Patients suffered from severe traumatic brain injury (sTBI, the list of abbreviations was shown in Table 1) usually require mechanical ventilation in the neurosurgical intensive care unit (ICU). Approximately 31.8% of patients in the TBI cohort have experienced tracheostomy, which is more frequent than patients in general ICU cohorts with rates of about 10% (1). As the state of unconsciousness is persistent, tracheostomy is commonly performed to maintain gas exchange to avoid hypoxemia and accelerate liberation from mechanical ventilation. With the stable airway access provided, the tracheostomy tube could also be convenient for suctioning (2). The main indications for tracheostomy in patients with sTBI include absence of protective airway reflexes, impairment of respiratory drive, prolonged mechanical ventilation, reduction of dead space to facilitate ventilatory weaning, and difficulties in managing secretions (1, 3). However, optimal timing for tracheostomy is still controversial.
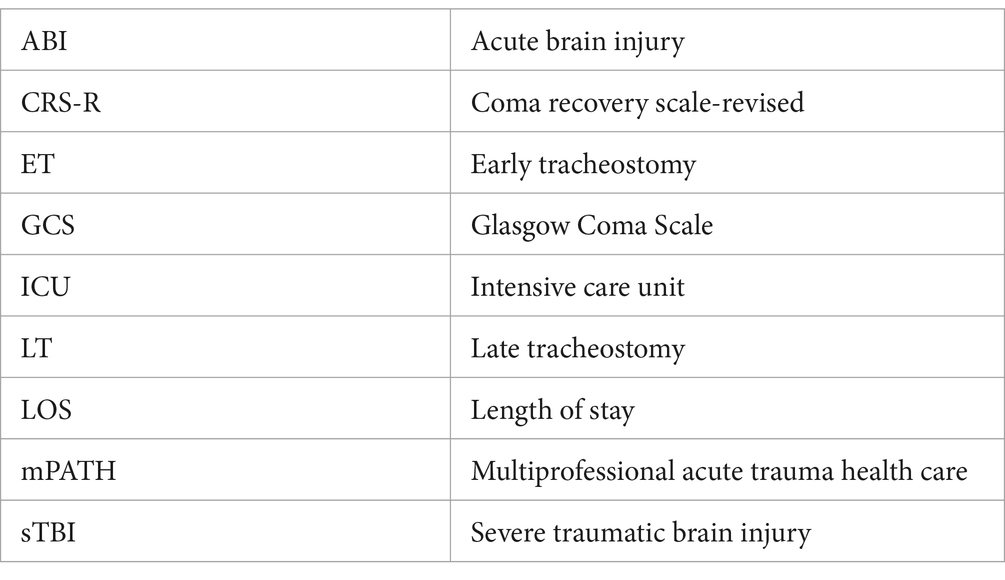
Table 1. List of abbreviations.
A safe and fast decannulation in tracheostomized patients with sTBI is considered as a main rehabilitative goal. However, there was substantial heterogeneity in tracheostomy care and decannulation practices among the different centers (4). In this study, we reviewed the effects of tracheostomy, tracheostomy timing, and decannulation timing to provide valuable information for clinicians. We further discussed the role of a multidisciplinary tracheostomy team, especially the nursing care protocol, in the clinical management of tracheostomized patients with sTBI.
The effects of tracheostomy on patients with sTBIIt has been reported that tracheostomy has advantages in improving outcomes of patients with sTBI compared with prolonged endotracheal intubation. Villemure-Poliquin N et al. (5) conducted a retrospective multicenter cohort study and examined the potential benefits of tracheostomy versus prolonged endotracheal intubation. Tracheostomy was shown to be associated with decreased 30-day mortality. The increased survival owing to tracheostomy was also confirmed by Stephen S et al. (6). Specifically, tracheostomy could comfort the patients by reducing oropharyngeal irritation, reducing sedative administration, and achieving more autonomy earlier (7). Besides, tracheostomy could decrease the risk of ventilator-associated pneumonia and ventilator-induced lung injury (8). Patients with long-term mechanical ventilation could also get positive weaning and shorter duration by tracheostomy. As an invasive procedure, tracheostomy would inevitably have risks for the airway, including tracheomalacia, hemorrhage, and tracheal stenosis (9). However, tracheostomy would still be recommended for sTBI patients when weighing the benefits and risks (10).
The timing of tracheostomy for patients with sTBIConventionally, tracheostomy is commonly used for patients with sTBI under the condition of Glasgow Coma Scale (GCS) score ≤ 8 and these who rely on a mechanical ventilator for more than 7 days (11, 12). According to the recommendations of the European Society of Intensive Care Medicine consensus (13), tracheostomy is strongly recommended in mechanically ventilated patients with acute brain injury (ABI) who have failed one or several trials of extubation. It should also be considered in mechanically ventilated patients with ABI who have persistently reduced consciousness levels (weak recommendation).
