Facet joint septic arthritis is a rare but severe infection that can give rise to serious clinical outcomes. Most common signs and symptoms are fever and back or neck pain.[1] Diagnosis of such conditions is difficult due to non-specific clinical presentation, leading to significant delay in management. The average age of patients is 55–59 and it most commonly affects immunocompromised patients.[2,3] Over 80% of cases occur at the lumbar spine.[2] Etiology of facet joint septic arthritis includes hematogenous spread, local spread from spondylodiscitis, epidural or paraspinal abscess, and iatrogenic causes including epidural catheterization or steroid injection.[4] Normal inflammatory markers cannot be exclude the possibility of this disease.[5] Magnetic resonance imaging (MRI) is the standard investigation.[6] Accurate and early diagnosis of the disease is key to improve clinical outcome. Most patients recover uneventfully or suffer mild neurological symptoms. Treatment options include antibiotics, drainage, or open debridement.[2]
Four cases of Chinese patients from 60 to 80 years old from our institution were demonstrated in this case series. There is little literature on this disease entity and most radiologists and clinicians may neglect this disease entity or put it at a low position in the list of differentials when approaching long-standing back pain despite treatment. This case series serves as a reminder of this disease to radiologists and clinicians and summarizes the imaging findings.
CASE SERIES Case 1A 61-year-old male hostel resident was admitted for a few days’ history of low back pain, fever, confusion, shortness of breath, and chills and rigors. He presented with bilateral lower limb weakness for a week. On physical examination, he was found to have bilateral lower limb weakness with medical research council (MRC) scores three out of five and hyporeflexia but normal bilateral upper limb powers. The bilateral lower limb sensation was preserved. No other neurological deficit was found. Lumbar puncture yielded methicillin-susceptible Staphylococcus aureus in culture results, high white cell counts, and percentage of polymorphs in cerebrospinal fluid. Acid-fast bacilli were not found. Blood culture also grew methicillin-susceptible S. aureus. Rocephin and vancomycin were given for 5 days after admission but the lower limb weaknesses did not improve.
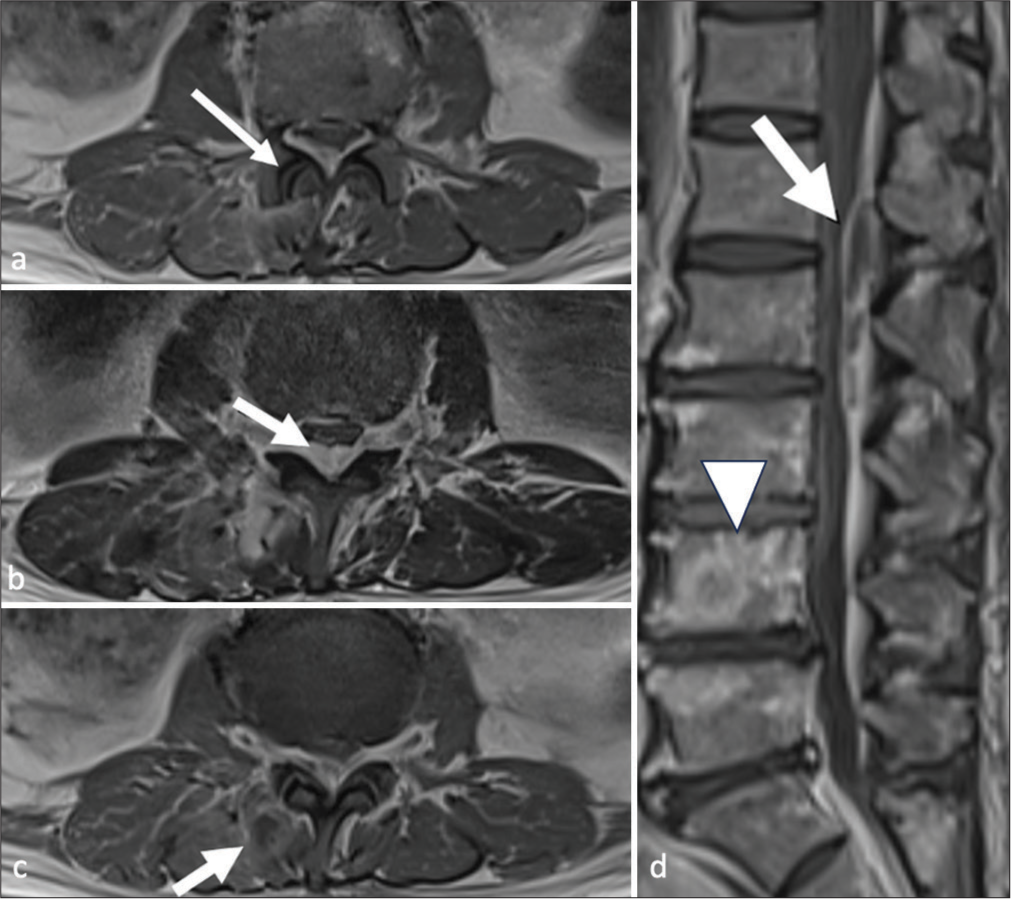
A gadolinium-enhanced MRI of the lumbosacral spine was done 5 days after admission. There was widening of the right L1/2 level facet joint [Figure 1a]. No associated bone erosion was observed. With the given clinical context, these features are suggestive of active facet joint septic arthritis. A large epidural abscess extended from T12 to L4 levels, causing compression on the thecal sac, most severe at L2 level [Figure 1b]. Small paraspinal abscesses over right paraspinal muscle [Figure 1c] were also noted. Sagittal view of contrast MRI images showed the epidural abscess from T12 to L4 level [Figure 1d].
