Type 1 diabetes (T1D) is a chronic autoimmune metabolic disorder characterized by a complete deficiency of insulin, leading to hyperglycemia and ketonemia (1). It is one of the most prevalent chronic illnesses affecting children and adolescents worldwide. Currently, over 1.2 million individuals under the age of 19 are diagnosed with T1D globally, and studies indicate that its incidence in pediatric populations is on the rise (2). Poor management of pediatric T1D is strongly associated with acute life-threatening events and long-term complications with significant morbidity and mortality. To minimize these risks, a comprehensive approach involving medical nutrition therapy, intensive insulin regimens, and frequent blood glucose monitoring is crucial. It is also essential that both the patient and their family receive thorough education about the disease and guidance on how to continuously assess and manage its progression. Individualized care plans are necessary, as each patient’s risk for hypoglycemia or hyperglycemia varies (3). Moreover, to ensure effective disease management direct medical supervision with regular short-term visits are recommended. Unfortunately, in pediatrics, despite recently advancements in glucose monitoring and insulin administration (4), adherence to treatment regimens is generally poor, significantly increasing incidence and severity of clinical problems.
(5) Several factors explain this finding. Among them, insufficient parent- and patient-provider communication, as satisfaction with these relationships have been found essential for good health outcomes and adherence to treatment recommendations. Unfortunately, it does not occur in many T1D cases, particularly for children living far from healthcare facilities or facing provider shortages. This situation often leads to poor access to care, resulting in inadequate diabetes management and a heightened risk of complications due to long travel distances and associated costs (6).
Telemedicine (TM), the use of electronic technology to facilitate the exchange of medical information between patients and healthcare providers (7), has been effective in addressing many issues related to the frequent need for in-person visits for chronic disease management (8). Although most research in this area has focused on adults (9–11), evidence suggests that TM may also benefit pediatric patients with chronic conditions (12–15), including T1D (16–20). However, despite promising results indicating TM’s potential as an alternative healthcare delivery model, challenges remain, particularly concerning its effectiveness in managing glycemic control in children and adolescents with T1D. Not all issues associated with TM use in this demographic have been fully resolved.
This narrative review explores the current knowledge surrounding TM use in pediatric T1D management.
2 MethodsTo reach the goal, a comprehensive review of literature was conducted using the MEDLINE/PubMed database, covering studies published from January 2000 to May 15, 2024. This time window was selected to capture the period during which TM has been developed and progressively used. The review included randomized placebo-controlled trials, controlled clinical trials, double-blind randomized controlled studies, systematic reviews, and meta-analyses. Exclusion criteria included non-English language papers, studies with insufficient data, non-peer-reviewed articles, duplicated, unavailable full texts, or abstract-only papers. The search strategy used combinations of keywords such as “Diabetes Mellitus, Type 1” AND (“Telemedicine” OR “Telemetry” OR “Telenursing” OR “Internet-Based Intervention”) AND (“Child” OR “Adolescent”), as well as “type 1 diabetes” AND “Telemedicine” OR “Telehealth” OR “children” OR “adolescents” OR “glucose metabolism.” All studies identified were assessed for relevance by VS and NP to the review based on the title and abstract. For studies that appeared to meet the inclusion criteria, or in cases when a definite decision could not be made based on the title and/or abstract alone, the full paper was obtained for detailed assessment by two researchers against the inclusion criteria. Any disagreement was resolved by consultation with a third independent reviewer (SE). The collected data were grouped and discussed according to their importance in defining the use of the different types of TM by families, patients and health providers, the relationship created between these users, and, finally, the impact of TM on the management of pediatric T1D.
3 Telemedicine characteristics and attitudes towards its use3.1 Types of telemedicineTM employs various telecommunication methods to facilitate the exchange of medical information between patients and healthcare providers (Table 1). These methods are designed to enhance the physician-patient relationship, support care plans, and promote prevention of complications and exacerbations by adhering to clinical guidelines and strategies aimed at empowering patients (20, 21). Additionally, TM provides a more comprehensive evaluation of the clinical, social, and economic needs of patients, potentially offering better health outcomes compared to traditional periodic in-person visits (22). TM methods are categorized as either asynchronous or synchronous, depending on whether they provide real-time, face-to-face interactions (23). Asynchronous communications include email, internet, cell phone, and automated messaging systems. In contrast, synchronous communications involve real-time, face-to-face interactions via videoconferencing tools such as television, digital cameras, webcams, and videophones. These technologies enable simultaneous connections between caregivers and multiple patients, offering a significant advantage, especially for patient and parent education.
