Advances in cardiac surgery over the last few decades have made it possible for over 90% of patients with congenital heart disease (CHD) to reach adulthood, with two-thirds of this population now being adults (1). Thus, the number of adults with congenital heart disease (ACHDs) is expected to increase in the coming years, raising more and more questions about their medical and surgical management. The heterogeneity of this population makes it complex to study. Indeed, ACHDs represent a spectrum of patients, ranging from chronically ill patients from birth, with cardiac and non-cardiac comorbidities and multiple cardiac interventions in their history, to asymptomatic patients whose congenital anomaly was incidentally revealed in adulthood. Regardless of their profile, ACHDs are likely to undergo primary or redo cardiac surgery, and the question arises as to the impact of this surgery on their quality of life as adults.
Quality of life (QoL) is a broad concept of individual wellbeing measured by patient-reported outcomes (PROs) (2). Alongside QoL, PROs enable the study of patients’ perceptions of health and illness, functional status, and psychological functioning. The “Assessment of Patterns of Patient-Reported Outcomes in Adults with Congenital Heart Disease—International Study” (APPROACH-IS) was designed to explore these issues in the ACHD population, using a uniform methodology that could be applied in various regions worldwide (3). The study has revealed geographical variations and provided new insights into the psychological, social, and behavioral factors influencing ACHDs’ QoL (4). However, no centers in Germany took part in this international project.
With the present study, based on elements of the APPROACH-IS methodology, we aimed to investigate the long-term impact of cardiac surgery in adulthood on QoL in patients with CHD from a German Center.
2 Material and methods 2.1 Study designIn this single-center, cross-sectional study, we selected patients with CHD who underwent cardiac surgery at the age of 18 years or older at the German Heart Center Munich between 2004 and 2013. For patients who underwent repeated operations in adulthood, the most recent operation was considered the reference point. Patients who had undergone isolated aortic valve procedures without prior cardiac intervention or operation before the age of 18 years were excluded from the patient selection. Furthermore, patients who had undergone cardiac transplantation, transvenous implantation of a pacemaker or implantable cardioverter-defibrillator (ICD) as an isolated procedure, and non-German-speaking patients were also excluded. Eligible subjects were invited to take part in the study. The recruited patients completed the surveys digitally via the Heartbeat Medical online platform (HRTBT Medical Solutions GmbH, Berlin, Germany). Patients’ clinical data were obtained after a review of the internal medical database.
2.2 Measured outcomesThe severity of CHD was defined according to the Bethesda classification (5). As not all were available in German, the surveys differed slightly from those of the APPROACH-IS (3, 6–12). The following surveys (German version) were selected for the assessment of the corresponding PROs:
1. Perceived health status and life satisfaction:
a. Veterans RAND 12-item mental and physical scores (VR-12)
b. EuroQol 5-Dimension Level (EQ-5D-5l)
c. Satisfaction with Life Scale (SWLS)
2. Psychological functioning (depression and sense of coherence):
a. Patient Health Questionnaire (PHQ-8)
b. Sense of Coherence (SOC-13)
3. Health risk behaviors: Health-Behavior Scale—Congenital Heart Disease (HBS-CHD)
4. Illness perception: Illness Perception Questionnaire-Revised (IPQ-R)
Details of the questionnaires and their scope of investigation are provided in Supplementary Table S1. An additional institutional questionnaire asked the patients about their social and demographic situation, functional status [New York Heart Association (NYHA) score], and subjective improvement in their wellbeing since their last cardiac operation. All questionnaires submitted to patients (in German) are available in the Supplementary Material.
2.3 Statistical analysisContinuous variables were reported as medians with interquartile ranges. Categorical variables were reported as frequencies with percentages. Score results were reported as medians with ranges (minimum–maximum) and mean with standard deviations. Demographic, medical, and surgical factors affecting a relevant percentage of subjects were selected as potential explanatory variables for the variation in score results. These included gender, severity of CHD, number of previous cardiac operations, age at first cardiac operation, age at last cardiac operation, age at study, presence of pacemaker or ICD, anticoagulant and beta-blocker therapy. As the scores of the scales in their original form have varying values and polarities, all scores were rescaled from 0 to 100 (0 being the worst subjective value and 100 being the best) to better illustrate their relationship with the clinical factors. The effect size was estimated using Pearson's correlation coefficient. P-values <0.05 were considered statistically significant.
To refine the granularity of the information reported by this study on ACHDs with different diagnoses and medical histories, we divided the patients into three groups according to the complexity of their primary diagnosis defined by the Bethesda classification: simple, moderate, or severe CHD. A comparison of patient characteristics and PROs between the groups was performed using a Kruskal–Wallis test or a pairwise Fisher's exact test as appropriate.
As absolute score values provide limited information, we compared the data obtained with those available in the literature on healthy subjects. However, the Health-Behavior Scale—Congenital Heart Disease was compared with young adults with CHD (median age 16.3 years), as the questionnaire was not administered to healthy subjects. After selecting studies with documented sample sizes, mean values, and standard deviations of the scores, we compared the results using Welch's t-test (11, 13–17). For the PHQ-8, a two-proportion Z-test was applied for patients reporting a score ≥10, which corresponds to the cut-off point for depression (16). Due to the mismatch between the questionnaires and the geographical diversity, we refrained from statistical comparisons with the APPROACH-IS and only reported its results for information. For better comprehension, the score results have also been rescaled from 0 to 100 for their graphical representation.