Export to PPT
Surgical drainage of epidural abscess and right L1 laminotomy were done on the same day of the scan and the bilateral lower limb powers were improved. Follow-up MRI scan after 1 month of the previous scan showed ongoing right L1/2 septic arthritis and resolved epidural abscess. The patient later developed pneumonia and eventually succumbed to it 2 months after admission.
Case 2This patient is a 50-year-old male presenting with 1 week onset of fever, low back pain, bilateral lower limb weakness and numbness. Physical examinations showed no neurological deficit. Lumbosacral radiograph revealed degenerative changes but no fracture or endplate erosion. White cell counts were elevated.
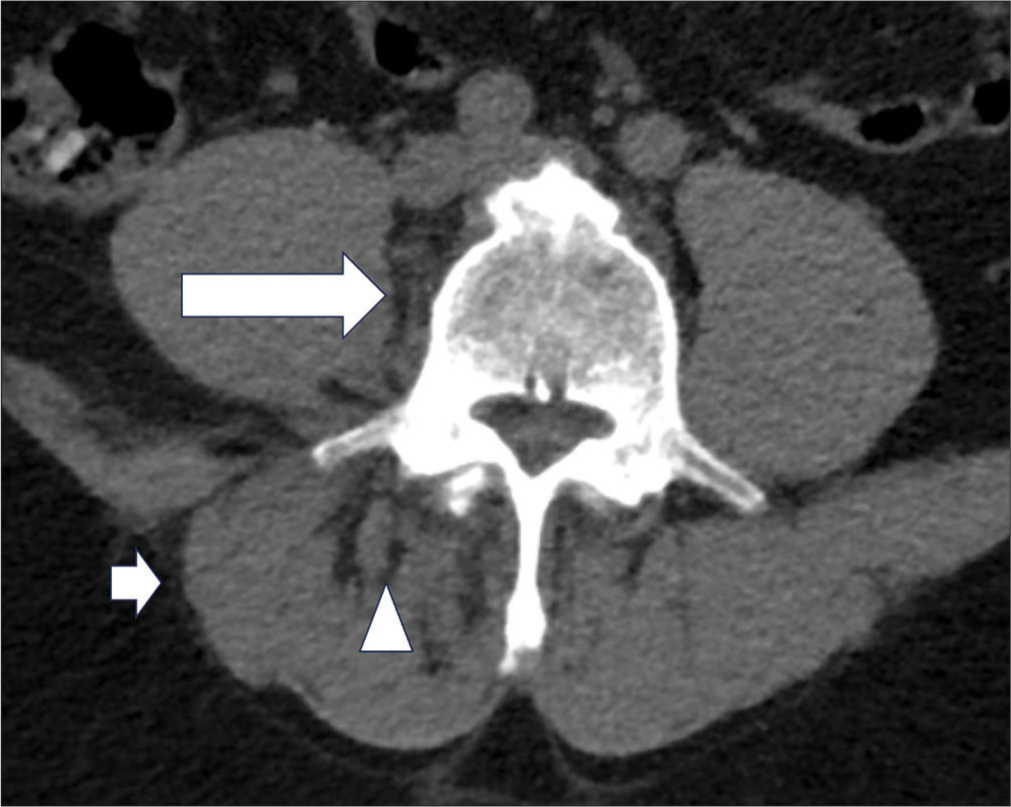
Contrast computed tomography (CT) lumbosacral spine done on the day after admission showed subtle increased fat strandings at the right retroperitoneal region adjacent to the L5 and S1 vertebrae [Figure 2]. Inflammatory changes were over the right erector spinae muscle [Figure 2]. Right erector spinae muscle was mildly swollen [Figure 2]. No bone erosion or rim-enhancing collection was detected.
