Inflammatory bowel disease (IBD) is a chronic, nonspecific intestinal inflammatory disease that mainly involves ulcerative colitis (UC) and Crohn's disease (CD) (1). Both UC and CD are incurable chronic diseases that can cause chronic inflammatory changes in the gastrointestinal tract (2, 3).In recent years, the global diagnosis rate of children and adolescents has been increasing, with high-risk onset ages between 15 and 35 years (4). Approximately 25% of cases are diagnosed before the age of 18 years (1), with more severe and faster developing intestinal infections observed in the pediatric population (2). IBD is a chronic intestinal disease that negatively affects both the mental health and quality of life of afflicted children (5). Although the disease may resolve after treatment, fatigue continues to affect the patient's daily life. Fatigue is the most annoying symptom in patients with inactive disease and the second most annoying symptom in patients with active disease (3).
Fatigue refers to subjectively continuous tiredness and a lack of energy and exhaustion, which reduces one's physical and mental activities and cannot be relieved through prolonged sleep (6). As reported, 86% of people with moderate to severe IBD experience fatigue, with fatigue remaining the most exhausting symptom even in remission and garnering more attention from patients relative to bowel symptoms (7). The Clinical Guidelines for the Management of IBD published in 2021 propose that fatigue cannot be ignored because it has a serious negative impact on people's quality of life (8). It affects physical, emotional, cognitive and social functioning and affects quality of life (9–11). The International Organization for Study of Inflammatory Bowel Diseases has reached a consensus stating that numerous IBD patients have reported a notable decrease in physical activity compared to their pre-diagnosis levels, attributing this to perceived fatigue (12). A study, which surveyed the levels of physical activity among 219 individuals diagnosed with inflammatory bowel disease (IBD), revealed a notably alarming proportion of inactivity among IBD patients, specifically 94 individuals (42.9%) (13). Exercise is a potential intervention for fatigue and a subsequent decrease in their physical activity levels has been found to exacerbate fatigue even further (14, 15). However, fatigue is often overlooked by healthcare professionals when assessing the severity of symptoms or outcomes of many diseases. The existing studies concerning the fatigue of patients with IBD lack population data for children in China. Hence, the aim of this study was to describe the prevalence and degree of fatigue in a cohort of pediatric IBD patients in China. In addition, we wanted to explore the possible associations between fatigue and/or markers of disease activity.
2 Methods 2.1 Study setting and samplingThe study was conducted in the Department of Gastroenterology of Children's Hospital of Nanjing Medical University.
Patients diagnosed with IBD were recruited via convenience sampling methods from the Department of Gastroenterology of Children's Hospital from 1 September 2021 until 31 November 2022. A total of 110 questionnaires were sent out onsite in this study, and 105 were effectively received, with an effective recovery rate of 95.45%. This study was performed in accordance with the principles of the Declaration of Helsinki. The ethics committee of Nanjing Children's Hospital affiliated with Nanjing Medical University approved the study protocol on 29 August 2023. The ethical number is 202302043-1.
2.2 Inclusion and exclusion criteriaThe inclusion criteria were being aged 5–18 years (consideration the factors of understanding, expressive capabilities, as well as the extent of admissions handled by pediatric medical institutions), having been diagnosed with IBD according to the expert consensus on the diagnosis and management of pediatric inflammatory bowel disease for more than one year (16), being able to understand and speak Chinese and having no history of cognitive impairment. The exclusion criteria were other conditions that inherently cause fatigue, independent of IBD or unwillingness to participate.
2.3 Instruments with validity and reliability 2.3.1 General information questionnaireA self-designed questionnaire was used, which included sex, age, geographical location, education status, source of medical expenses, duration of illness (/year), disease type, severity of disease [patients were asked about their number of bowel movements, presence of abdominal pain, presence of blood with defecation, and weight loss as mainly clinical symptoms combined pediatric ulcerative colitis activity index (PUCAI) for UC patients and pediatric Crohn's disease activity index (PCDAI) for CD patients.) (17, 18), complications (including gastrointestinal bleeding, enterobrosis, colon cancer or thrombus), body mass index (BMI) and medication use.
