Atlanto-occipital assimilation is a congenital craniovertebral junction malformation where the partial or complete fusion of atlas and occiput occurs. The incidence of atlanto-occipital assimilation was estimated to be 0.14–0.75% among the general population, affecting males and females equally.[1,2] Although most patients with atlanto-occipital assimilation are asymptomatic, some could be complicated by cervical cord compression. As a result, vigilant identification and accurate reporting of atlanto-occipital assimilation are essential. Flexion and extension radiography, computed tomography (CT), and magnetic resonance imaging all play important roles in diagnosing and evaluating complications of atlanto-occipital assimilation.
This pictorial review illustrates interesting cases of atlanto-occipital assimilation from Princess Margaret Hospital in Hong Kong, collected over the past 8 years. Numerous complications and associations of atlanto-occipital assimilation (e.g., basilar invagination, atlantoaxial subluxation, Chiari malformation, congenital vertebral bodies fusion, and compressive myelopathy) would be discussed, supported by real cases.
CLASSIFICATIONAtlanto-occipital assimilation is classified into three types:
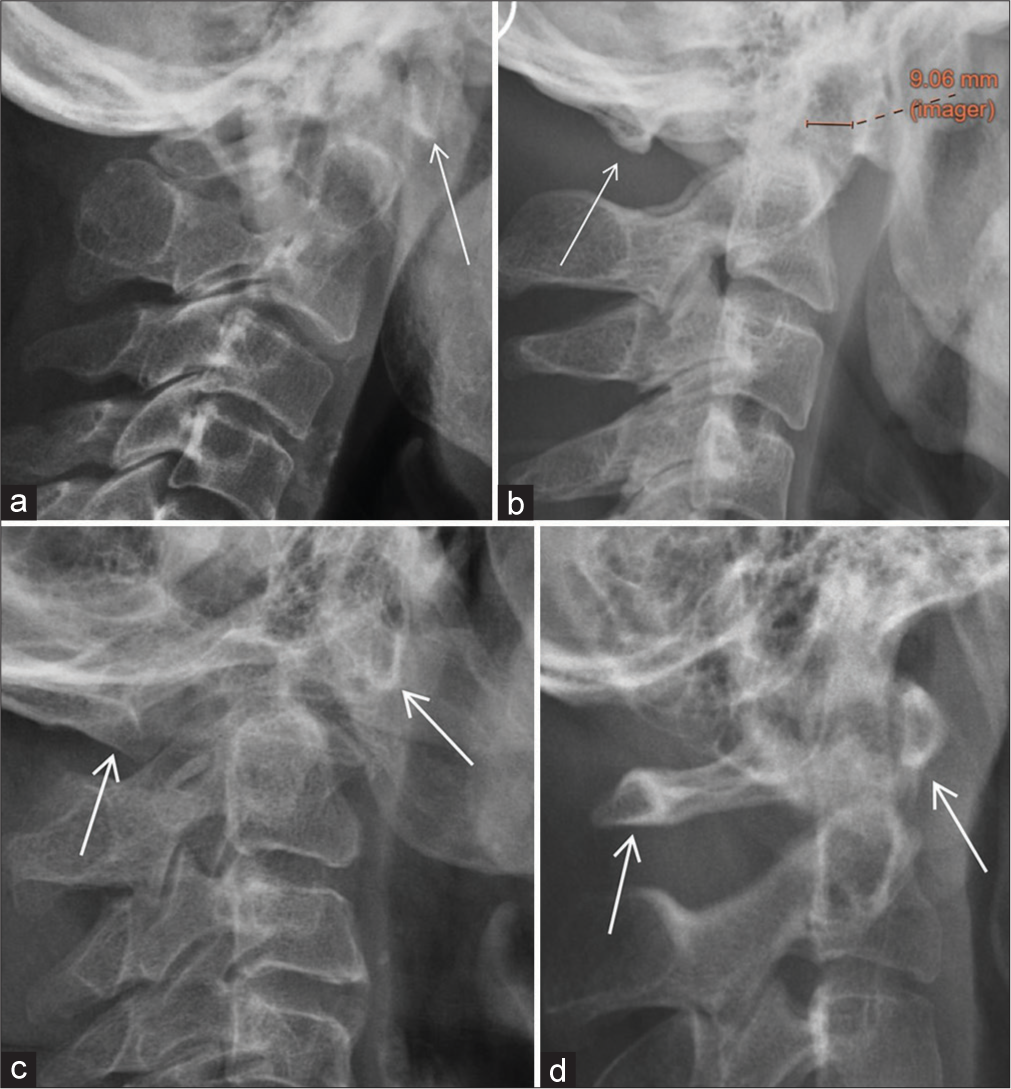
Anterior arch assimilation [Figure 1a]
Posterior arch assimilation [Figure 1b]
Assimilation of both anterior and posterior arches [Figure 1c].