Export to PPT
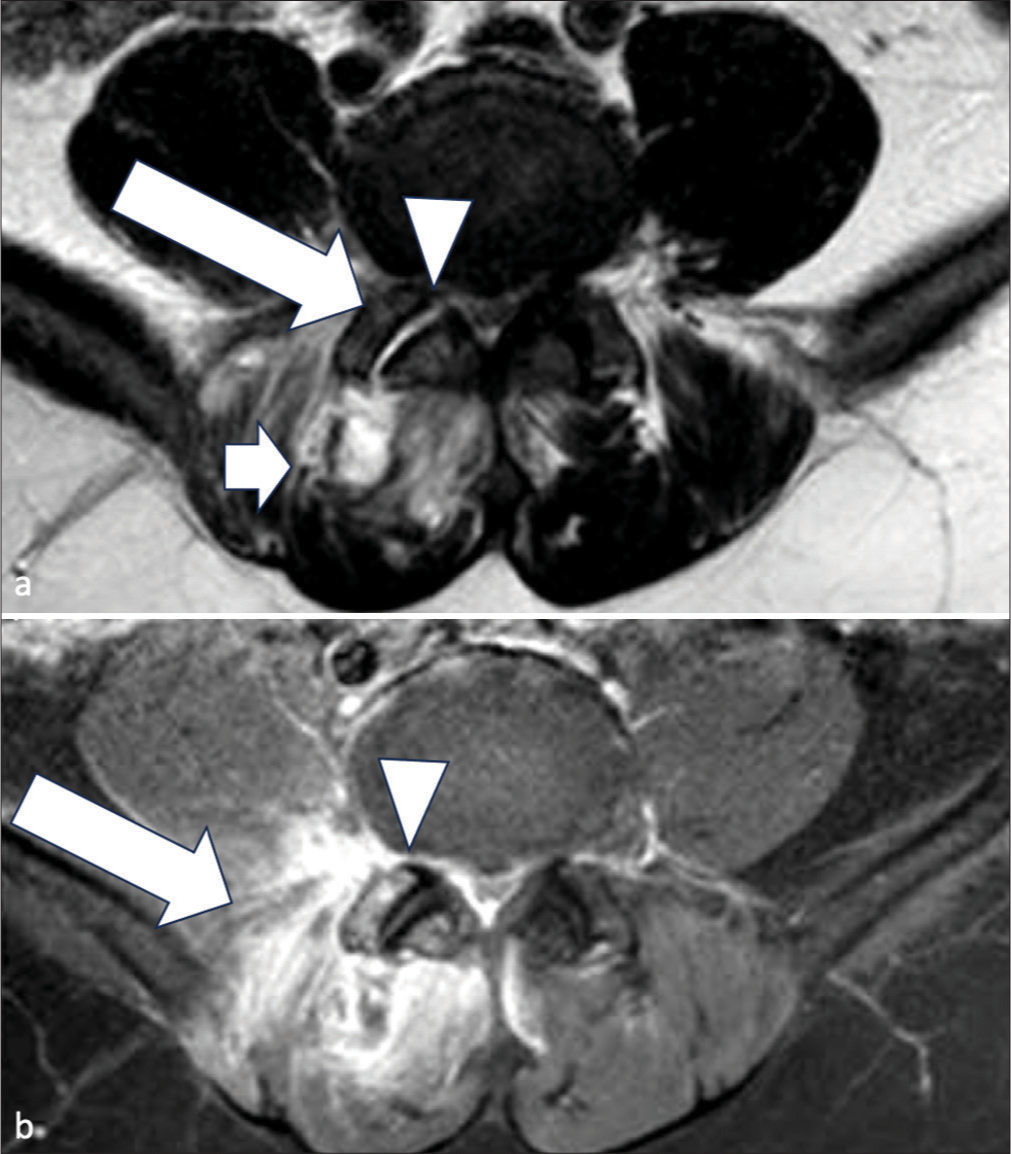
MRI of the lumbosacral spine was done a few days after CT and demonstrated joint space widening and effusion of the right L5/S1 facet joint [Figure 3a]. Abnormal marrow edema was noted at the adjacent articular processes [Figure 3a]. Right paraspinal muscle edema [Figure 3a] was also seen. Enhancement was seen around right L5/S1 facet joint [Figure 3b] and paraspinal region [Figure 3b].
