Diabetic Peripheral Neuropathy (DPN) is a prevalent neurological complication of diabetes. Between 11% and 49% of prediabetic patients can exhibit symptoms, even in the disease’s preliminary stages (Ziegler et al., 2008; Lee et al., 2015; Won et al., 2017). After a decade of affliction, 60%–90% of diabetic individuals might display various degrees of neuropathic impairments, nearly half of which are categorized as DPN (Tesfaye et al., 2010). These complications encompass challenges such as balance difficulties, excruciating neuropathic pain, and, in advanced instances, irreversible nerve injuries leading to diabetic foot ulcers and possible amputations (Morrison et al., 2012; Selvarajah et al., 2019). On an individual level, age remains a persistent risk factor for DPN (Liu et al., 2019). As patients age and disease duration elongates, the likelihood of developing DPN intensifies (Cabezas-Cerrato, 1998). On a macro scale, with rapid economic growth coupled with accelerated aging populations, the global number of elderly diabetic patients and those with DPN is anticipated to continually ascend (Yang et al., 2010; Powell et al., 2012; Xu et al., 2013; Wang et al., 2023). In 2019, the population of elderly diabetic individuals (aged 65–99) was approximately 135.6 million, accounting for 19.3%. This number is projected to soar to 195.2 million by 2030 (Brussels, 2019; Saeedi et al., 2019). With many elderly already having underlying conditions, the onset of DPN may precipitate more grave consequences and comorbidities. Consequently, efficacious and economical prevention and treatment strategies, alongside evaluation metrics, are paramount for this group. Traditional Chinese Medicine (TCM) has demonstrated certain therapeutic efficacy in treating DPN, offering diverse treatments that alleviate symptoms and delay disease progression through multiple targets and pathways (Yang et al., 2022).
With the burgeoning emphasis on high-quality clinical trial research within the TCM realm, there has been an influx of randomized controlled trials (RCTs) exploring diverse TCM interventions for DPN. Yet, an overarching synthesis of evidence in this area is notably absent. Evidence mapping, a methodological tool that traces its origins to Yale University’s research on complementary and alternative medicine, mandates a comprehensive retrieval and systemic summation of research attributes and outcomes. By utilizing graphical elucidations, it furnishes a lucid and precise portrayal of the research field’s evidence, advancements, and existing challenges (Katz et al., 2003; Li et al., 2011; Schmucker et al., 2013), enhancing the efficacy and applicability of research in the area. This serves researchers, guideline creators, clinical physicians, and other stakeholders (Bragge et al., 2011; Miake-Lye et al., 2016; Li et al., 2019). Our study collates and analyzes RCTs from the past 6 years on multi-method TCM treatments for DPN. By integrating charts with evidence mapping, we offer a comprehensive view of the current state of research in the domain. This also encapsulates its limitations, contributing towards the enhancement of research quality in the field (Bastian et al., 2010), aiming to bridge the gap in research synthesis on evidence.
2 Methods2.1 Data sources and searchesWe systematically searched several databases including Wanfang, China National Knowledge Infrastructure (CNKI), VIP, SinoMed, PubMed, Web of Science, and Cochrane Library for studies on traditional Chinese medicine (TCM) interventions in diabetic peripheral neuropathy (DPN). Considering the increasing attention to TCM treatment aspects in the DPN field in 2017, this approach allowed us to collect a large number of relevant time newer publications to provide a comprehensive reference for future research. The search timeframe was from January 2017 to October 2022, including only Chinese and English articles. Both MeSH terms and free-text terms were used. The search terms included but were not limited to “糖尿病性周围神经病变”, “糖尿病周围神经病变”, “中医”, “"中药”, and their English counterparts “Diabetes peripheral neuropathy”, “DPN”, “traditional Chinese medicine”, “herbal medicine”, and “TCM”. The search strategy for Web of Science was: [TS = (Diabetes peripheral neuropathy) OR TS = (DPN)] AND [TS = (traditional Chinese medicine) OR TS=(herbal medicine) OR TS = (TCM)].
2.2 Study selection2.2.1 Inclusion criteriaThe studies considered for inclusion were clinical RCTs that investigated TCM treatments for DPN. Participants in these studies could be patients diagnosed with DPN, with no restrictions regarding age, gender, disease duration, or comorbidities. The interventions examined in the selected studies could encompass a range of treatments including oral Chinese herbal decoctions, granules, proprietary Chinese medicines, Chinese medicine injections, acupuncture, foot baths, massage, fumigation washing, integrated TCM care, combined TCM therapies, etc.
2.2.2 Exclusion criteriaStudies were excluded if they were duplicated publications, inaccessible full-texts, animal or cellular experiments.
2.3 Data extraction and quality assessmentAll identified references were imported into NoteExpress3.7.0 for management. A group of five researchers conducted the literature screening, with one appointed as the team leader. To ensure consistency, 100 papers were pre-screened as a calibration exercise before the main screening, and uniform screening criteria were established. Titles and abstracts were initially screened for relevance. Potentially relevant papers were further assessed by reading the full text. Discrepancies during the screening were resolved through discussions led by the team leader. Relevant information was extracted using a standardized form, which included publication year, authors, sample size, trial period, combined drugs, interventions (categorized as oral Chinese medicine, proprietary medicine, TCM external treatments, herbal injections, integrated TCM care, multi-therapy combination, and others), and outcome measures.
2.4 Classification of TCM interventionsTo provide a clearer picture of TCM treatments for DPN, we categorized the TCM interventions from the included studies into seven types: oral Chinese medicines (including herbal decoctions and granules), proprietary Chinese medicines, external TCM therapies (like acupuncture, foot baths, massages, and fumigation), comprehensive TCM nursing, multi-therapy combinations, herbal injections, and others (which covers TCM exercise therapy and music therapy, etc.).
2.5 Data synthesis and analysisDescriptive statistics were presented both in text and graphical forms. Graphs were plotted using Origin 2021 software, with trend developments represented using line graphs, category distributions in pie charts, and evidence distributions in bubble charts (Tian et al., 2019).
3 Results3.1 Study selectionA total of 4,454 articles published over the past 6 years were identified through database searches. Of these, 1,229 RCTs on TCM interventions for DPN were included. The literature screening process and results are depicted in Figure 1.
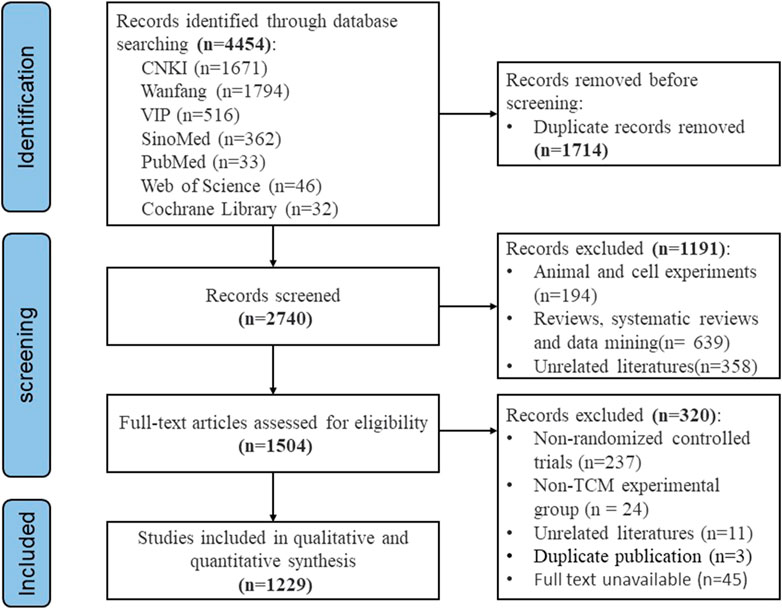
Figure 1. PRISMA flow diagram of literature selection process.