Statistical analysis and graphs were conducted and created with R, respectively (R Foundation for Statistical Computing, Vienna, Austria).
2.4 Ethical statementThis study was approved by the Institutional Review Board of the Technical University of Munich (No. 145/20 S-KH on 28/04/2020). All recruited patients consented to the anonymous processing and publication of their data.
3 Results 3.1 Demographic, clinical, and sociodemographic characteristicsAfter pre-selection, according to the criteria set out in the Methods section, 670 subjects were deemed eligible and invited to participate in the study. In total, 196 patients completed the questionnaires (participation rate of 29%). Patient characteristics with between-group comparisons are listed in Table 1. The median age at the time of the study was 43 years (37–53 years), and the median time since the last cardiac operation was 13.4 years (10.6–15.5 years). Approximately half of the patients had undergone more than one cardiac operation in their lifetime (55%). The severity of CHD was evenly distributed. Patients with severe CHD had a notably higher number of previous cardiac surgeries, were younger at the time of their first operation, and had a higher incidence of pacemaker or ICD implantation. Female patients were more represented in the group with simple CHD. The most frequent primary cardiac diagnoses were atrial septal defect (n = 34, 17%), tetralogy of Fallot (n = 22, 11%), and mixed aortic valve disease (n = 11, 6%). The most frequent cardiac procedures in adulthood were patch repair of an atrium septum defect (n = 31, 16%), replacement of a right ventricle-to-pulmonary artery conduit (n = 21, 11%), and mitral valvuloplasty (n = 20, 10%). Supplementary Tables S2, S3 provide complete lists of the patients’ primary cardiac diagnoses and cardiac procedures in adulthood, respectively. The analysis of the following data of the patients who were contacted but did not respond to the questionnaires (n = 474) revealed no statistically significant differences with the study sample: sex (male patients 47% vs. 46%, P = 0.9), age at last heart operation [30 (23–40) vs. 30 (24–41) years, P = 1], age at the time of the study [43 (36–53) vs. 43 (37–53) years, P = 0.9], and complexity of the congenital heart defect according to the Aristotle comprehensive complexity score [9.5 (7.0–11.5) vs. 9.5 (6.2–11.0) points, P = 1, the Bethesda score not being available for these patients].
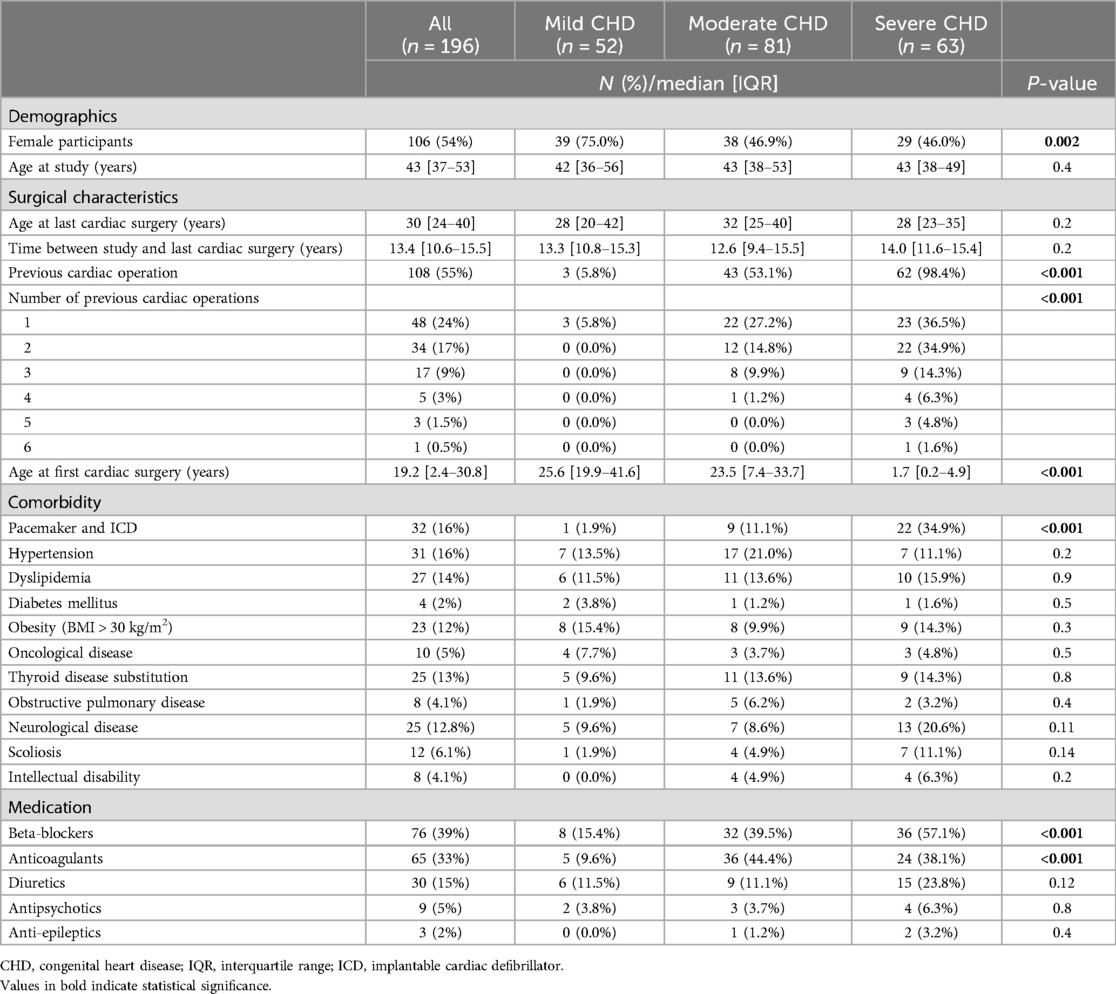
Table 1. Patient characteristics.