Export to PPT
After completion of a course of antibiotics, the white cell counts were normalized and fever resolved. He had no more low back pain or lower limb weakness afterward.
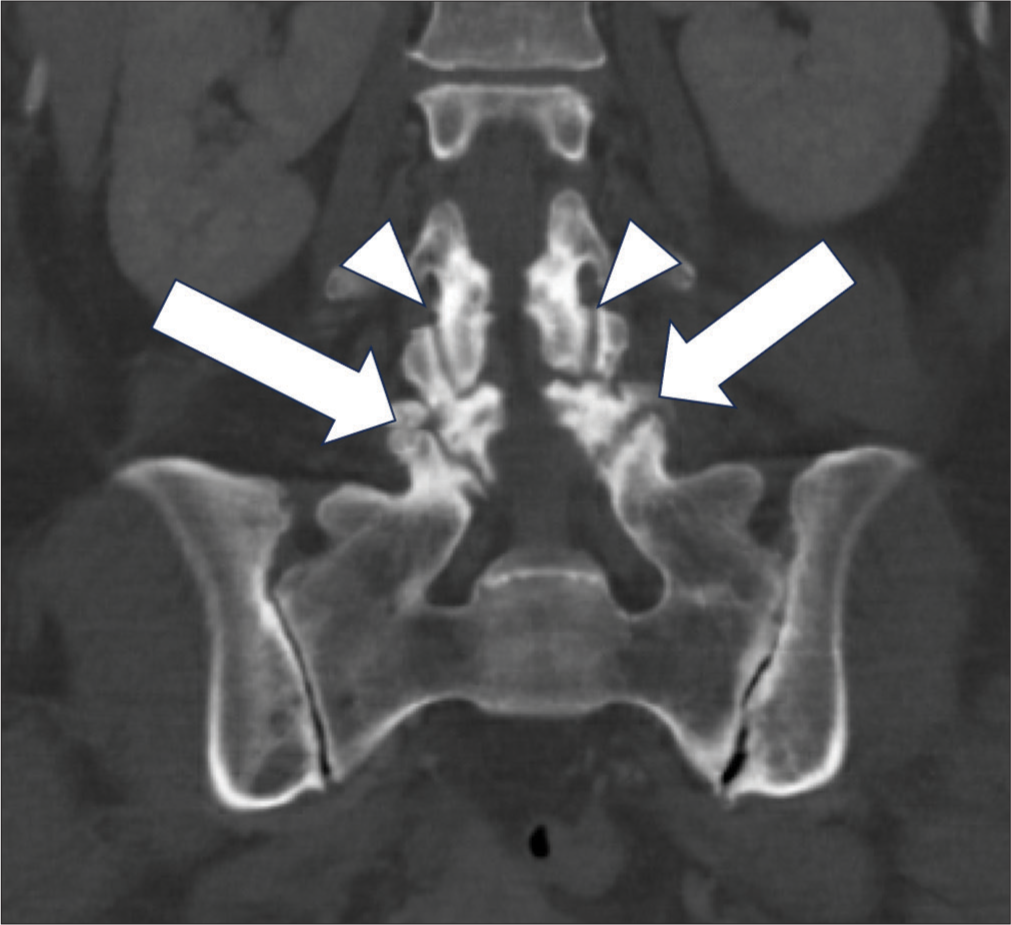
Case 3A 60-year-old lady with newly diagnosed diabetes mellitus presents with fever of unknown origin, low back pain for 1 week, and mild bilateral lower limb weakness. Physical examinations showed MRC scores of three out of three for bilateral lower limbs. There was no other neurological deficit. Blood counts showed raised white cell counts and blood culture grew Streptococcus agalactiae. An initial CT abdomen and pelvis on the same day of admission was done to rule out intra-abdominal sepsis. It showed no intra-abdominal septic source but diffuse sclerosis and subchondral irregularity of bilateral L4 and L5 articular processes around the facet joints [Figure 4], which was misinterpreted as degenerative changes at the time of reporting. Comparatively, smooth subchondral bone at bilateral L3–L4 facet joints was also noted [Figure 4]. Six weeks later, the patient had persistent low back pain and fever of unknown origin. She went to a private imaging center for a positron emission tomography–computed tomography (PET-CT) scan follow whole body to look for occult infection or malignancy. PET-CT whole body showed hypermetabolic erosion of bilateral L4/5 articular processes with narrowing of joint space [Figure 5a and b] and increased FDG uptake at right L5 lamina [Figure 5c and d]. There was increased FDG uptake of adjacent spinal canal at L5 level with corresponding hypodense epidural collection [Figure 5c and d]. Features were deemed suspicious of bilateral L4/5 facet joint septic arthritis and epidural abscess. However, there was mild FDG uptake at bilateral L3/4 facet joints [Figure 6] suggestive of degenerative changes.