3.2 Publication trendFrom January 2017 to October 2022, we analyzed 1,229 published RCTs of TCM interventions for DPN. Over the five complete years (2017–2021) included, the annual average number of publications was 223, with no significant fluctuations, indicating a plateau in the number of publications. It is evident that Wanfang has indexed the most articles on TCM interventions for DPN. This trend is illustrated in Figure 2.
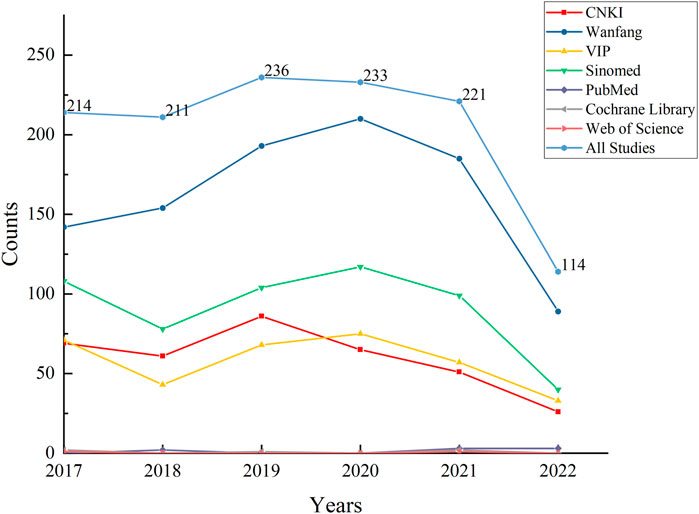
Figure 2. Overall publication trends of RCTs on TCM interventions for diabetic peripheral neuropathy over the past 6 years versus publication trends across databases.
3.3 Analysis of sample sizeAn assessment of the scale of the included RCTs revealed a range in sample size from a minimum of 28 to a maximum of 900. The majority of studies had a sample size between 50 and 100, followed by studies with a sample size between 100 and 200. Detailed distributions are presented in Table 1.
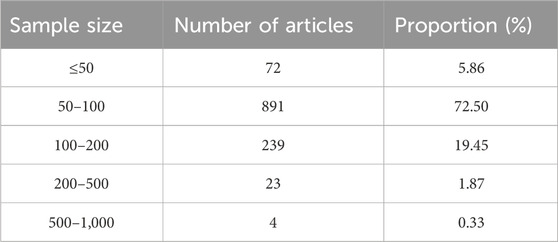
Table 1. Sample sizes of RCTs on TCM interventions for diabetic peripheral neuropathy over the past six years.
3.4 Positive drug usageOf the 1,229 included studies, 775 (63.06%) explicitly used positive agents, including mecobalamin, thioctic acid, and prostaglandins. Another 73 studies (5.94%) employed drugs described with phrases like “neurotrophic and circulatory improvement.” In contrast, 381 studies (31.00%) either did not use or did not mention positive drugs. These agents generally showed various degrees of improvement in DPN patients’ symptoms and signs (Zhang and Ning, 2008; Han et al., 2012; Shin et al., 2013; Ma et al., 2022).
Mecobalamin, an active Vitamin B12 formulation widely used in many parts of the world for DPN treatment, promotes nucleic acid and protein synthesis within neurons. It significantly aids myelin formation and axonal regeneration, repairing damaged nerve cells and improving nerve conduction velocity, ultimately enhancing symptom signs (Sawangjit et al., 2020; Branch Group Of Neurological Complications, 2021).
Thioctic acid, a potent antioxidant, acts by inhibiting lipid peroxidation, enhancing blood flow in neurotrophic vessels, and boosting the activity of the Na + -K + -ATPase enzyme. It directly neutralizes reactive oxygen clusters and free radicals, protecting endothelial function (Ziegler et al., 2011; Han et al., 2012; Branch Group Of Neurological Complications, 2021).
Prostaglandins, physiologically active unsaturated fatty acids, and related compounds can increase cyclic adenosine monophosphate (cAMP) levels in vascular smooth muscle cells, relaxing vascular smooth muscles, reducing blood viscosity, and improving microcirculation (Branch Group Of Neurological Complications, 2021).
3.5 The distribution of TCM therapiesOral Chinese medicine research dominated with 453 studies (36.86%), followed by external TCM therapies with 378 (30.76%). The remaining categories included multi-therapy combinations (244 studies), comprehensive TCM nursing (73), proprietary Chinese medicines (57), herbal injections (19), and others (5). The distribution is illustrated in Figure 3.
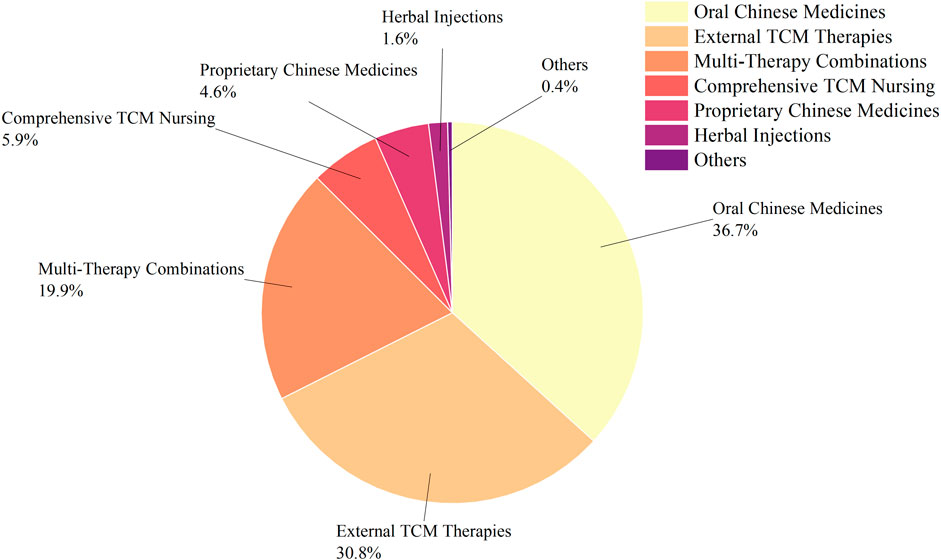
Figure 3. Classification of TCM interventions in RCTs for DPN treatment over the past 6 years.
Among the 453 studies with oral Chinese medicine as an intervention: The most frequently occurring interventions (with a frequency of ≥5) are, in descending order: Huangqi Guizhi Wuwu Decoction, Buyang Huanwu Decoction, Danggui Sini Decoction, Duhuo Jisheng Decoction, and Taohong Siwu Decoction.