Export to PPT
A normal radiograph of the craniovertebral junction is included as a reference [Figure 1d].
This classification is based on the differences in embryological origins of the anterior arch and posterior arch of the atlas. The clinical implication for classifying atlanto-occipital assimilation into three main groups is that different types of atlanto-occipital assimilation are associated with different types of basilar invagination. This will be further elaborated later.
EMBRYOLOGY AND GENETICSThe craniovertebral junction is an embryologically unstable region and is subjected to numerous variations, with atlanto-occipital assimilation being one of the most common anomalies.[3] The embryological instability of the craniovertebral junction is considered analogous to the lumbosacral region, where lumbarization of S1 and sacralization of L5 are commonly seen.
According to Pang and Thompson, the hypochordal bow of proatlas forms the anterior atlantal arch and the lateral dense zone of the C1 sclerotome forms the posterior atlantal arch. Due to their differences in embryological origin, different types of atlanto-occipital assimilation could therefore be observed radiologically.[3]
It is postulated that mutations of the Hox gene homologues could be responsible for causing atlanto-occipital assimilation, as demonstrated in mouse models. Inappropriate repression of Pax-1 may be responsible for combined atlanto-occipital assimilation and Klippel-Feil syndrome.[3]
ASSOCIATIONS AND COMPLICATIONSAtlanto-occipital assimilation is associated with numerous pathologies which should be actively searched for once it is identified. Associated complications should be mentioned in the radiology report since they are essential in guiding subsequent patient management.
Basilar invaginationAtlanto-occipital assimilation could be associated with both Type I and Type II basilar invagination.
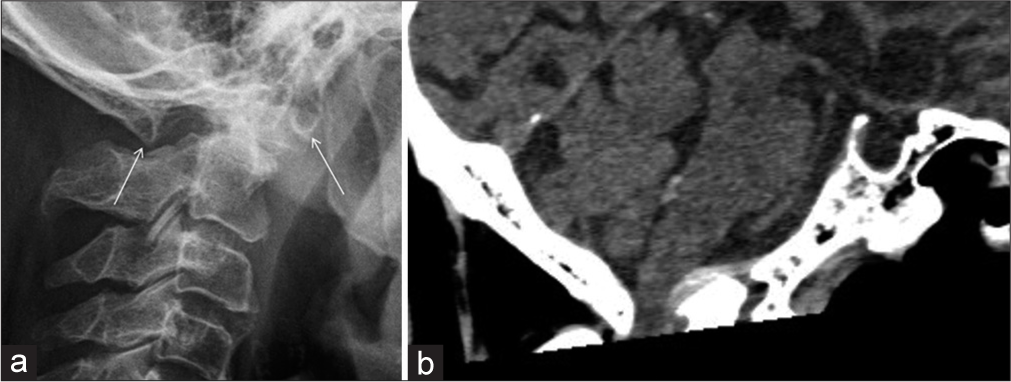
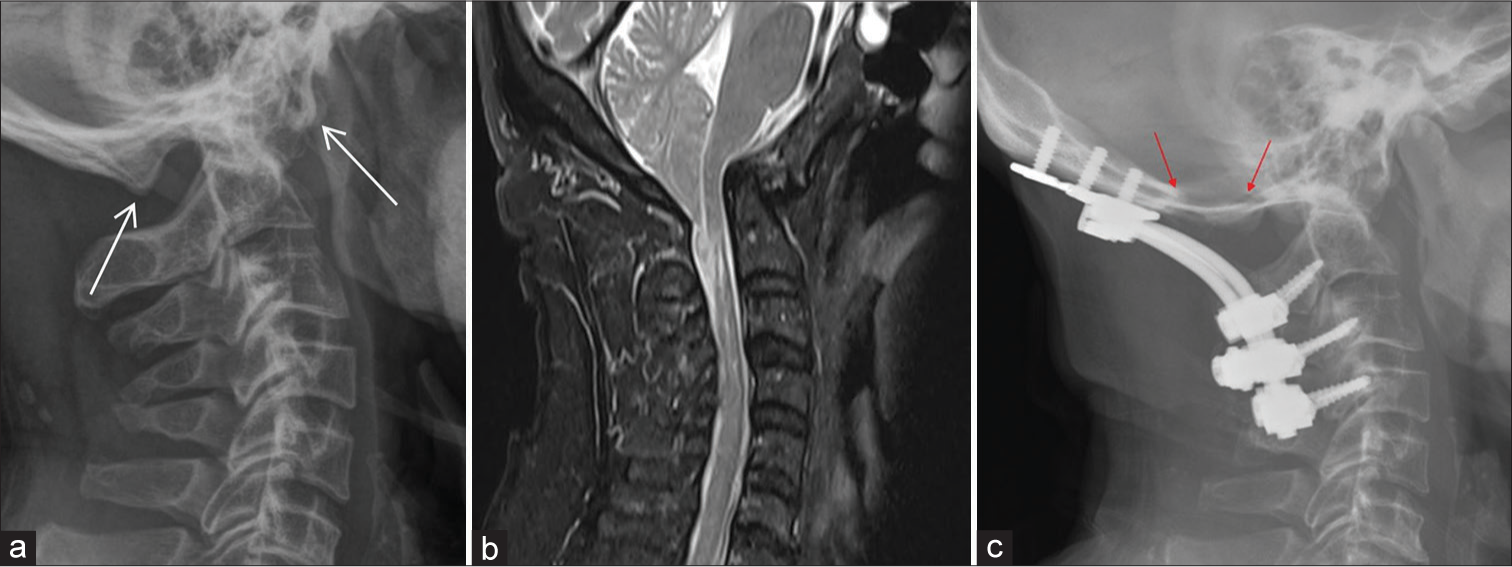
Type I basilar invagination refers to the odontoid process directly invaginating inside the foramen magnum and is associated with craniocervical instability [Figure 2]. Type II basilar invagination is not associated with craniocervical instability and is characterized by a flattened basicranium.