2.3.2 Multidimensional fatigue scale (MFS)The Multidimensional Fatigue Scale (MFS) was developed by Varni et al. (19) and later cross-culturally adapted by Bu Xiuqing et al. (20). It mainly measures the feelings of fatigue of children with chronic diseases in the past month, including three versions of 5–7 years old, 8–12 years old and 13–18 years old, which are composed of three dimensions of general fatigue, sleep fatigue and cognitive fatigue, with a total of 18 items. It was reverse scored with the Likert level 5 scoring method: 0 = 100 points (never happened), 1 = 75 points (almost never happened), 2 = 50 points (sometimes happened), 3 = 25 points (often happened), and 4 = 0 points (always happens). The lower the score is, the greater the degree of fatigue. The Cronbach's α coefficients of the three versions of the scales used in this study were 0.835, 0.842, and 0.924.
2.4 Data collectionThe researchers explained the purpose and completion requirements of the study to the IBD patients and their parents. The patients completed the general information questionnaire with the help of their parents and completed the MFS by themselves. For those with poor reading ability, the researchers read the questionnaire item by item to help them fill in, avoiding the use of suggestive language. The questionnaire was completed on the spot and returned to ensure its reliability. Before submitting the questionnaire, the healthcare professionals on duty will conduct a cross-verification of this information with the medical records. In the event of any discrepancies, the medical records shall be deemed as the authoritative source.
2.5 Data analysisThe data were entered into EpiData 3.1 to ensure accuracy. SPSS 23.0 statistical software was used to analyze the data. The measurement data with a normal distribution were described by x¯±s, and the counting data were represented by the frequency, constituent ratio and rate. T tests, ANOVA and multiple linear regression were used to analyze the influencing factors of fatigue in children with IBD, and p < 0.05 was considered to indicate statistical significance. Sample size calculation was conducted using G*Power software (21), with the statistical significance value accepted at p < 0.05 (two-tailed), setting an alpha error at 0.05, a statistical power at 0.8, and an effect size at 0.3. Taking into account a potential dropout rate of 20%, the final sample size was determined to be no less than 99 participants. Consequently, this study ultimately included a total of 110 cases.