For the 378 studies involving external TCM therapies: The most frequent interventions (with a frequency of ≥5) are, in descending order: acupuncture, foot bath, fumigation combined with external washing, external application, moxibustion, foot bath combined with massage, acupoint injection, external wash, external application combined with acupuncture, foot bath combined with external application, iontophoresis, foot bath combined with acupuncture, fumigation, fumigation combined with external washing and acupuncture, massage, foot bath combined with acupoint injection, and topical rubbing.
A detailed breakdown of the frequencies for each intervention is presented in Table 2. A comprehensive overview of oral Chinese medicines can be found in Tables 3, 4.
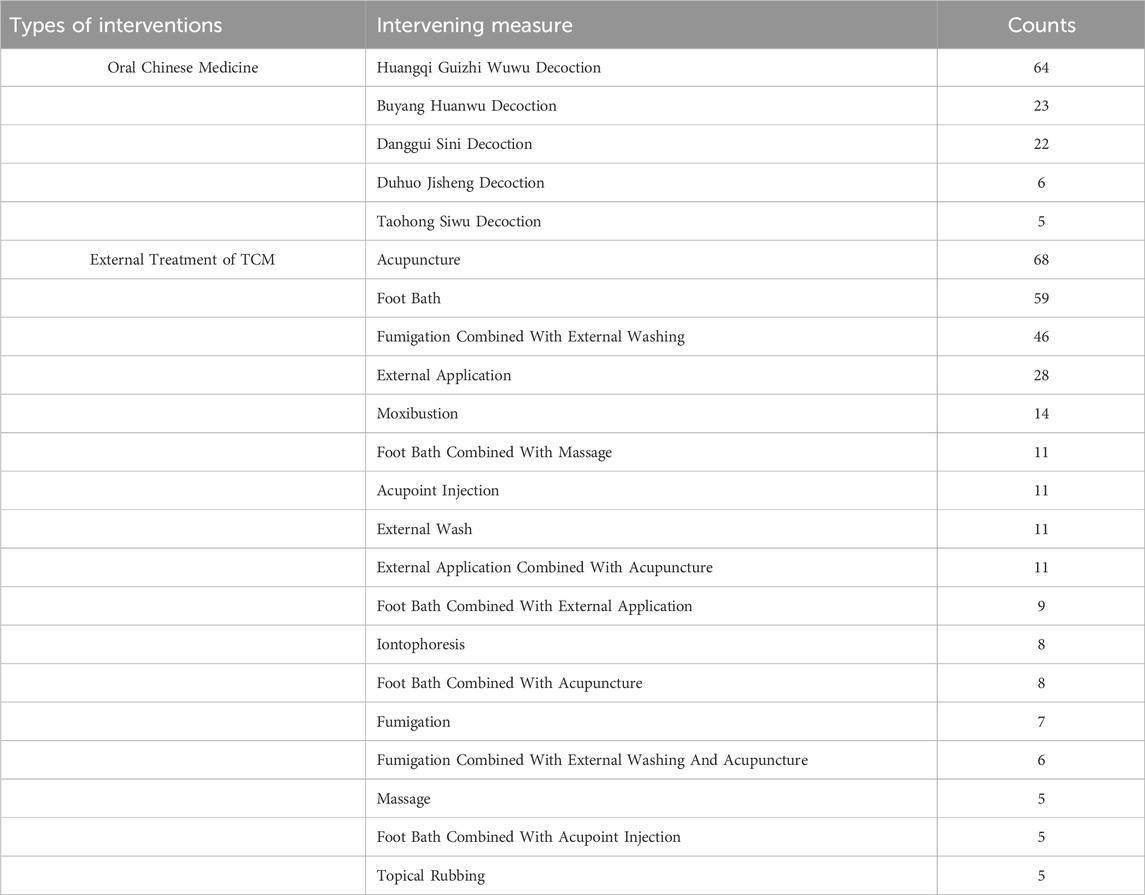
Table 2. Frequency of various intervention methods.
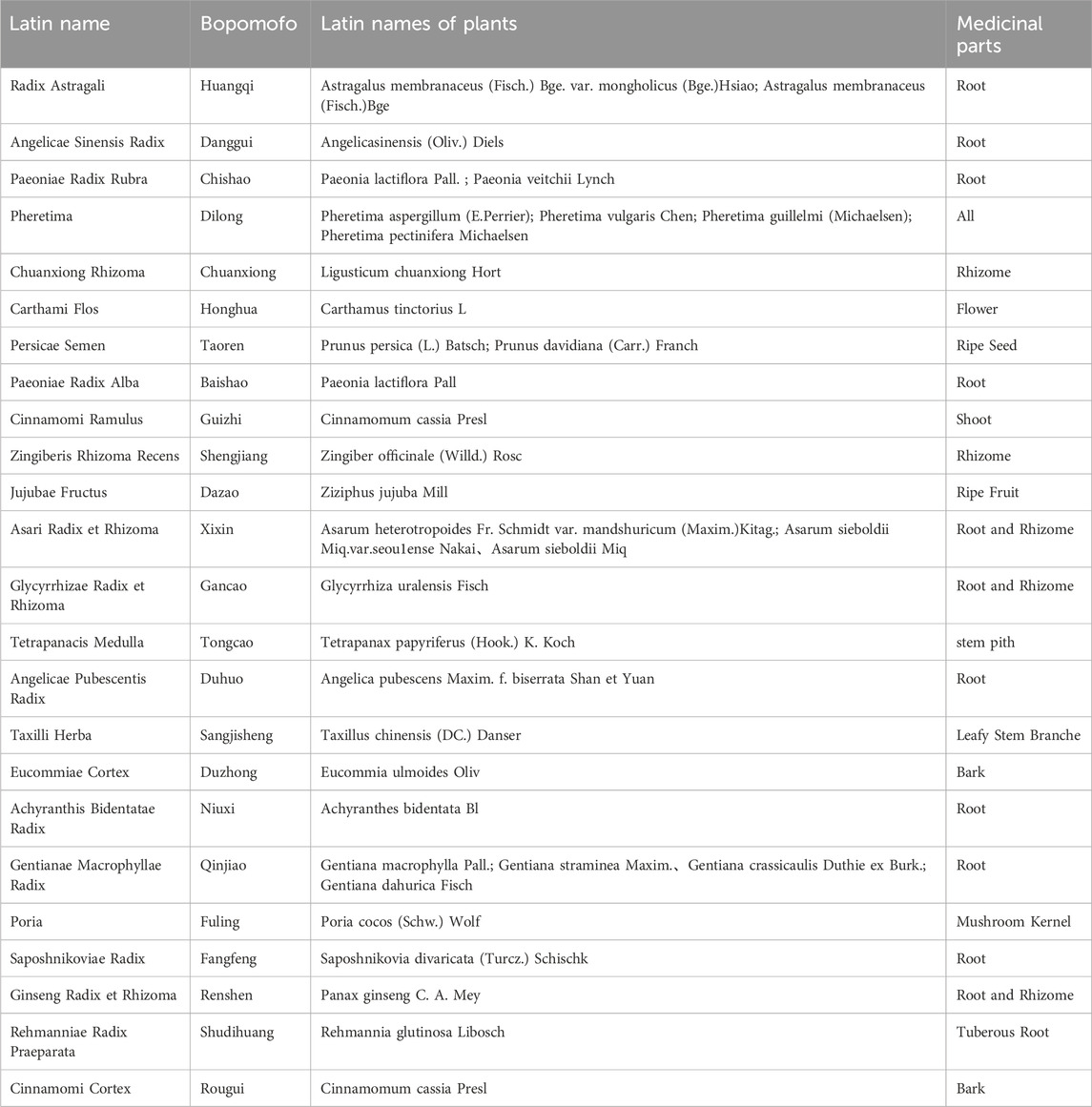
Table 3. Top 5 oral Chinese medicines: introduction to medicinal plants.