Although tracheostomy is generally indicated for patients with sTBI, the timing of tracheostomy for patients with sTBI is unclear (14). Tracheostomy is usually defined as early tracheostomy (ET, performed within 7 days of admission) or late tracheostomy (LT, performed more than 7 days after admission). A previous study classified ET and LT as tracheostomy performed ≤10 days and > 10 days after tracheal intubation, respectively (15). Another study defined ET and LT as tracheostomy performed ≤3 days and > 3 days after admission, respectively (16). The effects of early tracheostomy versus late tracheostomy have been explored. But the results are controversial. According to a retrospective, 15-year observational cohort study from January 1990 to December 2005, 3,277 patients with TBI were found to have a tracheostomy (17). The investigation indicated a relationship between tracheostomy timing and prognosis, and suggested that ET may lead to a better overall clinical outcome than LT. Similarly, Shibahashi K et al. (18) explored the performance of earlier tracheostomy (within 72 h of admission) and found a decrease in the duration of mechanical ventilation and length of stay (LOS) in patients with TBI, with acceptable mortality. Besides, a propensity-matched analysis on children’s patients with sTBI and a retrospective cohort study on adult patients both showed that ET was related with shorter hospital LOS and fewer complications (8, 19). Along with a decreased risk of pneumonia, a lower risk of deep venous thrombosis, and decubitus ulcer, a decreasing trend of pulmonary embolism was observed in ET. A lower incidence of gram-negative microorganism-related nosocomial pneumonia and shorter antibiotic duration use were also identified in ET (20). In a meta-analysis comparing ET and LT in sTBI or stroke, the mean time to tracheostomy in the ET cohort was 7.1 ± 0.00 days and 15.3 ± 0.01 days in the LT cohort. ET was shown to reduce the risk for ventilator-associated pneumonia and decrease mechanical ventilation duration in ICU and hospital LOS (21). Another meta-analysis comparing ET and LT in sTBI displayed similar results (10). However, a recent US national analysis showed that mortality was slightly higher in ET than in LT, while other benefits from ET notably existed (22). Villemure-Poliquin N et al. (5) revealed no effect on mortality was observed when comparing ET and LT. Relevant studies on time to tracheostomy in patients with severe TBI in Table 2.
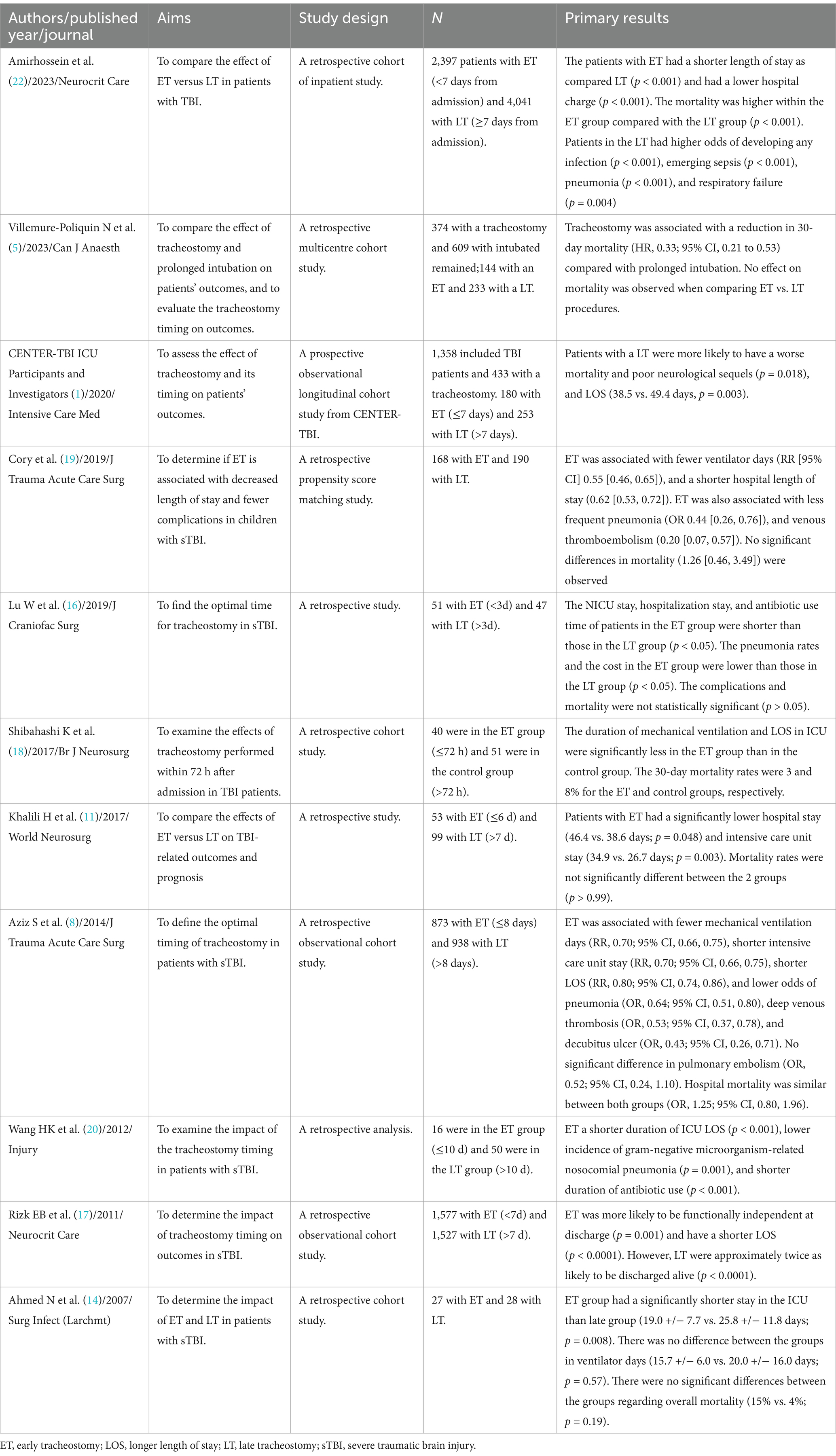
Table 2. Studies on time to tracheostomy in patients with severe TBI.
