In recent studies, there is limited evidence regarding postoperative analgesia in pediatric patients. Children are unable to express pain, resulting in a relative lack of postoperative pain treatment in children (1). Better postoperative analgesia can accelerate the recovery of children, alleviate their pain, shorten hospital stays, and improve parental satisfaction (2). Regional blockade is a crucial approach in the multimodal analgesia regimen for pediatric perioperative care, and caudal block (CB) has been extensively utilized for postoperative analgesia in pediatric patients (3). The widespread application of ultrasound-guided technology helps to accurately locate sacrococcygeal block, especially when children have sacral abnormalities and other issues (4). Meanwhile, some studies have shown that the use of CB can promote early postoperative mobility and hemodynamic stability in children (5). However, its application is gradually limited due to its short duration of analgesia and weakness such as urinary retention (6).
Currently, the quadratus lumborum block (QLB) has garnered increasing interest among both adults and children (7–10). There are four different types of QLB, including external QLB, posterior QLB, anterior QLB, and intramuscular QLB (11), which are in line with the relative position of the needle tip and the quadratus lumborum. The main mechanism of action of QLB (12–14) is that the lateral arcuate ligament not only serves as a connection between the thoracic fascia and transverse fascia but also provides a pathway for local anesthetics in QLB to spread to the thoracic paravertebral space, thereby alleviating somatic and visceral pain.
The present meta-analysis aimed to compare the postoperative analgesic effects of the QLB with those of traditional CB, including the postoperative rescue analgesic rate during 24 spread to the thoracic paravertebral space, thereby alleviatirates of postoperative complications, in order to identify the advantages and disadvantages of the two analgesic methods.
Materials and methods Study objectivesThe overall objective of this study is to compare the analgesic effects of QLB vs. CB in children undergoing abdominal surgery. The primary outcome is the postoperative rescue analgesia rate, defined as the proportion of patients requiring additional analgesics such as acetaminophen or ibuprofen when their pain score exceeds the predefined threshold within 24 h after surgery. Secondary outcomes include resting pain scores (on a 0–10 scale) at 30 min, 4 h, 12 h, and 24 h post-operatively, the time to first rescue analgesia, the incidence of postoperative nausea and vomiting (PONV), and postoperative complications (such as post-block infection, local anesthetic allergy, hematoma, nerve injury, and local anesthetic toxicity). This systematic review was registered under PROSPERO, ID CRD 42023441447.
Search strategyThe primary literature search was performed in July 2023, and the PubMed, Cochrane Library, Web of Science, and Embase databases were searched from inception until July 2023. To ensure that no newly published article was dropped, the secondary literature search was conducted in August 2023. During the initial literature search, we searched the terms edQL OR quadratus lumborum OR QL block OR QLB OR quadratus lumborum block)” AND “(CB OR caudal block OR caudal epidural blocks OR caudal analgesia OR caudal blockade OR caudal anesthesia OR caudal regional anesthesia OR caudal extradural anesthesia)” AND “(pediatric OR children OR infant OR adolescent OR schoolchild OR preschool OR teens OR youth)”. The secondary literature search was carried out the same as the primary literature search to find new articles.
Study selection criteriaThis meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (6). The inclusion criteria were as follows: (1) Comparing the effects of analgesia between the QLB and CB for pediatric patients undergoing abdominal surgery; (2) Consideration of the rate of postoperative rescue analgesia as the outcome; (3) Randomized controlled trials (RCTs). The exclusion criteria were as follows: (1) Receiving additional treatment in the control or experimental groups; (2) Duplicate publication; (3) An indeterminate type of study or non-RCTs; (4) Failure to extract valid data; (5) Unavailability of the full text of study; (6) Conference abstracts; (7) Reviews or systematic reviews.
Two independent reviewers reviewed and identified studies based on the previously mentioned strategy. Any discrepancies were resolved by discussing them with a third reviewer.