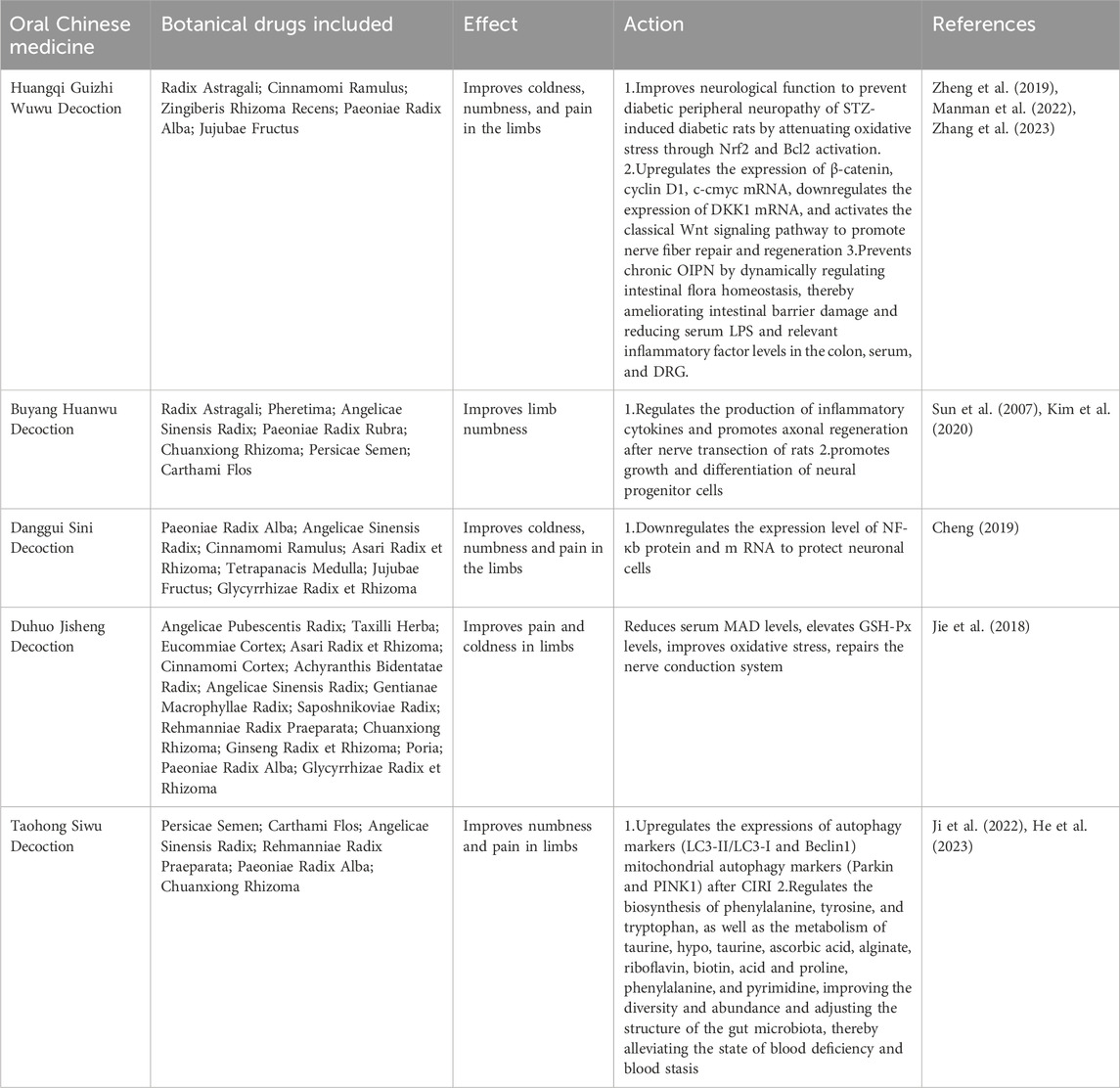
Table 4. Composition, therapeutic effects, and pharmacological actions of oral Chinese medicines.
3.6 Duration of treatmentOf the 1,229 studies, 1,103 (89.75%) specified the duration of treatment, while 126 (10.25%) did not. Among the seven categories of interventions, Comprehensive TCM Nursing had the highest proportion of studies that did not specify the duration at 67.1%. Conversely, Herbal Injections (0%), Others (0%), and Proprietary Chinese Medicines (3.51%) had the lowest proportions of unspecified durations. Among the studies that specified the duration, Proprietary Chinese Medicines had the longest average treatment duration at 77.07 days, while Comprehensive TCM Nursing had the shortest at 31.67 days. See Table 5.
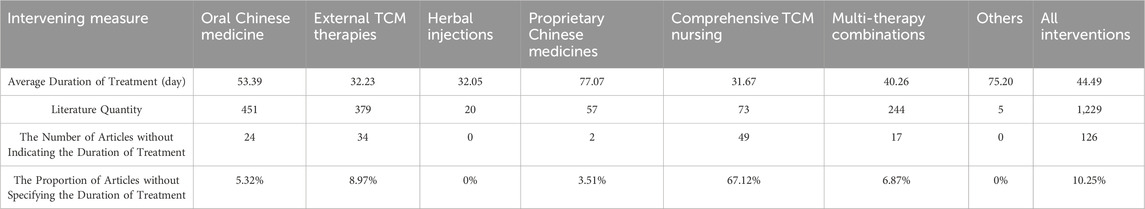
Table 5. Average duration of intervention and proportion of studies without specified duration.
3.7 Outcome measuresA comprehensive analysis of the outcome measures employed in the included RCT studies on TCM treatment for DPN was conducted. These outcome measures were categorized into 17 types, including neurophysiological evaluations, neuropathy scores, safety indicators, hemorheology, etc. Details for some of the outcome measure categories are provided in Table 6.
