A perforated peptic ulcer (PPU) is a common disease that requires emergency surgery and is the cause of one-third of all peptic ulcer-related deaths (1, 2). Despite a decrease in the absolute number of admissions and surgeries performed, there has been an increase in the absolute number of in-hospital and postoperative mortality rates (2–4). Thus, in recent years, in-hospital mortality for PPUs in Russia has increased from 12.11% to 13.23% and postoperative mortality from 10.77% to 12.5% (3). This trend is consistent with data from other countries. According to observational studies, the deterioration in results can be attributed to a significantly increased rate of comorbidity which has led to multiple increases in patients with American Society of Anesthesiologists (ASA) scores of 4–5 over the last several decades (2, 4).
These statistical trends have prompted a search for ways to improve patient outcomes. Advances in endoscopic technology have led to an increasing trend of laparoscopic surgery for PPUs worldwide. It is currently assumed that laparoscopic surgeries are either comparable to or substantially superior to open surgeries (1).
The number of systematic reviews (SRs) and meta-analyses in surgery is growing exponentially. However, heterogeneity, certain types of biases, and sparse data can cause misrepresentation of the combined results of primary studies in a pooled analysis. Meta-epidemiology, as a form of evidence synthesis, allows for the pooling of data and assessment of the diversity present in multiple and overlapping SRs (5, 6).
Aim of the researchThis study aimed to summarize evidence from systematic reviews of randomized controlled trials (RCTs) and reanalyze outcome data on laparoscopic suture repair of PPUs using trial sequential analysis.
Materials and methodsThere is no existing guidance on how to incorporate data excluded from primary studies into overviews of reviews appropriately (5). In the present meta-review, we used a meta-epidemiological approach and trial sequential analysis (TSA) that combined a conventional meta-analysis methodology with meta-analytic sample size considerations.
Search strategyComprehensive search without language restriction was conducted by all the authors. The Cochrane Library, PubMed, Embase, MEDLINE, CINAHL, eLibrary, and ClinicalTrials.gov were searched before 1 June 2024 for all relevant systematic reviews.
An electronic search with filters designed for retrieving systematic reviews was conducted (7). A supplemental manual search for additional potentially relevant publications was subsequently conducted using citation searching and the “snowball” method. The result of the comprehensive systematic review search is presented in a PRISMA flow diagram.
Inclusion criteriaFor the meta-review, only SRs (with or without meta-analyses) of laparoscopic repair of PPUs were identified and considered. The study design of interest for the TSA was the RCTs included in the relevant SRs.
Exclusion criteriaThe exclusion criteria included studies of any design other than RCT, articles in a language other than English and systematic reviews without a statistical analysis of results.
Data collectionThe authors independently extracted data from the selected studies. The basic information about the characteristics of each systematic review included authors, year of publication, number of included studies, their design, and number of participants. Information about the RCTs included in the selected SRs (authors, years of research, country of research, and number of participants) was also extracted. We mapped primary study overlap within the included SRs as suggested by Pollock et al. (2023) (5).
Assessment of methodological qualityTwo meta-review authors (SP and TN) independently assessed the methodological quality of the selected SRs. Critical appraisal tools from the Oxford Centre for Evidence-Based Medicine were used (8). Information about the risk of bias of the RCTs contained within the relevant SRs was presented as narrative data.
Statistical analysisCopenhagen Trial Unit's software was used in the TSA to control for random errors and repetitive testing of the accumulated data.
TSA is a statistical tool designed to eliminate false positive conclusions (type I errors) and false negative conclusions (type II errors), providing more information on the precision and uncertainty of meta-analysis results. TSA is a methodology that combines the estimation of the total sample sizes of all included trials to meta-analyze the threshold for statistical significance (9).
For the determination of the sample size and to provide strong evidence of an intervention effect, the diversity-adjusted required information size (DARIS) was calculated. DARIS also allows one to set the boundaries of futility and indicate when a conclusion of no effect can be made conclusively before the required amount of information is reached (9).
We calculated the mean and standard deviation from the sample size and the median, range, or interquartile range for the meta-analytic reanalysis if necessary (10). The TSA was conducted according to the statistical methodology presented by Thorlund et al. (9). We estimated the diversity measure used to quantify heterogeneity (D2) and calculated the DARIS. The trial sequential monitoring boundaries were constructed on the basis of the DARIS using the Land and DeMets method (11). If the required sample size is reached, the boundaries of sequential monitoring or futility zone are crossed and further research may not be necessary.