Data extractionThe data extraction was performed by two researchers. Some studies used graphs to show the outcomes in lieu of data, thus, it was attempted to contact corresponding authors to obtain original data. Nevertheless, if no reply was received from the corresponding authors for the original data, GetData tool was used to extract values for each data point.
The following data were extracted: first author's name, country, date of publication, study design, the sample size of experimental and control groups, participants' characteristics, surgical procedures, analgesic methods (medication type, dose, tube placement, duration), time of follow-up, the rescue analgesia, pain scores [time of evaluation, mean, and standard deviation (SD)], the incidence rates of postoperative complications or by-affects (e.g., PONV). For the quantitative analysis, the numeric rating scale (NRS) or the visual analogue scale (VAS) scores were calculated in the range of 0–10 points (0 = no pain, 10 = extreme pain). Pain scores reported as face, legs, activity, cry, consolability (FLACC), or Children's Hospital of Eastern Ontario pain scale (CHEOPS) were transformed to a scale ranging from 0 to 10 points.
Statistical analysisWe conducted meta-analysis for all outcomes. The data was analyzed using Review Manager V5.3. (Cochrane Collaboration, Copenhagen). A weighted average difference or standard average difference was used to analyze the continuous data, and 95% confidence intervals (CIs) were used to combine different scales. Data were presented as mean, and SD values were extracted directly. Data were presented as median using the following formula: (a + m + b)/3, where a = Q25 and b = Q75 to convert median to mean, and data were presented as interquartile range (IQR) using the following formula: SD = IQR/1.349 to convert IQR to SD. Data were presented as CI using the following formula: 95% CI = x ± 1.96*SE, where SD = SE* √n to convert CI to SD. The above-mentioned statistical formulas were previously described by Hozo et al. (15). We used I2 statistics to quantify heterogeneity. If I2 ≤ 50%, we chose a fixed effects model; if I2 > 50%, we chose a random effects model.
Results Description of included studiesA total of 41 trials were identified in the primary literature search, and there were 21 of the records after duplicates were removed. Based on the inclusion and exclusion criteria, 9 trials were excluded, and 12 trials were further screened, of which 5 trials were removed (Figure 1) (13, 16–21). Characteristics of the included studies are listed in Table 1. A summary of findings is reported in Table 2. The risk of bias (RoB) assessment is reported in Figures 2, 3, with the randomization process and selection of reported results being the most common sources of potential bias.

Figure 1. Search flow chart.
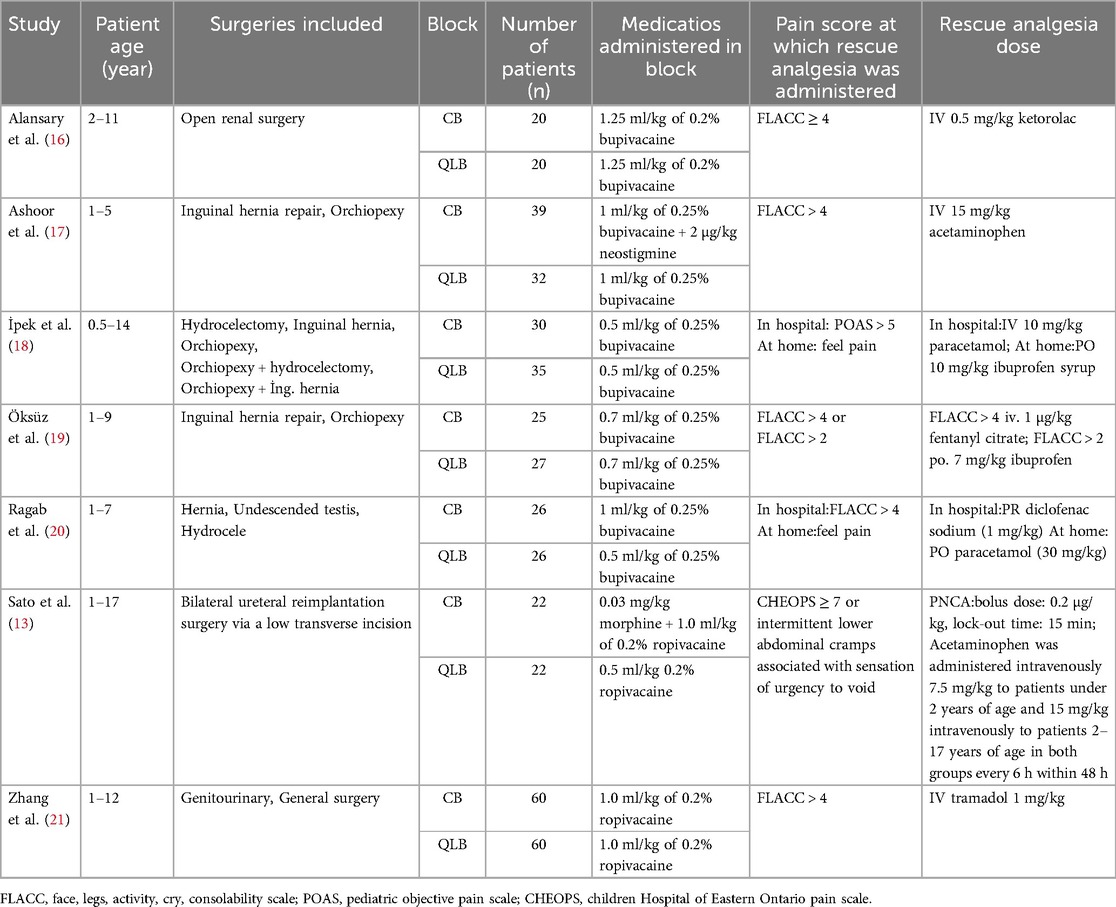
Table 1. Characteristics of included studies.
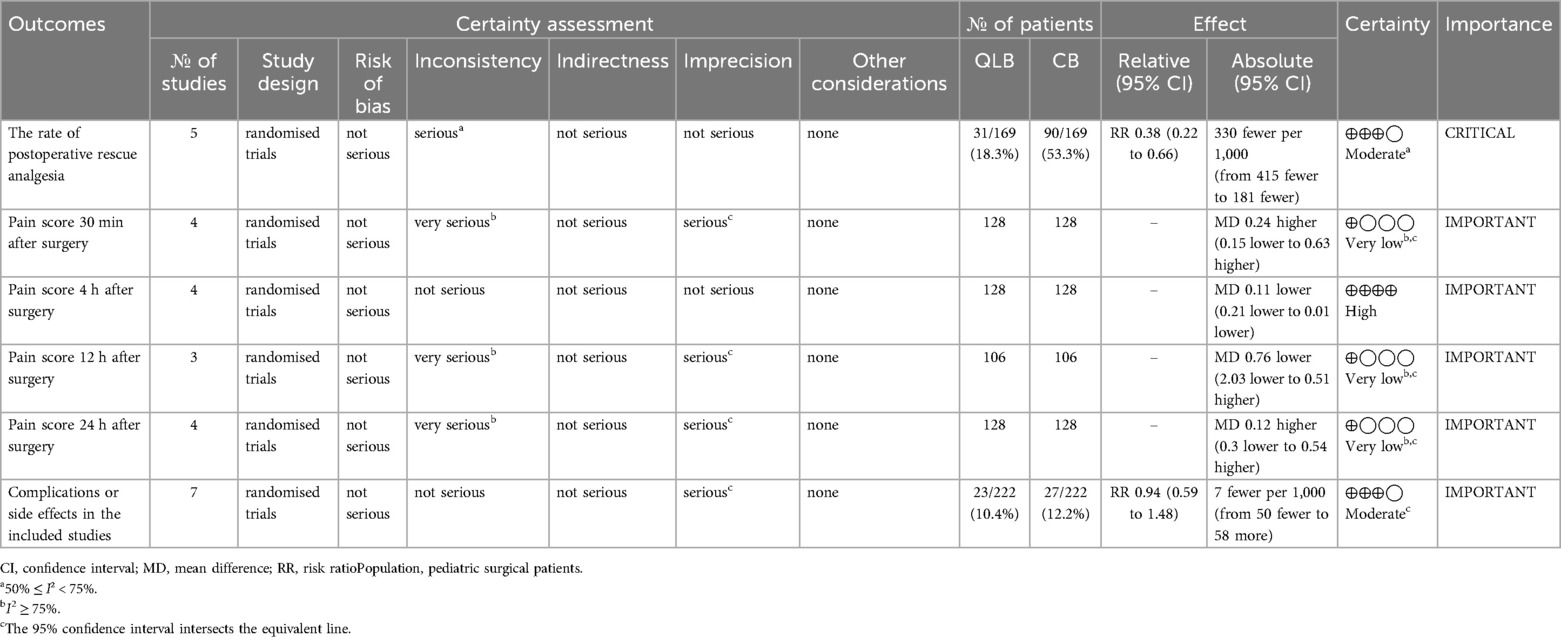
Table 2. Summary of findings.