Details of sociodemographic characteristics, as reported by the patients, are listed in Table 2. The majority of patients were married or in a partnership (70%), were engaged in a professional activity (85% with full-time or part-time jobs), and had a driver's license (94%). The patients in the group with simple CHD were more likely to be married or in a partnership and had more children than the other two groups.
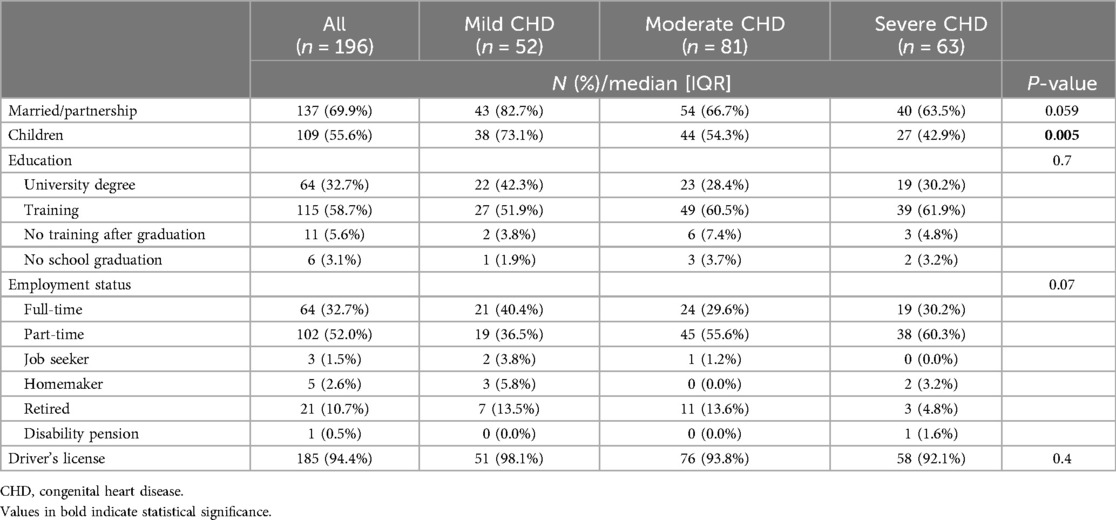
Table 2. Sociodemographic characteristics.
3.2 Patient-reported outcomesScore results are detailed in Table 3 and plotted in Figure 1. According to the institutional questionnaire, most patients reported improved wellbeing after the cardiac operation and were in functional NYHA class I or II. Except for the EQ-5D-5l (visual analog scale, VAS), which was slightly lower for the severe CHD group, the results regarding the patients’ perceived health status and life satisfaction, psychological functioning, and health risk behaviors were similar between the patient groups. Illness perception showed the most significant variation between the groups, with patients with severe CHD reporting significantly inferior results in all items except “Personal Control.”