In general, priority seems to be given to ET for patients with sTBI rather than delayed tracheostomy or LT. However, high-quality evidence is lacking. In 2020, an international consensus panel attempted to provide a recommendation regarding the optimal timing of tracheostomy in patients with ABI. But they failed due to contradictory and low-quality evidence (13). Following that, results from CENTER-TBI as a prospective observational longitudinal cohort study on patients with TBI were reported (1). The study demonstrated that LT was more likely to have a worse neurological outcome, poor neurological sequels, and longer LOS. Due to various tracheostomy timing, different brain injury severity, and a mix of isolated brain injury versus multiple injury, there was a broad variability in current studies. Standardized comparisons are needed in future research. Given the variable indications for mechanical ventilation and the different underlying lung mechanics in patient subgroups, more detailed information is needed to implement guidelines (23).
The timing of decannulation for patients with sTBIThe majority of patients with tracheostomy who survive to hospital discharge could be successfully decannulated (24). An early decannulation could avoid secondary complications, such as respiratory infections and airway obstructions, to improve clinical outcomes and facilitate the recovery (25). However, the indications and optimal time for decannulation remain unclear. According to a systematic scoping review on critically ill patients in mixed ICU, the assessment criterion differed as informed consent, clinical stability, airway patency, physiological decannulation, swallowing assessment, consciousness level, effectiveness of cough, and clearance of secretions (26). However, it would not be adequate for patients with sTBI. Because patients with sTBI are usually in a coma, and the ability of self-body control and executing simple voluntary tasks are lost.
Weaning protocols are difficult for decision-making. There are numerous and confounding factors to judge. For example, common comorbidities such as diabetes and acute kidney injury would influence the chances for decannulation in patients with sTBI (27). Despite that, identifying efficient factors for time to decannulation is essential for safe weaning. It is reported that the predictive factors for safe removal of the tracheal tube in patients with ABI including high neurological status, TBI rather than stroke or anoxic brain lesions, younger age, effective swallowing, an effective cough, and the absence of pulmonary infections (28). Independent breathing and airway protection may indicate successful decannulation in patients with sTBI. Perin C et al. (29) found that mean expiratory pressure, spontaneous cough, and cough strength were positive predictors of tracheostomy tube removal. However, in a decannulation study on 74 patients with ABI, airway patency, cough reflex test, SpO2, and GCS ≥ 8 showed high specificity but low sensitivity (30). Shrestha KK et al. also proposed that consciousness level based on GCS score was not significant in successful decannulation (31). Meanwhile, a higher coma recovery scale-revised (CRS-R) score was suggested to accurately evaluate the state of consciousness, which was demonstrated to be associated with a higher probability of decannulation (32). Thus, accurate parameters for accessing consciousness need to be used for studies on decannulation indications in depth.
Several methods have been observed to contribute to successful decannulation. Lanini B et al. (33) emphasized the roles of flexible bronchoscopy and thought it would guide successful tracheostomy weaning. Zanata Ide L et al. (34) thought that phonation and coughing were helpful for early tracheal decannulation in 20 patients with TBI. Moreover, the swallowing ability was verified in a retrospective study with a Danish population of 324 participants. Eskildsen SJ et al. (35) found that an improvement in swallowing ability during the initial 4 weeks of rehabilitation was associated with an 8.2-day reduction in time to decannulation. This study concluded that swallowing ability is a potentially significant factor with reduced time to decannulation. Relevant studies on time to decannulation in patients with severe TBI in Table 3. In general, the clinical criteria for tracheostomy decannulation in patients with sTBI included: (1) toleration of tracheostomy tube capping for 72 h (36); (2) Absence of severe dysphagia, defined as the ability to manage secretions (37); (3) endoscopic patency of airways (lumen diameter > 50%) (38); (4) swallowing instrumental assessment (penetration assessment scale 5, no aspiration events); and (5) blue dye test (absence of blue traces) (30).