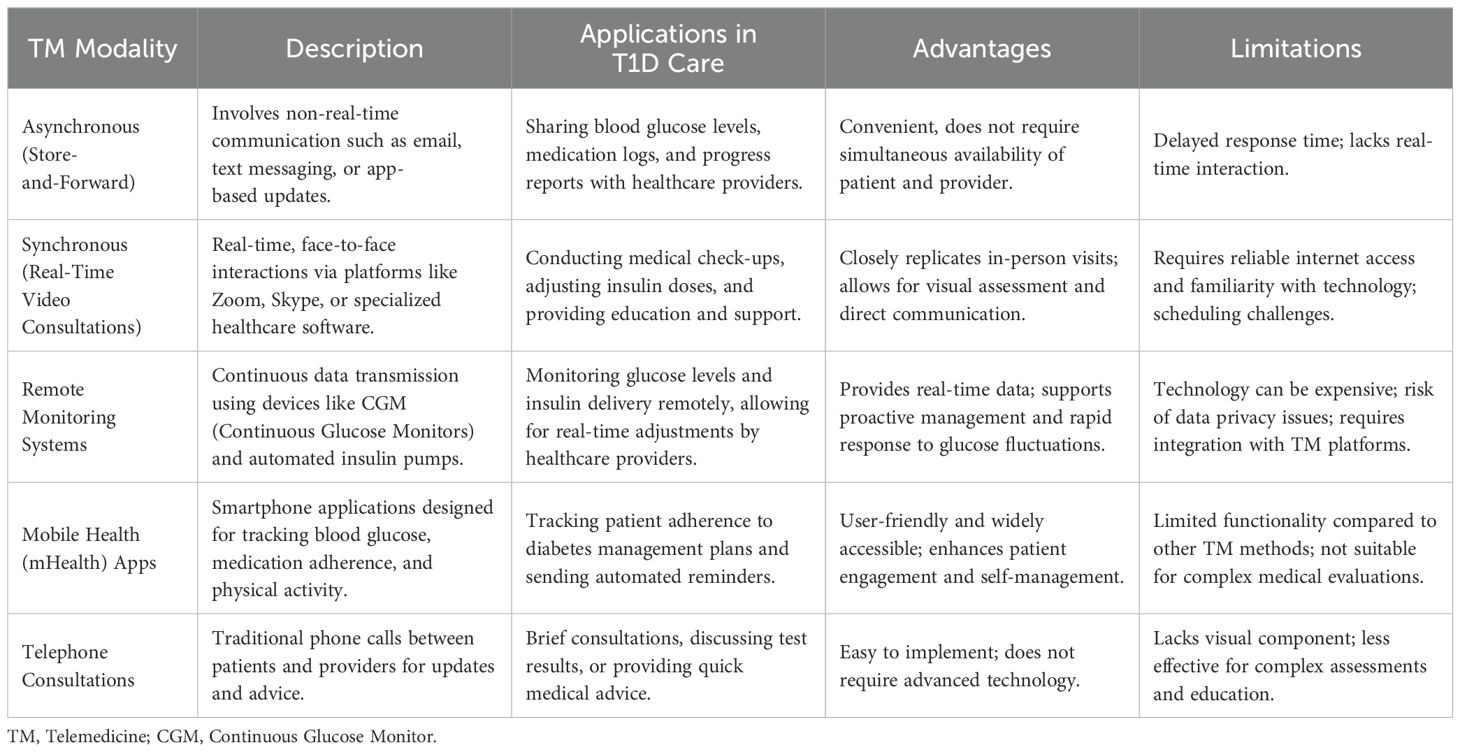
Table 1. Telemedicine modalities and their applications in pediatric type 1 diabetes (T1D) care.
3.2 Adoption of telemedicneBefore the COVID-19 pandemic, the use of TM in pediatric T1D care was limited, with telephone being the most common method of communication. A Canadian study found that, prior to the pandemic, TM accounted for less than 5% of all consultations and was primarily used for patients who faced difficulties accessing specialists in person (24). However, due to restrictions implemented by health authorities to limit the spread of SARS-CoV-2 (25), TM usage surged in the early months of the pandemic. The adoption of different technologies varied depending on their complexity. Initially, both patients and doctors faced challenges accessing the necessary equipment and familiarizing themselves with more complex TM methods. Additionally, some clinics hesitated to adopt synchronous communication methods immediately. Nevertheless, as access to technology improved and healthcare workers’ attitudes toward TM became more favorable, synchronous methods gained widespread acceptance and became a common approach in pediatric T1D care. A study assessing changing preferences for pediatric T1D care showed a significant shift towards using video visits over telephone consultations between the early and later phases of the pandemic, mainly due to their ease of use, advantages for learning, and higher interface quality (26). Face-to-face interactions increased from 46% to 92% of all TM visits. Furthermore, the increase in more advanced synchronous communication correlated with higher participation rates among children or adolescents (81% to 92%) and a greater involvement of healthcare workers in the TM visit (36% to 80%).
3.3 Adoption of telemedicine by families, patients and healthcare workersRegardless of the method used, most studies report that patients and parents generally accept TM for pediatric T1D management and view it as an improvement. Bassi et al. evaluated patient and parent satisfaction after the introduction of televisits during the pandemic (27). The study found that the majority of patients and parents (74.1%) did not find the absence of in-person visits problematic and were satisfied with the TM service. The majority of respondents felt able to effectively communicate their medical concerns (89.9%) and receive high-quality care (92.4%), although satisfaction was higher among insulin pump users compared to those on multiple daily injections (92.4% vs. 82.5%; P = 0.023). Additionally, satisfaction levels were notably higher among families living farther from their healthcare providers (97.7% vs. 89.1%; P = 0.017). Similar findings were observed in other studies (24, 26, 28). Crossen et al. assessed T1D patient satisfaction with video-based care after six months of TM use and found that 94% of participants were very satisfied, citing improved access to care teams, enhanced monitoring of blood glucose levels, and increased knowledge of diabetes technology (29). Other studies highlighted TM’s benefits, including more comprehensive metabolic data transmission and better communication between caregivers and peers (30–34). Moreover, TM was shown to reduce diabetes-related stress, depressive symptoms, and hypoglycemia anxiety in parents of children with T1D. In a video-based telehealth intervention called Cognitive Adaptations to Reduce Emotional Stress (CARES), 41 parents of children with T1D participated in an 8–12-week program. The results indicated significant reductions in depressive symptoms and hypoglycemia fears, both at the end of the intervention and three months later.