3 ResultsAll 105 (100%) distributed questionnaires were valid. Thus, the study included 105 participants, 71 (67.62%) of whom were male. Furthermore, 95 (90.48%) patients had CD. The age of the participants ranged from 6 to 18 years, with a median (Me) of 16 years (interquartile ranges 14–18). Table 1 shows the demographics of the study sample.
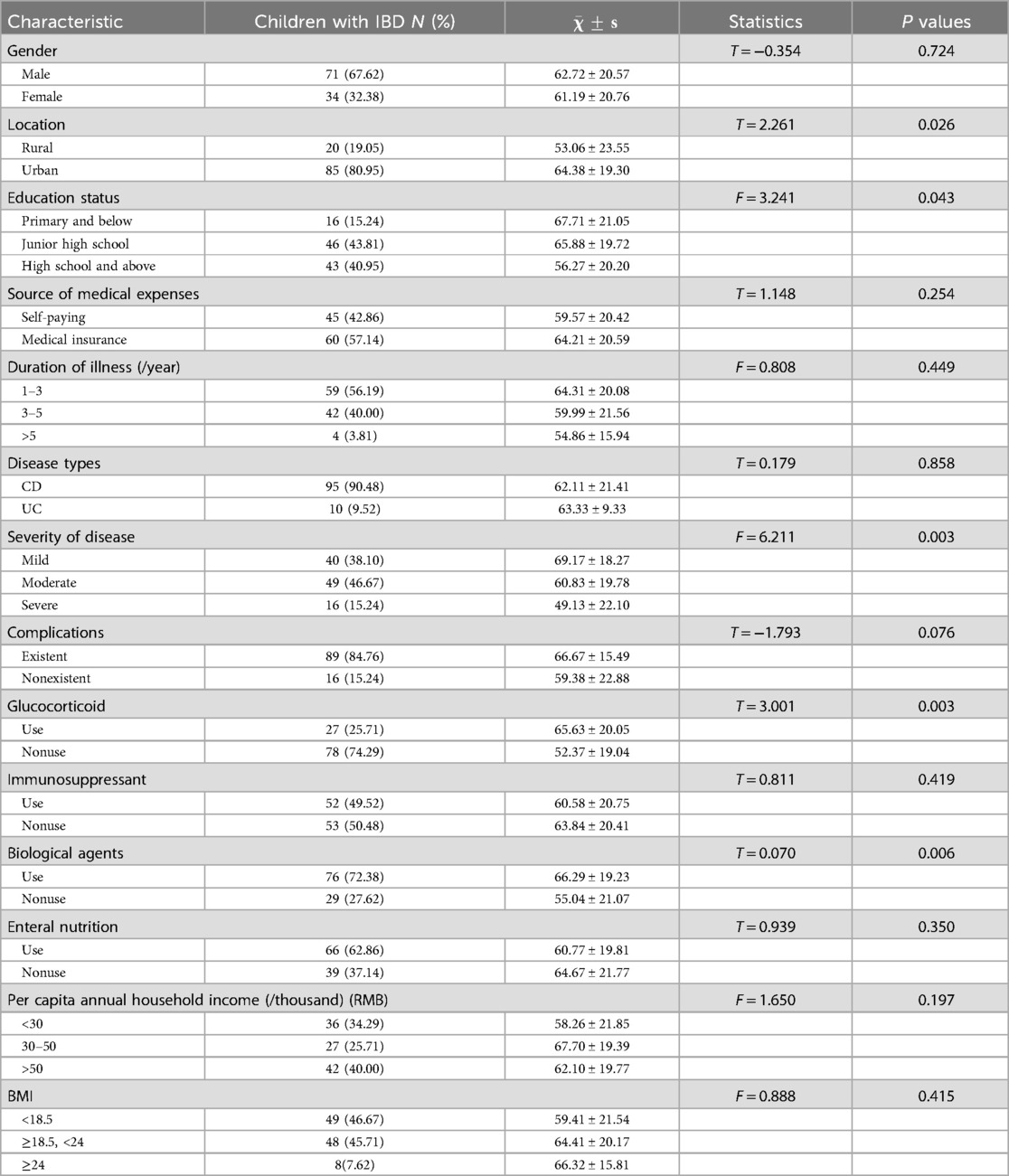
Table 1. Demographic data of cases.
The total score of fatigue in children and adolescents with inflammatory bowel disease was 62.22 ± 20.55, with the lowest score of 11 and the highest score of 100. Among the three dimensions of the questionnaire, the highest average score was 65.16 ± 28.75, which was achieved for the “cognitive fatigue” dimension, whereas the “sleep/rest fatigue” dimension received the lowest average score (60.63 ± 20.07). The level of “general fatigue” was 60.87 ± 24.68 (Table 2).
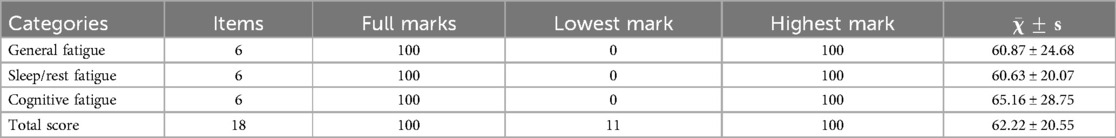
Table 2. Total and individual scores for fatigue dimensions.
The results of the univariate analysis of the degree of fatigue in patients with IBD revealed significant differences according to region, age, disease severity, and use of corticosteroids and biological agents (p < 0.05). No significant differences were found in gender, source of medical expenses, disease course, disease type, immunosuppressants, enteral nutrition use, or per capita annual household income (p > 0.05) (Table 1).
Taking total fatigue as the dependent variable, area, education level, disease severity and glucocorticoid application, and biologic application were significantly different in the univariate analysis, and BMI, which has clinical significance, was incorporated into the multivariate analysis. Reference variables were set for education level, disease severity and body weight, with education status as primary school, disease severity as mild and body weight as reference variables (Table 3). The results revealed that urban residence, nonuse of glucocorticoids and use of biological agents were protective factors against fatigue (p < 0.05), whereas malnutrition, severe disease severity and high school education or above were risk factors for fatigue (p < 0.05) (Table 4).