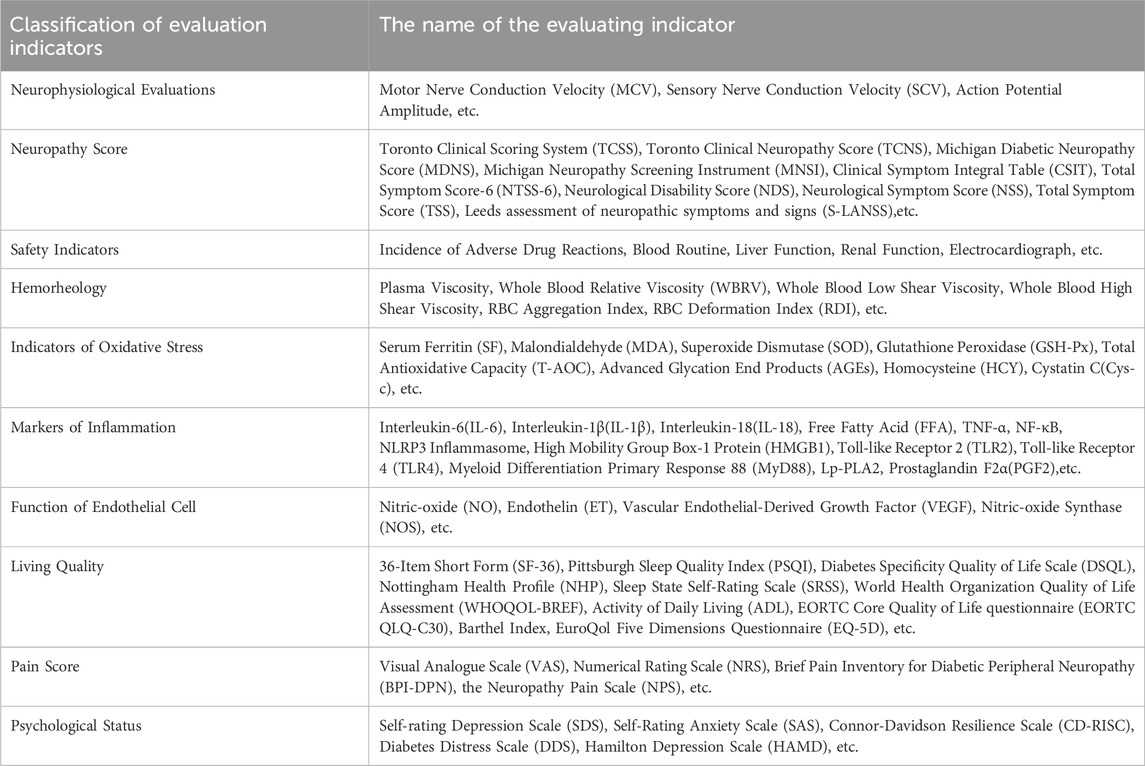
Table 6. Details of selected outcome measure categories.
Based on the assessment metrics utilized in the included RCT, studies on TCM, treatment for DPN, we categorized them into 17 types. The detailed contents for some of these categories are listed in Table 7.
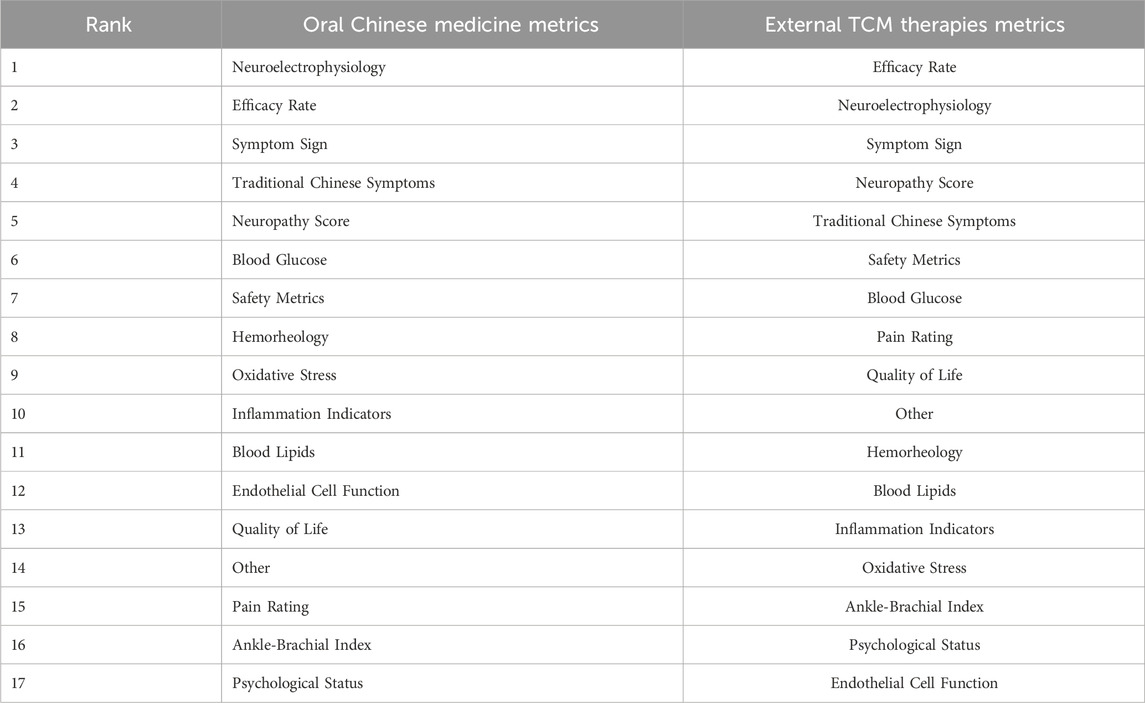
Table 7. Evaluation metrics rankings by treatment approach.
Bubble diagrams indicate that clinical RCTs of common oral Chinese medicine treatments for diabetic peripheral neuropathy often focus on metrics such as Neuroelectrophysiology, Efficacy Rate, and Symptom Sign. In contrast, those metrics like Endothelial Cell Function, Quality of Life, and Ankle-Brachial Index receive less attention, as shown in Figure 4.
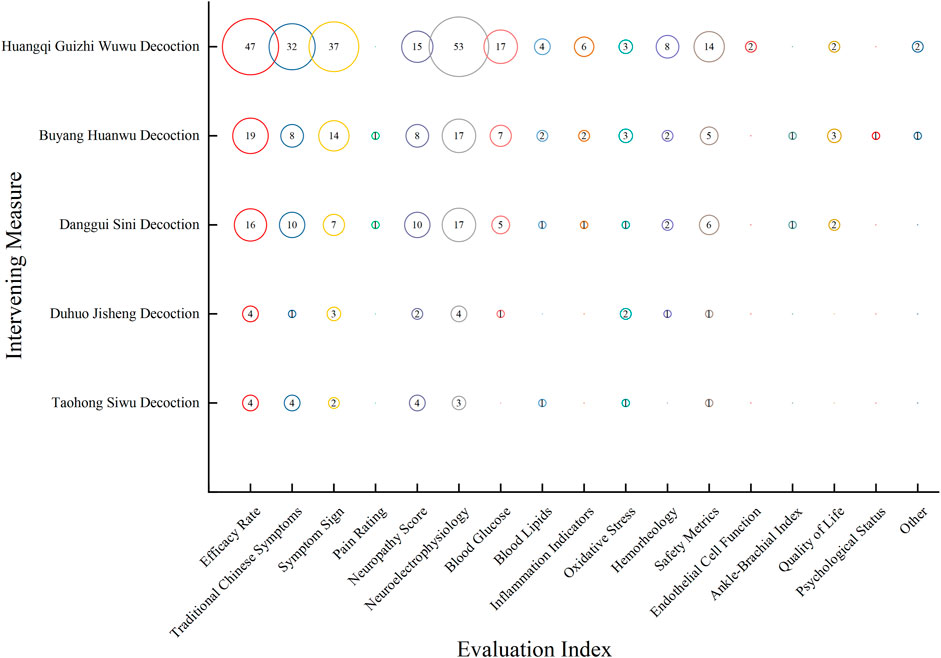
Figure 4. Distribution of evidence on evaluation metrics in clinical RCTs for the treatment of DPN with oral Chinese medicine over the last 6 years. The size of each circle represents the number of publications that employed a particular evaluation metric for this intervention.
