,430, 14.86%) compared to FF/UMEC/VI (2,314, 5.92%). Supplementary Table S5 shows that 320 PTs met the criteria of the study algorithm. After sorting by IC values, there were 141 PTs associated with BUD/GLY/FOR and 259 PTs associated with FF/UMEC/VI.
As shown in Table 4, a total of 17 PTs belonging to 7 socs were screened based on the top 10 highest IC values for each drug. In Respiratory, thoracic, and mediastinal disorders, the pharyngeal and vocal folds category of PTs were pharyngeal erythema (BUD/GLY/FOR: N = 9, 0.055%, ROR = 17.57, IC = 4.11; FF/UMEC/VI: N = 6, 0.015%, ROR = 4.79, IC = 2.25), vocal cord disorder (BUD/GLY/FOR: N = 9, 0.055%, ROR = 22.1, IC = 4.43; FF/UMEC/VI: N = 10, 0.026%, ROR = 9.81, IC = 2.42), dysphonia (BUD/GLY/FOR: 1.20%, N = 197, ROR = 12.98, IC = 3.48; FF/UMEC/VI: N = 751, 1.92%, ROR = 20.45, IC = 4.32), aphonia (BUD/GLY/FOR: N = 52, 0.32%, ROR = 13.64, IC = 3.75; FF/UMEC/VI: N = 116, 0.30%, ROR = 12.65, IC = 3.64). FF/UMEC/VI also had risks of vocal cord dysfunction (N = 10, 0.026%, ROR = 16.28, IC = 4.00), paranasal sinus inflammation (N = 4, 0.010%, ROR = 18.42, IC = 4.17), increased viscosity of bronchial secretion (N = 6, 0.015%, ROR = 15.89, IC = 3.96), which were not present in BUD/GLY/FOR. On Gastrointestinal disorders, the PTs common to both drugs were oral mucosal exfoliation (BUD/GLY/FOR: N = 3, 0.018%, ROR = 10.06, IC = 3.32; FF/UMEC/VI: N = 3, 0.0076%, ROR = 3.67, IC = 1.87). Coated in mouth (N = 14, 0.036%, ROR = 33.74, IC = 5.01) and tongue coated (N = 16, 0.041%, ROR = 19.38, IC = 4.24) were the top ten PTs with IC values unique to FF/UMEC/VI.