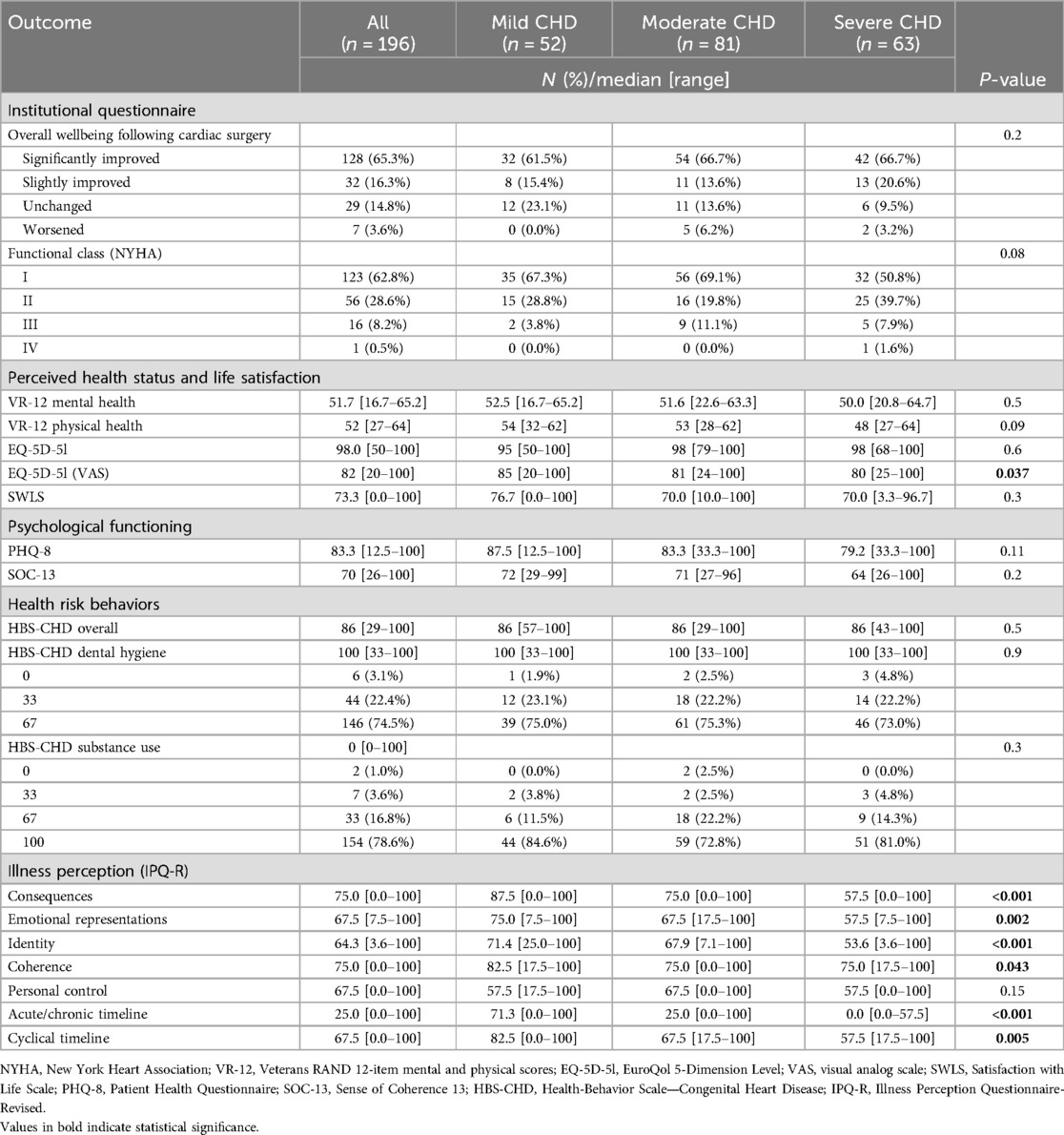
Table 3. Patient-reported outcomes.
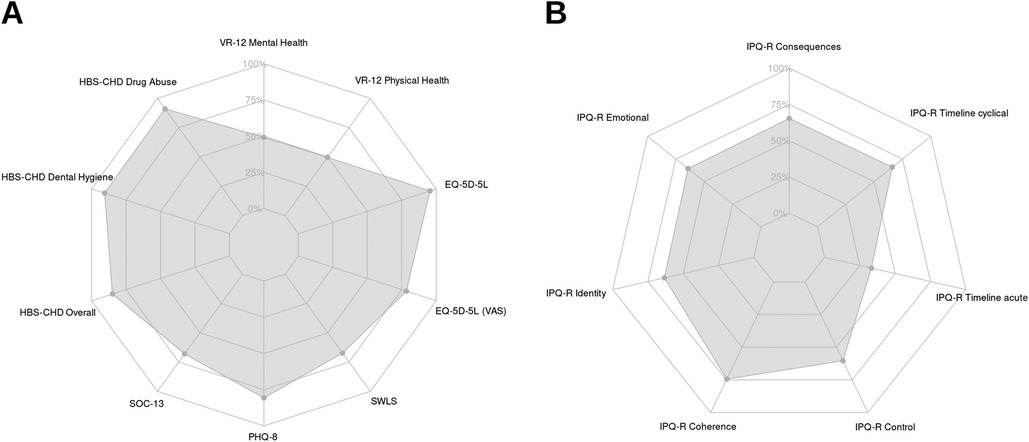
Figure 1. Radar chart of the patient-reported outcomes, rescaled from 0 to 100 (0 being the worst subjective value and 100 being the best). (A) Perceived health status and life satisfaction, psychological functioning, and health risk behaviors; (B) illness perception. VR-12, Veterans RAND 12-item mental and physical scores; EQ-5D-5l, EuroQol 5-Dimension Level; VAS, visual analog scale; SWLS, Satisfaction with Life Scale; PHQ-8, Patient Health Questionnaire; SOC-13, Sense of Coherence 13; HBS-CHD, Health-Behavior Scale—Congenital Heart Disease; IPQ-R, Illness Perception Questionnaire-Revised; CHD, congenital heart disease.
3.3 Correlation of scores with clinical factorsThe results of the correlation analysis are depicted in Figure 2. Older age at last cardiac surgery, older age during the study, having a pacemaker, and beta-blocker medication were all associated with worse perceived physical health. Aging was associated with better perceived mental health and greater coherence. Female patients reported significantly lower risks in overall health behavior and dental hygiene.