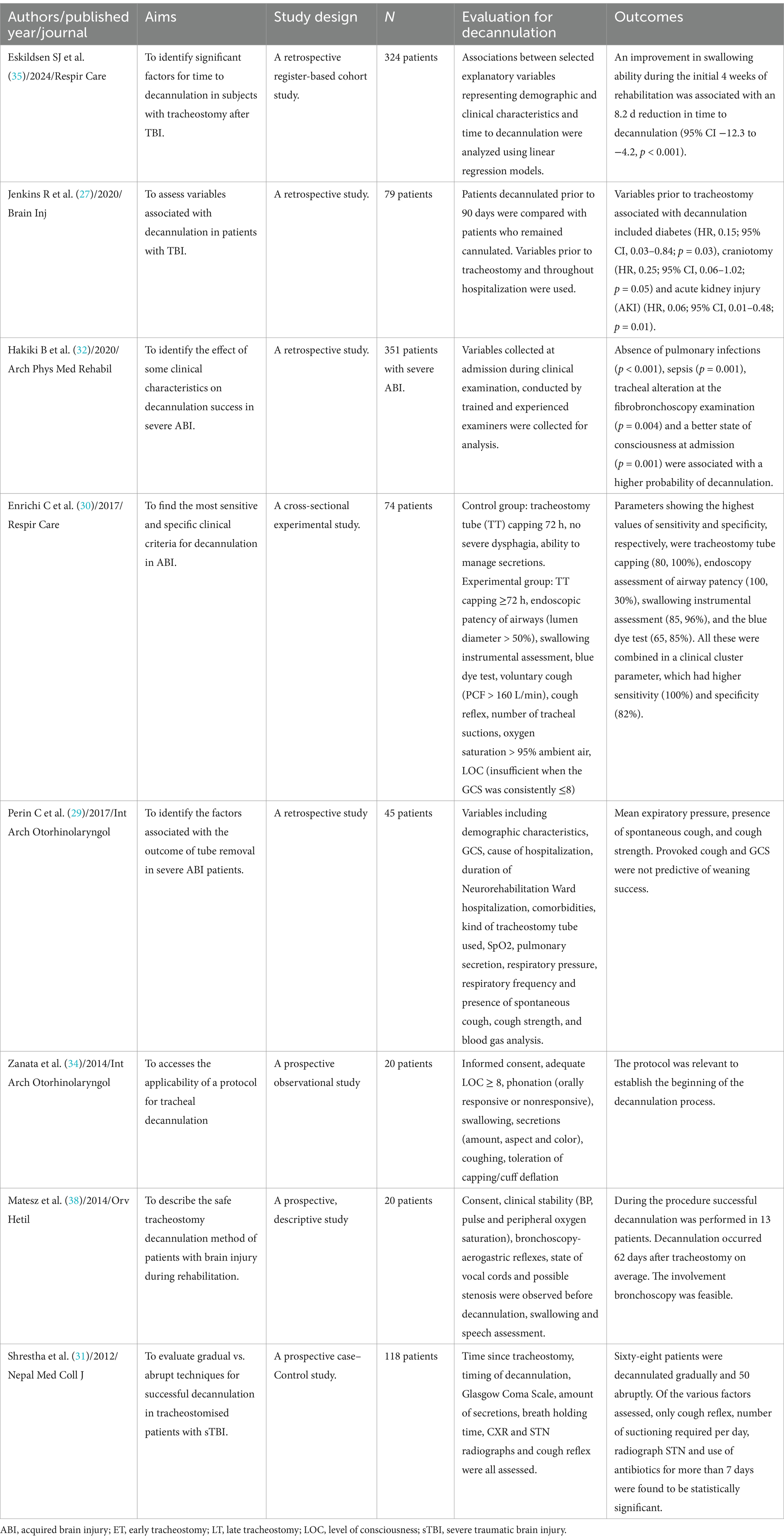
Table 3. Studies on time to decannulation in patients with severe TBI.
Multidisciplinary tracheostomy teamInadequate tracheostomy timing, nursing care, and unsafe decannulation would lead to complications, such as aggravated pneumonia, prolonged intubation, or induced paroxysmal sympathetic hyperactivity (39). Therefore, a multidisciplinary team trained and qualified is essential. Patients would benefit from a specialized multidisciplinary tracheostomy team. LeBlanc J et al. (40) retrospectively compared the effect of a multidisciplinary tracheostomy team from 27 patients before implementation of the tracheostomy team approach and 34 patients followed by the team. The team comprised trauma surgeons and residents, respiratory therapists, speech-language pathologists, and clinical nurse specialists. The results suggested that patients in the multidisciplinary group had a significantly shorter LOS and decreased time to decannulation. Based on research in the Level I trauma center of Carolinas Medical Center of America, Alvin et al. (41) investigated whether the multidisciplinary team would decrease LOS. The team was called a dedicated multiprofessional acute trauma health care (mPATH) team, consisting of a physical, occupational, speech, and respiratory therapist, nurse navigator, social worker, advanced care provider, and physician. They retrospectively compared the patients in the year before the mPATH team was established (n = 60) to those in the first full year following the team implementation (n = 70). As the primary endpoint, LOS obviously decreased due to the successful team. Meanwhile, a cost savings of US $11,238 per index hospitalization was observed. Thirty-day readmission and mortality rates had no significant change. Hence, the involvement of a multidisciplinary team is feasible during the entire hospitalization from tracheostomy to decannulation. However, it should be noted that the population sample size of the above study is limited, and more prospective research evidence is needed.