Figure 2. The risk of bias graph for included randomized controlled trials.
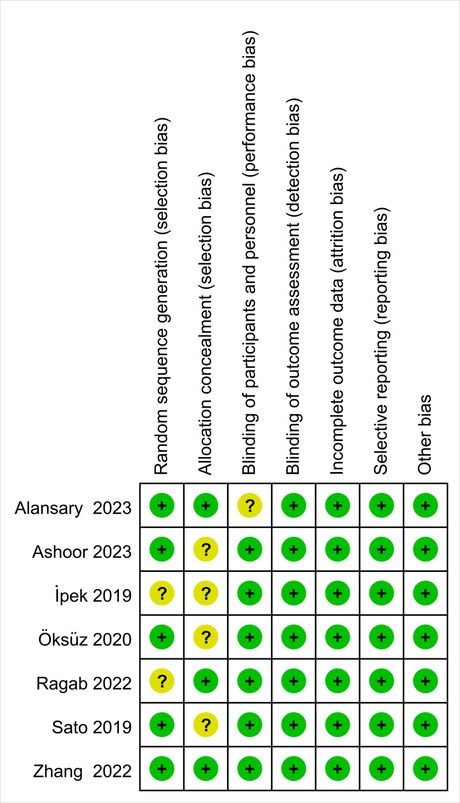
Figure 3. The risk of bias summary for included randomized controlled trials.
The rate of postoperative rescue analgesiaSix trials (13, 16–19, 21) that enrolled 392 patients reported the rate of postoperative rescue analgesia. Compared with caudal analgesia, QLB showed a significant reduction in the rate of postoperative rescue analgesia. [relative risk (RR) = 0.37; 95% CI = 0.26 to 0.51; P < 0.01; [I2 = 50%, P = 0.07], Figure 4]. Among these trials, only five of them (13, 16, 17, 19, 21) utilized posterior QLB, whereas the trial by İpek et al. (18) employed lateral QLB. In order to exclude the influence of different QLB approaches on the results, subgroup analysis was conducted, and the final result was similar. [RR = 0.33; 95% CI = 0.23 to 0.47; P < 0.01; (I2 = 49%, P = 0.10), Figure 4].