From the perspective of diabetes specialists, including diabetologists and diabetes nurses, studies indicate that TM is considered a valuable tool for improving patient care. It allows for more frequent contacts, timely monitoring, and precise adjustments in therapy (35). However, achieving these benefits depends on healthcare providers’ familiarity with technology, a positive attitude towards virtual consultations, and a consensus on the roles and responsibilities of all professionals involved in patient care.
The minimal number of patients and endocrinologists who opted to discontinue TM after its introduction highlights the generally positive attitudes toward this intervention. In a few cases, challenges to TM adoption included concerns over privacy due to the use of shared platforms rather than personal devices, lack of integration between TM systems and existing electronic health records, and the use of technological devices that were not engaging for children and adolescents. Furthermore, the financial burden of acquiring necessary equipment and covering provider costs posed significant barriers for economically disadvantaged populations, particularly in regions where healthcare systems do not provide free communication services (36–38).
3.4 Unsolved problems regarding satisfaction with telemedicineDespite these favorable findings, some questions remain unanswered regarding patient, family, and healthcare provider satisfaction with TM for pediatric T1D management. One issue is determining the best way to organize TM services. A recent systematic review and meta-analysis of 20 studies published before May 1, 2023, involving 1,704 children and adolescents with T1D (mean age 13.5 years, median diabetes duration at baseline 6.2 years) found significant heterogeneity among the studies (38). Various forms of TM were used, with differing types of information exchanged and diverse participants involved in the communication process. In 30% of the studies, smart wearable devices were employed, while 25% used smartphone applications, 15% utilized modems, 15% engaged in web-based videoconferencing, and 10% relied on telephone; 5% did not report this information. Healthcare providers used smartphone applications in 25%, websites in 15%, web conferences in 15%, telephone in 15%, and SMS text messaging in 15%. This variety created numerous combinations. Additionally, satisfaction assessments varied, with patients’ opinions often mediated by parents (in about half of the cases) and healthcare professionals’ feedback provided by individual providers in 50% of the studies, while the remaining studies involved a specialist diabetes care team consisting of diabetologists, nurses, dietitians, and psychologists. TM interventions addressed various aspects, including glucose monitoring, insulin dose adjustments, health information dissemination, and physical activity guidance, either individually or in combination (39). These limitations prevent firm conclusions regarding the best and most effective way to organize TM services for pediatric T1D care. Further limitations arise from the short duration of outcome monitoring in most studies, making it unclear whether TM satisfaction persists beyond periods when in-person visits are restricted. It is important to note that most studies on TM were conducted during the COVID-19 pandemic, and information on the impact of TM on younger children is limited. Consequently, there is insufficient evidence to determine whether TM effectively addresses the unique needs of children with T1D.
4 Impact of telemedicine on the patient-healthcare provider relationshipStudies examining the impact of TM on interactions between pediatric T1D patients and healthcare providers generally show high levels of satisfaction with remote consultations. The findings reveal that TM introduces several advantages, significantly enhancing patient-caregiver interactions. One notable benefit is the increase in the frequency of consultations, often reaching or surpassing the levels recommended by professional medical organizations. For example, a study involving 54 pediatric patients (mean age 12.1 ± 4.1 years) tracked over 12 months before and after the introduction of TM demonstrated an increase in specialist contacts from 2.0 ± 1.3 to 2.9 ± 1.3 per year (P = 0.0001), which aligns closely with the recommendations of the American Diabetes Association (ADA) (40). Additionally, patients and their families experienced fewer disruptions to school and work, and financial burdens associated with attending appointments were reduced.
Similar outcomes were reported in other studies, including one by Kaushal et al., who evaluated 555 patients with a mean age of 12.3 ± 3.4 years. Their research showed that TM led to an increase in the frequency of diabetes visits from 3.8 ± 1.7 to 4.3 ± 2.2 per year (P < 0.001), with 92% of these visits conducted virtually (41).
From the outset, TM’s ability to reduce time and financial burdens for patients and families was evident, even when asynchronous technologies were initially used. For example, Chase et al. assessed the impact of biweekly blood glucose data transmission using the Acculink modem over six months in a group of adolescents, without any associated in-person visits during this period (42). Compared to controls, who attended three clinic visits (at 0, 3, and 6 months) and had the option to telephone or fax blood glucose results as needed, the TM group experienced significantly lower overall expenses (P < 0.001) and fewer school absences, averaging 0.4 days per visit. Additionally, parents in the TM group did not miss working days, whereas parents of children receiving standard care missed an average of 0.5 days per clinical visit. Specifically, the mean cost per patient for the modem-based approach was $163, covering modem and cable costs, provider training, patient education, and computer use. In contrast, the mean cost per patient for traditional care was $305, including clinic visits, travel, and accommodation when necessary.