Nursing careIn a recent methodological study conducted in a public hospital in the city of Belém in Brazil (42), 34 nursing professionals participated in this survey. Developed through two phases: (I) target audience characterization and (II) technology development, and guided by the 5W2H management tool: 1 – What; 2 – Who; 3 – When; 4 – Where; 5 – Why; 1 – How; 2 – How Much, investigators thought the educational demands and continuing health education, with an emphasis on standardizing care through a protocol, were important for critical patients with tracheostomy. Although the study was limited by the lack of content validity by expert judges, appearance validity by design judges, semantic validity by the target audience, and usability assessment, clinical significance may truly exist. Because they appealed that care protocols and educational technologies were effective tools to address inconsistent topics in assisting patients with tracheostomy in NICU. A cross-sectional descriptive study involving a self-administered questionnaire conducted in a tertiary medical center in Saudi Arabia also recommended continuous training and competency evaluation for delivering optimal nursing care (43).
Tracheostomy is an invasive procedure and requires the participation of specialized multidisciplinary tracheostomy team collaboration (44). Among those, if the nursing work is not in place, various complications could arise, and the clinical prognosis would be affected. Hence, evidence-based nursing for patients with tracheostomy is beneficial to form standardized practices and prevent complications (45).
According to our experience, an individualized and feasible respiratory care plan should be developed by the supervising nurse based on the patient’s condition. Firstly, different body postures should be used for patients with different disease conditions. For example, patients with irritating cough should be given a semi-recumbent position. Secondly, the suction method should be adjusted based on coughing and changes in airway pressure. The appropriate suction tube should be selected, and airway patency should be ensured. Each suction time should be approximately 15 s to prevent situations such as hypoxia and suffocation caused by prolonged suction. Thirdly, attention should be paid to airway humidification. After tracheostomy, the patient’s respiratory tract is in direct contact with air. Therefore, sodium chloride solution should be used for humidification. Simultaneously, a tracheostomy mask could be used to achieve a humidification effect. The gas could be humidified and filtered to protect the tracheal mucosa. Finally, complication care for stoma is important. Nurses should strengthen nursing patrols, check the incision, and prevent infection. The incision needs to be kept clean, the tracheal cuff should be replaced promptly, and disinfected with alcohol or iodine solution. Observe the incision for secretions, collect and culture bacteria, and use sensitive antibiotics to prevent infection.
DiscussionTracheostomy and its decannulation are common procedures for patients with sTBI. Although ET is mostly reported to be associated with decreased LOS and fewer complications, mortality remains controversial. The different outcomes reported in different studies are likely associated with the various patient models used. Evaluations for ET or LT are more effective when considering 7 days as a cut-off point. Further investigation into standardized patient models could provide more precise insights into the optimal timing for tracheostomy and improve patient outcomes across diverse clinical settings. In addition, the current evidence on protocols for the assessment of tracheostomy decannulation is inadequate. Most recommendations are insufficient due to time bias, population bias, or the small sample size owing to the nature of the study. With the results from CENTER-TBI proving that ET can improve patient outcomes, more prospective randomized controlled trials exploring the timing of tracheostomy and decannulation are warranted to provide clinical guidelines.
The multidisciplinary tracheostomy care is important and its scope is expanding in order to manage the complex needs and expectations of tracheostomy patients. Initiatives such as the Global Tracheostomy (Quality Improvement) Collaborative have the potential to collect meaningful patient-level data around the quality of care delivered (46). Quality improvement programs such as this can deliver data that are relevant to patients and their families, multidisciplinary health care professionals and also hospital administrators that can comprehensively benchmark the effectiveness of multidisciplinary tracheostomy care in the future (47). Even when overlapping with other roles from the multidisciplinary team, specialist nursing programs including continuous training and competency evaluation have been shown to be a cost-effective method of improving hospital-wide tracheostomy care.
There are some limitations in this review. Firstly, the included literatures were relatively insufficient. Several researches published before 2000 years were ruled out. And only English literature has been adopted. Articles in other languages such as Chinese, German, and French were not available. Secondly, we only focused on the results and conclusions of the existing research, and did not further analyze the data of the study comprehensively. In addition, the evidence of the multidisciplinary tracheostomy team and nursing care were not powerful. Therefore, some insights may be controversial.
ConclusionAn ET performed within 7 days of admission in TBI patients could increase the opportunity of patient’s early rehabilitation. The toleration of tracheostomy tube capping, the ability to manage secretions, the endoscopic patency of airways, the swallowing ability, and the blue dye test may be potentially factors for early decannulation decision-making. A multidisciplinary tracheostomy team with specialist nursing care is crucial to improve clinical outcomes and prevent complications.