Export to PPT
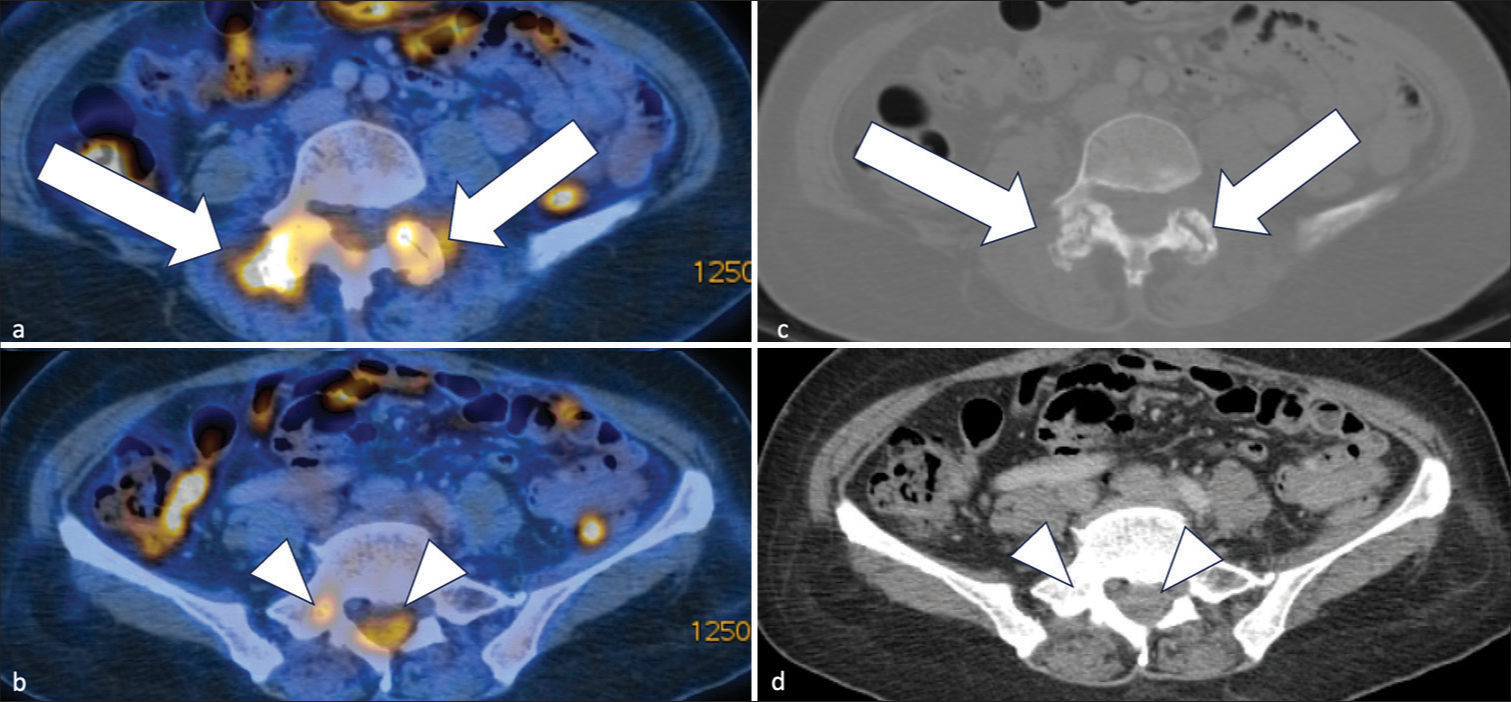
Export to PPT
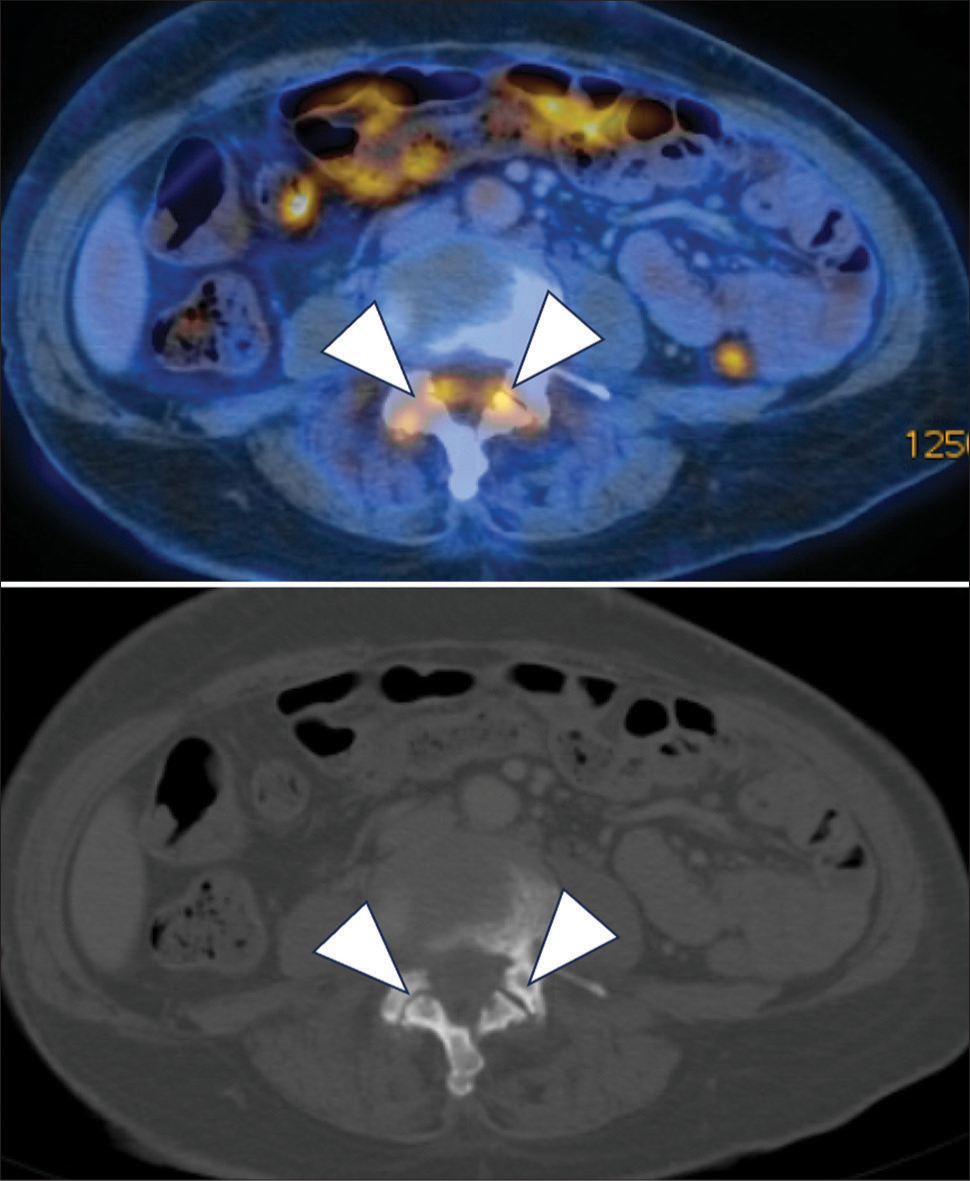
Export to PPT
MRI lumbosacral spine in T2-weighted sequences done at 2 weeks after admission showed erosion of bilateral L4/5 facet joint surfaces [Figure 7]. Adjacent paraspinal muscle edema was observed at the bilateral L4/5 facet joints [Figure 7], with the right side being more severely affected. These confirm septic arthritis of bilateral L4/5 facet joints. It was complicated by epidural abscess with epicenter at L5 level [Figure 8]. White cell counts and symptoms resolved after a course of antibiotics. Follow-up contrast CT lumbosacral spine after treatment showed the epidural abscess had resolved [Figure 9].