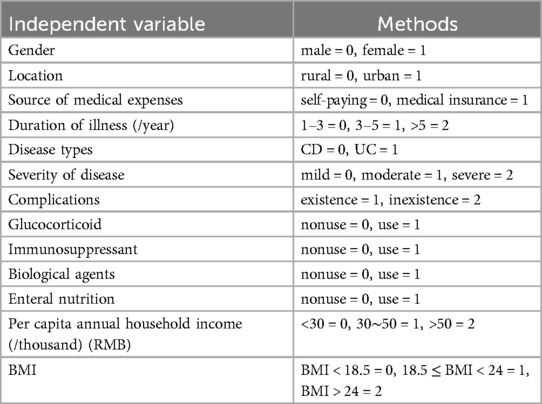
Table 3. Independent variable assignment methods.
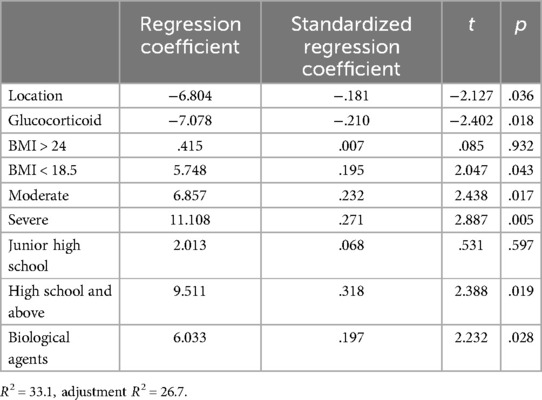
Table 4. Multifactor analysis of factors affecting fatigue.
4 Discussion 4.1 Fatigue in children and adolescents with IBDThe total fatigue score of children with IBD was 62.22 ± 20.55, a value that differed from the results of Lucia (22). This discrepancy might be related to racial differences. Furthermore, Grossman revealed that children with CD of different races reported varying levels of anxiety and fatigue (23).
In this study, the comparison of the scores of various dimensions revealed that sleep/rest fatigue and general fatigue were at higher levels, but cognitive fatigue was at a lower level. The outcomes herein were similar to those of Marcus (11), possibly because patients were more sensitive to physical rather than psychological symptoms. In adult patients with IBD, fatigue is closely related to anxiety, depression, and other emotional symptoms (24). However, the number of relevant studies in children is insufficient, so these cases are easily ignored. These findings suggest that we should pay attention not only to physical fatigue but also to psychological fatigue when managing fatigue in IBD patients.
4.2 Analysis of influencing factors of fatigue in children and adolescents with IBD 4.2.1 Fatigue and regionThis study suggests that the degree of fatigue among children living in cities is lower than that among those living in rural areas. The reason is that the income of the urban population is higher than that of the rural population, and per capita income affects investment in health (25). The health literacy level of urban residents is generally higher than that of rural residents. Moreover, with respect to equal access to basic medical and health services in urban and rural areas, problems such as insufficient total supply and an unbalanced supply structure exist, so rural residents have relatively limited access to public health resources compared with urban residents (26). Therefore, the disease diagnosis and treatment of children living in cities are more timely. Furthermore, parents of children in cities receive more support from communities and schools than do their rural counterparts. Consequently, parents who are urban residents can better master the methods of drug application and management for their children and guide them in symptom management. These parents also pay more attention to and insist on regular follow-up and long-term control, so the fatigue management of their children is more scientific.
In addition to improving access to medical treatment in rural areas, targeted health education should be conducted for children in different areas, with a special emphasis on disease management and fatigue relief in rural children. Furthermore, greater attention should be given to the regular follow-up of children in rural areas to promote scientific symptom management and relieve their fatigue.
4.2.2 Fatigue and ageAge is positively correlated with the degree of fatigue in children and adolescents, which is the same as the findings of Lucia's study of fatigue in children with IBD (22). From the perspective of social psychology, children gradually enter puberty from school age, which is a critical period of growth and development. They face great changes in body and mind and are more sensitive to changes in all aspects of body and mind (27). As the child grows, the understanding of the disease and the perception of symptoms increase. Furthermore, the hospital attendance and disease burden of IBD negatively impact school attendance and then cause school difficulties, consequently producing greater psychological stress to children (28). Negative emotions affect their disease management and aggravate their fatigue.