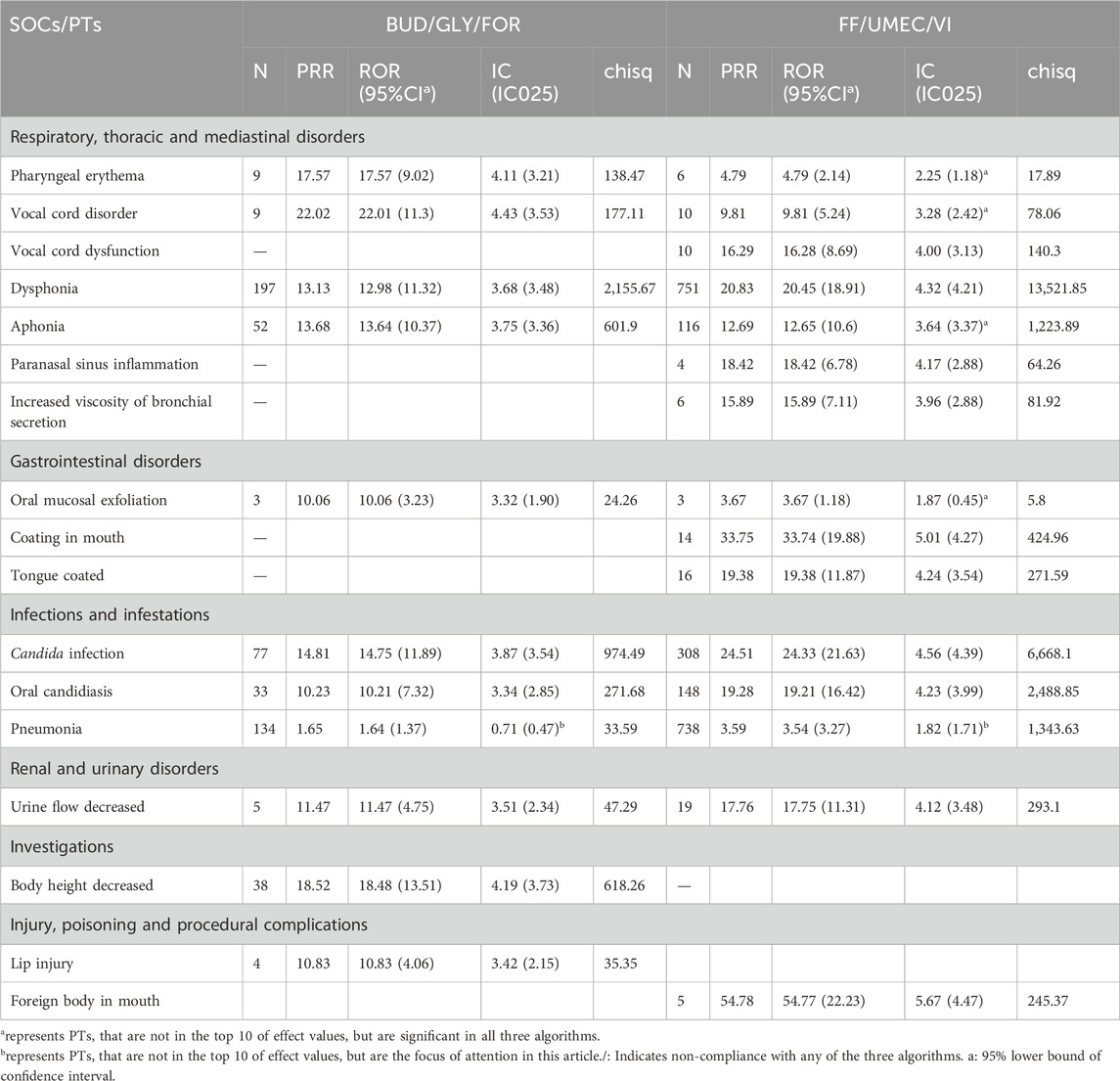
Table 4. BUD/GLY/FOR and FF/UMEC/VI AE signal strength reporting at preferred term (PT) levels.
In Infections and infestations, candida infection (BUD/GLY/FOR: N = 77, 0.47%, ROR = 14.75, IC = 3.87; FF/UMEC/VI: N = 308, 0.79%, ROR = 24.33, IC = 4.56) and oral candidiasis (BUD/GLY/FOR: N = 33, 0.20%, ROR = 10.21, IC = 3.34; FF/UMEC/VI: N = 148, 0.38%, ROR = 19.21, IC = 4.23) are PTs common to both drugs. In addition, the effects of pneumonia (not in the top 10, but we were interested) were (BUD/GLY/FOR: N = 134, 0.82%, ROR = 1.64, IC = 0.71; FF/UMEC/VI: N = 738, 1.89%, ROR = 3.54, IC = 1.82), respectively. Urine flow decreased (BUD/GLY/FOR: N = 5, 0.031%, ROR = 11.47, IC = 3.54; FF/UMEC/VI: N = 19, 0.049%, ROR = 17.75, IC = 4.12) belongs to the category of renal and urinary disorders, which is correlated in both drugs. In Investigations, BUD/GLY/FOR was associated with decreased height (N = 38, 0.23%, ROR = 18.48, IC = 4.19). In Injury, poisoning, and procedural complications, BUD/GLY/FOR has a PT for lip injury (N = 4, 0.024%, ROR = 10.83, IC = 3.42), while FF/UMEC/VI has a PT for foreign body in mouth (N = 16, 0.041%, ROR = 54.77, IC = 5.67). Supplementary Table S6 shows the number of AEs grouped by sex, age, and reporting countries at the PT level.
