Ziconotide is a non-opioid analgesic that has contributed to a paradigm shift in pain treatment. It is a synthetic derivative of ω-Conotoxin MVIIA found in the venom of the marine snail Conus magus. The molecule consists of 25 amino acids containing 6 cysteine residues linked by three disulfide bridges that fold the structure and produce the characteristic 3D structure that is critical for its mechanism of action based on the selective blockade of N-type voltage-gated calcium channels (Cav2.2) (Brookes et al., 2017). These channels play a crucial role in the release of neurotransmitters, such as glutamate and substance P, responsible for pain transmission (Zamponi et al., 2015; Moore and McCrory, 2017).
Several cases of ziconotide-treated patients experiencing adverse effects, particularly neuropsychiatric symptoms, have been reported in the literature, including confusion, disorientation, decreased alertness, somnolence, drowsiness, hallucinations or other changes in perception and mood. These symptoms were already known from early clinical trials, and can last for as long as ziconotide is administered and for up to 2 weeks after discontinuation, although in some cases they may persist (Smith and Deer, 2009).
Indeed, there are some patient profiles that are more prone to experience these side effects, such as those with pre-existing psychiatric disorders (Smith and Deer, 2009). However, since this drug is usually prescribed by non-mental healthcare professionals, psychiatric symptoms are described briefly and vaguely as ‘hallucinations’ or ‘confusion.’ Thus, such a non-specific symptoms could be compatible with diagnoses as diverse as delirium or psychosis.
Despite the knowledge of the mechanism of action of the ziconotide and its association with neuropsychiatric adverse effects, there is a gap in the literature regarding the underlying physiological mechanisms. Although some hypotheses suggest that psychotic symptoms may be favored by the blockade of Cav2.2 in the prefrontal cortex and its relationship with dopaminergic neurotransmission (Burdge et al., 2018), no work has explored a specific pathway that may be involved in the appearance of these symptoms.
Therefore, our aim is to describe, from a novel psychiatric perspective, a ziconotide-induced psychotic episode with a wide range of neuropsychiatric symptoms. At the same time, this case report allowed a scoping review to analyze the clinical diversity of other published cases and to hypothesize about possible specific pathways associated with these adverse symptoms.
2 MethodsThis case report was selected and described by the same mental health professionals that attended the patient. For this purpose, consent was requested from the patient herself and her relatives to obtain data from the clinical history.
Subsequently, a scoping review was conducted following the criteria of the PRISMA-ScR Statement, which was registered in the Open Science Framework (doi: 10.17605/OSF.IO/7C8RQ). A systematic review was completed on December 11, 2023, in the Web of Science, Pubmed and Embase databases. This combination was used because it ensured a recall of almost 96% of the papers (Bramer et al., 2017).
The terms chosen for the search were: ziconotide AND (psycho* OR delirium OR hallucination OR delusion). No filter was added, but the field code /exp was added to these terms in Embase to search for the related narrower or child terms. The references obtained (Figure 1) were entered into the systematic review management software COVIDENCE. The PICOS (participants, intervention, context, outcomes, and study design) framework was used to establish eligibility criteria. Two reviewers analyzed independently the results obtained according to the inclusion and exclusion criteria, and the resulting discrepancies were resolved by a third reviewer.