The needs of children with IBD must be addressed by ensuring effective partnerships between education and health and targeting those with risk factors for poor attendance with preventative measures. The emotional and mental states of adolescent children must be emphasized, and the use of strategies to minimize the healthcare burden and provide more integrated care can directly impact service provision.
4.2.3 Fatigue and drug useChildren treated with biologics had less fatigue than did those not treated with biologics. This finding is similar to the results of the study by Borren (29) which examined the longitudinal trajectory of fatigue in patients who started biotherapy for more than one year and confirmed that fatigue improved with the start of biotherapy and the relief of clinical symptoms. At present, the only biological agent approved for clinical use in China is infliximab, a medication that mainly targets soluble and transmembrane tumor necrosis factor (TNF)-α, which is a powerful proinflammatory cytokine that plays a role in the dysregulation of the mucosal immune response in IBD (30). Thus, infliximab may alleviate fatigue through cytokine action and may also alleviate fatigue by improving clinical symptoms in children.
Children who used glucocorticoids had greater degrees of fatigue than those who did not use them did, and this result was also reached by van Langenberg et al. (31). This finding might be related to the serious side effects of corticosteroids. Corticosteroid treatment can lead to adrenal insufficiency in IBD patients, affect the healing of peptic ulcers, and increase the risk of respiratory tract infection and sepsis (32). Therefore, in the future, in the management of fatigue symptoms in children and adolescents, attention should be given to drug use in children and timely treatment of drug side effects.
4.2.4 Fatigue and BMIBMI is a reliable indicator of protein energy malnutrition and is a simple and feasible method for screening for malnutrition. According to their BMI grades, 46.67% of the children with IBD were malnourished. The present study revealed that the fatigue of malnourished children is more serious than that of other children, an outcome that is the same as that reported by Whelan et al. (33). IBD is associated with anorexia. Typical symptoms include abdominal pain, diarrhea and vomiting. These symptoms further lead to discomfort and loss of appetite. IBD in children often leads to changes in dietary behavior due to hospitalization and dietary restrictions to control gastrointestinal symptoms. By hindering dietary intake, IBD symptoms further aggravate the symptoms of fatigue. Furthermore, many deficiencies in micronutrients, such as iron (34) and vitamin B12 (35), occur in children with IBD. These trace elements are closely related to fatigue symptoms. Therefore, clinical guidelines emphasize the nutritional status of children with IBD and recommend enteral nutrition therapy as a first-line dietary source of CD-induced remission in mild to moderate IBD in children by highlighting regular detection and timely correction of micronutrient levels (33). However, in this study, there was no significant correlation between the use of enteral nutrition and symptoms of fatigue in children. The reason may be related to the time and preparation of enteral nutrition or the size of the sample. A large sample study is needed to determine the relationship between the use or duration of enteral nutrition and symptoms of fatigue in children.
4.2.5 Fatigue and disease severityOur investigation revealed that children with moderate to severe IBD severity are more fatigued than are children with mild severity, an outcome that is similar to that of Pellino (36) but differs from that of Chavarría (37). The sample size of the study and research tool have an impact on the results of the study. Severe diseases are often accompanied by severe clinical symptoms, such as abdominal pain and diarrhea, and the severity of the disease is closely related to children's anxiety, depression, and loneliness (38), indicating that mental factors can directly affect the symptoms of fatigue. Therefore, the severity of illness affects children's fatigue symptoms both physically and psychologically.
4.3 Strengths and limitations of the workThis study directly evaluated fatigue and related variables from the perspective of children and identified multiple factors related to fatigue in IBD patients, providing a reference for further research and eventual clinical application. This work suggested that in addition to actively treating diseases and managing concurrent mental disorders, attention should also be given to children's nutritional status and understanding of diseases, and personalized management methods should be provided.
There are several limitations in this study. First, a cross-sectional survey was adopted in the study. Owing to the drawbacks of the survey method, the causal relationship cannot be determined. In addition, owing to the small sample size, the study results may be affected by confounding factors. This study only investigated 110 cases of pediatric IBD, exceeding the minimum sample size of 82 calculated by G*Power software. However, it is still a small sample study. A small sample size may give rise to significant random errors and elevated false-negative rates, which could result in some fatigue-associated factors being overlooked and excluded from the analysis. The distribution of CDs vs. UCs in the sample is another limitation of this study. This study employed a stringent sampling methodology, encompassing all children with IBD who fulfilled the inclusion criteria from September 1, 2021, to November 31, 2022. This approach ensured the absence of any selection bias. Future studies with larger sample sizes and multiple centers are needed to confirm the relevant conclusions.