The statistical computations of the TSA were performed by two co-authors (S.P. and T.N.). The type I (α risk) and type II (β risk) errors were set to 5% and 20%, respectively. We considered the control (laparotomy) group event proportion (Pc) as binary data and made an a priori estimate of a realistic intervention effect, expressed as a relative risk reduction (RRR) of 10%.
For continuous outcomes, the DARIS was calculated from an alpha error of 5%, a beta error of 20%, the estimated variance, and a minimal relevant difference (MIRD). Similar to published Cochrane Reviews, we considered the MIRD to be 1 cm for pain on a visual analog scale (VAS), 1 day for hospital stay, and 15 min for operative time (12, 13).
Results Study selection, methodological quality, and results of SRsIn total, 16 relevant Cochrane and non-Cochrane SRs and a protocol of the network meta-analysis of RCTs that address laparoscopic repair of PPUs were identified and critically appraised (Figure 1, Tables 1, 2) (1, 14–29).
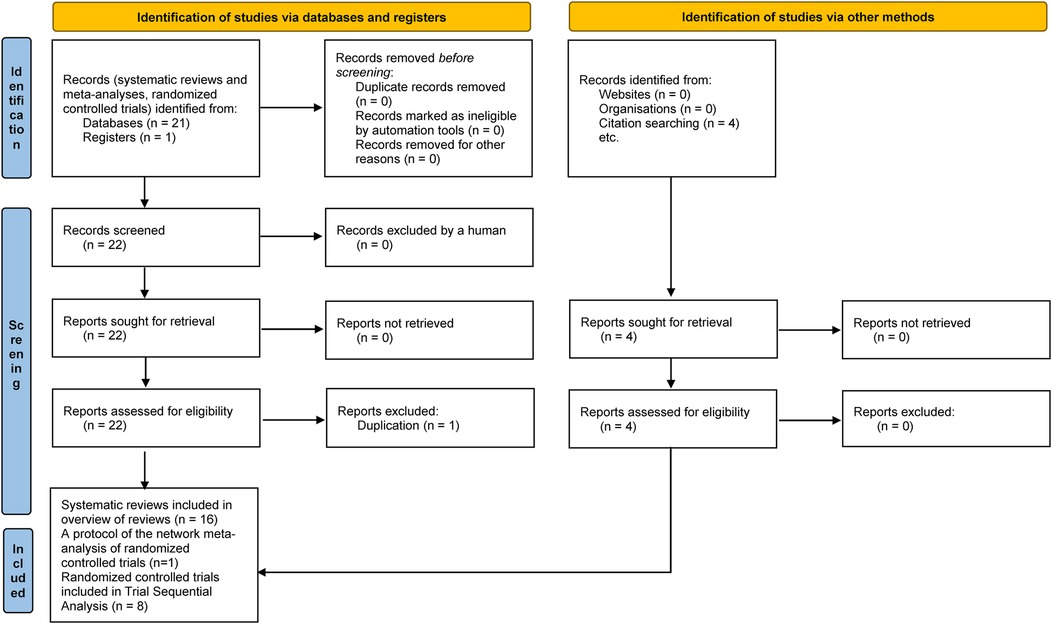
Figure 1. Stages of the comprehensive systematic review search.
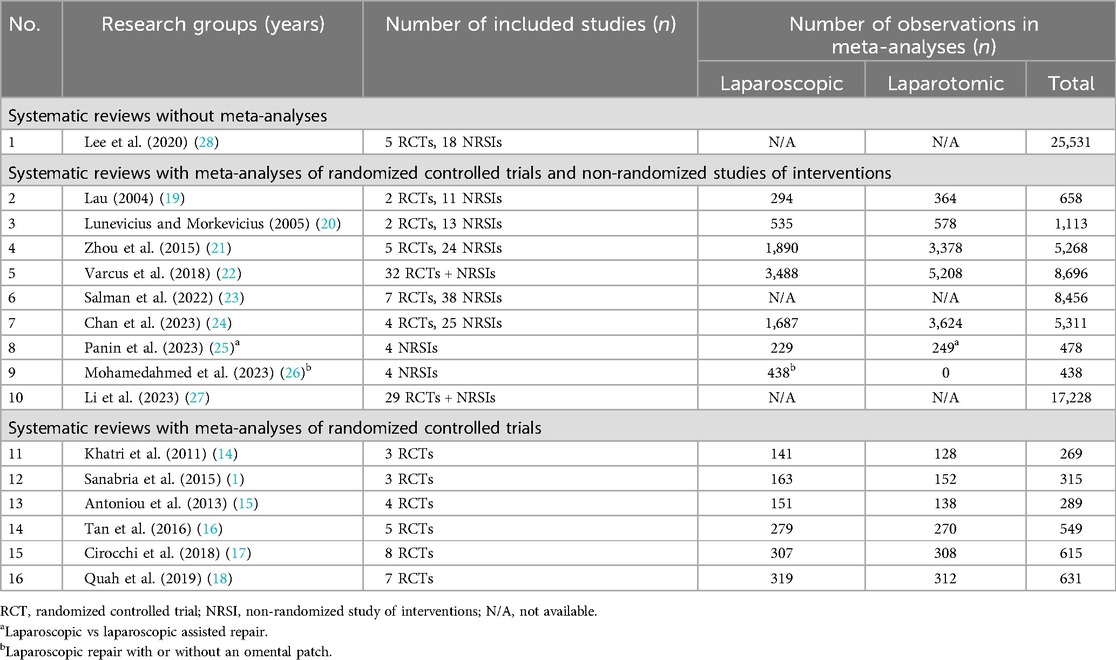
Table 1. Systematic reviews of laparoscopic repair for perforated peptic ulcer disease.