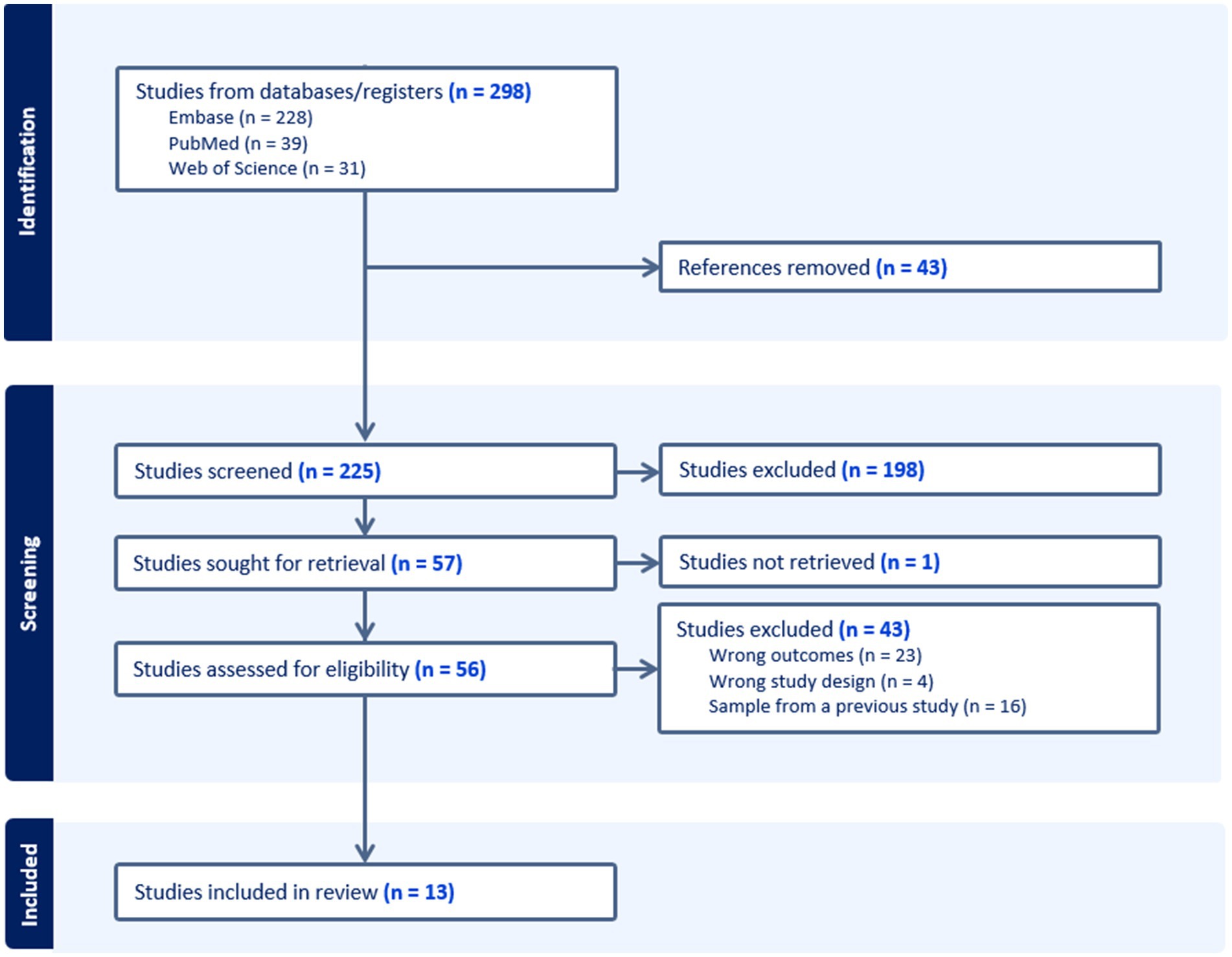
Figure 1. PRISMA flow diagram of study selection.
As inclusion criteria, case reports or case series were considered, whether in the form of an article, posters or oral communication, which included patients treated with ziconotide and who had presented psychosis, hallucinations, delusions or delirium. As exclusion criteria, we rejected those studies in which the psychopathology could not be clearly attributed to ziconotide, considering that the use of opioids can lead to confusional or even psychotic symptoms; studies that only provide the prevalence of neuropsychiatric adverse effects, but do not examine in depth the course of the disease itself; those cases in which there was a history of psychiatric disorders; and those studies whose language was not English or Spanish. The results of the studies obtained were grouped according to the clinical presentation and/or reported symptomatology (hallucinations, delirium, psychosis or delirium).
3 Results 3.1 Case presentationThe patient was a 54-year-old woman who was admitted to the psychiatric emergency room for auditory verbal hallucinations that began a few weeks earlier. Concretely, she felt that her son and his partner were talking about her and insulting her through speakers.
Her medical history included hypothyroidism and a thoracic sarcomatoid mesothelioma diagnosed in November 2010, with multiple recurrences in the following 12 years and secondary chronic refractory pain since 2011. At the time of her consultation in the psychiatric emergency room (2023), the patient was suffering from radicular syndrome under palliative treatment with intrathecal pump of morphine 2% (19 mL) and ziconotide 100 μg/day, she had fentanyl 100 μg rescues every 72 h. The rest of her usual treatment included lormetazepam 2 mg at night, lacosamide 200 mg every 12 h, levothyroxine 50 μg every morning and metamizole 575 mg on demand.
Regarding her psychiatric history, she has suffered from dysthymia since 2006 and had been treated with escitalopram 10 mg and alprazolam 0.5 mg until 2013, when she discontinued them.