In addition, this research identified several PTs that had not previously received attention and existed outside the drug leaflets (DailyMed, 2024a; DailyMed, 2024b). Supplementary Table S7 showed the presence of BUD/GLY/FOR with hypoacusis (N = 62, 0.38%, ROR = 3.98, IC = 1.99). Supplementary Table S7 shows the presence of PTs in the vascular disorders category in FF/UMEC/VI, including arterial disorder (N = 4, 0.010%, ROR = 4.45, IC = 2.15), aneurysm (N = 11, 0.028%, ROR = 3.99, IC = 1.99), and arterial occlusive disease (N = 8, 0.020%, ROR = 2.12, IC = 1.08), and arteriosclerosis exists in BUD/GLY/FOR (N = 5, 0.031%, ROR = 2.42, IC = 0.12). There are PTs associated with malignancy in both FF/UMEC/VI and BUD/GLY/FOR.
In order to examine the changes in each signal over time, the present study was time-scanned for BUD/GLY/FOR and FF/UMEC/VI for pneumonia, dysphonia, oral candidiasis, aphonia, candida infection, body height decreased, urine, decreased, tongue coated, vocal cord disorder, and cancer. The results (Supplementary Figures S1, S2) showed unstable associations between pneumonia and BUD/GLY/FOR and unstable associations between cancer-related signals and FF/UMEC/VI and BUD/GLY/FOR. The associations of the other signals with drugs remained consistent across years.
DiscussionTo our knowledge, there are few previous articles analyzing the AE of single inhaler triple-therapy drugs. Respiratory, thoracic and mediastinal disorders, injury, poisoning and procedural complications, and eye disorders were the SOCs for which the two drugs fit the study algorithm. Device use problems are common and well-known PTs for both drugs, with BUD/GLY/FOR having a significantly higher rate of device use problems than FF/UMEC/VI. After excluding PTs for substance use problems and treatment of disease, we screened a total of 17 PTs from 7 SOCs based on the top 10 highest ICs for each drug. We also analyzed pneumonia, an important PT, in both drugs. In addition, a number of PTs that are uncommon and exist outside of the drug leaflets are included in the discussion.
BUD/GLY/FOR and FF/UMEC/VI are essential medications for COPD, with common AEs stemming from the drug itself and the form of administration. In the SOCs of injury, poisoning, and procedural complications, device use issues were common to both medications for the PT. There have been few comparative studies analyzing BUD/GLY/FOR and FF/UMEC/VI on device use issues. We found through our research that BUD/GLY/FOR had a higher incidence of equipment use problems compared to FF/UMEC/VI. BUD/GLY/FOR uses a pressurized metered-dose inhaler (pMDI). This inhaler requires hand pressure to test the patient’s hand-mouth coordination and can easily compromise efficacy due to improper handling. The dry powder inhaler (DPI) of FF/UMEC/VI is relatively simple to operate. In addition to the operation of the device, the pulmonary deposition rate of the drug cannot be ignored. The pMDI of BUD/GLY/FOR utilizes a co-suspension delivery technique that is less susceptible to delivery variability and therefore may have better lung deposition rates (Dunn et al., 2020). Usmani et al. found by computerized respiratory imaging that BUD/GLY/FOR had significantly higher drug deposition in small and large airways than FF/UMEC/VI (Usmani et al., 2023). It is necessary to choose the inhaler according to the patient’s characteristics and usage habits.
Since both drugs are inhaled from the mouth via the wrapping of the lips, they then pass through the pharynx into the lungs. Any body part in the pathway could come into contact with the drug, resulting in an adverse event. Our study identified multiple PTs in three SOCs affected by the drug inhalation pathway, including respiratory, thoracic and mediastinal disorders (laryngeal, vocal folds, and voice-related PT), gastrointestinal disorders (Oral mucosal exfoliation, coating in the mouth, and tongue coated) and injury, poisoning and procedural complications (lip injury and foreign body in mouth). The above PTs may be associated with mucosal damage to the mouth, tongue, vocal cords, and other areas caused by ICS use (Rachelefsky et al., 2007; Ozbilen et al., 2010). However, these PTs do not usually result in discontinuation of therapy (Yang et al., 2023). It may reduce the incidence of associated PTs by urging patients to rinse their mouths promptly after inhalation of medications and to reduce swallowing.