More recent data confirm the time-saving and economic benefits of TM. Crossen et al. calculated that the median duration of a video visit, including time spent uploading diabetes device data, was 33 minutes (range: 12–110 minutes). In comparison, in-person clinic visits had a median duration of 240 minutes, ranging from 120 to 4,320 minutes (29). This equated to an average time savings of 186 minutes per visit (range: 70–4,274 minutes), highlighting TM’s efficiency and its potential to significantly reduce the time burden for patients and families.
5 Impact of telemedicine on type 1 diabetes managementStudies investigating the impact of TM on the management of T1D suggest that the increased frequency of patient-provider interactions through TM may contribute to improved glycemic control and reductions in HbA1c levels (Table 2). HbA1c concentration is the gold standard for assessing long-term blood glucose control, and elevated HbA1c levels above 58 mmol/mol (7.5%) are consistently associated with negative outcomes in T1D (43). Accordingly, most studies on the impact of TM on T1D management have monitored changes in HbA1c levels during remote consultations. However, the results have been inconsistent. Some studies have shown that TM use leads to significant reductions in HbA1c levels, closely correlated with the frequency of remote consultations (44–48). In contrast, other studies have found TM to be as effective as, or sometimes less effective than, traditional in-person visits for managing glucose levels (16, 49–54). This variability makes it difficult to draw definitive conclusions about the efficacy of TM in improving glycemic control.
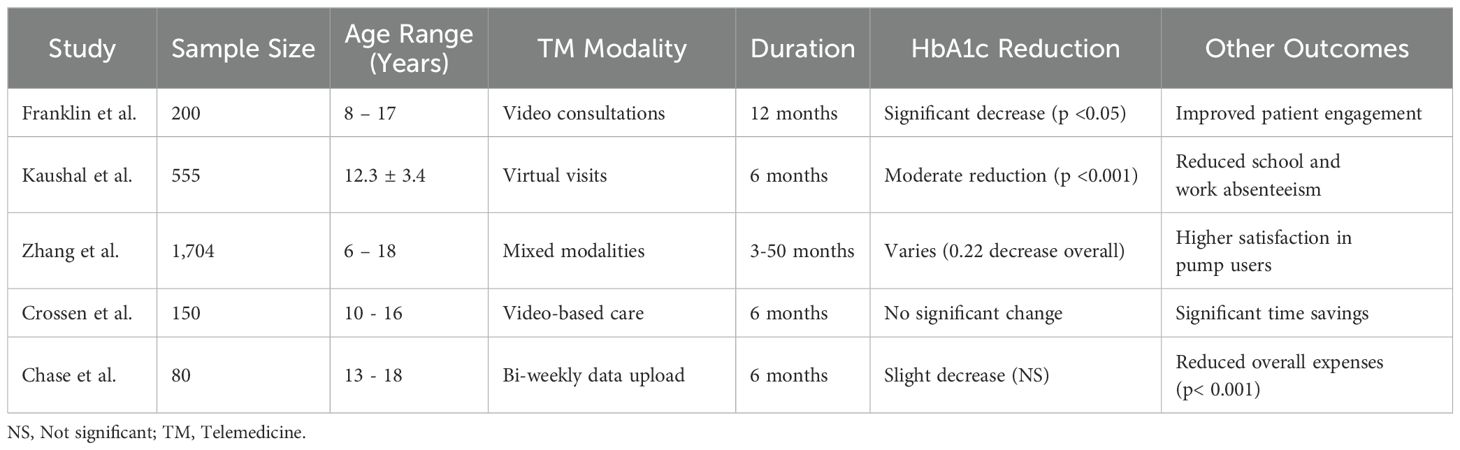
Table 2. Summary of main studies investigating the impact of telemedicine on glycemic control in pediatric type 1 diabetes.
Conflicting results also arise when evaluating other glucose management parameters besides HbA1c. For example, a meta-analysis showed that while TM was associated with a reduction in hypoglycemia incidence compared to controls [mean difference (MD) –0.15, 95% CI –0.57 to 0.27; P = 0.49], the difference was not statistically significant, making it unclear whether TM had a meaningful impact (51). Further doubts about the efficacy of TM emerge when considering the methodological limitations of studies on HbA1c variations. Although many of these studies were randomized clinical trials, only 25% adequately described their randomization strategies and allocation concealment. Additionally, many studies failed to report on withdrawals and dropouts, weakening the reliability of their findings.