5 ConclusionFatigue is common in IBD patients, and several factors contributed to fatigue in our study. To date, the mechanism of fatigue is not clear, and there is no scientific and effective systematic management mode. Therefore, after a comprehensive understanding of fatigue symptoms and their influencing factors in patients with different types of IBD, systematic, comprehensive and targeted interventions should be developed to help patients maximize the improvement of fatigue symptoms, help patients return to society and improve their quality of life.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statementThe studies involving humans were approved by the Ethics Committee of Nanjing Childrens' Hospital affiliated to Nanjing Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributionsYZ: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing, Funding acquisition, Software. JC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. YW: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. WC: Data curation, Methodology, Visualization, Writing – review & editing. ML: Conceptualization, Formal Analysis, Funding acquisition, Resources, Supervision, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
AcknowledgmentsThe authors would like to thank all the study participants and their parents.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2024.1519779/full#supplementary-material
AbbreviationsIBD, inflammatory bowel disease; UC, ulcerative colitis; CD, Crohn's disease; BMI, body mass index; MFS, multidimensional fatigue scale.
References2. Däbritz J, Gerner P, Enninger A, Claßen M, Radke M. Inflammatory bowel disease in childhood and adolescence. Dtsch Arztebl Int. (2017) 114(19):331–8. doi: 10.3238/arztebl.2017.0331
PubMed Abstract | Crossref Full Text | Google Scholar
3. Farrell D, McCarthy G, Savage E. Self-reported symptom burden in individuals with inflammatory bowel disease. J Crohns Colitis. (2016) 10(3):315–22. doi: 10.1093/ecco-jcc/jjv218
PubMed Abstract | Crossref Full Text | Google Scholar
5. Szigethy EM, Allen JI, Reiss M, Cohen W, Perera LP, Brillstein L, et al. White paper AGA: the impact of mental and psychosocial factors on the care of patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. (2017) 15(7):986–97. doi: 10.1016/j.cgh.2017.02.037
PubMed Abstract | Crossref Full Text | Google Scholar
6. Donovan KA, Jacobsen PB, Small BJ, Munster PN, Andrykowski MA. Identifying clinically meaningful fatigue with the fatigue symptom inventory. J Pain Symptom Manage. (2008) 36(5):480–7. doi: 10.1016/j.jpainsymman.2007.11.013
PubMed Abstract | Crossref Full Text | Google Scholar
7. Stjernman H, Tysk C, Almer S, Ström M, Hjortswang H. Worries and concerns in a large unselected cohort of patients with Crohn’s disease. Scand J Gastroenterol. (2010) 45(6):696–706. doi: 10.3109/00365521003734141
PubMed Abstract | Crossref Full Text | Google Scholar
10. Nunes MDR, Jacob E, Bomfim EO, Lopes-Junior LC, de Lima RAG, Floria-Santos M, et al. Fatigue and health related quality of life in children and adolescents with cancer. Eur J Oncol Nurs. (2017) 29:39–46. doi: 10.1016/j.ejon.2017.05.001
PubMed Abstract | Crossref Full Text | Google Scholar
11. Marcus SB, Strople JA, Neighbors K, Weissberg-Benchell J, Nelson SP, Limbers C, et al. Fatigue and health-related quality of life in pediatric inflammatory bowel disease. Clin Gastroenterol Hepatol. (2009) 7(5):554–61. doi: 10.1016/j.cgh.2009.01.022
PubMed Abstract | Crossref Full Text | Google Scholar
12. Ananthakrishnan AN, Kaplan GG, Bernstein CN, Burke KE, Lochhead PJ, Sasson AN, et al. Lifestyle, behaviour, and environmental modification for the management of patients with inflammatory bowel diseases: an international organization for study of inflammatory bowel diseases consensus. Lancet Gastroenterol Hepatol. (2022) 7(7):666–78. doi: 10.1016/S2468-1253(22)00021-8