Infection is a category of adverse events that cannot be ignored in BUD/GLY/FOR and FF/UMEC/VI. Regarding infections and infestations, we found that the proportions and effect sizes of oral Candida infections were significantly greater in FF/UMEC/VI than in BUD/GLY/FOR. This finding fits with the study of Dekuijzen et al., who found that oral Candida infections were less likely to occur in BUD/GLY/FOR (Dekhuijzen et al., 2016). Few previous studies have compared the risk of pneumonia with three inhalations of a drug, so we focused on the outcomes of pneumonia across the two drugs. The results showed that there was a risk of pneumonia with both drugs, with BUD/GLY/FOR having a much smaller risk of pneumonia than FF/UMEC/VI. Pneumonia risk was significantly and positively correlated with ICS use (Rønn et al., 2023). Similar to our findings, previous studies have found that patients receiving budesonide/formoterol have a substantially lower risk of pneumonia than those receiving fluticasone/salmeterol (Janson et al., 2013; Yang et al., 2017). However, a meta-analysis showed no relevant difference in the risk of pneumonia between FF/UMEC/VI and BDP/FOR/GLY (Rogliani et al., 2022).
FF/UMEC/VI and BUD/GLY/FOR had a higher risk for two categories of SOCs, vascular disease, and neoplasms, not seen in drug leaflets or previous studies. Regarding vascular disorders, PTs with arterial disorders, aneurysms, and arterial occlusive disease were seen in FF/UMEC/VI, while the PT with atherosclerosis was seen in BUD/GLY/FOR, and the reason for this association is unclear. A previous meta-analysis showed no significant difference in cardiovascular risk between the two drugs (Rogliani et al., 2022). Our study found lung cancer-associated AEs in both FF/UMEC/VI and BUD/GLY/FOR users. In addition to lung cancer PT, thoracic cancer and brain neoplasm malignant have also been found to be associated with FF/UMEC/VI. However, the results of the time-scan plots showed that the correlation between BUD/GLY/FOR and FF/UMEC/VI and tumor was unstable across years. BUD/GLY/FOR and FF/UMEC/VI have not been reported to increase tumor risk in past large clinical trials and meta-analyses (Lipson et al., 2020; Ferguson et al., 2018; Heo, 2021; Bourdin et al., 2021). Therefore, we believe that we cannot link FF/UMEC/VI and BUD/GLY/FOR to tumor-associated PTs and that it may be the chronic inflammation of asthma or COPD that contributes to tumorigenesis.
In BUD/GLY/FOR, body height decreased is the PT that exists outside of the drug leaflets. We speculated that BUD/GLY/FOR may affect the height development of minors. Pedersen found that although budesonide affects growth rates in the first few years of treatment, children can eventually reach normal adult height (Agertoft and Pedersen, 2000). However, a meta-analysis found that adolescent patients treated with budesonide 400 μg/d for an average of 4.3 years had a mean reduction in height of 1.20 cm (Zhang et al., 2014). Another study noted that fluticasone at the same dose was less inhibitory to growth than budesonide (Axelsson et al., 2019). Supplementary Table S6 analyzes the number of occurrences of body height decreased in BUD/GLY/FOR in different age groups. Unfortunately, we cannot conclude that BUD/GLY/FOR affects the height of minors due to the fact that most of the age data are missing. The relationship between BUD/GLY/FOR and height loss needs to be further substantiated. Hypoacusis is also an uncommon AE for BUD/GLY/FOR, suggesting that BUD/GLY/FOR may affect the auditory system.