Clinical RCTs of prevalent TCM External Treatment pay more attention to Efficacy Rate, Neuroelectrophysiology, and Symptom Sign, while metrics such as Endothelial Cell Function and Psychological Status are often overlooked. Both treatment approaches prioritize Neuroelectrophysiology, Efficacy Rate, and Symptom Sign, with lesser emphasis on Ankle-Brachial Index and Psychological Status, as depicted in Figure 5.
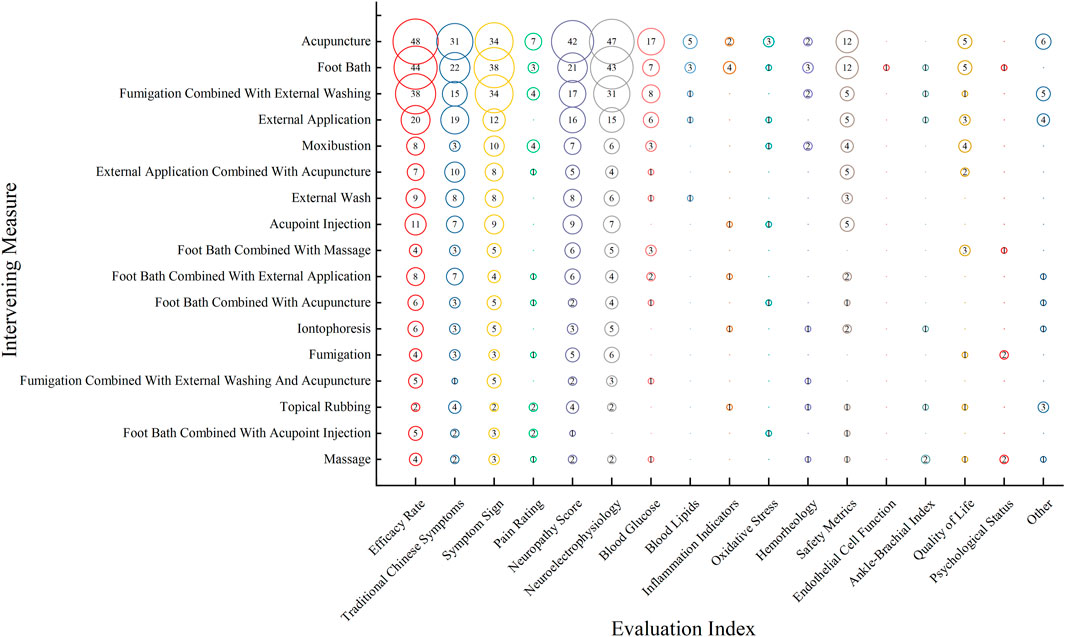
Figure 5. Distribution of evidence on evaluation metrics in Clinical RCTs for the treatment of DPN with TCM external treatment over the last 6 years. The size of each circle represents the number of publications that employed a particular evaluation metric for this intervention.
4 DiscussionThis study represents the first comprehensive examination of clinical RCTs regarding the TCM treatment of DPN over the past 6 years, using an evidence map approach. Through an in-depth analysis encompassing publication trends, study scale, positive drug usage, intervention categories, duration of treatment, and evaluation metrics, we shed light on the current evidence, research advancements, and challenges in TCM’s treatment of DPN. This review aims to guide future RCT research in this domain, assisting in refining both research focus and design.
4.1 TCM treatment for DPN: integrative trends and requirementsFrom the 1,229 RCT articles reviewed, the number of TCM studies addressing DPN has remained relatively stable over the past 6 years. Notably, up to 80% of these studies were of small scale, with sample sizes of fewer than 100 participants. Several studies displayed design flaws such as ambiguous sample sources, insufficient descriptions of randomization and blinding methods, a lack of baseline characteristics for trial participants, and an absence of drug washout periods, all of which could significantly influence the study outcomes.
However, concurrently, we observed a significant trend integration where nearly 70% of the interventions combined modern drugs like metformin, alpha-lipoic acid, and ipragliflozin with TCM. This combination potentially offers a dual therapeutic approach, fully harnessing the rapid and quantitative effects of modern drugs and the holistic and long-term benefits of TCM. For instance, while modern drugs might swiftly stabilize the blood sugar levels in diabetic patients, TCM can provide long-term health benefits by adjusting the overall balance in the body. Additionally, TCM often emphasizes moderating lifestyle habits, dietary practices, and emotional states, crucial aspects that might be overlooked in modern medicinal treatments.
Such integration underscores the advantages of combining traditional and modern medicine, offering patients a more comprehensive and integrative treatment modality. However, studies solely relying on traditional Chinese methods remain scarce. This may reflect an integration trend between TCM and contemporary medicine, suggesting an imperative for more exclusive TCM clinical trials to ascertain its efficacy. In the future, conducting large-scale, multi-center clinical randomized controlled trials would be valuable to confirm the effectiveness of TCM interventions. Such studies could compare TCM treatments with standard medications to assess non-inferiority, thus offering evidence to back the use of TCM as a standalone option in the prevention and management of diabetic peripheral neuropathy. (Hulley et al., 2017; Wang et al., 2022).
The inconsistency observed in the diagnostic criteria across RCT literature, with some studies providing clear guidelines while others merely confirming a diagnosis of diabetic peripheral neuropathy, underlines the necessity for uniform diagnostic standards in future research. To enhance the rigor and comparability of RCTs, it is crucial to use explicit diagnostic criteria. Researchers are encouraged to consult established guidelines, such as the American Diabetes Association’s position statement on Diabetic Neuropathy (Pop-Busui et al., 2017), the Standards of Medical Care in Diabetes-2020 (Association, 2020), and the Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition) (Society, 2021), to ensure consistency and reliability in the field.
4.2 Diversity of outcome measures and the necessity of quantification in TCM syndrome diagnosisA variety of efficacy evaluation indices were used, with DPN diagnostic-related indices, such as symptom and sign assessment, neurophysiological tests, and nerve lesion scoring (Fang et al., 2017), as well as TCM syndrome scores and overall efficacy rates being the primary ones. However, attention to the ankle-brachial index and psychological states was notably lacking. As a commonly used composite index, the efficacy rate is frequently applied based on the “Guidelines for Clinical Research of New Chinese Medicines” and “Standards for the Evaluation of TCM Syndromes” and combines various evaluation metrics, causing significant variability between studies and a lack of scientific rigor (Zhang et al., 2020). Future studies should opt for primary, singular symptoms or signs to determine relative objective evaluation criteria. It's also recommended that DPN researchers collaboratively explore a Core Outcome Set (COS) and develop common COS guidelines, aiming to simplify trial design, select efficacy evaluation indices, reduce outcome reporting bias, and minimize inter-study outcome reporting heterogeneity (Clarke, 2007; Yu et al., 2016).