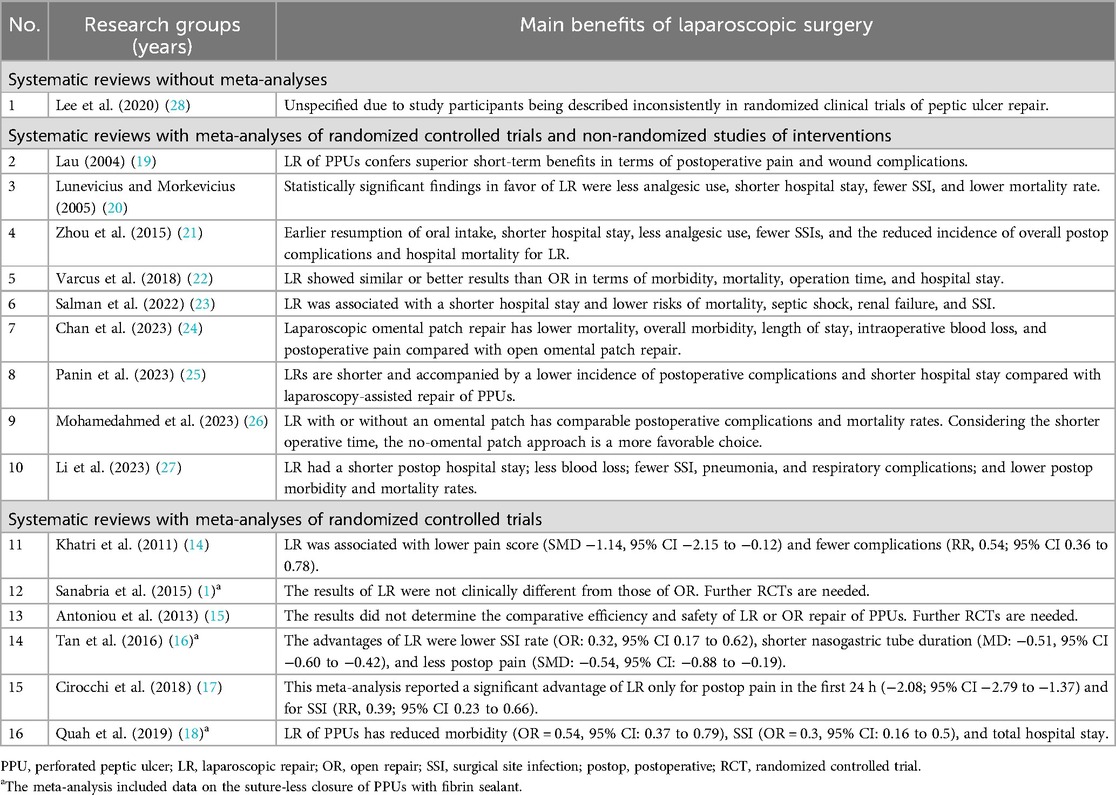
Table 2. Main results of meta-analyses of randomized controlled trials and non-randomized studies of interventions.
The aim of the planned network meta-analysis (29) was to compare surgical (including laparoscopic) and alternative approaches for the treatment of PPUs. The conclusions of the already published SRs were heterogeneous. Mismatches between systematic reviews' results were caused by substantial non-equivalence across included trial populations, different approaches to the application of laparoscopic repair of PPUs, and the various designs of the primary trials.
The main benefits of laparoscopic repair of PPUs according to the SRs that included results of RCTs and non-randomized studies of interventions (NRSIs) and the main conclusions of six meta-analyses that only polled the results of RCTs are presented in Table 2.