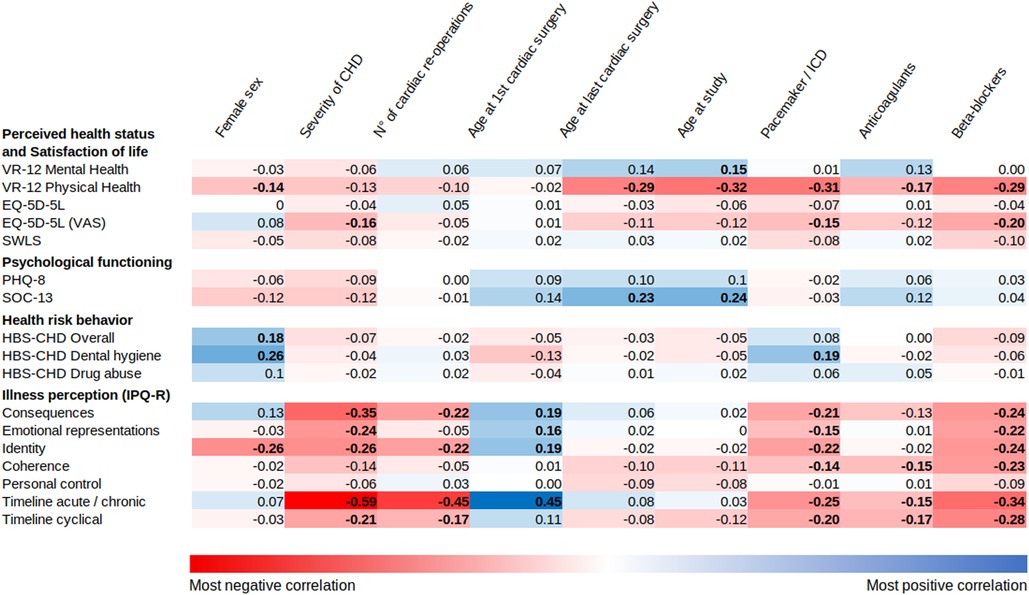
Figure 2. Correlations between clinical factors and the patient-reported outcomes rescaled from 0 to 100. The coefficients (r) from Pearson's correlation test are displayed. Positive correlations are highlighted in blue and negative correlations in red. Bold values indicate a significant P-value.
Of all the factors, the PROs from the IPQ-R showed the most remarkable occurrence of statistically significant associations with the investigated variables, especially the “Consequences” (i.e., the believed impact of the disease on various aspects of the patient's life), “Timeline acute/chronic” (i.e., the perceived duration of the disease), and “Identity” (i.e., the symptoms the patient attributes to the illness) items. The severity of CHD, number of previous cardiac operations, and beta-blocker medication had the strongest substantial negative correlations with illness perception. In contrast, older age at first cardiac surgery had the most significant positive correlation.
3.4 Comparison with representative samplesDetails of the comparison of patient-reported outcomes with representative samples are listed in Table 4, and the results are plotted in Figure 3. The study population presented significantly better physical health perceptions and a sense of coherence than the available data on healthy subjects. Furthermore, the data showed a lower risk of dental hygiene compared with the selected sample of young adults with CHD. The results reported by APPROACH-IS for scores equivalent to our study are also listed in Table 4 as a reference.
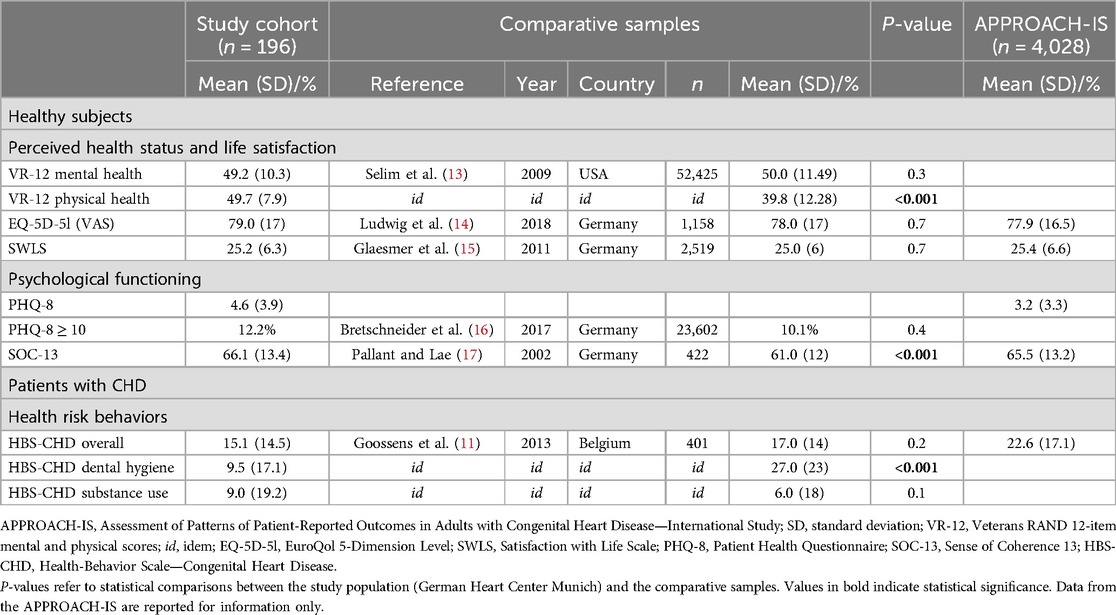
Table 4. Comparison of patient-reported outcomes with representative samples.