The study is a pharmacovigilance analysis based on the FDA’s Adverse Event Reporting System, which is characterized by data derived from the real world. However, there are undeniable limitations to this study. First, relying on reports initiated by patients, physicians, and pharmaceutical companies to the FDA may result in underreporting and inaccuracy of specific adverse events. Second, patients and professionals report different accuracies resulting in the possibility that some AEs may be inaccurate, which leads to some bias in the results. Thus, there are areas for improvement at the data level of uncertainty of causality and duplication of reporting (Yu et al., 2021). Third, the study could not be cross-analyzed with other drugs, which may also have caused some bias. In addition, some relevant information, such as age and sex, was missing from the data, which affected the accuracy of further subgroup analysis. Finally, due to the lack of data related to the drug beclomethasone dipropionate/formoterol fumarate/glycopyrronium bromide in the database, we compared only the drugs BUD/GLY/FOR and FF/UMEC/VI. These limitations should be considered when making clinical management and decisions regarding pharmacovigilance data for BUD/GLY/FOR and FF/UMEC/VI.
ConclusionOur study found that the most common AEs present on the drug leaflets for BUD/GLY/FOR and FF/UMEC/VI included device use issues, multiple pharyngeal problems, pneumonia, candida infections, and urinary retention. Of these, the risk of pneumonia and candida infection was higher for FF/UMEC/VI than for BUD/GLY/FOR, and the risk of AEs associated with device use issues was higher for BUD/GLY/FOR than for FF/UMEC/VI. Outside of the drug leaflets, both drugs were associated with a higher risk of AEs in vascular disorders, and BUD/GLY/FOR group had a higher risk of AEs in body height decreased and hypoacusis. Our study provides valuable insights into the safety of the clinical use of BUD/GLY/FOR and FF/UMEC/VI, and clinicians should remain vigilant for potential AEs.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributionsZR: Conceptualization, Methodology, Software, Visualization, Writing–original draft. SY: Data curation, Software, Writing–review and editing. YF: Data curation, Software, Writing–review and editing. BX: Data curation, Methodology, Writing–review and editing. XC: Methodology, Writing–review and editing. DL: Conceptualization, Methodology, Writing–original draft. QM: Conceptualization, Funding acquisition, Methodology, Writing–review and editing.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the National Natural Science Foundation of China (82074422), Science and technology Innovation Project of China Academy of Chinese Medical Sciences (CI2021A01101), and National Public Hospital Reform and High-quality Development Demonstration Project (Haidian District, Beijing) (11010822T000001740154).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2024.1460407/full#supplementary-material
SUPPLEMENTARY FIGURE S1 | Information components of BUD/GLY/FOR and FF/UMEC/VI over time in AEs with top ten IC values.
SUPPLEMENTARY FIGURE S2 | Information components of BUD/GLY/FOR and FF/UMEC/VI over time in tumor-related AEs.
ReferencesAgertoft, L., and Pedersen, S. (2000). Effect of long-term treatment with inhaled budesonide on adult height in children with asthma. N. Engl. J. Med. 343 (15), 1064–1069. doi:10.1056/NEJM200010123431502
PubMed Abstract | CrossRef Full Text | Google Scholar
Axelsson, I., Naumburg, E., Prietsch, S. O., and Zhang, L. (2019). Inhaled corticosteroids in children with persistent asthma: effects of different drugs and delivery devices on growth. Cochrane Database Syst. Rev. 6 (6), CD010126. doi:10.1002/14651858.CD010126.pub2