PubMed Abstract | Crossref Full Text | Google Scholar
13. Gravina AG, Pellegrino R, Durante T, Palladino G, D'Onofrio R, Mammone S, et al. Inflammatory bowel diseases patients suffer from significant low levels and barriers to physical activity: the “BE-FIT-IBD” study. World J Gastroenterol. (2023) 29(41):5668–82. doi: 10.3748/wjg.v29.i41.5668
PubMed Abstract | Crossref Full Text | Google Scholar
14. Van de Vijver E, Van Gils A, Beckers L, Van Driessche Y, Moes ND, van Rheenen PF. Fatigue in children and adolescents with inflammatory bowel disease. World J Gastroenterol. (2019) 25(5):632–43. doi: 10.3748/wjg.v25.i5.632
PubMed Abstract | Crossref Full Text | Google Scholar
15. Gravina AG, Pellegrino R, Palladino G, Imperio G, Ventura A, Cipullo M, et al. Profiling the patient with inflammatory bowel disease in the relationship between physical activity and partner/social network status: a post hoc patient-tailored analysis of the "BE-FIT-IBD" study. Gastroenterol Hepatol. (2024) S0210-5705(24)00161-4. English, Spanish. doi: 10.1016/j.gastrohep.2024.502203
PubMed Abstract | Crossref Full Text | Google Scholar
16. The Subspecialty Group of Gastroenterology, the Society of Pediatrics, Chinese Medical Association, The Subspecialty Group of Clinical Nutrition, the Society of Pediatrics, Chinese Medical Association. Expert consensus on the diagnosis and management of pediatric inflammatory bowel disease (in Chinese). Chin J Pediatr. (2019) 57(7):501–7. doi: 10.3760/cma.j.issn.0578-1310.2019.07.002
Crossref Full Text | Google Scholar
17. Turner D, Otley AR, Mack D, Hyams J, de Bruijne J, Uusoue K, et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology. (2007) 133(2):423–32. doi: 10.1053/j.gastro.2007.05.029
PubMed Abstract | Crossref Full Text | Google Scholar
18. Hyams JS, Ferry GD, Mandel FS, Gryboski JD, Kibort PM, Kirschner BS, et al. Development and validation of a pediatric Crohn’s disease activity index. J Pediatr Gastroenterol Nutr. (1991) 12(4):439–47. doi: 10.1002/j.1536-4801.1991.tb10268.x
PubMed Abstract | Crossref Full Text | Google Scholar
19. Varni JW, Burwinkle TM, Katz ER, Meeske K, Dickinson P. The PedsQL in pediatric cancer: reliability and validity of the pediatric quality of life inventory generic core scales, multidimensional fatigue scale, and cancer module. Cancer. (2002) 94(7):2090–106. doi: 10.1002/cncr.10428
PubMed Abstract | Crossref Full Text | Google Scholar
20. Bu XQ, Ye QM, Liu K, Varni JW, You LM. Formulation of Chinese version of PedsQLTM multidimensional fatigue scale (in Chinese). Modern Clin Nursing. (2014) 13(11):72–5. doi: 10.3969/j.issn.1001-3482.2015.01.25
Crossref Full Text | Google Scholar
21. Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39(2):175–91. doi: 10.3758/BF03193146
PubMed Abstract | Crossref Full Text | Google Scholar
22. Casadonte CJL, Brown J, Strople J, Neighbors K, Fei L, Alonso EM. Low insulin-like growth factor-1 influences fatigue and quality of life in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. (2018) 67(5):616–21. doi: 10.1097/MPG.0000000000002057
PubMed Abstract | Crossref Full Text | Google Scholar
23. Grossman A, Mauer E, Gerber LM, Long MD, Kappelman MD, Gupta N. Black/African American patients with pediatric Crohn’s disease report less anxiety and fatigue than white patients. J Pediatr. (2020) 225:146–51. doi: 10.1016/j.jpeds.2020.05.042
PubMed Abstract | Crossref Full Text | Google Scholar