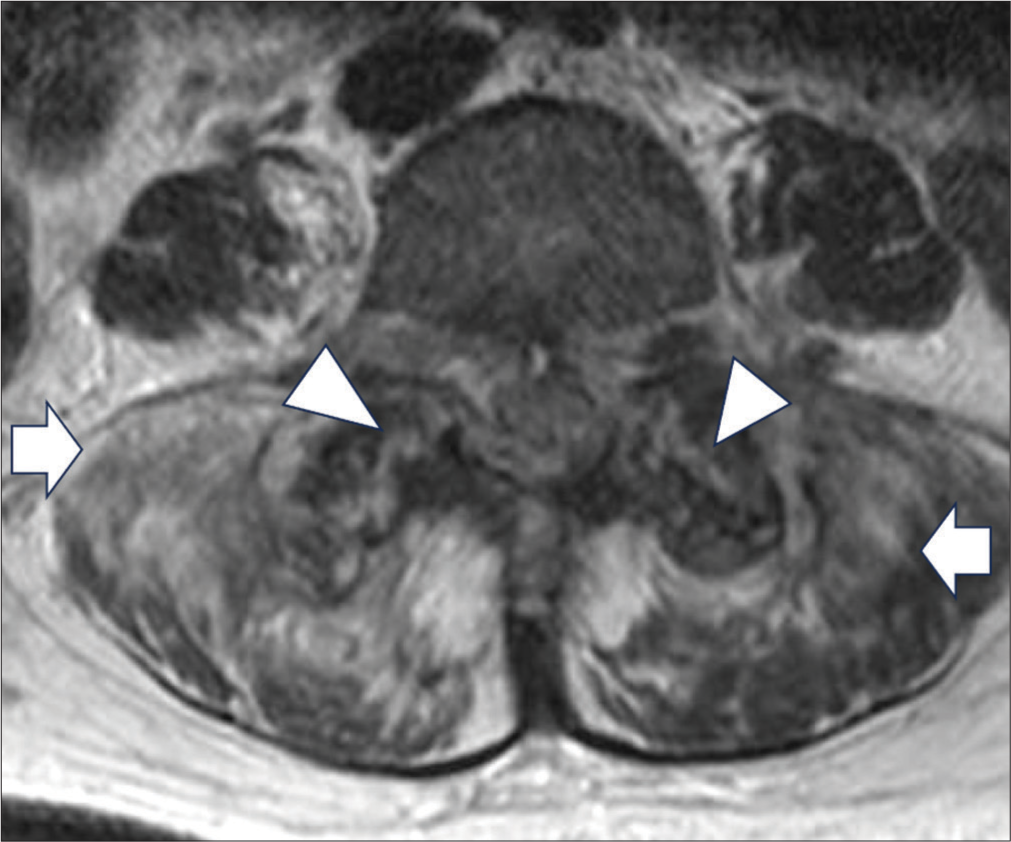
Export to PPT

Export to PPT

Export to PPT
Case 4A 79-year-old lady with a history of cervical myelopathy presented with worsening neck pain for a few weeks. Physical examinations showed myelopathic hand signs and mildly reduced bilateral upper limb power with MRC scores four out of five. Plain CT cervical spine was done due to increasing neck pain recently. It showed right C3/C4 facet joint destruction and widening [Figure 10]. Septic arthritis was suspected given the single joint involvement and features.

Export to PPT
MRI cervical spine showed that the right C3/4 facet joint surface irregularities with increased T2 hyperintense signals over articular processes [Figure 11a and b]. Features suggest right C3/4 facet joint septic arthritis. Epidural abscess was also noted at the right C5 level [Figure 11c].
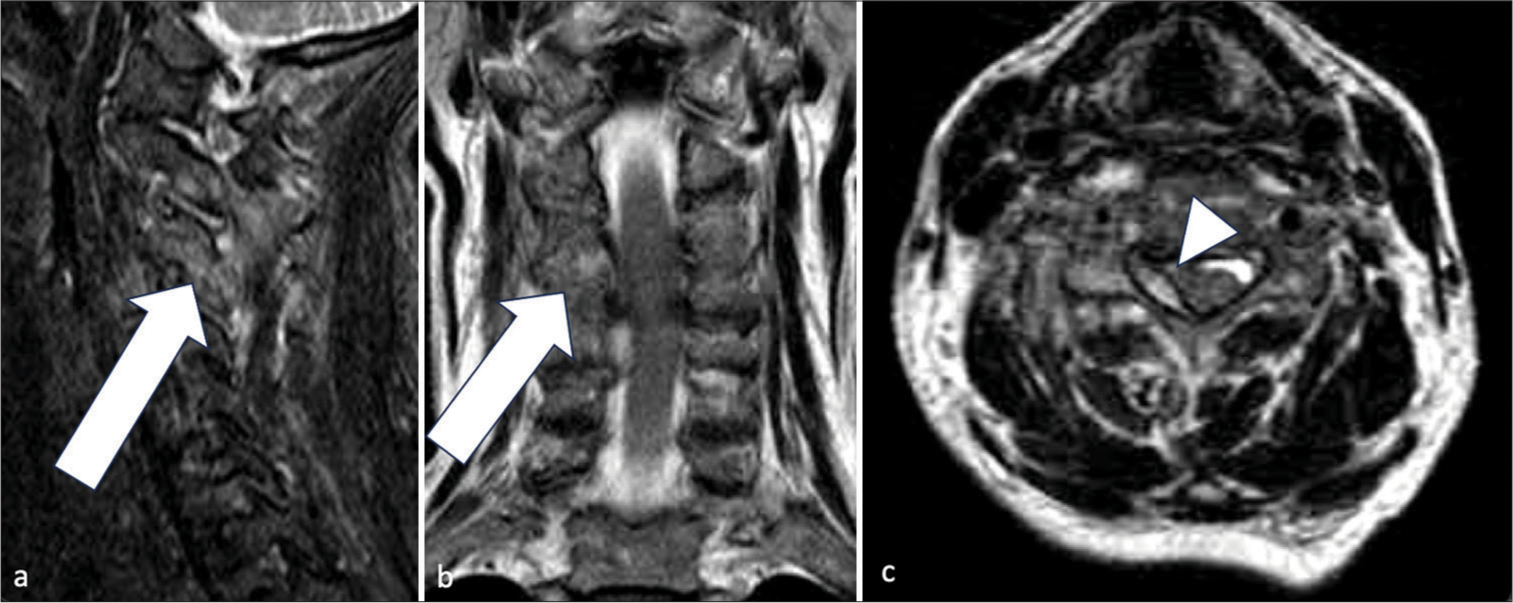
Export to PPT
The patient underwent C3–5 laminectomy for spinal decompression, drainage of epidural abscess, and C3/4 fusion. Follow-up blood tests showed normalized white cell counts and fever and neck pain subsided.
DISCUSSIONFacet joint septic arthritis is easy to be overlooked when clinicians and radiologists approach a case of low back pain, especially those with a long-standing history of spondylosis. There is not much literature on this disease, many of them being case reports or series. The cases demonstrated above include cases in which the diagnosis of facet joint septic arthritis can be missed easily if attending doctors do not have this differential in mind.[7] It presents with non-specific clinical symptoms and has variable clinical picture. It resembles spondylodiscitis clinical and biochemically.[8] MRI is both sensitive and specific to diagnose this disease especially within 2 days of infection.[9] Radiological changes may lag behind the clinical improvement. Therefore, follow-up MRI images should always be correlated clinically with the patient’s condition.
To summarize the imaging findings, CT findings of facet joint septic arthritis include widening of facet joint, erosion of joint surface, and adjacent fat strandings. Paraspinal abscess may be present in advanced cases. In MRI, it will show bone marrow edema of adjacent articular processes, widening of joint, erosion of joint surface, and paraspinal muscle edema with or without abscess. Epidural abscess is sometimes present.