On initial psychiatric evaluation, the patient was conscious but disoriented as to time, place, and person. Her appearance was cachectic, and her attitude was suspicious and distressed. Slow thinking was noted as well as incoherent and derailed speech evidencing delusions of prejudice toward his son and his partner. The patient also described self-references, being spied on through electronic devices, and false recognition phenomena. Moreover, she admitted to having complex visual hallucinations (human figures), gustatory (dysgeusia) and olfactory (parosmia). The patient also had a long history of depressed mood in response to the prolonged oncologic process, with passive suicidal ideation, hyporexia, and insomnia.
Complementary tests, brain CT and chest X-ray showed no significant findings of oncologic progression. Toxicological analysis was positive for morphine and benzodiazepines, compatible with her usual medication. Family members reported that the only significant change prior to her current situation was the adjustment of analgesic medication 8 days before due to inadequate pain control, increasing ziconotide from 0.2 µg/day to a total dose of 7.5 µg/day.
The patient was admitted to the psychiatric ward, where she presented gait instability, tremor, and fluctuation of temporal and spatial orientation during the first days of admission. She maintained a certain level of uneasiness and suspicion with her relatives and healthcare professionals, introducing them to her delusions of harm, and having episodes of hostility that required the administration of intramuscular haloperidol and five-point mechanical restraint to ensure her own safety. Olanzapine (15 mg/day) was initiated, but the patient continued with delusional, hallucinatory, false recognitions and mumbling speech.
Considering the complex clinical picture, the possibility of organic psychosis or psychosis induced by some of her usual treatments was suggested, as this picture was compatible with the adverse effects of ziconotide. Given the clinical suspicion, a progressive reduction of intrathecal ziconotide was agreed with the Pain Management Unit until discontinuation.
As the dose of ziconotide was reduced, the psychotic symptoms disappeared, until they completely resolved 48 hours after drug withdrawal. After 12 days of hospitalization, the condition was classified as a ziconotide-induced psychotic episode. The dose of olanzapine was reduced to 5 mg and the patient was referred to the Pain Unit for pain control, where the antipsychotic was eventually discontinued without recurrence of delusional symptoms.