Author contributionsXM: Writing – original draft, Writing – review & editing. YuZ: Writing – original draft, Writing – review & editing. QC: Investigation, Writing – original draft, Writing – review & editing. YeZ: Conceptualization, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from the Scientific Research Program of Wuxi Health Commission (No. Q202209) to Yelei Zhang.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes References1. Robba, C, Galimberti, S, Graziano, F, Wiegers, EJA, Lingsma, HF, Iaquaniello, C, et al. Tracheostomy practice and timing in traumatic brain-injured patients: a CENTER-TBI study. Intensive Care Med. (2020) 46:983–94. doi: 10.1007/s00134-020-05935-5
PubMed Abstract | Crossref Full Text | Google Scholar
2. Heffner, JE, Miller, KS, and Sahn, SA. Tracheostomy in the intensive care unit. Part 1: indications, technique, management. Chest. (1986) 90:269–74. doi: 10.1378/chest.90.2.269
PubMed Abstract | Crossref Full Text | Google Scholar
3. Raimondi, N, Vial, MR, Calleja, J, Quintero, A, Cortés, A, Celis, E, et al. Evidence-based guidelines for the use of tracheostomy in critically ill patients. J Crit Care. (2017) 38:304–18. doi: 10.1016/j.jcrc.2016.10.009
PubMed Abstract | Crossref Full Text | Google Scholar
4. Zivi, I, Valsecchi, R, Maestri, R, Maffia, S, Zarucchi, A, Molatore, K, et al. Early rehabilitation reduces time to Decannulation in patients with severe acquired brain injury: a retrospective study. Front Neurol. (2018) 9:559. doi: 10.3389/fneur.2018.00559
PubMed Abstract | Crossref Full Text | Google Scholar
5. Villemure-Poliquin, N, Costerousse, O, Lessard Bonaventure, P, Audet, N, Lauzier, F, Moore, L, et al. Tracheostomy versus prolonged intubation in moderate to severe traumatic brain injury: a multicentre retrospective cohort study. Can J Anaesth. (2023) 70:1516–26. doi: 10.1007/s12630-023-02539-7
PubMed Abstract | Crossref Full Text | Google Scholar
6. Humble, SS, Wilson, LD, JW, MK, Leath, TC, Song, Y, Davidson, MA, et al. eds. Tracheostomy risk factors and outcomes after severe traumatic brain injury. Brain Inj. (2016) 30:1642–7. doi: 10.1080/02699052.2016.1199915
PubMed Abstract | Crossref Full Text | Google Scholar
7. Nieszkowska, A, Combes, A, Luyt, CE, Ksibi, H, Trouillet, JL, Gibert, C, et al. Impact of tracheotomy on sedative administration, sedation level, and comfort of mechanically ventilated intensive care unit patients. Crit Care Med. (2005) 33:2527–33. doi: 10.1097/01.ccm.0000186898.58709.aa
PubMed Abstract | Crossref Full Text | Google Scholar
8. Alali, AS, Scales, DC, Fowler, RA, Mainprize, TG, Ray, JG, Kiss, A, et al. Tracheostomy timing in traumatic brain injury: a propensity-matched cohort study. J Trauma Acute Care Surg. (2013) 76, 70:–76; discussion 76-8. doi: 10.1097/TA.0b013e3182a8fd6a
PubMed Abstract | Crossref Full Text | Google Scholar
10. de Franca, SA, Tavares, WM, Salinet, ASM, Paiva, WS, and Teixeira, MJ. Early tracheostomy in severe traumatic brain injury patients: a Meta-analysis and comparison with late tracheostomy. Crit Care Med. (2020) 48:e325–31. doi: 10.1097/ccm.0000000000004239
PubMed Abstract | Crossref Full Text | Google Scholar
11. Khalili, H, Paydar, S, Safari, R, Arasteh, P, Niakan, A, and Abolhasani, FA. Experience with traumatic brain injury: is early tracheostomy associated with better prognosis? World Neurosurg. (2017) 103:88–93. doi: 10.1016/j.wneu.2017.02.060
PubMed Abstract | Crossref Full Text | Google Scholar
12. Lu, Q, Xie, Y, Qi, X, Li, X, Yang, S, and Wang, Y. Is early tracheostomy better for severe traumatic brain injury? A meta-analysis. World Neurosurg. (2018) 112:e324–30. doi: 10.1016/j.wneu.2018.01.043
PubMed Abstract | Crossref Full Text | Google Scholar
13. Robba, C, Poole, D, McNett, M, Asehnoune, K, Bösel, J, Bruder, N, et al. Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. (2020) 46:2397–410. doi: 10.1007/s00134-020-06283-0
PubMed Abstract | Crossref Full Text | Google Scholar
15. Andriolo, B, Andriolo, R, Saconato, H, Atallah, Á, Valente, O, and S,. Early versus late tracheostomy for critically ill patients. Cochrane Database Syst Rev. (2015) 2018:CD007271. doi: 10.1002/14651858.CD007271.pub3
PubMed Abstract | Crossref Full Text | Google Scholar
16. Lu, W, Wu, T, Cui, P, Zhang, J, Sheng, X, and Ding, Z. Timing of tracheotomy in patients with severe traumatic brain injury. J Craniofac Surg. (2019) 30:2168–70. doi: 10.1097/scs.0000000000005721