We mapped out the primary studies that were included in the systematic reviews of randomized controlled trials (30–38). Khatri et al. did 't specify which RCTs were included in their SR (14). Information about the amount of overlap between SRs is presented in Table 3.
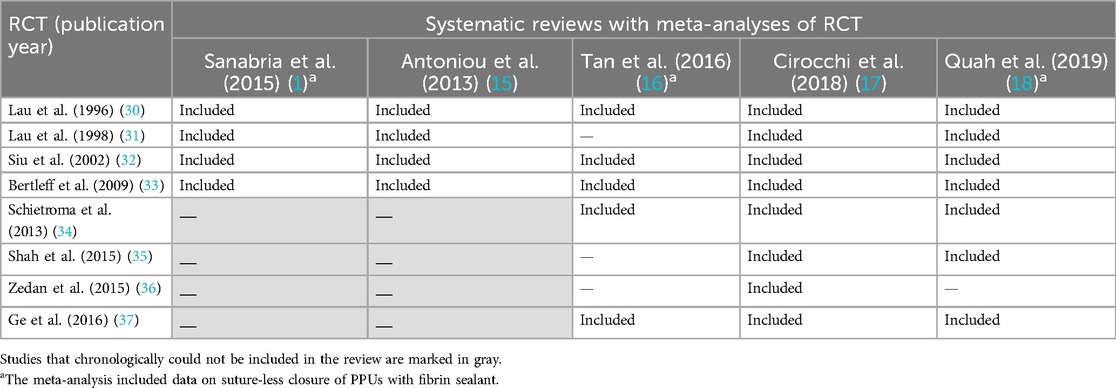
Table 3. The primary studies contained within included systematic reviews of RCT (mapping of overlapping).
Three overlapping reviews of RCTs met the inclusion criteria of the current meta-review and analyzed laparoscopic repair with sutures alone or in combination with an omental patch without fibrin sealant (14, 15, 17). There were no available data regarding the systematic review's methodology in the meta-analysis of Khatri et al. (14). The methodological quality of the systematic reviews of RCTs conducted by Antoniou et al. and Cirocchi et al. are presented in Table 4 according to the critical appraisal tools of the Oxford Centre for Evidence-Based Medicine.
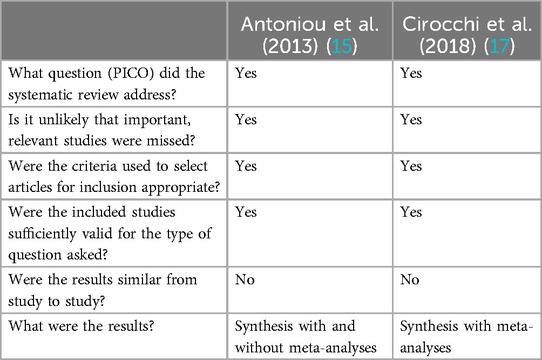
Table 4. Critical appraisal sheet of the relevant systematic reviews.
RCTs contained within the included systematic reviewsSince an additional TSA had been planned, we summarized the information of all the published RCTs included in the relevant SRs which are presented in Table 5.

Table 5. General information about the randomized controlled trials of laparoscopic repair of perforated peptic ulcers.
An evaluation of the domain-specific risk of bias of each RCT included in the relevant SRs was already conducted by the systematic review authors. There was a high risk of performance and detection bias due to a lack of blinding. Blinding was not possible as the RCTs compared open surgery with laparoscopy (1, 16).
Synthesis of resultsAs there were no supplements to the existing primary study evaluations, in the next step of the meta-review, we extracted the outcome data reported in each of the included SRs (Table 6).
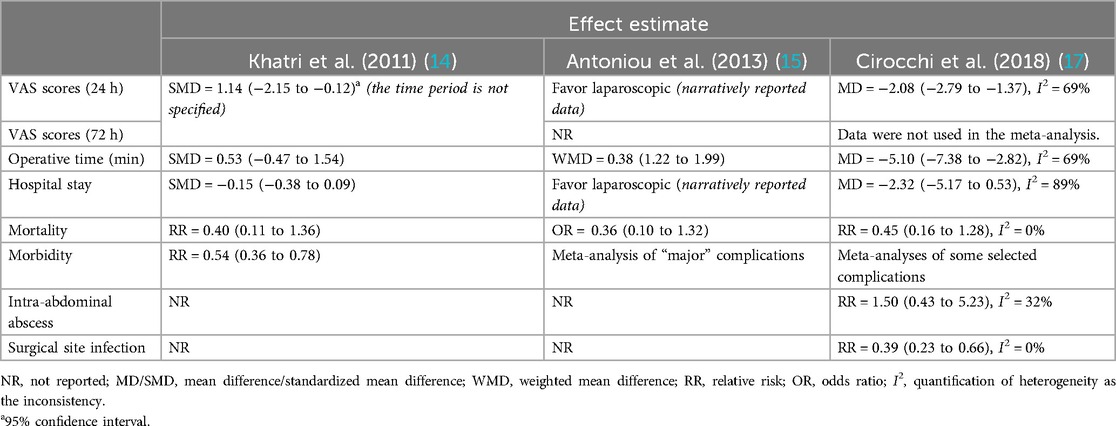
Table 6. Summarized outcome data of systematic reviews.