PubMed Abstract | CrossRef Full Text | Google Scholar
Bourdin, A., Molinari, N., Ferguson, G. T., Singh, B., Siddiqui, M. K., Holmgren, U., et al. (2021). Efficacy and safety of budesonide/glycopyrronium/formoterol fumarate versus other triple combinations in COPD: a systematic literature review and network meta-analysis. Adv. Ther. 38 (6), 3089–3112. doi:10.1007/s12325-021-01703-z
PubMed Abstract | CrossRef Full Text | Google Scholar
Brown, E. G. (2003). Methods and pitfalls in searching drug safety databases utilising the Medical Dictionary for Regulatory Activities (MedDRA). Drug Saf. 26 (3), 145–158. doi:10.2165/00002018-200326030-00002
PubMed Abstract | CrossRef Full Text | Google Scholar
Dekhuijzen, P. N. R., Batsiou, M., Bjermer, L., Bosnic-Anticevich, S., Chrystyn, H., Papi, A., et al. (2016). Incidence of oral thrush in patients with COPD prescribed inhaled corticosteroids: effect of drug, dose, and device. Respir. Med. 120, 54–63. doi:10.1016/j.rmed.2016.09.015
PubMed Abstract | CrossRef Full Text | Google Scholar
Dransfield, M. T., Crim, C., Criner, G. J., Day, N. C., Halpin, D. M. G., Han, M. K., et al. (2021). Risk of exacerbation and pneumonia with single-inhaler triple versus dual therapy in IMPACT. Ann. Am. Thorac. Soc. 18 (5), 788–798. doi:10.1513/AnnalsATS.202002-096OC
PubMed Abstract | CrossRef Full Text | Google Scholar
Dunn, L. J., Kerwin, E. M., DeAngelis, K., Darken, P., Gillen, M., and Dorinsky, P. (2020). Pharmacokinetics of budesonide/glycopyrrolate/formoterol fumarate metered dose inhaler formulated using co-suspension delivery technology after single and chronic dosing in patients with COPD. Pulm. Pharmacol. Ther. 60, 101873. doi:10.1016/j.pupt.2019.101873
PubMed Abstract | CrossRef Full Text | Google Scholar
Feagins, L. A., Abdelsayed, G. G., and Schairer, J.FDA-Related Matters Committee of the American College of Gastroenterology (2019). Reporting adverse drug events. Am. J. Gastroenterol. 114 (9), 1411–1413. doi:10.14309/ajg.0000000000000374
PubMed Abstract | CrossRef Full Text | Google Scholar
Ferguson, G. T., Darken, P., Ballal, S., Siddiqui, M. K., Singh, B., Attri, S., et al. (2020). Efficacy of budesonide/glycopyrronium/formoterol fumarate metered dose inhaler (bgf mdi) versus other inhaled corticosteroid/long-acting muscarinic antagonist/long-acting β2-agonist (ICS/LAMA/LABA) triple combinations in COPD: a systematic literature review and network meta-analysis. Adv. Ther. 37 (6), 2956–2975. doi:10.1007/s12325-020-01311-3
PubMed Abstract | CrossRef Full Text | Google Scholar
Ferguson, G. T., Rabe, K. F., Martinez, F. J., Fabbri, L. M., Wang, C., Ichinose, M., et al. (2018). Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, phase 3 randomised controlled trial. Lancet Respir. Med. 6 (10), 747–758. doi:10.1016/S2213-2600(18)30327-8
PubMed Abstract | CrossRef Full Text | Google Scholar
Ismaila, A. S., Haeussler, K., Czira, A., Youn, J. H., Malmenäs, M., Risebrough, N. A., et al. (2022). Fluticasone furoate/umeclidinium/vilanterol (FF/UMEC/VI) triple therapy compared with other therapies for the treatment of COPD: a network meta-analysis. Adv. Ther. 39 (9), 3957–3978. doi:10.1007/s12325-022-02231-0
PubMed Abstract | CrossRef Full Text | Google Scholar
Janson, C., Larsson, K., Lisspers, K. H., Ställberg, B., Stratelis, G., Goike, H., et al. (2013). Pneumonia and pneumonia related mortality in patients with COPD treated with fixed combinations of inhaled corticosteroid and long acting β2 agonist: observational matched cohort study (PATHOS). BMJ 346, f3306. doi:10.1136/bmj.f3306