Export to PPT
It is postulated that type I basilar invagination is more associated with anterior arch assimilation since the anterior arch of the atlas and the atlantoaxial ligament system share a common embryological origin. Type II basilar invagination, on the other hand, is more associated with posterior arch assimilation.[4]
Type I basilar invagination is more prone to direct brainstem compression due to odontoid process indentation. Type II basilar invagination can lead to a reduction in posterior cranial fossa volume and subsequent Chiari malformation.[5]
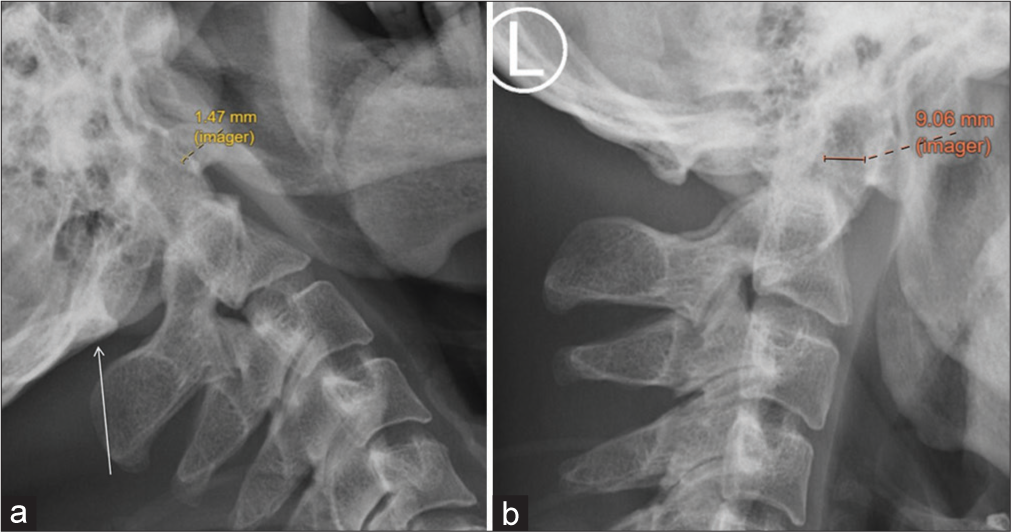
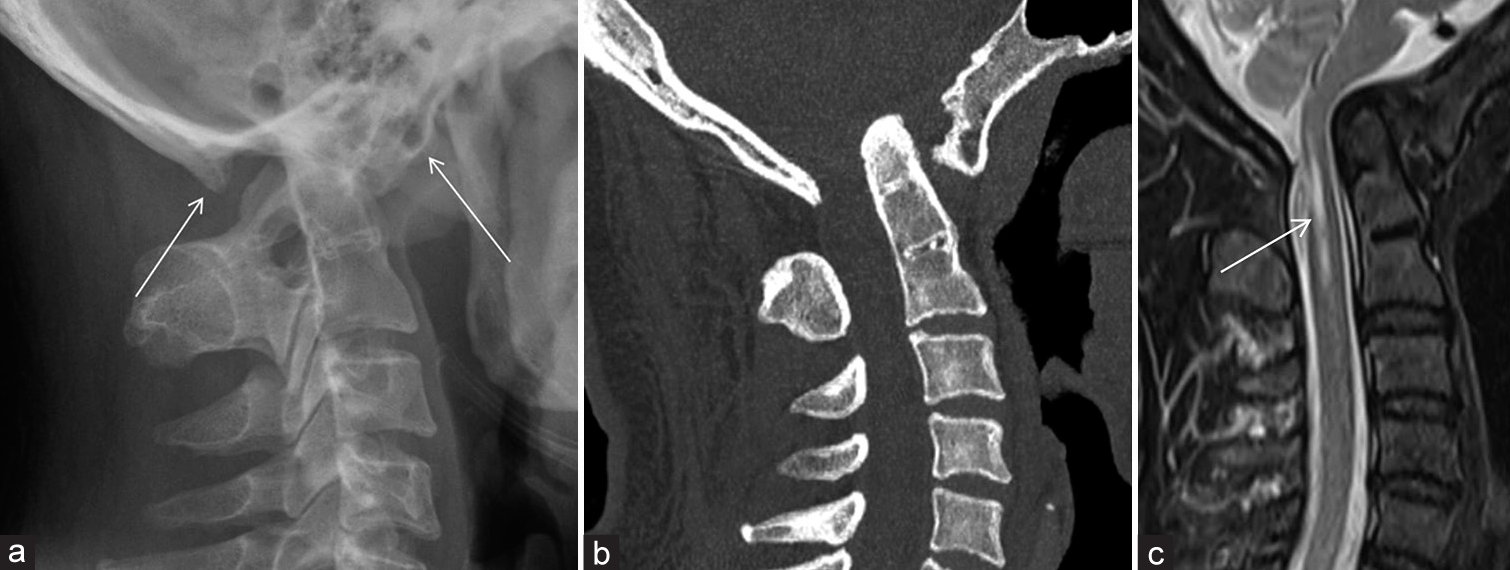
Anteroposterior atlantoaxial subluxationThe distance between the anterior arch of C1 and the dens in a fully flexed position should be <3 mm in adults and <5 mm in children.[6] The atlantoaxial subluxation can be occult in a standard lateral view of the cervical spine. Flexion and extension radiographs are helpful in detecting occult anteroposterior atlantoaxial subluxation [Figure 3].