There was no significant difference between laparoscopic and open repair in terms of mortality. However, the results of all meta-analyses favor laparoscopic surgery with regard to less postoperative pain and enhanced recovery (14, 15, 17). One meta-analysis also noted a reduction in the incidence of postoperative wound complications (17).
Trial sequential analysisThe reanalysis of the meta-analytic findings and adjustments of sample size by the TSA confirmed that laparoscopic repair was associated with less postoperative pain. The inferences about statistical significance were confirmed by the strength of the evidence (Table 7, Supplementary Figures S2А,B) and future trials are unlikely to change them.
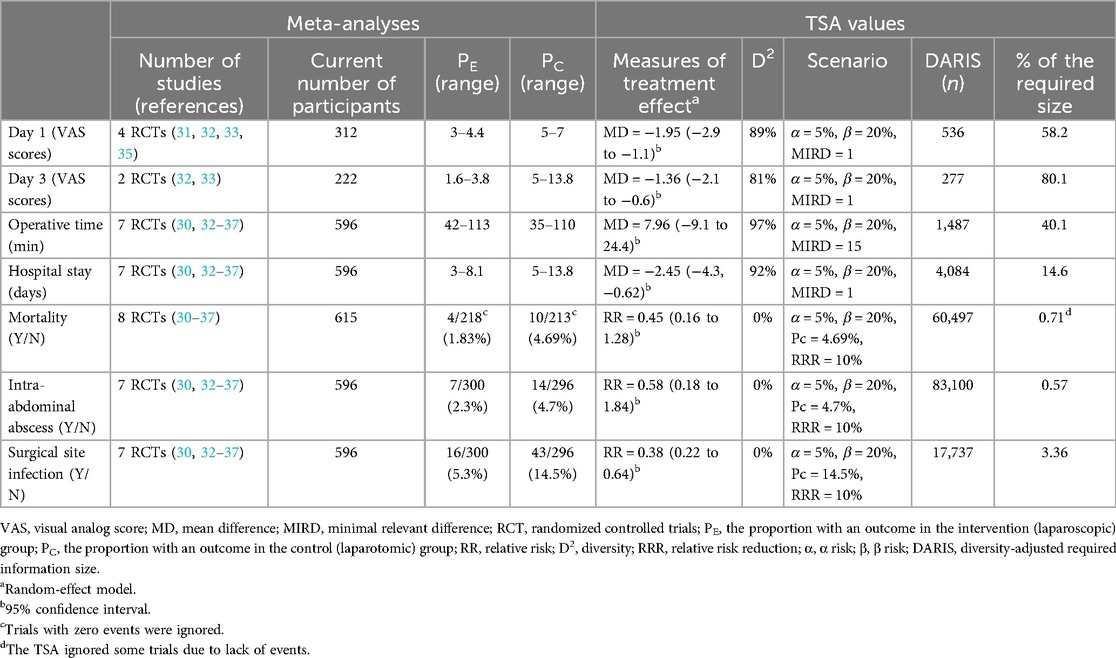
Table 7. Reanalysis of meta-analytic findings with additional values from the trial sequential analysis.
The calculated DARIS for operative time and hospital stay were 40.1% and 14.6%, respectively, and the TSA showed neither significant benefit nor harm of laparoscopic surgery in the attained information size in the meta-analysis (Table 7, Supplementary Figures S3A,B).
Further trials with regard to mortality, surgical site infection, and intra-abdominal abscesses are not very promising because the DARIS did not exceed 5% after the combined results of all the available RCTs. Thus, the main significant results include a reduction in both pain on postoperative day 1 and the duration of the procedure (Table 7, Supplementary Figures 4A–C).
DiscussionA perforated peptic ulcer is a common surgical condition. The results of treatment of certain groups of patients, e.g., comorbid patients, remain unsatisfactory. This is despite obvious advances in surgical and anesthetic techniques and intensive care approaches. One direction for improving treatment outcomes appears to be the introduction of evidence-based techniques and practices (1). Clinical guideline recommendations are based on the combined results of randomized trials in meta-analyses.