3.2 Scoping reviewA total of 13 papers (9 case reports, 4 case series) were included in this scoping review (Burdge et al., 2018; Su et al., 2021; Phan and Waldfogel, 2015; Whitlow et al., 2015; Abdelsayed et al., 2022; Stewart and Sarria, 2014; Kapural et al., 2009; Ayuga-Loro et al., 2011; Obafemi and Roth, 2013; Grajny et al., 2020; de la Calle Gil et al., 2015; Levin et al., 2002; Penn and Paice, 2000). They included 30 cases of patients with ziconotide who presented adverse effects, 21 of which consisted of neuropsychiatric symptoms (Table 1).
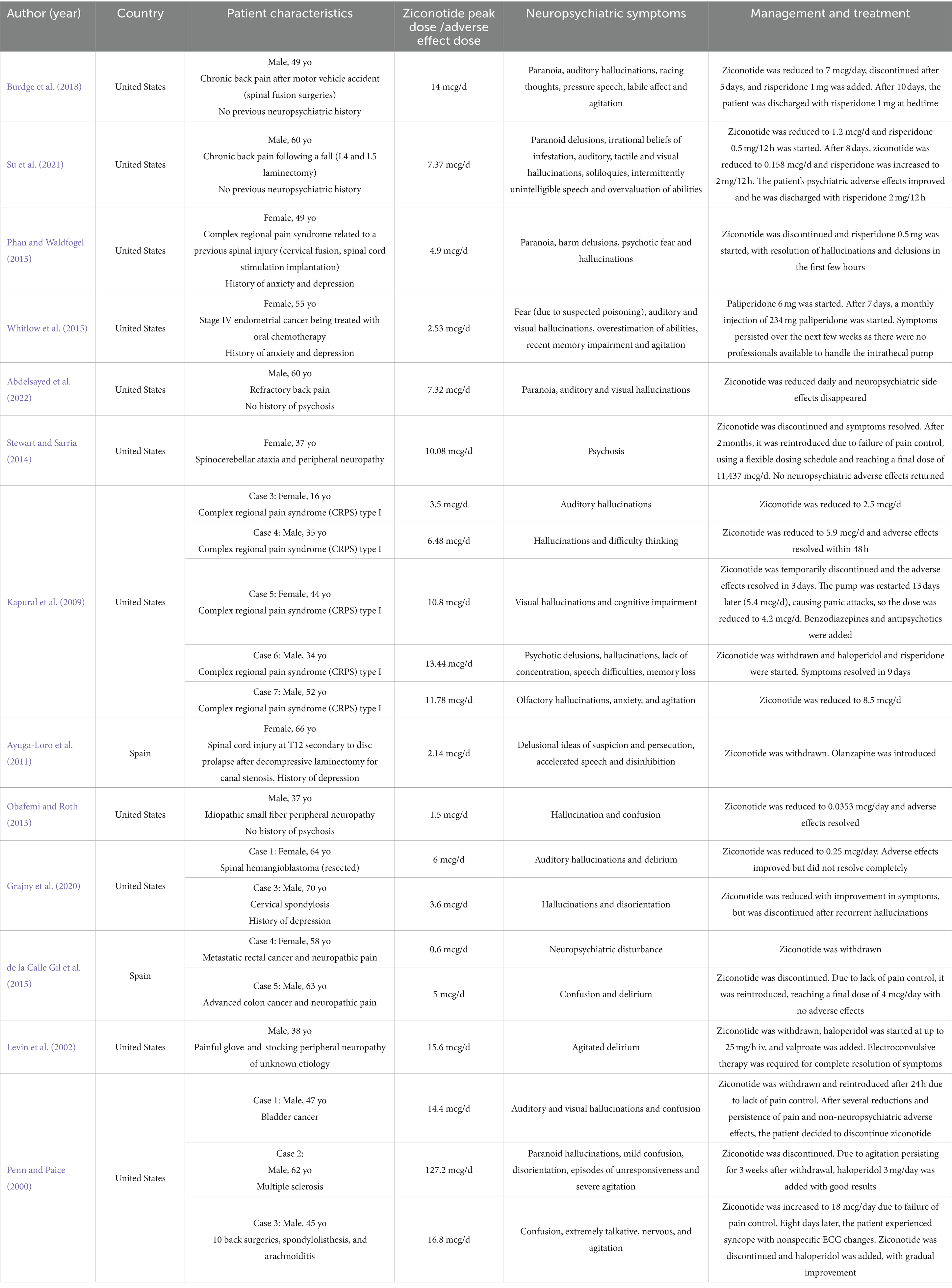
Table 1. Summary table of ziconotide case report characteristics.
Considering the data in the table, it can be seen that most of the studies are from the United States. There is a male predominance in the occurrence of adverse effects (13 men vs. 8 women). Among the studies that recorded psychiatric antecedents (Burdge et al., 2018; Su et al., 2021; Phan and Waldfogel, 2015; Whitlow et al., 2015; Abdelsayed et al., 2022; Ayuga-Loro et al., 2011; Obafemi and Roth, 2013; Grajny et al., 2020), half of the patients had them (Phan and Waldfogel, 2015; Whitlow et al., 2015; Ayuga-Loro et al., 2011; Grajny et al., 2020) and the other half did not (Burdge et al., 2018; Bramer et al., 2017; Abdelsayed et al., 2022; Obafemi and Roth, 2013). On the other hand, the doses at which the adverse effects occurred were highly variable, ranging from a minimum of 0.6 mcg/d (Levin et al., 2002) to a maximum of 127.2 mcg/d (Webster, 2015).
In 7 patients the presentation was described as a “psychosis” (Burdge et al., 2018; Su et al., 2021; Phan and Waldfogel, 2015; Whitlow et al., 2015; Abdelsayed et al., 2022; Stewart and Sarria, 2014; Kapural et al., 2009), with auditory hallucinations and paranoid delusions in 5 of them (Burdge et al., 2018; Su et al., 2021; Phan and Waldfogel, 2015; Whitlow et al., 2015; Abdelsayed et al., 2022), and visual hallucinations in 3 cases (Su et al., 2021; Whitlow et al., 2015; Abdelsayed et al., 2022). However, in Stewart and Sarria (2014) the symptoms of the psychotic episode were not specified and in Kapural et al. (2009) they spoke of “psychotic delusions and hallucinations.” In addition to the above, one case had psychotic (delusions of persecution, suspiciousness) and mania-like symptoms (verbosity, disinhibition) (Ayuga-Loro et al., 2011). Continuing with hallucinations, these also occurred in isolation, with one case describing auditory hallucinations, another visual hallucinations, and yet another unspecified hallucinations (Kapural et al., 2009).