CT spine may occasionally be the first cross sectional image in cases of facet joint septic arthritis. As shown in above cases, early stages of the disease may only show subtle fat strandings in the paravertebral region. Apart from examining the vertebral bodies and intervertebral disc, facet joints should always be screened for any bony erosion or widened joint space. MRI spine can be considered if there is any suspicion of this disease. Early detection of facet joint septic arthritis guides management and saves the patient from unnecessary investigations and treatment.
Facet joint arthrosis can be mimicker of septic arthritis. Contralateral side and one to two levels superior or inferior of facet joints can be compared for any significant asymmetry or difference. Septic arthritis has to be excluded if there are clinical and biochemical signs of infection. Accurate and early diagnosis of the disease and differentiation from arthrosis are important to improve clinical outcome.
In short, there are a few learning points from the above cases:
Septic arthritis of the facet joint should be considered after ruling out common causes of back pain and in patients with signs of infection.
MRI is the best imaging modality for diagnosis of septic arthritis of facet joints. Follow-up MRI scan is helpful if the initial MRI scan shows equivocal findings.
CT spine may demonstrate early signs of septic arthritis including fat strandings in the paravertebral region. Other signs including bony erosion or widened joint space are supportive of the diagnosis. Degenerative changes, on the other hand, will show osteophytes and narrowed joint spaces.
Given the difficulty in diagnosis, future research can focus on improving diagnostic techniques, such as 3T MRI images instead of routine 1.5T MRI images for better resolution of facet joint spaces.
CONCLUSIONFacet joint septic arthritis is a rare but significant clinical condition that poses diagnostic challenges due to its non-specific presentation. Early and accurate diagnosis, primarily through MRI, is essential for effective treatment and prevention of complications. This case series highlights the need for heightened clinical awareness and consideration of this diagnosis in patients presenting with back pain and signs of infection. Future research should focus on improving diagnostic techniques.
留言 (0)