This study found only 16 relevant Cochrane and non-Cochrane SRs that address laparoscopic repair of PPUs (1, 14–29). Their conclusions were heterogeneous due to a substantial non-equivalence across trial populations, different approaches of laparoscopic repair for PPU, and various designs.
Only three reviews of overlapping RCTs met the inclusion criteria of the meta-review and analyzed laparoscopic repair with sutures alone or in combination with an omental patch (14, 15, 17). Despite the popular opinion of experts about the advantages of laparoscopy, no differences were reported in most of the clinical outcomes. The only access-related significant difference was in lower postoperative pain scores after laparoscopic repair on day 2 (according to data from two RCTs). This also was the only parameter that achieved 82% of the DARIS. Hence, subsequent studies are unlikely to change this conclusion.
For the other evaluation criteria, the DARIS scores ranged from 0.57% (intra-abdominal abscess) to 58.2% (pain on postoperative day 1). The calculated DARIS for operative time and hospital stay were 40.1% and 14.6%, respectively, and the TSA showed neither significant benefit nor harm of laparoscopic surgery in the attained information size in the meta-analysis. Further trials with regard to mortality, surgical site infection, and intra-abdominal abscesses are not very promising because the DARIS did not exceed 5% after combining the results of eight RCTs.
To our knowledge, this is the first study of laparoscopic suture repair of perforated peptic ulcer disease that summarizes evidence from systematic reviews in the format of meta-review with trial sequential analysis.
There remains a lack of high-quality evidence-based research. Over the past three decades, only eight RCTs have been conducted worldwide (1, 17). At the same time, it must be stated that the DARIS will not be achieved in the foreseeable future in terms of the main indicator of treatment effectiveness—mortality rate.
Future research should explore metadata on issues where a TSA is available and the DARIS is achievable. It seems important to focus on the efficacy and safety of minimally invasive PPU treatment technologies in subgroups of patients with comorbidity or immunosuppression, in the elderly, etc.
ConclusionSummarization of evidence from systematic reviews and reanalysis using TSA confirmed sufficient evidence for one postoperative outcome. Laparoscopic suture repair of PPUs is accompanied by lower pain scores at 24–72 h compared with open repair, improving postoperative recovery. On the issue of postoperative complications and mortality, achieving a DARIS through additional studies seems unpromising.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributionsSP: Data curation, Methodology, Supervision, Writing – original draft, Writing – review & editing. TN: Data curation, Methodology, Supervision, Writing – original draft, Writing – review & editing. IS: Writing – original draft. KM-M: Writing – original draft. AS: Writing – review & editing. AP: Writing – original draft. AA: Writing – original draft. AB: Writing – original draft.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2025.1496192/full#supplementary-material
References1. Sanabria A, Villegas MI, Morales Uribe CH. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev. (2015) 2015(Issue 2):CD004778. doi: 10.1002/14651858.CD004778.pub3
Crossref Full Text | Google Scholar
2. Costa G, Fransvea P, Lepre L, Liotta G, Mazzoni G, Biloslavo A, et al. Perforated peptic ulcer (PPU) treatment: an Italian nationwide propensity score-matched cohort study investigating laparoscopic vs open approach. Surg Endosc. (2023) 37(7):5137–49. doi: 10.1007/s00464-023-09998-5
PubMed Abstract | Crossref Full Text | Google Scholar
3. Revishvili A, Olovyanny VE, Sazhin VP, Markov PV, Gogia B, Gorin DS, et al. Surgical care in the Russian Federation. Information and analytical collection for 2022. M. 2023; 186 (in Russian).
4. Dadfar A, Edna TH. Epidemiology of perforating peptic ulcer: a population-based retrospective study over 40 years. World J Gastroenterol. (2020) 26(35):5302–13. doi: 10.3748/wjg.v26.i35.5302
PubMed Abstract | Crossref Full Text | Google Scholar
5. Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. “Chapter V: overviews of reviews.” In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 6.4 (updated August 2023). Cochrane (2023). Available online at: www.training.cochrane.org/handbook (Accessed May 14, 2024).