Additionally, 4 patients presented delirium, either with auditory and visual hallucinatory symptoms (Obafemi and Roth, 2013), auditory only (Grajny et al., 2020), or without any psychiatric symptoms (de la Calle Gil et al., 2015; Levin et al., 2002). Although not named as such in the cases, 5 patients presented symptoms suggestive of delirium (agitation and disorientation alternating with unresponsiveness, confusion…), either with visual and auditory hallucinations (Penn and Paice, 2000), olfactory hallucinations (Kapural et al., 2009), or unspecified hallucinations (Grajny et al., 2020), or without them (Penn and Paice, 2000).
The most important strategies for the management of neuropsychiatric symptoms have been the reduction and discontinuation of ziconotide. In turn, several studies have added the use of antipsychotics, the most common being risperidone (Burdge et al., 2018; Su et al., 2021; Phan and Waldfogel, 2015; Kapural et al., 2009) and haloperidol (Kapural et al., 2009; Levin et al., 2002; Penn and Paice, 2000). Finally, electroconvulsive therapy has been used as a strategy (Levin et al., 2002).
4 DiscussionThe case report presented is of particular interest because it shows almost the totality of the adverse effects produced by ziconotide, providing an opportunity to reflect on its action on Cav2.2, the distribution of these channels and the relationship of all this with the aforementioned adverse effects.
Previous studies have estimated that 12% of patients treated with ziconotide have hallucinations, 3% have paranoid reactions, and 1–2% have psychosis. In addition, it has also been shown to increase the incidence of suicidality, suicide attempts, and suicidal ideations. From a neurological point of view, up to 33% may present confusion and 2% delirium (Webster, 2015). As in our case report, most of the published cases present auditory hallucinations and paranoid delusions, being generally classified as psychosis. However, the clinical overlap with delirium is striking. In this sense, a larger number of cases may not have been classified as psychosis because they are not usually described by psychiatrists, leaving psychopathology and diagnostic judgment in the background. Thus, our case report presents a psychiatric perspective that enriches the debate on the adverse neuropsychiatric effects of ziconotide.
On the other hand, the non-specificity and variety of symptoms may be due to the mechanism of action of ziconotide, which would be involved in the pathophysiological pathways responsible for symptoms of psychosis and delirium. This possibility is supported by the fact that individuals with a history of psychiatric disorders are more susceptible to ziconotide-induced adverse effects (Poli and Ciaramella, 2011), as it happens in our case report, where the patient presents dysthymia of years of evolution. That common susceptibility would be in line with the Research Domain Criteria (RDoC) approach (Cuthbert and Insel, 2013).
It has been observed that cannabinoid receptor 1 (CB1R) mediated inhibition of Cav2.2 presynaptic channels is able to suppress GABA release (a phenomenon known as depolarization-induced suppression of inhibition) (Lozovaya et al., 2009; Borgan et al., 2021). As a consequence, there is an augmentation in presynaptic dopamine in areas with an increased presence of CB1R in GABAergic neurons, such as in the cortex or striatum (Borgan et al., 2021; Szabó et al., 2014), which has been associated with the presence of positive symptoms (Borgan et al., 2021) and schizophrenia itself (Fusar-Poli and Meyer-Lindenberg, 2013). In fact, partial agonism of CB1R has been shown to be capable of producing positive, negative psychotic symptoms and cognitive deficits in healthy volunteers (Borgan et al., 2021). This suggests that inhibition of Cav2.2 channels, which is the mechanism of action of ziconotide, could play a central role in the generation of psychotic symptoms. In support of this, the CACNA1B gene, which codes for Cav2.2 channels, has been shown to be associated with schizophrenia (Andrade et al., 2019). On the other hand, the CB1R-Cav2.2 binomial is also able to suppress glutamate release in the hippocampus and anterior cingulate cortex through a similar mechanism of action (depolarization-induced suppression of excitation phenomenon) (Borgan et al., 2021), which has been associated with the occurrence of delusions and hallucinations (Egerton and Stone, 2012) and the presence of depression (Moriguchi et al., 2019; Duman et al., 2019). In fact, the Cav2.2 receptor has been directly linked to the appearance of depressive symptomatology in mice (Caminski et al., 2022). Regarding suicidal ideation, it has been hypothesized to be due to the inhibition of neurotransmitter release in areas of the brain associated with mood and cognition (e.g., prefrontal and cerebral cortex) (Webster, 2015). Likewise, CACNA1B gene has also been linked to major depressive disorder and suicide (Andrade et al., 2019) and even to bipolar disorder.