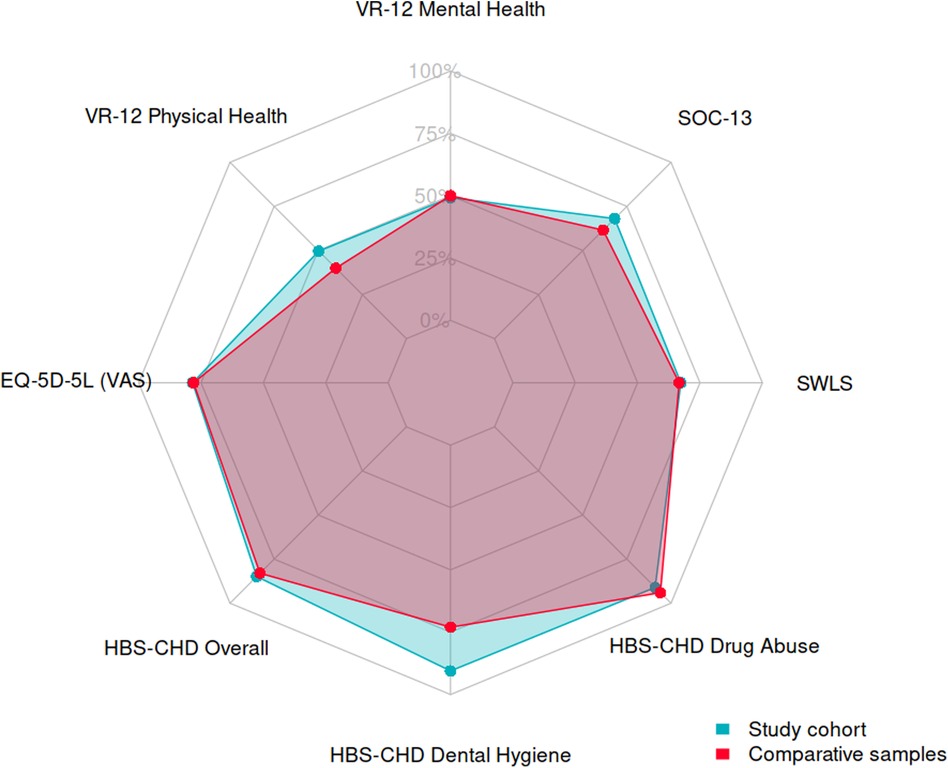
Figure 3. Radar chart comparing the patient-reported outcomes between the study cohort (blue) and selected samples (red), with scores rescaled from 0 to 100. VR-12, Veterans RAND 12-item mental and physical scores; EQ-5D-5l, EuroQol 5-Dimension Level; SWLS, Satisfaction with Life Scale; PHQ-8, Patient Health Questionnaire, SOC-13, Sense of Coherence 13; HBS-CHD, Health-Behavior Scale—Congenital Heart Disease.
4 DiscussionIn this study, we aimed to assess the long-term QoL of patients with CHD after cardiac surgery in adulthood. Upon direct inquiry, the majority of patients reported a subjective improvement in their wellbeing after the cardiac operation. Perceived health status, life satisfaction, and psychological functioning were comparable to those of healthy subjects from Germany and other countries, as were the health risk behaviors compared to a representative sample of young adults with CHD. Of all the measured outcomes, illness perception was the most influenced by the investigated clinical factors, predominantly by the severity of CHD.
With more than 4,000 patients recruited from 15 different countries, the APPROACH-IS has provided rich information on the subjective wellbeing of ACHDs and their correlates (4). Medical, demographic, behavioral, psychological, and social factors were identified. Social factors appeared to be notably complex, involving individual (e.g., partnership, educational level, and employment status) and contextual elements (e.g., healthcare system resources and performance). Moreover, the study showed that the relative contribution of each factor varies between countries and cultures (18). Considering the results reported by the APPROACH-IS, QoL in our study cohort was within the international range. More importantly, the QoL of our patients several years after cardiac surgery was also equivalent to that of healthy subjects. This information must be considered when advising ACHDs who are undergoing primary or redo surgery and should also be familiar to their attending cardiologists. As a surgeon, one is often confronted with the reluctance of patients and/or their attending cardiologist to proceed with surgery when it is formally indicated. One of the reasons for this reluctance is the fear of loss of quality of life associated with cardiac surgery. However, postponing surgery is detrimental to cardiac function and may lead to higher morbidity and mortality (19). Our study showed that a population of CHD patients who underwent cardiac surgery in adulthood reported a good quality of life and subjective improvement of wellbeing following the operation. These observations should reassure the patients concerned and their attending cardiologist, limiting postponed operations and their harmful consequences.