6. López-López JA, Rubio-Aparicio M, Sánchez-Meca J. Overviews of reviews: concept and development. Psicothema. (2022) 2(2):175–81. doi: 10.7334/psicothema2021.586
Crossref Full Text | Google Scholar
7. Lee E, Dobbins M, DeCorby K, McRae L, Tirilis D, Husson H. An optimal search filter for retrieving systematic reviews and meta-analyses. BMC Med Res Methodol. (2012) 12:51. doi: 10.1186/1471-2288-12-51
PubMed Abstract | Crossref Full Text | Google Scholar
9. Thorlund K, Engstrøm J, Wetterslev J, Brok J, Imberger G, Gluud C. User Manual for Trial Sequential Analysis (TSA) [pdf]. 2nd ed. Copenhagen: Copenhagen Trial Unit (2017). p. 1–119. Downloadable from ctu.dk/tsa
10. Kwon D, Reis IM. Simulation-based estimation of mean and standard deviation for meta-analysis via Approximate Bayesian Computation (ABC). BMC Med Res Methodol. (2015) 15:61. doi: 10.1186/s12874-015-0055-5
PubMed Abstract | Crossref Full Text | Google Scholar
12. Vaughan J, Gurusamy KS, Davidson BR. Day-surgery versus overnight stay surgery for laparoscopic cholecystectomy. Cochrane Database Syst Rev. (2013) 2013(Issue 7):CD006798. doi: 10.1002/14651858.CD006798.pub4
PubMed Abstract | Crossref Full Text | Google Scholar
13. Gurusamy KS, Davidson C, Gluud C, Davidson BR. Early versus delayed laparoscopic cholecystectomy for people with acute cholecystitis. Cochrane Database Syst Rev. (2013) (Issue 6):CD005440. doi: 10.1002/14651858.CD005440.pub3
PubMed Abstract | Crossref Full Text | Google Scholar
14. Khatri KM, Sajid S, Baig K, Sayegh M, Singh K. Laparoscopic versus open perforated peptic ulcer suture repair: an updated meta-analysis. Surg Endosc. (2011) 25:S54–S148. doi: 10.1007/s00464-011-1603-7
Crossref Full Text | Google Scholar
15. Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Meta-analysis of laparoscopic versus open repair of perforated peptic ulcer. JSLS. (2013) 17(1):15–22. doi: 10.4293/108680812X13517013317752
PubMed Abstract | Crossref Full Text | Google Scholar
16. Tan S, Wu G, Zhuang Q, Xi Q, Meng Q, Jiang Y, et al. Laparoscopic versus open repair for perforated peptic ulcer: a meta analysis of randomized controlled trials. Int J Surg. (2016) 33(Pt A):124–32. doi: 10.1016/j.ijsu.2016.07.077
PubMed Abstract | Crossref Full Text | Google Scholar
17. Cirocchi R, Soreide K, Di Saverio S, Rossi E, Arezzo A, Zago M, et al. Meta-analysis of perioperative outcomes of acute laparoscopic versus open repair of perforated gastroduodenal ulcers. J Trauma Acute Care Surg. (2018) 85(2):417–25. doi: 10.1097/TA.0000000000001925
PubMed Abstract | Crossref Full Text | Google Scholar
18. Quah GS, Eslick GD, Cox MR. Laparoscopic repair for perforated peptic ulcer disease has better outcomes than open repair. J Gastrointest Surg. (2019) 23(3):618–25. doi: 10.1007/s11605-018-4047-8
PubMed Abstract | Crossref Full Text | Google Scholar
21. Zhou C, Wang W, Wang J, Zhang X, Zhang Q, Li B, et al. An updated meta-analysis of laparoscopic versus open repair for perforated peptic ulcer. Sci Rep. (2015) 5:13976. doi: 10.1038/srep13976
PubMed Abstract | Crossref Full Text | Google Scholar
22. Varcus F, Paun I, Duta C, Dobrescu A, Frandes M, Tarta C. Laparoscopic repair of perforated peptic ulcer. Minerva Chir. (2018) 73(2):188–93. doi: 10.23736/S0026-4733.18.07603-4
PubMed Abstract | Crossref Full Text | Google Scholar
23. Salman MA, Issa M, Salman A, Tourky M, Elewa A, Alrahawy M, et al. Surgical management of perforated peptic ulcer: a comparative meta-analysis of laparoscopic versus open surgery. Surg Laparosc Endosc Percutan Tech. (2022) 32(5):586–94. doi: 10.1097/SLE.0000000000001086
PubMed Abstract | Crossref Full Text | Google Scholar
24. Chan KS, Ng STC, Tan CHB, Gerard G, Oo AM. A systematic review and meta-analysis comparing postoperative outcomes of laparoscopic versus open omental patch repair of perforated peptic ulcer. J Trauma Acute Care Surg. (2023) 94(1):e1–13. doi: 10.1097/TA.0000000000003799