Dysregulation of neurotransmitters such as dopamine, GABA and glutamate in the prefrontal cortex has also been proposed as a causal hypothesis for delirium (Webster, 2015; Maldonado, 2013), being compatible with the pathophysiological mechanism of Cav2.2. In addition, the role of glutamate in the neuropsychiatric symptomatology present in anti-NMDA encephalitis has been demonstrated (Kayser and Dalmau, 2016) and it is speculated that both GABA and glutamate may be involved in the psychotic and affective symptomatology of Kleine-Levin syndrome (Ortega-Albás et al., 2021; Hédou et al., 2022). Finally, similar psychomimetic effects have been observed with analgesic treatments such as ketamine, which is a NMDA receptor antagonist (Corlett et al., 2016; Cheng et al., 2018).
Regarding the limitations of the study, only clinical cases were included. At the same time, not all cases explained whether there was a psychiatric history, nor did they give an accurate description of the neuropsychiatric symptomatology. Moreover, in those that did, this information was not described by mental health professionals. These facts limit the ability to infer causality, to analyze in depth the elements involved in the occurrence of these adverse effects, and thus to generalize the results. Nevertheless, the control of confounding factors such as the use of opioids and the temporal coincidence between the introduction of ziconotide and the appearance of adverse effects invite further studies to elucidate the physiopathological mechanisms responsible, which could be of interest in the study of psychosis and schizophrenia.
5 ConclusionChronic pain is a subjective symptom which is difficult to measure and has an impact on people’s quality of life. At the same time, it has traditionally been underdiagnosed and undertreated. Opioids are drugs of first choice in these conditions, although they are not always effective or adequately tolerated. Moreover, the U.S. opioid crisis has highlighted the need for alternatives to opioids because of their high addictive risk. For this reason, other analgesics have been developed to solve this problem. Ziconotide is one of them, characterized by its peculiar origin and for being the first Cav2.2 channel antagonist used for severe chronic pain via intrathecal route. However, the mechanism of action could be related in processes other than analgesia, involving neurotransmitters such as dopamine, GABA and glutamate in brain areas related to the onset of neuropsychiatric symptoms.
Although these adverse effects are not common, their appearance in patients without a psychiatric history and the risk of decompensation in those with a mental disorder suggest that certain precautions should be taken when administering this drug. In this sense, clinicians should carefully evaluate individuals with pre-existing psychiatric disorders before prescribing ziconotide. Slow titration is advisable, and clinical response as well as the occurrence of adverse effects should be closely monitored (Smith and Deer, 2009). In the event of adverse symptoms, an early and individualized approach must be taken, considering discontinuation of ziconotide or combining antipsychotics (Webster, 2015).
Therefore, it is not only necessary to investigate the mechanism of action of Cav2.2 channels in the appearance of these symptoms, but also to expand the registry of cases presenting these undesired effects in order to better understand their heterogeneity and phenomenology.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributionsMP: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. RG-V: Conceptualization, Writing – original draft, Writing – review & editing. JP-M: Writing – original draft, Writing – review & editing. MB: Writing – original draft, Writing – review & editing. IE: Conceptualization, Supervision, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study received funding from Fundación de Investigación del Hospital Provincial de Castellón (CAFI 24–J02). The funders were not involved in the study design, data collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