Nevertheless, the shortcomings of these estimates and their limited discriminatory power should be noted. The results from the illness perception questionnaire remind us of the impact of the disease on the daily life of these patients, which may be insufficiently captured by QoL questionnaires. In line with other studies, we found that the severity of CHD is a crucial determinant of illness perception: the more severe the disease, the worse the illness perception (20, 21). The significant correlations observed between outcomes and disease severity suggest that the underlying disease confounds clinical factors such as the number of cardiac reoperations and cardiac comorbidities, which are more prevalent in patients with severe CHD. Moreover, the resilience—in this case, the ability to accept an impaired health status and adapt positively—of patients born with a congenital disease is a well-known phenomenon, whose influence on psychometric tests makes a comparison of the outcomes with healthy subjects problematic. As an illustration, Moons P. et al. demonstrated that a sense of coherence, a representative measure of resilience, positively influenced QoL in ACHDs, with substantial inter-country variation (22).
A methodological advantage of the APPROACH-IS protocol is that it covers a wide range of PROs whose items are conceptually clearly defined, and enables comparisons to be made thanks to its uniform nature. Nevertheless, not all aspects are covered by this protocol. In our study of patients who had undergone cardiac surgery in previous years, no questionnaire specifically addressed the issue of pain and functional status in the region of the sternotomy (or of any peripheral cannulation) or cosmetic considerations regarding the appearance of the scar. Similarly, social aspects were poorly investigated, and we have created an institutional questionnaire to compensate for this lack of information. Economic status, the influence of which on the quality of life in ACHDs has been documented by other authors, was also not analyzed (23). Finally, this protocol, like all questionnaires investigating patient subjectivity, is not free from measurement bias. We have already mentioned resilience in the chronically ill; inter-sex variations in the impact of symptoms on daily life, cognitive status, and any psychological disorders are other parameters with little or no measurability that may also have affected the results (24).
In any case, the generally good QoL in our cohort should not eclipse the occasional poor outcomes that reflect the distress experienced by the most severely ill patients. These cases should be acknowledged and, if necessary, addressed with appropriate diagnostic and therapeutic interventions. Specific studies of the most severely ill patients, such as those with univentricular hearts, have revealed lower QoL and more negative illness perceptions (21). To address this issue, we are conducting a study on the QoL of adult patients with Fontan circulation who were operated on at our center (25).
This study was limited by its single-center design, the number of participants, and their heterogeneous diagnoses and interventions. The samples selected for the comparative analysis are also heterogeneous and limited to the data available in the literature. Nevertheless, our aim was not to draw broadly applicable conclusions comparing ACHDs to healthy individuals, but to provide insights specific to an under-researched German cohort focusing on surgical outcomes.
5 ConclusionsSeveral years after cardiac surgery in adulthood, adults with congenital heart disease reported a subjective improvement in their wellbeing, a life satisfaction comparable to that of healthy individuals, and low health risk behaviors. Illness perception strongly correlated with the severity of the underlying congenital heart disease.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by the Institutional Review Board of the Technical University of Munich. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsTS: Formal Analysis, Methodology, Writing – original draft. PB: Data curation, Investigation, Writing – review & editing. DK: Writing – review & editing. OT: Supervision, Writing – review & editing. PH: Writing – review & editing. MO: Writing – review & editing. JC: Writing – review & editing. JP: Methodology, Project administration, Supervision, Writing – review & editing. JH: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing.
FundingThe authors declare that no financial support was received for the research, authorship and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2024.1501680/full#supplementary-material
AbbreviationsCHD, congenital heart disease; ACHDs, adults with congenital heart disease; QoL, quality of life; APPROACH-IS, Assessment of Patterns of Patient-Reported Outcomes in Adults with Congenital Heart Disease—International Study; VR-12, Veterans RAND 12-item mental and physical scores; EQ-5D-5l, EuroQol 5-Dimension Level; VAS, visual analog scale; SWLS, Satisfaction with Life Scale; PHQ-8, Patient Health Questionnaire; SOC-13, Sense of Coherence 13; HBS-CHD, Health-Behavior Scale—Congenital Heart Disease; IPQ-R, Illness Perception Questionnaire-Revised.