PubMed Abstract | CrossRef Full Text | Google Scholar
Javed, F., and Kumar, A. (2024). Identification of signal of clindamycin associated renal failure acute: a disproportionality analysis. Curr. Drug Saf. 19 (1), 123–128. doi:10.2174/1574886318666230228142856
PubMed Abstract | CrossRef Full Text | Google Scholar
Kendall, R., Martin, A. A., Shah, D., Shukla, S., Compton, C., and Ismaila, A. S. (2023). Cost-effectiveness of single-inhaler triple therapy (FF/UMEC/VI) versus tiotropium monotherapy in patients with symptomatic moderate-to-very severe COPD in the UK. Int. J. Chron. Obstruct Pulmon Dis. 18, 1815–1825. doi:10.2147/COPD.S400707
PubMed Abstract | CrossRef Full Text | Google Scholar
Lee, H. W., Park, J., Jo, J., Jang, E. J., and Lee, C. H. (2019). Comparisons of exacerbations and mortality among regular inhaled therapies for patients with stable chronic obstructive pulmonary disease: systematic review and Bayesian network meta-analysis. PLoS Med. 16 (11), e1002958. doi:10.1371/journal.pmed.1002958
PubMed Abstract | CrossRef Full Text | Google Scholar
Lee, L. A., Bailes, Z., Barnes, N., Boulet, L. P., Edwards, D., Fowler, A., et al. (2021). Efficacy and safety of once-daily single-inhaler triple therapy (FF/UMEC/VI) versus FF/VI in patients with inadequately controlled asthma (CAPTAIN): a double-blind, randomised, phase 3A trial. Lancet Respir. Med. 9 (1), 69–84. doi:10.1016/S2213-2600(20)30389-1
PubMed Abstract | CrossRef Full Text | Google Scholar
Lipson, D. A., Barnhart, F., Brealey, N., Brooks, J., Criner, G. J., Day, N. C., et al. (2018). Once-Daily single-inhaler triple versus dual therapy in patients with COPD. N. Engl. J. Med. 378 (18), 1671–1680. doi:10.1056/NEJMoa1713901
PubMed Abstract | CrossRef Full Text | Google Scholar
Lipson, D. A., Crim, C., Criner, G. J., Day, N. C., Dransfield, M. T., Halpin, D. M. G., et al. (2020). Reduction in all-cause mortality with fluticasone furoate/umeclidinium/vilanterol in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 201 (12), 1508–1516. doi:10.1164/rccm.201911-2207OC
PubMed Abstract | CrossRef Full Text | Google Scholar
Mannino, D., Bogart, M., Wu, B., Germain, G., Laliberté, F., MacKnight, S. D., et al. (2022). Adherence and persistence to once-daily single-inhaler versus multiple-inhaler triple therapy among patients with chronic obstructive pulmonary disease in the USA: a real-world study. Respir. Med. 197, 106807. doi:10.1016/j.rmed.2022.106807
PubMed Abstract | CrossRef Full Text | Google Scholar
Martinez, F. J., Rabe, K. F., Ferguson, G. T., Wedzicha, J. A., Singh, D., Wang, C., et al. (2021). Reduced all-cause mortality in the ethos trial of budesonide/glycopyrrolate/formoterol for chronic obstructive pulmonary disease. A randomized, double-blind, multicenter, parallel-group study. Am. J. Respir. Crit. Care Med. 203 (5), 553–564. doi:10.1164/rccm.202006-2618OC
PubMed Abstract | CrossRef Full Text | Google Scholar
Matera, M. G., Calzetta, L., Rogliani, P., Hanania, N., and Cazzola, M. (2024). Cardiovascular events with the use of long-acting muscarinic receptor antagonists: an analysis of the FAERS database 2020-2023. Lung 202, 119–125. doi:10.1007/s00408-024-00677-3
PubMed Abstract | CrossRef Full Text | Google Scholar
Ozbilen, A. G., Uzun Adatepe, N., Kaytaz, A., Edizer, D. T., Gemicioglu, B., Yagiz, C., et al. (2010). Evaluation of laryngeal findings in users of inhaled steroids. Eur. Arch. Otorhinolaryngol. 267 (6), 917–923. doi:10.1007/s00405-009-1141-2
PubMed Abstract | CrossRef Full Text | Google Scholar