Moreover, other factors, aside from TM, may have contributed to observed reductions in HbA1c levels. For instance, Franklin et al. suggested that the HbA1c improvements in their study were likely due to the intensity of insulin treatment rather than TM alone (53). Similarly, Zhang et al.’s systematic review and meta-analysis reported that HbA1c levels were assessed at intervals ranging from 3 to 50 months post-TM introduction (38). A global evaluation indicated a significant reduction in HbA1c levels by 0.22 (95% CI –0.33 to –0.10; P < 0.001) with TM. However, subgroup analysis revealed that TM was not effective at 3 months (MD –0.30, 95% CI –0.62 to 0.02; P = 0.07) or at 12 months (MD 0.04, 95% CI –0.33 to 0.40; P = 0.85). A significant improvement was only observed at the 6-month mark (MD –0.21, 95% CI –0.37 to –0.05; P = 0.01). This suggests TM’s effectiveness may peak around 6 months, but it may diminish over time. Alternatively, these HbA1c trends could be influenced by the so-called honeymoon phase of T1D, where patients experience a temporary period of remission with lower insulin needs and stable HbA1c levels, typically beginning about 3 months after the onset of insulin therapy and lasting several months (54).
The improvements in glycemic control observed with TM could also be attributed to concurrent use of advanced technologies such as continuous glucose monitors (CGM) and insulin pumps. Studies have shown that these devices, especially when integrated into automated insulin delivery systems, can significantly enhance glycemic control in both adults and children. For example, a recent multicenter, open-label randomized controlled trial involving 80 pediatric patients with poorly controlled T1D (HbA1c ≥8.5%) demonstrated that an automated insulin delivery system significantly reduced HbA1c levels from 10.5 ± 1.9% to 8.1 ± 1.8% after 13 weeks, whereas the control group saw no improvement (HbA1c remained at 10.4 ± 1.6% to 10.6 ± 1.8%). Moreover, no significant adverse events occurred in the TM group, while the control group reported one case of severe hypoglycemia and two cases of diabetic ketoacidosis (51). The role of these new technologies is further supported by evidence showing that studies where TM was less effective were conducted before 2010, a period when such technologies were not widely utilized. In contrast, studies with positive results were carried out more recently, coinciding with the increased adoption of CGM and insulin pumps (55).
Furthermore, TM studies provide limited information on its impact beyond glycemic control in pediatric T1D management. While insulin dosage adjustment, dietary advice, physical activity guidance, and health education are common aspects of TM, clinical outcomes beyond blood glucose levels are seldom reported. For instance, information on blood pressure, weight, and other relevant clinical markers is often lacking. Only a few studies have assessed the impact of TM on quality of life (QoL), and even these provide inconsistent results. The use of the Diabetes Quality of Life for Youth score did not show a significant difference between TM and usual care (impact of diabetes: P = 0.59; diabetes-related worries: P = 0.71; satisfaction with diabetes: P = 0.68) (56). Conversely, studies using non–youth-specific QoL indicators, such as the frequency of self-monitoring blood glucose and hypoglycemia incidence, reported statistically significant improvements (MD –0.24, 95% CI –0.45 to –0.02; P = 0.04) (57).
6 ConclusionsT1D management is one of the areas where TM has the potential to provide substantial benefits for patients, families, and healthcare systems. Table 3 summarizes benefits and challenges of TM in pediatric T1D. Overall, despite limitations previously reported, available studies suggest that TM can improve T1D care when both patients and providers are familiar with the technology and maintain a positive attitude towards remote consultations (38, 56). Under these conditions, TM increases patient-provider interactions, matching or even exceeding the frequency of traditional in-person visits. This results in various benefits, such as reduced travel-related burdens, time savings, and decreased financial costs for families. More frequent communication also helps patients and families better understand the disease, its monitoring requirements, and how to effectively use glucose monitoring and insulin infusion devices. Additionally, healthcare providers can offer more timely and precise medical monitoring and therapy adjustments through TM.