Export to PPT
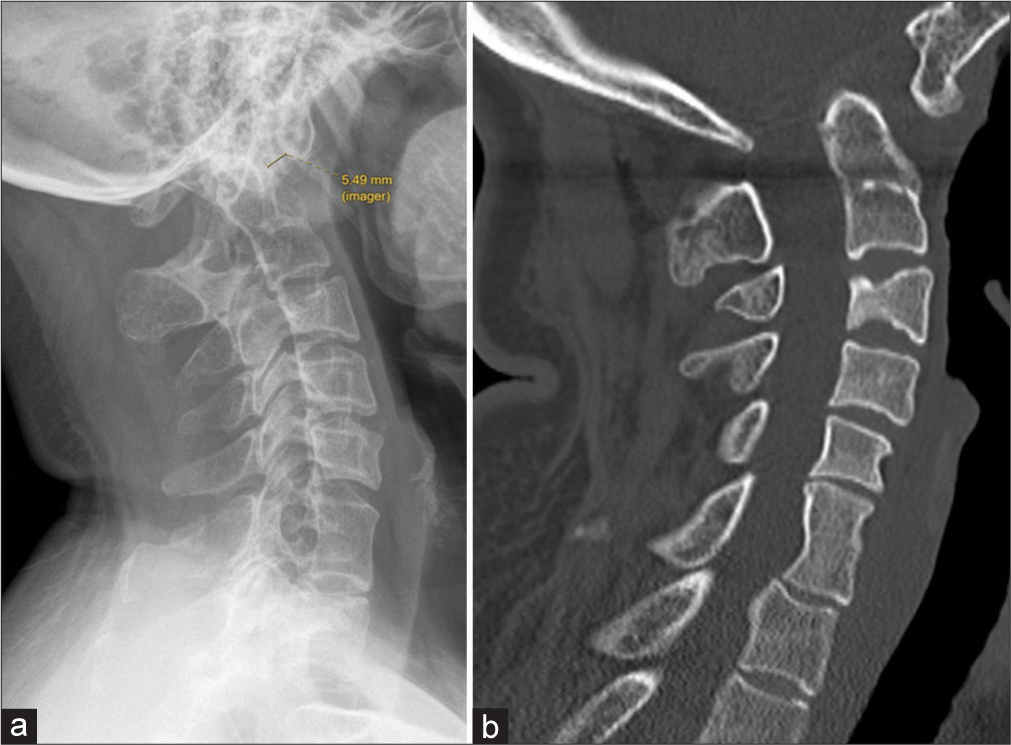
Fusion of adjacent vertebral bodiesAtlanto-occipital assimilation could be associated with numerous types of fusion of vertebral bodies. By far, a fusion of C2/3 vertebral bodies would be the most common. Examples are illustrated in the following cases [Figures 4-6]. In patients with a congenital fusion of vertebral bodies or Klippel-Feil syndrome, the wasp-waist sign could be observed, meaning that the anteroposterior diameter of the affected discovertebral joint is smaller than the diameter of the superior and inferior limits of the vertebral bodies adjacent to uninvolved discs[7] [Figure 6].

Export to PPT

Export to PPT
Export to PPT
Chiari malformationAtlanto-occipital assimilation can be associated with Chiari I malformation, which is characterized by the descent of the cerebellar tonsil through the foramen magnum into the upper cervical canal. The cerebellar tonsil would appear pointed, resembling a peg-like appearance [Figure 7]. Around 40% of the patients suffering from Chiari I malformation would develop cervical cord syrinx. This is particularly common when the patient is symptomatic.[8]
Export to PPT
Chiari 1 malformation is postulated to be related to a mesodermal defect that causes a congenitally small posterior fossa, leading to overcrowding of its contents, subsequently resulting in tonsillar herniation.[9] As a result, surgical management by posterior fossa decompression (e.g., suboccipital craniectomy and expansile duroplasty) can be considered for patients with symptomatic Chiari I malformation. The aim of posterior fossa decompression is to expand the posterior fossa volume, thereby decompressing the cervicomedullary junction, re-establishing cerebrospinal fluid circulation, and reducing the size of the syrinx.[10,11]
Cervical compressive myelopathyAlthough most cases of atlanto-occipital assimilation are asymptomatic, cervical cord compression can occur. Cervical cord compression is usually associated with basilar invagination, anteroposterior atlantoaxial subluxation, and Chiari malformation, as illustrated above [Figure 8].
Export to PPT
CONCLUSIONAtlanto-occipital assimilation is an entity that is easily missed in our daily reporting if not actively looked for. Aside from diagnosing it under dedicated imaging of the cervical spine, atlanto-occipital assimilation could also be incidentally diagnosed in the CT brain, where the atlanto-occipital joint may sometimes be partially included. Accurate reporting of atlanto-occipital assimilation is of clinical importance due to its association with atlantoaxial instability and cord compression. The following items are recommended to be mentioned while reporting cases of atlanto-occipital assimilation.
Type of atlanto-occipital assimilation (anterior arch assimilation/posterior arch assimilation/assimilation of both arches)
Presence of atlantoaxial instability (e.g., basilar invagination and anteroposterior atlantoaxial subluxation)
Presence of fusion of neighboring vertebral bodies (most commonly C2/3 congenital fusion)
Presence of complications (e.g., cord compression and Chiari malformation).
留言 (0)