Paly, V. F., Vallejo-Aparicio, L. A., Martin, A., Izquierdo, J. L., Riesco, J. A., Soler-Cataluña, J. J., et al. (2022). Cost-effectiveness of once-daily single-inhaler COPD triple therapy in Spain: IMPACT trial. Int. J. Chron. Obstruct Pulmon Dis. 17, 3097–3109. doi:10.2147/COPD.S366765
PubMed Abstract | CrossRef Full Text | Google Scholar
Rachelefsky, G. S., Liao, Y., and Faruqi, R. (2007). Impact of inhaled corticosteroid-induced oropharyngeal adverse events: results from a meta-analysis. Ann. Allergy Asthma Immunol. 98 (3), 225–238. doi:10.1016/S1081-1206(10)60711-9
PubMed Abstract | CrossRef Full Text | Google Scholar
Rogliani, P., Ora, J., Cavalli, F., Cazzola, M., and Calzetta, L. (2022). Comparing the efficacy and safety profile of triple fixed-dose combinations in COPD: a meta-analysis and IBiS score. J. Clin. Med. 11 (15), 4491. doi:10.3390/jcm11154491
PubMed Abstract | CrossRef Full Text | Google Scholar
Rønn, C., Sivapalan, P., Eklöf, J., Kamstrup, P., Biering-Sørensen, T., Bonnesen, B., et al. (2023). Hospitalization for chronic obstructive pulmonary disease and pneumonia: association with the dose of inhaled corticosteroids. A nation-wide cohort study of 52 100 outpatients. Clin. Microbiol. Infect. 29 (4), 523–529. doi:10.1016/j.cmi.2022.11.029
PubMed Abstract | CrossRef Full Text | Google Scholar
Sakaeda, T., Tamon, A., Kadoyama, K., and Okuno, Y. (2013). Data mining of the public version of the FDA adverse event reporting system. Int. J. Med. Sci. 10 (7), 796–803. doi:10.7150/ijms.6048
PubMed Abstract | CrossRef Full Text | Google Scholar
Sharma, A., and Kumar, A. (2022). Identification of novel signal of clobazam-associated drug reaction with eosinophilia and systemic symptoms syndrome: a disproportionality analysis. Acta Neurol. Scand. 146 (5), 623–627. doi:10.1111/ane.13690
PubMed Abstract | CrossRef Full Text | Google Scholar
Silberstein, S. D., Reshef, S., Cohen, J. M., Gandhi, S., Seminerio, M., Ramirez Campos, V., et al. (2023). Adverse events reported with therapies targeting the cgrp pathway during the first 6 Months post-launch: a retrospective analysis using the FDA adverse events reporting system. Adv. Ther. 40 (2), 445–459. doi:10.1007/s12325-022-02346-4
PubMed Abstract | CrossRef Full Text | Google Scholar
Singh, J. (2015). International conference on harmonization of technical requirements for registration of pharmaceuticals for human use. J. Pharmacol. Pharmacother. 6 (3), 185–187. doi:10.4103/0976-500X.162004
PubMed Abstract | CrossRef Full Text | Google Scholar
Usmani, O., Li, G., De Backer, J., Sadafi, H., Wu, L., and Marshall, J. (2023). Modeled small airways lung deposition of two fixed-dose triple therapy combinations assessed with in silico functional respiratory imaging. Respir. Res. 24 (1), 226. doi:10.1186/s12931-023-02534-y
PubMed Abstract | CrossRef Full Text | Google Scholar
van Puijenbroek, E. P., Bate, A., Leufkens, H. G. M., Lindquist, M., Orre, R., and Egberts, A. C. G. (2002). A comparison of measures of disproportionality for signal detection in spontaneous reporting systems for adverse drug reactions. Pharmacoepidemiol Drug Saf. 11 (1), 3–10. doi:10.1002/pds.668
PubMed Abstract | CrossRef Full Text | Google Scholar
Virchow, J. C., Kuna, P., Paggiaro, P., Papi, A., Singh, D., Corre, S., et al. (2019). Single inhaler extrafine triple therapy in uncontrolled asthma (TRIMARAN and TRIGGER): two double-blind, parallel-group, randomised, controlled phase 3 trials. Lancet 394 (10210), 1737–1749. doi:10.1016/S0140-6736(19)32215-9
PubMed Abstract | CrossRef Full Text | Google Scholar
Yang, H. H., Lai, C. C., Wang, Y. H., Yang, W. C., Wang, C. Y., Wang, H. C., et al. (2017). Se
留言 (0)