PubMed Abstract | Crossref Full Text | Google Scholar
17. Rizk, EB, Patel, AS, Stetter, CM, Chinchilli, VM, and Cockroft, KM. Impact of tracheostomy timing on outcome after severe head injury. Neurocrit Care. (2011) 15:481–9. doi: 10.1007/s12028-011-9615-7
PubMed Abstract | Crossref Full Text | Google Scholar
18. Shibahashi, K, Sugiyama, K, Houda, H, Takasu, Y, Hamabe, Y, and Morita, A. The effect of tracheostomy performed within 72 h after traumatic brain injury. Br J Neurosurg. (2017) 31:564–8. doi: 10.1080/02688697.2017.1302071
PubMed Abstract | Crossref Full Text | Google Scholar
19. McLaughlin, C, Darcy, D, Park, C, Lane, C, Mack, W, Bliss, D, et al. Timing of tracheostomy placement among children with severe traumatic brain injury: a propensity-matched analysis. J Trauma Acute Care Surg. (2019) 87:818–26. doi: 10.1097/ta.0000000000002237
PubMed Abstract | Crossref Full Text | Google Scholar
20. Wang, HK, Lu, K, Liliang, PC, Wang, KW, Chen, HJ, Chen, TB, et al. The impact of tracheostomy timing in patients with severe head injury: an observational cohort study. Injury. (2012) 43:1432–6. doi: 10.1016/j.injury.2011.03.059
PubMed Abstract | Crossref Full Text | Google Scholar
21. Tavares, WM, Araujo de França, S, Paiva, WS, and Teixeira, MJ. Early tracheostomy versus late tracheostomy in severe traumatic brain injury or stroke: a systematic review and meta-analysis. Aust Crit Care. (2023) 36:1110–6. doi: 10.1016/j.aucc.2022.12.012
PubMed Abstract | Crossref Full Text | Google Scholar
22. Azari, A, Mirmoeeni, S, Momtaz, D, Kotzur, T, Murtha, G, Garcia, C, et al. Early versus late tracheostomy in patients with traumatic brain injury: a US Nationwide analysis. Neurocrit Care. (2023) 40:551–61. doi: 10.1007/s12028-023-01778-2
PubMed Abstract | Crossref Full Text | Google Scholar
23. Hosokawa, K, Ishii, J, Ota, K, and Shime, N. Early tracheostomy in brain injury: more details are needed for seeking best practice. Crit Care Med. (2020) 48:e984–5. doi: 10.1097/ccm.0000000000004424
PubMed Abstract | Crossref Full Text | Google Scholar
24. Stelfox, HT, Crimi, C, Berra, L, Noto, A, Schmidt, U, Bigatello, LM, et al. Determinants of tracheostomy decannulation: an international survey. Crit Care. (2008) 12:R26. doi: 10.1186/cc6802
PubMed Abstract | Crossref Full Text | Google Scholar
25. Santus, P, Gramegna, A, Radovanovic, D, Raccanelli, R, Valenti, V, Rabbiosi, D, et al. A systematic review on tracheostomy decannulation: a proposal of a quantitative semiquantitative clinical score. BMC Pulm Med. (2014) 14:201. doi: 10.1186/1471-2466-14-201
PubMed Abstract | Crossref Full Text | Google Scholar
26. Kutsukutsa, J, Kuupiel, D, Monori-Kiss, A, Del Rey-Puech, P, and Mashamba-Thompson, TP. Tracheostomy decannulation methods and procedures for assessing readiness for decannulation in adults: a systematic scoping review. Int J Evid Based Healthc. (2019) 17:74–91. doi: 10.1097/xeb.0000000000000166
PubMed Abstract | Crossref Full Text | Google Scholar
27. Jenkins, R, Badjatia, N, Haac, B, van Besien, R, Biedlingmaier, JF, Stein, DM, et al. Factors associated with tracheostomy decannulation in patients with severe traumatic brain injury. Brain Inj. (2020) 34:1106–11. doi: 10.1080/02699052.2020.1786601
PubMed Abstract | Crossref Full Text | Google Scholar
28. Gallice, T, Cugy, E, Branchard, O, Dehail, P, and Moucheboeuf, G. Predictive factors for successful Decannulation in patients with tracheostomies and brain injuries: a systematic review. Dysphagia. (2024) 39:552–72. doi: 10.1007/s00455-023-10646-2
PubMed Abstract | Crossref Full Text | Google Scholar
29. Perin, C, Meroni, R, Rega, V, Braghetto, G, and Cerri, CG. Parameters influencing tracheostomy Decannulation in patients undergoing rehabilitation after severe acquired brain injury (sABI). Int Arch Otorhinolaryngol. (2017) 21:382–9. doi: 10.1055/s-0037-1598654
PubMed Abstract | Crossref Full Text | Google Scholar
30. Enrichi, C, Battel, I, Zanetti, C, Koch, I, Ventura, L, Palmer, K, et al. Clinical criteria for tracheostomy Decannulation in subjects with acquired brain injury. Respir Care. (2017) 62:1255–63. doi: 10.4187/respcare.05470
PubMed Abstract | Crossref Full Text | Google Scholar
31. Shrestha, KK, Mohindra, S, and Mohindra, S. How to decannulate tracheostomised severe head trauma patients: a comparison of gradual vs abrupt technique. Nepal Med Coll J. (2012) 14:207–11.