AcknowledgmentsThe authors would like to thank Professor Gonzalo Haro for his valuable diagnostic approach to the clinical case, which made it possible to publish this manuscript.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ReferencesAbdelsayed, N., Whitlow, B., Harned, M., Craig, J., and Grider, J. (2022). A case of prolonged psychosis with intrathecal ziconotide. Neuromodulation Technol. Neural Interface 25:S16. doi: 10.1016/j.neurom.2022.02.146
Crossref Full Text | Google Scholar
Andrade, A., Brennecke, A., Mallat, S., Brown, J., Gomez-Rivadeneira, J., Czepiel, N., et al. (2019). Genetic associations between voltage-gated calcium channels and psychiatric disorders. Int. J. Mol. Sci. 20:3537. doi: 10.3390/ijms20143537
PubMed Abstract | Crossref Full Text | Google Scholar
Ayuga-Loro, F., Brocalero-Camacho, A., Quintas-López, M. V., and Cabrera-Feria, J. R. (2011). Efectos adversos neuropsiquiátricos del ziconotide intratecal. Rev. Neurol. 52, 61–63. doi: 10.33588/rn.5201.2010475
Crossref Full Text | Google Scholar
Borgan, F., Kokkinou, M., and Howes, O. (2021). The cannabinoid CB1 receptor in schizophrenia. Biol. Psychiatry Cogn. Neurosci Neuroimaging 6, 646–659. doi: 10.1016/j.bpsc.2020.06.018
Crossref Full Text | Google Scholar
Bramer, W. M., Rethlefsen, M. L., Kleijnen, J., and Franco, O. H. (2017). Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst. Rev. 6:245. doi: 10.1186/s13643-017-0644-y
PubMed Abstract | Crossref Full Text | Google Scholar
Brookes, M. E., Eldabe, S., and Batterham, A. (2017). Ziconotide monotherapy: a systematic review of randomised controlled trials. Curr. Neuropharmacol. 15, 217–231. doi: 10.2174/1570159x14666160210142056
PubMed Abstract | Crossref Full Text | Google Scholar
Caminski, E. S., Antunes, F. T. T., Souza, I. A., Dallegrave, E., and Zamponi, G. W. (2022). Regulation of N-type calcium channels by nociceptin receptors and its possible role in neurological disorders. Mol. Brain 15:95. doi: 10.1186/s13041-022-00982-z
Crossref Full Text | Google Scholar
Cheng, W. J., Chen, C. H., Chen, C. K., Huang, M. C., Pietrzak, R. H., Krystal, J. H., et al. (2018). Similar psychotic and cognitive profile between ketamine dependence with persistent psychosis and schizophrenia. Schizophr. Res. 199, 313–318. doi: 10.1016/j.schres.2018.02.049
PubMed Abstract | Crossref Full Text | Google Scholar
Corlett, P. R., Honey, G. D., and Fletcher, P. C. (2016). Prediction error, ketamine and psychosis: an updated model. J. Psychopharmacol. 30, 1145–1155. doi: 10.1177/0269881116650087
PubMed Abstract | Crossref Full Text | Google Scholar
de la Calle Gil, A. B., Peña Vergara, I., Cormane Bornacelly, M. A., and Pajuelo Gallego, A. (2015). Intrathecal ziconotide and morphine for pain relief: a case series of eight patients with refractory cancer pain, including five cases of neuropathic pain. Neurol. Therapy 4, 159–168. doi: 10.1007/s40120-015-0035-z
PubMed Abstract | Crossref Full Text | Google Scholar
Duman, R. S., Sanacora, G., and Krystal, J. H. (2019). Altered connectivity in depression: GABA and glutamate neurotransmitter deficits and reversal by novel treatments. Neuron 102, 75–90. doi: 10.1016/j.neuron.2019.03.013
PubMed Abstract | Crossref Full Text | Google Scholar
Egerton, A., and Stone, J. M. (2012). The glutamate hypothesis of schizophrenia: neuroimaging and drug development. Curr. Pharm. Biotechnol. 13, 1500–1512. doi: 10.2174/138920112800784961
Crossref Full Text | Google Scholar
Fusar-Poli, P., and Meyer-Lindenberg, A. (2013). Striatal presynaptic dopamine in schizophrenia, part II: meta-analysis of [(18)F/(11)C]-DOPA PET studies. Schizophr. Bull. 39, 33–42. doi: 10.1093/schbul/sbr180
PubMed Abstract | Crossref Full Text | Google Scholar
Grajny, K., Durphy, J., Adam, O., Azher, S., Gupta, M., and Molho, E. (2020). Ziconotide-induced Oro-lingual dyskinesia: 3 cases. Tremor Other Hyperkinetic Mov. 10:37. doi: 10.5334/tohm.431
PubMed Abstract | Crossref Full Text | Google Scholar
Hédou, J., Cederberg, K. L., Ambati, A., Lin, L., Farber, N., Dauvilliers, Y., et al. (2022). Proteomic biomarkers of Kleine-Levin syndrome. Sleep 45:097. doi: 10.1093/sleep/zsac097