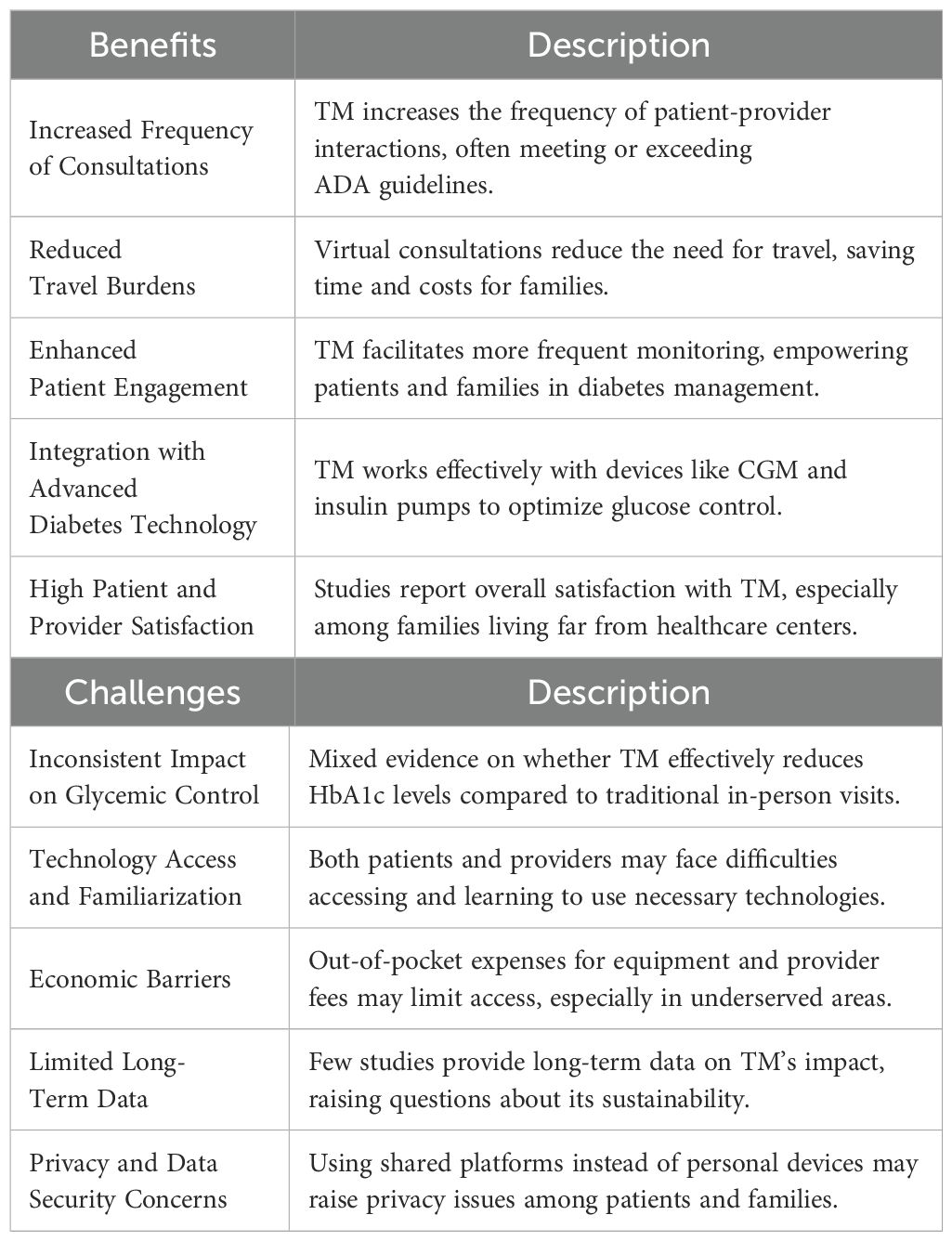
Table 3. Benefits and challenges of telemedicine in pediatric T1D management.
Despite these benefits, studies remain too generic to identify the most effective methods for maximizing satisfaction among patients and healthcare providers. Non-glucose-related clinical parameters such as blood pressure and weight, which are vital for holistic T1D management, often remain unaddressed during TM visits. Additionally, essential components of diabetes care—such as pubertal staging, examination of injection sites for lipohypertrophy or infection, and physical screening for complications (e.g., foot exams or retinopathy evaluations)—are either suboptimal or entirely absent in the TM setting. This lack of hands-on assessment may lead to delayed identification and intervention for potential complications. Therefore, a balanced approach combining in-person visits and telemedicine is critical to ensure comprehensive care. In-person visits can facilitate thorough physical examinations, structured screenings, and interpersonal connection, while TM offers convenience and increased frequency of interaction for addressing glucose management, education, and psychosocial support. By integrating these modalities, healthcare providers can leverage the strengths of both approaches, ensuring optimal outcomes while addressing the logistical challenges often faced by patients and their families. Moreover, studiesdo not sufficiently address the challenges of different TM approaches. Further research is needed to identify the optimal TM approach tailored to each patient’s needs, family circumstances, and available medical support. Establishing an ideal TM model is essential not only to enhance the already observed benefits but also to determine under which conditions TM can positively influence the T1D disease course. Current data do not definitively establish whether TM provides glycemic control comparable to that achieved through traditional in-person care. If equivalent control is confirmed, the social and economic advantages TM offers would make it a compelling option for the management of pediatric T1D, justifying its wider adoption in treating children and adolescents with this condition. Furthermore, future studies should assess the significance of potential challenges associated with telemedicine in managing T1D, including concerns about the privacy and security of collected data, limited access to reliable internet and technology, and the economic burden of implementing and maintaining these systems.
Author contributionsSE: Conceptualization, Funding acquisition, Supervision, Validation, Writing – original draft, Writing – review & editing. VS: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. FF: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. MS: Supervision, Validation, Writing – original draft, Writing – review & editing. NP: Supervision, Validation, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The publication of this manuscript was supported by the Laboratory for Clinical Pediatric Research, University of Parma, Parma, Italy (PED-2024-10).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statementThe author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References2. Patterson CC, Karuranga S, Salpea P, Saeedi P, Dahlquist G, Soltesz G, et al. Worldwide estimates of incidence, prevalence and mortality of type 1 diabetes in children and adolescents: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. (2019) 157:107842. doi: 10.1016/j.diabres.2019.107842
PubMed Abstract | Crossref Full Text | Google Scholar
3. Lindholm Olinder A, DeAbreu M, Greene S, Haugstvedt A, Lange K, Majaliwa ES, et al. ISPAD Clinical Practice Consensus Guidelines 2022: Diabetes education in children and adolescents. Pediatr Diabetes. (2022) 23:1229–42. doi: 10.1111/pedi.13418
PubMed Abstract | Crossref Full Text | Google Scholar
5. Chiang JL, Kirkman MS, Laffel LM, Peters AL, Type 1 Diabetes Sourcebook Authors. Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes Care. (2014) 37:2034–54. doi: 10.2337/dc14-1140
PubMed Abstract | Crossref Full Text | Google Scholar
6. Vachon GC, Ezike N, Brown-Walker M, Chhay V, Pikelny I, Pendergraft TB. Improving access to diabetes care in an inner-city, community-based outpatient health center with a monthly open-access, multistation group visit program. J Natl Med Assoc. (2007) 99:1327–36.