PubMed Abstract | Crossref Full Text | Google Scholar
25. Panin SI, Beburishvili AG, Fedorov AV, Sazhin IV, Mikhin IV, Nishnevich EV, et al. Laparoscopic versus laparoscopy-assisted suturing of perforated peptic ulcers (meta-analysis). Khirurgiia. (2023) 2:72–8. (In Russ.). doi: 10.17116/hirurgia202302172
Crossref Full Text | Google Scholar
26. Mohamedahmed AYY, Albendary M, Patel K, Ayeni AA, Zaman S, Zaman O, et al. Comparison of omental patch closure versus simple closure for laparoscopic repair of perforated peptic ulcer: a systematic review and meta-analysis. Am Surg. (2023) 89(5):2005–13. doi: 10.1177/00031348211067991
PubMed Abstract | Crossref Full Text | Google Scholar
27. Li ZW, Tong Y, Liu F, Liu XR, Lv Q, Tang KL, et al. A comparative study on laparoscopic and open surgical approaches for perforated peptic ulcer repair: efficacy and outcomes analysis. Langenbecks Arch Surg. (2023) 408(1):435. doi: 10.1007/s00423-023-03171-1
PubMed Abstract | Crossref Full Text | Google Scholar
28. Lee MJ, Coe PO, O'Donoghue R, Peirson M, Saha A. Variation in descriptors of patient characteristics in randomized clinical trials of peptic ulcer repair: a systematic review. Br J Surg. (2020) 107(12):1570–9. doi: 10.1002/bjs.11771
PubMed Abstract | Crossref Full Text | Google Scholar
29. Wadewitz E, Friedrichs J, Grilli M, Vey J, Zimmermann S, Kleeff J, et al. Approaches for the treatment of perforated peptic ulcers: a network meta-analysis of randomised controlled trials—study protocol. BMJ Open. (2024) 14(3):e082732. doi: 10.1136/bmjopen-2023-082732
PubMed Abstract | Crossref Full Text | Google Scholar
30. Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, Dawson JJW, et al. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. (1996) 224:131–8. doi: 10.1097/00000658-199608000-00004
PubMed Abstract | Crossref Full Text | Google Scholar
31. Lau JY, Lo SY, Ng EK, Lee DW, Lam YH, Chung SC. A randomized comparison of acute phase response and endotoxemia in patients with perforated peptic ulcers receiving laparoscopic or open patch repair. Am J Surg. (1998) 175:325–7. doi: 10.1016/s0002-9610(98)00006-3
PubMed Abstract | Crossref Full Text | Google Scholar
32. Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, et al. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. (2002) 235(3):313–9. doi: 10.1097/00000658-200203000-00001
PubMed Abstract | Crossref Full Text | Google Scholar
33. Bertleff MJ, Halm JA, Bemelman WA, van der Ham AC, van der Harst E, Oei HI, et al. Randomized clinical trial of laparoscopic versus open repair of the perforated peptic ulcer: the LAMATrial. World J Surg. (2009) 33(7):1368–73. doi: 10.1007/s00268-009-0054-y
PubMed Abstract | Crossref Full Text | Google Scholar
34. Schietroma M, Piccione F, Carlei F, Sista F, Cecilia EM, Amicucci G. Peritonitis from perforated peptic ulcer and immune response. J Invest Surg. (2013) 26(5):294–304. doi: 10.3109/08941939.2012.762073
PubMed Abstract | Crossref Full Text | Google Scholar
35. Shah FH, Mehta SG, Gandhi MD, Saraj . Laparoscopic peptic ulcer perforation closure: the preferred choice. Indian J Surg. (2015) 77(Suppl 2):403–6. doi: 10.1007/s12262-013-0853-0
PubMed Abstract | Crossref Full Text | Google Scholar
36. Zedan AS, Lolah MA, Badr ML, Ammar MS. Laparoscopic versus open repair of perforated duodenal peptic ulcer: a randomized controlled trial. Menoufia Med J. (2015) 28(Issue 1):11. doi: 10.4103/1110-2098.155945
Crossref Full Text | Google Scholar
37. Ge B, Wu M, Chen Q, Chen Q, Lin R, Liu L, et al. A prospective randomized controlled trial of laparoscopic repair versus open repair for perforated peptic ulcers. Surgery. (2016) 159(2):451–8. doi: 10.1016/j.surg.2015.07.021
PubMed Abstract | Crossref Full Text | Google Scholar
38. Wang Q, Ge B, Huang Q. A prospective randomized controlled trial of laparoscopic repair versus open repair for perforated peptic ulcers. Zhonghua Wei Chang Wai Ke Za Zhi. (2017) 20(3):300–3. Chinese.28338164
留言 (0)