Diagnosis and treatment in TCM are determined by a combination of disease diagnosis, symptoms, and syndrome identification. TCM syndrome is an essential aspect in addition to disease diagnosis and symptomatology. Issues with the TCM syndrome scoring system in RCT studies of TCM treatment for DPN include the lack of scientific quantification of symptom scoring and the subjective nature of efficacy judgments. It's suggested that future research could utilize a scoring system for syndrome efficacy metrics, based on the severity of DPN-related symptoms and signs and the contribution defined by TCM syndrome characteristics, thereby transforming TCM syndrome metrics into objective, quantifiable ones.
4.3 Comprehensive perspectives on DPN-related complications and TCM treatmentDPN and lower limb vascular lesions are pivotal contributors to diabetic foot ulcers. Their severity has been positively correlated (Song, 2018). The ankle-brachial index, a significant measure for evaluating lower limb arterial status, provides considerable prognostic insight for DPN patients (Hinchliffe et al., 2020; Sorber and Abularrage, 2021).
Interestingly, between 26% and 50% of DPN patients also report symptoms of anxiety or depression (Gore et al., 2005; Zhao and Qi, 2022). Persistent symptoms, such as abnormal limb sensations and functional impairments in DPN patients, increase their susceptibility to depressive states. Such depressive conditions not only intensify their pain and numbness but also diminish their motivation to control blood sugar, exacerbating their condition and creating a vicious cycle (DU Shun-Tang et al., 2022).
Several oral TCM medications have demonstrated efficacy in treating diabetes-associated depression by attenuating insulin resistance, mitigating oxidative stress, and modulating the nervous system (Lu et al., 2020). Furthermore, non-pharmacological TCM interventions like acupuncture and massage excel in alleviating pain, anxiety, and depressive symptoms, significantly enhancing patients’ quality of life (Yan, 2013; Wang et al., 2018). We recommend that future research on TCM for DPN broaden its scope beyond merely alleviating symptoms to encompass the overall quality of life and mental health of patients. This approach will contribute to a more holistic evidence base supporting the use of TCM in treating DPN.
Our findings indicate that non-pharmacological treatments like acupuncture and moxibustion, alongside oral Chinese medicine, are increasingly utilized for DPN management. We recommend that future research should focus on conducting more RCTs and meta-analyses specifically on these non-pharmacological Chinese medicine therapies, such as acupuncture for DPN. This approach will enable a more comprehensive evaluation of the effectiveness of non-pharmacological Chinese medicine treatments on DPN.
4.4 Study limitations and future directionsWhile this study provides substantial evidence for the clinical investigation of TCM in treating DPN, it is not without limitations:
The search scope was confined to clinical randomized controlled trials published in Chinese and English databases over the recent 6 years, resulting in a relatively narrow range of included study types. To gain a more comprehensive understanding of this field, future studies should consider broadening their search criteria to encompass various types of studies and explore other literature sources, such as clinical trial registration platforms.
In illustrating evidence distribution, interventions were categorized and distinguished based on type. This method’s shortcoming is that some intervention categories may encapsulate different drugs and operational methods. Furthermore, interventions within the same category might not be uniformly implemented, potentially influencing the research outcomes to varying degrees. No detailed quality assessment was carried out for the included studies, suggesting that the evidence distribution might be affected by biases to some extent.
Building on the previous discussion, we acknowledge the absence of a quantitative synthesis of data as a limitation. Future studies should incorporate quantitative analyses, such as meta-analyses, to provide more definitive conclusions regarding the effectiveness of TCM treatments for DPN. Such efforts will help clarify the magnitude of effects of various TCM treatments and identify promising approaches for further clinical investigation. By addressing these limitations and embracing a more comprehensive research methodology, future research can significantly advance our understanding and application of TCM in treating DPN.
5 ConclusionThis study systematically evaluated the clinical RCTs of TCM in addressing DPN, a significant complication of diabetes, using an evidence mapping approach. Despite the breadth of studies in this area, challenges such as inconsistent trial designs, predominant focus on standalone TCM treatments, varied intervention methods, and restricted evaluation metrics remain (Zhang et al., 2021).
To improve research quality regarding this pivotal diabetes complication, future studies should emphasize rigorous RCT design and apt selection of evaluation criteria. Moreover, establishing an online research database specifically tailored for TCM treatment of DPN—with a standardized literature extraction format—would be beneficial, promoting collaborative research and facilitating re-assessment of data. By integrating global research expertise, it's essential to advance the synergy of TCM and modern medicine, aiming to enhance therapeutic outcomes and better the quality of life for patients grappling with this complication.
Our research accentuates the profound role of TCM in tackling DPN as a notable diabetes complication, providing meaningful insights for informed medical decisions and optimized clinical practices. This investigation endeavors to bolster the scientific underpinning of clinical practices, aiming to elevate patient satisfaction and understanding of DPN within the larger context of diabetes-related complications.
In conclusion, the potential of TCM in addressing DPN as a significant diabetes complication is evident. We look forward to further research that explores its potential efficacy in this domain.
Data availability statementThe raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Author contributionsYF: Writing–original draft, Writing–review and editing. YW: Writing–original draft, Writing–review and editing. ZL: Writing–original draft, Writing–review and editing. KH: Writing–original draft, Writing–review and editing. YG: Writing–original draft. SX: Writing–original draft. QL: Writing–original draft. XL: Writing–original draft, Writing–review and editing. GZ: Writing–review and editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the Science and Technology Innovation Project of China Academy of Chinese Medical Sciences (No. CI2021A01608).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer XG declared a shared parent affiliation with the author(s) YF, YG, and SX to the handling editor at the time of review.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ReferencesBastian, H., Glasziou, P., and Chalmers, I. (2010). Seventy-five trials and eleven systematic reviews a day: how will we ever keep up? PLos Med. 7 (9), e1000326. doi:10.1371/journal.pmed.1000326
PubMed Abstract | CrossRef Full Text | Google Scholar
Bragge, P., Clavisi, O., Turner, T., Tavender, E., Collie, A., and Gruen, R. L. (2011). The Global Evidence Mapping Initiative: scoping research in broad topic areas. BMC Med. Res. Methodol. 11, 92. doi:10.1186/1471-2288-11-92
PubMed Abstract | CrossRef Full Text | Google Scholar
Branch Group Of Neurological Complications (2021). Expert consensus on diagnosis and treatment of diabetic neuropathy (2021 edition). Chin. J. Diabetes Mellitus 13 (6), 540–557. doi:10.3760/cma.j.cn115791-20210310-00143
CrossRef Full Text | Google Scholar
Brussels (2019). IDF diabetes atlas. 9th edn. USA: International Diabetes Federation.