PubMed Abstract | Google Scholar
7. Kvedar J, Coye MJ, Everett W. Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff (Millwood). (2014) 33:194–9. doi: 10.1377/hlthaff.2013.0992
PubMed Abstract | Crossref Full Text | Google Scholar
10. Ezeamii VC, Okobi OE, Wambai-Sani H, Perera GS, Zaynieva S, Okonkwo CC, et al. Revolutionizing healthcare: how telemedicine is improving patient outcomes and expanding access to care. Cureus. (2024) 16:e63881. doi: 10.7759/cureus.63881
PubMed Abstract | Crossref Full Text | Google Scholar
11. Kim HJ, Tomaszewski M, Zhao B, Lam E, Enns R, Bressler B, et al. Impact of telehealth on medication adherence in chronic gastrointestinal diseases. J Can Assoc Gastroenterol. (2022) 5:203–7. doi: 10.1093/jcag/gwac016
PubMed Abstract | Crossref Full Text | Google Scholar
13. Dev V, Mittal A, Joshi V, Meena JK, Dhanesh Goel A, Didel S, et al. Cost analysis of telemedicine use in paediatric nephrology-the LMIC perspective. Pediatr Nephrol. (2024) 39:193–201. doi: 10.1007/s00467-023-06062-1
PubMed Abstract | Crossref Full Text | Google Scholar
14. Faiçal AVB, Mota LR, Correia DA, Monteiro LP, Souza EL, Terse-Ramos R. Telehealth for children and adolescents with chronic pulmonary disease: systematic review. Rev Paul Pediatr. (2023) 42:e2024111.
PubMed Abstract | Google Scholar
16. Shulman RM, O'Gorman CS, Palmert MR. The impact of telemedicine interventions involving routine transmission of blood glucose data with clinician feedback on metabolic control in youth with type 1 diabetes: a systematic review and meta-analysis. Int J Pediatr Endocrinol. (2010) 2010:536957. doi: 10.1186/1687-9856-2010-536957
PubMed Abstract | Crossref Full Text | Google Scholar
17. Guljas R, Ahmed A, Chang K, Whitlock A. Impact of telemedicine in managing type 1 diabetes among school-age children and adolescents: an integrative review. J Pediatr Nurs. (2014) 29:198–204. doi: 10.1016/j.pedn.2013.10.013
PubMed Abstract | Crossref Full Text | Google Scholar
18. Rochmah N, Farahdina F, Deakandi WY, Putri QAN, Nuzula TM, Fedora K, et al. The role of telemedicine in type 1 diabetes children during COVID-19 pandemic era: A systematic review and meta-analysis. Open Access Maced J Med Sci. (2023) 11:38–43. doi: 10.3889/oamjms.2023.10097
Crossref Full Text | Google Scholar
19. Garcia JF, Faye E, Reid MW, Pyatak EA, Fox DS, Bisno DI, et al. Greater telehealth use results in increased visit frequency and lower physician related-distress in adolescents and young adults with type 1 diabetes. J Diabetes Sci Technol. (2023) 17:878–86. doi: 10.1177/19322968221146806
PubMed Abstract | Crossref Full Text | Google Scholar
20. Raymond JK. Models of care for adolescents and young adults with type 1 diabetes in transition: shared medical appointments and telemedicine. Pediatr Ann. (2017) 46:e193–7. doi: 10.3928/19382359-20170425-01
PubMed Abstract | Crossref Full Text | Google Scholar
21. Esposito S, Rosafio C, Antodaro F, Argentiero A, Bassi M, Becherucci P, et al. Information and Training on the Use of Telemedicine in Pediatric Population: Consensus Document of the Italian Society of Telemedicine (SIT), of the Italian Society of Preventive and Social Pediatrics (SIPPS), of the Italian Society of Pediatric Primary Care (SICuPP), of the Italian Federation of Pediatric Doctors (FIMP), and of the Syndicate of Family Pediatrician Doctors (SIMPeF). The contribution of teleconsultation and video-conferencing to diabetes care: a systematic literature review. J Pers Med. (2023) 13:314. doi: 10.3390/jpm13020314
PubMed Abstract | Crossref Full Text | Google Scholar
22. Verhoeven F, van Gemert-Pijnen L, Dijkstra K, Nijland N, Seydel E, Steehouder M. The contribution of teleconsultation and video-conferencing to diabetes care: a systematic literature review. J Med Internet Res. (2007) 9:e37.