References1. Moons P, Bovijn L, Budts W, Belmans A, Gewillig M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation. (2010) 122(22):2264–2272. doi: 10.1161/CIRCULATIONAHA.110.946343
PubMed Abstract | Crossref Full Text | Google Scholar
2. Acquadro C, Berzon R, Dubois D, et al. Incorporating the patient’s perspective into drug development and communication: an ad hoc task force report of the patient-reported outcomes (PRO) harmonization group meeting at the Food and Drug Administration, February 16, 2001. Value Heal. (2003) 6(5):522–531. doi: 10.1046/j.1524-4733.2003.65309.x
Crossref Full Text | Google Scholar
3. Apers S, Kovacs AH, Luyckx K, et al. Assessment of patterns of patient-reported outcomes in adults with congenital heart disease—international study (APPROACH-IS): rationale, design, and methods. Int J Cardiol. (2015) 179(20130607):334–342. doi: 10.1016/j.ijcard.2014.11.084
PubMed Abstract | Crossref Full Text | Google Scholar
4. Moons P, Luyckx K, Kovacs AH. Patient-reported outcomes in adults with congenital heart disease: what have we learned from APPROACH-IS? Int J Cardiol Congenit Hear Dis. (2021) 2:100074. doi: 10.1016/j.ijcchd.2020.100074
Crossref Full Text | Google Scholar
5. Warnes CA, Liberthson R, Danielson GK, et al. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. (2001) 37(5):1170–1175. doi: 10.1016/S0735-1097(01)01272-4
PubMed Abstract | Crossref Full Text | Google Scholar
6. Buchholz I, Feng YS, Buchholz M, Kazis LE, Kohlmann T. Translation and adaptation of the German version of the Veterans Rand—36/12 item health survey. Health Qual Life Outcomes. (2021) 19(1):1–16. doi: 10.1186/s12955-021-01722-y
PubMed Abstract | Crossref Full Text | Google Scholar
9. Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. (2009) 114(1-3):163–173. doi: 10.1016/j.jad.2008.06.026
PubMed Abstract | Crossref Full Text | Google Scholar
11. Goossens E, Luyckx K, Mommen N, et al. Health risk behaviors in adolescents and emerging adults with congenital heart disease: psychometric properties of the health behavior scale-congenital heart disease. Eur J Cardiovasc Nurs. (2013) 12(6):544–557. doi: 10.1177/1474515113475934
PubMed Abstract | Crossref Full Text | Google Scholar
12. Gaab J, Latanzia-Bunschoten S, Sprott H. (2008) Illness perception questionnaire. In: Diagnostische Verfahren in der Rehabilitation. Göttingen: Hogrefe (2008). p. 109–11.
13. Selim AJ, Rogers W, Fleishman JA, et al. Updated U.S. population standard for the veterans RAND 12-item health survey (VR-12). Qual Life Res. (2009) 18(1):43–52. doi: 10.1007/s11136-008-9418-2
PubMed Abstract | Crossref Full Text | Google Scholar
15. Glaesmer H, Grande G, Braehler E, Roth M. The German version of the satisfaction with life scale (SWLS) psychometric properties, validity, and population-based norms. Eur J Psychol Assess. (2011) 27(2):127–132. doi: 10.1027/1015-5759/a000058
Crossref Full Text | Google Scholar
16. Bretschneider J, Kuhnert R, Hapke U. Depressive symptomatik bei erwachsenen in Deutschland. J Heal Monit. (2017) 2(3):81–88. doi: 10.17886/RKI-GBE-2017-058
Crossref Full Text | Google Scholar
17. Pallant JF, Lae L. Sense of coherence, well-being, coping and personality factors: further evaluation of the sense of coherence scale. Pers Individ Dif. (2002) 33(1):39–48. doi: 10.1016/S0191-8869(01)00134-9
Crossref Full Text | Google Scholar
18. Moons P, Kovacs AH, Luyckx K, et al. Patient-reported outcomes in adults with congenital heart disease: inter-country variation, standard of living and healthcare system factors. Int J Cardiol. (2018) 251:34–41. doi: 10.1016/j.ijcard.2017.10.064
PubMed Abstract | Crossref Full Text | Google Scholar
19. Beurtheret S, Tutarel O, Diller GP, et al. Contemporary cardiac surgery for adults with congenital heart disease. Heart. (2017) 103(15):1194–1202. doi: 10.1136/heartjnl-2016-310384
PubMed Abstract | Crossref Full Text | Google Scholar
20. Rassart J, Apers S, Kovacs AH, et al. Illness perceptions in adult congenital heart disease: a multi-center international study. Int J Cardiol. (2017) 244:130–138. doi: 10.1016/j.ijcard.2017.06.072
PubMed Abstract | Crossref Full Text | Google Scholar
21. Holbein CE, Fogleman ND, Hommel K, et al. A multinational observational investigation of illness perceptions and quality of life among patients with a Fontan circulation. Congenit Heart Dis. (2018) 13(3):392–400. doi: 10.1111/chd.12583
PubMed Abstract | Crossref Full Text | Google Scholar
22. Moons P, Apers S, Kovacs AH, et al. Sense of coherence in adults with congenital heart disease in 15 countries: patient characteristics, cultural dimensions and quality of life. Eur J Cardiovasc Nurs. (2021) 20(1):48–55. doi: 10.1177/1474515120930496
PubMed Abstract | Crossref Full Text | Google Scholar
23. Barreda RL, Guerrero A, De la Cuadra JC, et al. Poverty, quality of life and psychological wellbeing in adults with congenital heart disease in Chile. PLoS One. (2020) 15(10):1–12. doi: 10.1371/journal.pone.0240383
Crossref Full Text | Google Scholar
24. Moons P. Patient-reported outcomes in congenital cardiac disease: are they as good as you think they are? Cardiol Young. (2010) 20(Suppl 3):143–148. doi: 10.1017/S1047951110001216
留言 (0)