PubMed Abstract | Crossref Full Text | Google Scholar
Kapural, L., Lokey, K., Leong, M. S., Fiekowsky, S., Stanton-Hicks, M., Sapienza-Crawford, A. J., et al. (2009). Intrathecal ziconotide for complex regional pain syndrome: seven case reports. Pain Practice 9, 296–303. doi: 10.1111/j.1533-2500.2009.00289.x
PubMed Abstract | Crossref Full Text | Google Scholar
Levin, T., Petrides, G., Weiner, J., Saravay, S., Multz, A. S., and Bailine, S. (2002). Intractable delirium associated with ziconotide successfully treated with electroconvulsive therapy. Psychosomatics 43, 63–66. doi: 10.1176/appi.psy.43.1.63
Crossref Full Text | Google Scholar
Lozovaya, N., Min, R., Tsintsadze, V., and Burnashev, N. (2009). Dual modulation of CNS voltage-gated calcium channels by cannabinoids: focus on CB1 receptor-independent effects. Cell Calcium 46, 154–162. doi: 10.1016/j.ceca.2009.07.007
PubMed Abstract | Crossref Full Text | Google Scholar
Maldonado, J. R. (2013). Neuropathogenesis of delirium: review of current etiologic theories and common pathways. Am. J. Geriatr. Psychiatry 21, 1190–1222. doi: 10.1016/j.jagp.2013.09.005
PubMed Abstract | Crossref Full Text | Google Scholar
Moriguchi, S., Takamiya, A., Noda, Y., Horita, N., Wada, M., Tsugawa, S., et al. (2019). Glutamatergic neurometabolite levels in major depressive disorder: a systematic review and meta-analysis of proton magnetic resonance spectroscopy studies. Mol. Psychiatry 24, 952–964. doi: 10.1038/s41380-018-0252-9
PubMed Abstract | Crossref Full Text | Google Scholar
Ortega-Albás, J. J., López, R., Martínez, A., Carratalá, S., Echeverria, I., and Ortega, P. (2021). Kleine-Levin syndrome, GABA, and glutamate. J. Clin. Sleep Med. 17, 609–610. doi: 10.5664/jcsm.9058
PubMed Abstract | Crossref Full Text | Google Scholar
Phan, S. V., and Waldfogel, J. M. (2015). Ziconotide-induced psychosis: a case report. Gen. Hosp. Psychiatry 37, 97.e11–97.e12. doi: 10.1016/j.genhosppsych.2014.10.001
Crossref Full Text | Google Scholar
Poli, P., and Ciaramella, A. (2011). Psychiatric predisposition to autonomic and abnormal perception side-effects of ziconotide: a case series study. Neuromodulation 14, 219–224. doi: 10.1111/j.1525-1403.2011.00334.x
Crossref Full Text | Google Scholar
Smith, H. S., and Deer, T. R. (2009). Safety and efficacy of intrathecal ziconotide in the management of severe chronic pain. Ther. Clin. Risk Manag. 5, 521–534. doi: 10.2147/tcrm.s4438
Crossref Full Text | Google Scholar
Stewart, B., and Sarria, J. (2014). Analgesia and psychosis: intrathecal ziconotide in a young hospice patient with spinocerebellar ataxia and painful peripheral neuropathy. J. Pain 15:S72. doi: 10.1016/j.jpain.2014.01.297
Crossref Full Text | Google Scholar
Su, A., Johnson, H., Taylor, C., and Oros, S. (2021). Ziconotide-induced psychosis in patient without previous psychiatric history: a case report. Pers. Med. Psychiatry 29-30:100086. doi: 10.1016/j.pmip.2021.100086
Crossref Full Text | Google Scholar
Szabó, G. G., Lenkey, N., Holderith, N., Andrási, T., Nusser, Z., and Hájos, N. (2014). Presynaptic calcium channel inhibition underlies CB₁ cannabinoid receptor-mediated suppression of GABA release. J. Neurosci. 34, 7958–7963. doi: 10.1523/JNEUROSCI.0247-14.2014
PubMed Abstract | Crossref Full Text | Google Scholar
Webster, L. R. (2015). The relationship between the mechanisms of action and safety profiles of intrathecal morphine and ziconotide: a review of the literature. Pain Med. 16, 1265–1277. doi: 10.1111/pme.12666
PubMed Abstract | Crossref Full Text | Google Scholar
Whitlow, J., Mu, K., Coverdale, J. H., and Shah, A. A. (2015). Ziconotide-associated psychosis treated with invega. Psychiatr. Ann. 45, 64–66. doi: 10.3928/00485713-20150212-02
Crossref Full Text | Google Scholar
Zamponi, G. W., Striessnig, J., Koschak, A., and Dolphin, A. C. (2015). The physiology, pathology, and pharmacology of voltage-gated calcium channels and their future therapeutic potential. Pharmacol. Rev. 67, 821–870. doi: 10.1124/pr.114.009654
留言 (0)