PubMed Abstract | Google Scholar
32. Hakiki, B, Draghi, F, Pancani, S, Portaccio, E, Grippo, A, Binazzi, B, et al. Decannulation after a severe acquired brain injury. Arch Phys Med Rehabil. (2020) 101:1906–13. doi: 10.1016/j.apmr.2020.05.004
PubMed Abstract | Crossref Full Text | Google Scholar
33. Lanini, B, Binazzi, B, Romagnoli, I, Chellini, E, Pianigiani, L, Tofani, A, et al. Tracheostomy decannulation in severe acquired brain injury patients: the role of flexible bronchoscopy. Pulmonology. (2023) 29:S80–5. doi: 10.1016/j.pulmoe.2021.05.006
PubMed Abstract | Crossref Full Text | Google Scholar
34. Zanata Ide, L, Santos, RS, and Hirata, GC. Tracheal decannulation protocol in patients affected by traumatic brain injury. Int Arch Otorhinolaryngol. (2014) 18:108–14. doi: 10.1055/s-0033-1363467
PubMed Abstract | Crossref Full Text | Google Scholar
35. Eskildsen, SJ, Hansen, CA, Kallemose, T, Curtis, DJ, Wessel, I, and Poulsen, I. Factors associated with time to Decannulation in patients with tracheostomy following severe traumatic brain injury. Respir Care. (2024) 69:566–74. doi: 10.4187/respcare.11376
PubMed Abstract | Crossref Full Text | Google Scholar
36. Ceriana, P, Carlucci, A, Navalesi, P, Rampulla, C, Delmastro, M, Piaggi, GC, et al. Weaning from tracheotomy in long-term mechanically ventilated patients: feasibility of a decisional flowchart and clinical outcome. Intensive Care Med. (2003) 29:845–8. doi: 10.1007/s00134-003-1689-z
PubMed Abstract | Crossref Full Text | Google Scholar
37. Garuti, G, Reverberi, C, Briganti, A, Massobrio, M, Lombardi, F, and Lusuardi, M. Swallowing disorders in tracheostomised patients: a multidisciplinary/multiprofessional approach in decannulation protocols. Multidiscip Respir Med. (2014) 9:36. doi: 10.1186/2049-6958-9-36
PubMed Abstract | Crossref Full Text | Google Scholar
38. Matesz, I, Dénes, Z, Belinszkaja, G, Frey, E, Nagy, H, Tarjányi, S, et al. Bronchoscopy-guided decannulation of tracheostomy in patients with brain injury. Orv Hetil. (2014) 155:1108–12. doi: 10.1556/oh.2014.29947
PubMed Abstract | Crossref Full Text | Google Scholar
39. Li, Z, Chen, J, Zhang, D, Lv, L, and Hou, L. Tracheostomy as a risk factor for paroxysmal sympathetic hyperactivity in severe traumatic brain injury. World Neurosurg. (2019) 123:e156–61. doi: 10.1016/j.wneu.2018.11.101
PubMed Abstract | Crossref Full Text | Google Scholar
40. LeBlanc, J, Shultz, JR, Seresova, A, de Guise, E, Lamoureux, J, Fong, N, et al. Outcome in tracheostomized patients with severe traumatic brain injury following implementation of a specialized multidisciplinary tracheostomy team. J Head Trauma Rehabil. (2010) 25:362–5. doi: 10.1097/HTR.0b013e3181cd67ea
PubMed Abstract | Crossref Full Text | Google Scholar
41. Perry, A, Mallah, M, Cunningham, K, Christmas, A, Marrero, J, Gombar, M, et al. PATHway to success: implementation of a multiprofessional acute trauma health care team decreased length of stay and cost in patients with neurological injury requiring tracheostomy. J Trauma Acute Care Surg. (2019) 88:176–9. doi: 10.1097/ta.0000000000002494
Crossref Full Text | Google Scholar
42. Lima, F, Neves, W, Dias, A, Mendes, C, Simor, A, Pimentel, I, et al. Nursing care protocol for critical users with tracheostomy under mechanical ventilation. Rev Bras Enferm. (2024) 77:e20230337. doi: 10.1590/0034-7167-2023-0337
留言 (0)