Cabezas-Cerrato, J. (1998). The prevalence of clinical diabetic polyneuropathy in Spain: a study in primary care and hospital clinic groups. Neuropathy Spanish Study Group of the Spanish Diabetes Society (SDS). Diabetologia 41 (11), 1263–1269. doi:10.1007/s001250051063
PubMed Abstract | CrossRef Full Text | Google Scholar
Cheng, S. (2019). Exploration of Danggui Sini decoction on GlucoseuriaBased on NF-kappa B signaling pathway protectivemechanism of peripheral neuropathy indiabetic rats. Changchun Univ. Chin. Med.
Fang, Z., Wu, Y., and Zhao, J. (2017). Guidelines for clinical diagnosis and treatment of diabetic peripheral neuropathy in traditional Chinese medicine (2016 edition). J. Tradit. Chin. Med. 58 (07), 625–630. doi:10.13288/j.11-2166/r.2017.07.025
CrossRef Full Text | Google Scholar
Gore, M., Brandenburg, N. A., Dukes, E., Hoffman, D. L., Tai, K. S., and Stacey, B. (2005). Pain severity in diabetic peripheral neuropathy is associated with patient functioning, symptom levels of anxiety and depression, and sleep. J. Pain Symptom Manage. 30 (4), 374–385. doi:10.1016/j.jpainsymman.2005.04.009
PubMed Abstract | CrossRef Full Text | Google Scholar
Han, T., Bai, J., Liu, W., and Hu, Y. (2012). A systematic review and meta-analysis of α-lipoic acid in the treatment of diabetic peripheral neuropathy. Eur. J. Endocrinol. 167 (4), 465–471. doi:10.1530/EJE-12-0555
PubMed Abstract | CrossRef Full Text | Google Scholar
He, Y., Jiang, H., Du, K., Wang, S., Li, M., Ma, C., et al. (2023). Exploring the mechanism of Taohong Siwu Decoction on the treatment of blood deficiency and blood stasis syndrome by gut microbiota combined with metabolomics. Chin. Med. 18 (1), 44. doi:10.1186/s13020-023-00734-8
PubMed Abstract | CrossRef Full Text | Google Scholar
Hinchliffe, R. J., Forsythe, R. O., Apelqvist, J., Boyko, E. J., Fitridge, R., Hong, J. P., et al. (2020). Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes/Metabolism Res. Rev. 36 (S1), e3276. doi:10.1002/dmrr.3276
PubMed Abstract | CrossRef Full Text | Google Scholar
Hulley, S. B., Cummings, S. R., Browner, W. S., Grady, D. G., and Newman, T. B. (2017). Designing clinical research. 4 ed. Beijing: Peking University Medical Press.
Ji, Z. J., Shi, Y., Li, X., Hou, R., Yang, Y., Liu, Z. Q., et al. (2022). Neuroprotective effect of Taohong Siwu decoction on cerebral ischemia/reperfusion injury via mitophagy-NLRP3 inflammasome pathway. Front. Pharmacol. 13, 910217. doi:10.3389/fphar.2022.910217
PubMed Abstract | CrossRef Full Text | Google Scholar
Jie, C., Lixin, T., Suzhen, N., and Chunfang, G. (2018). The effect of "du huo ji sheng tang" given with oral administration or fumigation to the MDA and GSH-px levels of Qi deficiency and blood stasis type of diabetic patients with peripheral neuropathy. Jiangsu J. Traditional Chin. Med. 50 (12), 27–30.
Katz, D. L., Williams, A. L., Girard, C., Goodman, J., Comerford, B., Behrman, A., et al. (2003). The evidence base for complementary and alternative medicine: methods of Evidence Mapping with application to CAM. Altern. Ther. Health Med. 9 (4), 22–30.
PubMed Abstract | Google Scholar
Kim, K. J., Hwang, J., Park, J. Y., and Namgung, U. (2020). Augmented Buyang Huanwu Decoction facilitates axonal regeneration after peripheral nerve transection through the regulation of inflammatory cytokine production. J. Ethnopharmacol. 260, 113063. doi:10.1016/j.jep.2020.113063
PubMed Abstract | CrossRef Full Text | Google Scholar
Lee, C. C., Perkins, B. A., Kayaniyil, S., Harris, S. B., Retnakaran, R., Gerstein, H. C., et al. (2015). Peripheral neuropathy and nerve dysfunction in individuals at high risk for type 2 diabetes: the PROMISE cohort. Diabetes Care 38 (5), 793–800. doi:10.2337/dc14-2585
PubMed Abstract | CrossRef Full Text | Google Scholar
Li, L., Yang, K., Tian, J., Sun, T., Zhang, P., Yi, K., et al. (2011). Single-step mineralization of woodpile chitosan scaffolds with improved cell compatibility. Chin. J. Evidence-Based Pediatr. 6 (03), 230–237. doi:10.1002/jbm.b.31811
PubMed Abstract | CrossRef Full Text | Google Scholar
Li, M., Zhang, F., Cai, R., Wang, J., Wang, P., Zhang, J., et al. (2019). The current situation of study on evidence mapping. Chin. J. Drug Eval. 36 (03), 161–164.
Lu, Y., An, T., Tian, H., Gao, X., Wang, F., Wang, S., et al. (2020). Depression with comorbid diabetes: what evidence exists for treatments using traditional Chinese medicine and natural products? Front. Pharmacol. 11, 596362. doi:10.3389/fphar.2020.596362
PubMed Abstract | CrossRef Full Text | Google Scholar
Ma, Y., Chen, J., Huang, X., and Liu, Y. (2022). The efficacy and safety of mecobalamin combined with Chinese medicine injections in the treatment of diabetic peripheral neuropathy: a systematic review and Bayesian network meta-analysis of randomized controlled trials. Front. Pharmacol. 13, 957483. doi:10.3389/fphar.2022.957483
PubMed Abstract | CrossRef Full Text | Google Scholar
Manman, L., Zhenfeng, F., Jian, J., Junfeng, G., Jianfang, C., Chunping, H. U., et al. (2022). Dose-response relationship of different doses of Huangqi Guizhi Wuwu Decoction in the treatment of diabetic peripheral neuropathy and their influence on classic Wnt signaling pathway. Mod. J. Integr. Traditional Chin. West. Med. 31 (14), 1922–1927. doi:10.3969/j.issn.1008-8849.2022.14.005
CrossRef Full Text | Google Scholar
Miake-Lye, I. M., Hempel, S., Shanman, R., and Shekelle, P. G. (2016). What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst. Rev. 5, 28. doi:10.1186/s13643-016-0204-x
PubMed Abstract | CrossRef Full Text | Google Scholar
Morrison, S., Colberg, S. R., Parson, H. K., and Vinik, A. I. (2012). Relation between risk of falling and postural sway complexity in diabetes. Gait Posture 35 (4), 662–668. doi:10.1016/j.gaitpost.2011.12.021
PubMed Abstract | CrossRef Full Text | Google Scholar
Pop-Busui, R., Boulton, A. J., Feldman, E. L., Bril, V., Freeman, R., Malik, R. A., et al. (2017). Diabetic neuropathy: a position statement by the American diabetes association. Diabetes Ca
留言 (0)