25. Huang CF, Tang XB, Yang YS. Analysis on the impact of urban and rural residents per capita disposable income to health care expenditure and regional difference (in Chinese). Soft Sci Health. (2017) 31(12):23–7. doi: 10.3969/j.issn.1003-2800.2017.12.001
Crossref Full Text | Google Scholar
26. Liu YO. Realization of equalization of basic medical and health services from the perspective of urban‒rural integrated development (in Chinese). China Economic & Trade Herald. (2021) M(08):86–7. doi: 10.3969/j.issn.1007-9777.2021.23.028
Crossref Full Text | Google Scholar
27. Zhou H, Zhang C, Shen X, Zheng XF, Wu YM, Ying JH. Cancer-related fatigue status and influencing factors in children with acute lymphoblastic leukemia (in Chinese). Chin Nurs Manag. (2021) 21(4):508–11. doi: 10.3969/j.issn.1672-1756.2021.04.007
Crossref Full Text | Google Scholar
28. Ye Y, Manne S, Treem WR, Bennett D. Prevalence of inflammatory bowel disease in pediatric and adult populations: recent estimates from large national databases in the United States, 2007–2016. Inflamm Bowel Dis. (2020) 26(4):619–25. doi: 10.1093/ibd/izz182
PubMed Abstract | Crossref Full Text | Google Scholar
29. Borren NZ, Tan W, Colizzo FP, Luther J, Garber JJ, Khalili H, et al. Longitudinal trajectory of fatigue with initiation of biologic therapy in inflammatory bowel diseases: a prospective cohort study. J Crohns Colitis. (2020) 14(3):309–15. doi: 10.1093/ecco-jcc/jjz148
PubMed Abstract | Crossref Full Text | Google Scholar
30. Hemperly A, Vande Casteele N. Clinical pharmacokinetics and pharmacodynamics of infliximab in the treatment of inflammatory bowel disease. Clin Pharmacokinet. (2018) 57(8):929–42. doi: 10.1007/s40262-017-0627-0
PubMed Abstract | Crossref Full Text | Google Scholar
31. van Langenberg DR, Gibson PR. Factors associated with physical and cognitive fatigue in patients with Crohn’s disease: a cross-sectional and longitudinal study. Inflamm Bowel Dis. (2014) 20(1):115–25. doi: 10.1097/01.MIB.0000437614.91258.70
PubMed Abstract | Crossref Full Text | Google Scholar
32. Blackwell J, Selinger C, Raine T, Parkes G, Smith MA, Pollok R. Steroid use and misuse: a key performance indicator in the management of IBD. Frontline Gastroenterol. (2021) 12(3):207–13. doi: 10.1136/flgastro-2019-101288
PubMed Abstract | Crossref Full Text | Google Scholar
33. Whelan K, Murrells T, Morgan M, Cummings F, Stansfield C, Todd A, et al. Food-related quality of life is impaired in inflammatory bowel disease and associated with reduced intake of key nutrients. Am J Clin Nutr. (2021) 113(4):832–44. doi: 10.1093/ajcn/nqaa395
PubMed Abstract | Crossref Full Text | Google Scholar
35. Huang S, Ma J, Zhu M, Ran Z. Status of serum vitamin B and folate in patients with inflammatory bowel disease in China. Intest Res. (2017) 15(1):103–8. doi: 10.5217/ir.2017.15.1.103
PubMed Abstract | Crossref Full Text | Google Scholar
36. Pellino G, Sciaudone G, Caserta V, Candilio G, De Fatico GS, Gagliardi S, et al. Fatigue in inflammatory bowel diseases: relationship with age and disease activity. Int J Surg. (2014) 12(Suppl 2):S60–3. doi: 10.1016/j.ijsu.2014.08.379
PubMed Abstract | Crossref Full Text | Google Scholar
37. Chavarría C, Casanova MJ, Chaparro M, Barreiro-de Acosta M, Ezquiaga E, Bujanda L, et al. Prevalence and factors associated with fatigue in patients with inflammatory bowel disease: a multi centre study. J Crohns Colitis. (2019) 13(8):996–1002. doi: 10.1093/ecco-jcc/jjz024
Crossref Full Text | Google Scholar
38. Qualter P, Rouncefield-Swales A, Bray L, Blake L, Allen S, Probert C, et al. Depression, anxiety, and loneliness among adolescents and young adults with IBD in the UK: the role of disease severity, age of onset, and embarrassment of the condition. Qual Life Res. (2021) 30(2):497–506. doi: 10.1007/s11136-020-02653-9
留言 (0)