PubMed Abstract | Google Scholar
23. Verhoeven F, Tanja-Dijkstra K, Nijland N, Eysenbach G, van Gemert-Pijnen L. Asynchronous and synchronous teleconsultation for diabetes care: a systematic literature review. J Diabetes Sci Technol. (2010) 4:666–84. doi: 10.1177/193229681000400323
PubMed Abstract | Crossref Full Text | Google Scholar
24. Fung A, Irvine M, Ayub A, Ziabakhsh S, Amed S, Hursh BE. Evaluation of telephone and virtual visits for routine pediatric diabetes care during the COVID-19 pandemic. J Clin Transl Endocrinol. (2020) 22:100238. doi: 10.1016/j.jcte.2020.100238
PubMed Abstract | Crossref Full Text | Google Scholar
26. Niyyati S, Fung A, Zhang Q, Ng C, Amed S, Bone JN, et al. Patient perceptions of telehealth for pediatric type 1 diabetes during the COVID-19 pandemic: A follow-up study. Can J Diabetes. (2023) 47:579–86.e6. doi: 10.1016/j.jcjd.2023.05.005
PubMed Abstract | Crossref Full Text | Google Scholar
27. Bassi M, Strati MF, Parodi S, Lightwood S, Rebora C, Rizza F, et al. Patient satisfaction of telemedicine in pediatric and young adult type 1 diabetes patients during Covid-19 pandemic. Front Public Health. (2022) 10:857561.
PubMed Abstract | Google Scholar
28. Katzow MW, Steinway C, Capossela E, Chen J, Chen V, Fenster T, et al. Utilization and patient-reported outcomes of direct-to-consumer telemedicine during the first 6 weeks of the COVID-19 pandemic in the largest pediatric ambulatory network in New York State. Telemed J E Health. (2024) 30:e1944–53. doi: 10.1089/tmj.2023.0483
PubMed Abstract | Crossref Full Text | Google Scholar
29. Crossen S, Glaser N, Sauers-Ford H, Chen S, Tran V, Marcin J. Home-based video visits for pediatric patients with poorly controlled type 1 diabetes. J Telemed Telecare. (2020) 26:349–55. doi: 10.1177/1357633X19828173
PubMed Abstract | Crossref Full Text | Google Scholar
30. Branger PJ, van't Hooft A, van der Wouden JC, Moorman PW, van Bemmel JH. Shared care for diabetes: supporting communication between primary and secondary care. Int J Med Inform. (1999) 53:133–42. doi: 10.1016/S1386-5056(98)00154-3
PubMed Abstract | Crossref Full Text | Google Scholar
31. Hess R, Bryce CL, McTigue K, Fitzgerald K, Zickmund S, Olshansky E, et al. The diabetes patient portal: patient perspectives on structure and delivery. Diabetes Spectrum. (2006) 2006:106–10. doi: 10.2337/diaspect.19.2.106
Crossref Full Text | Google Scholar
32. Whittaker SL, Adkins S, Phillips R, Jones J, Horsley MA, Kelley G. Success factors in the long-term sustainability of a telediabetes programme. J Telemed Telecare. (2004) 10:84–8. doi: 10.1258/135763304773391512
PubMed Abstract | Crossref Full Text | Google Scholar
33. Losiouk E, Lanzola G, Del Favero S, Boscari F, Messori M, Rabbone I, et al. Parental evaluation of a telemonitoring service for children with Type 1 Diabetes. J Telemed Telecare. (2018) 24:230–7. doi: 10.1177/1357633X17695172
PubMed Abstract | Crossref Full Text | Google Scholar
34. Hart RI, Kimbell B, Rankin D, Allen JM, Boughton CK, Campbell F, et al. Parents' experiences of using remote monitoring technology to manage type 1 diabetes in very young children during a clinical trial: Qualitative study. Diabetes Med. (2022) 39:e14828. doi: 10.1111/dme.14828
PubMed Abstract | Crossref Full Text | Google Scholar
35. Frielitz FS, Dördelmann J, Lemke S, Lange K, Hiort O, Katalinic A, et al. Assessing the benefits and challenges of video consultations for the treatment of children with type 1 diabetes - A qualitative study among diabetes professionals. Exp Clin Endocrinol Diabetes. (2021) 129:831–6.
PubMed Abstract | Google Scholar
36. Hilliard ME, Levy W, Anderson BJ, Whitehouse AL, Commissariat PV, Harrington KR, et al. Benefits and barriers of continuous glucose monitoring in young children with type 1 diabetes. Diabetes Technol Ther. (2019) 21:493–8. doi: 10.1089/dia.2019.0142
PubMed Abstract | Crossref Full Text | Google Scholar
37. March CA, Nanni M, Kazmerski TM, Siminerio LM, Miller E, Libman IM. Modern diabetes devices in the school setting: Perspectives from school nurses. Pediatr Diabetes. (2020) 21:832–40. doi: 10.1111/pedi.13015
PubMed Abstract | Crossref Full Text | Google Scholar
38. Zhang K, Huang Q, Wang Q, Li C, Zheng Q, Li Z, et al. Telemedicine in improving glycemic control among children and adolescents with type 1 diabetes mellitus: systematic review and meta-analysis. J Med Internet Res. (2024) 26:e51538. doi: 10.2196/51538
留言 (0)