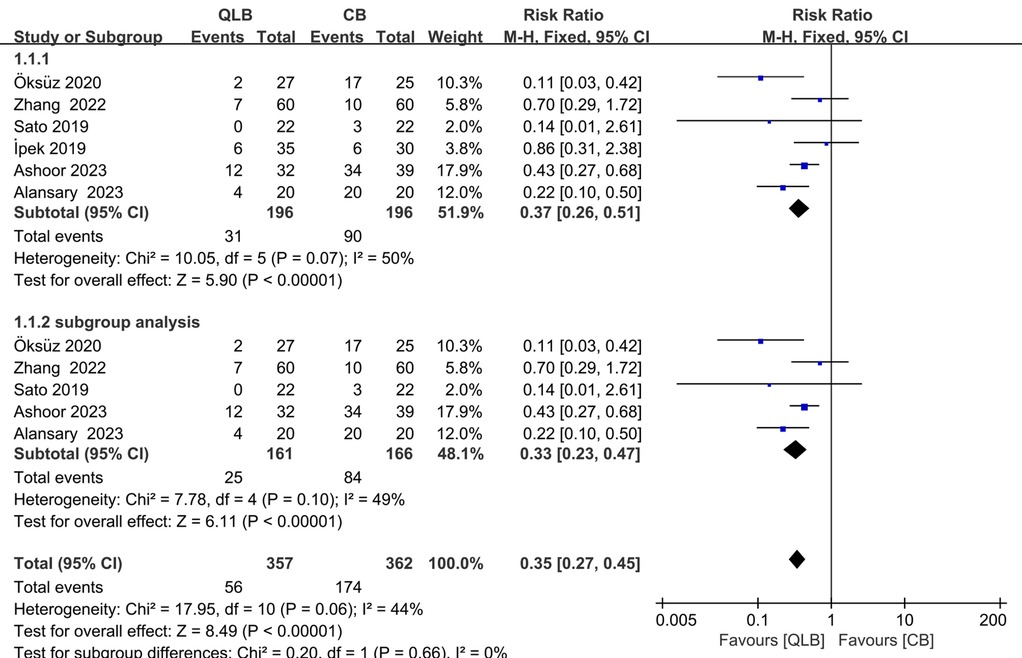
Figure 4. Forest plots of primary outcome of the rate of postoperative rescue analgesia.
Postoperative pain scoresThe postoperative pain scores at 0.5, 4, 12, and 24 h were investigated, and all studies reported pain scores at 0.5, 4, and 24 h. However, only 3 studies reported pain scores at 12 h (16, 20, 21), except for the trial conducted by Stato. M et al. (13) However, data from only four studies (13, 16, 20, 21) were analyzed in the forest plot. Because data conducted by Ashoor et al. (17) and Ipek et al. (18) were presented as graphs rather than specific values, and no original data could be obtained. In addition, the pain scores in the study conducted by Öksüz et al. (19) were reported in the form of a median, which could not be converted to the form of mean and standard deviation due to the skewed distribution of the data.
Pain score 30 min after surgeryAt 30 min after surgery, there was no significant difference in pain scores between the two methods (SMD = 0.24; 95% CI = −0.15 to 0.63; P = 0.22; Figure 5), and this result was influenced by real heterogeneity (I2 = 75%, P = 0.007).
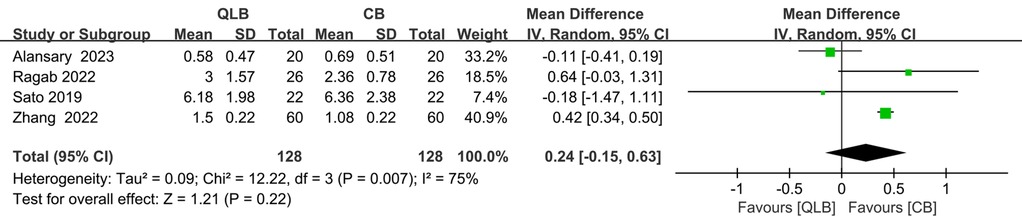
Figure 5. Forest plot of pain score 30 min after surgery.
Pain score 4 h after surgeryAt 4 h after surgery, the pain score of the QLB group was lower than that of the CB group, and the results were statistically significant [SMD = −0.11; 95% CI = −0.21 to −0.01; P = 0.02, (I2 = 0%, P = 0.41); Figure 6].

Figure 6. Forest plot of pain score 4 h after surgery.
Pain score 12 h after surgeryAt 12 h after surgery, there was no significant difference in pain scores between the two methods (SMD = −0.76; 95% CI = −2.03 to 0.51; P = 0.24; Figure 7), and this result was influenced by real heterogeneity (I2 = 98%, P < 0.01).
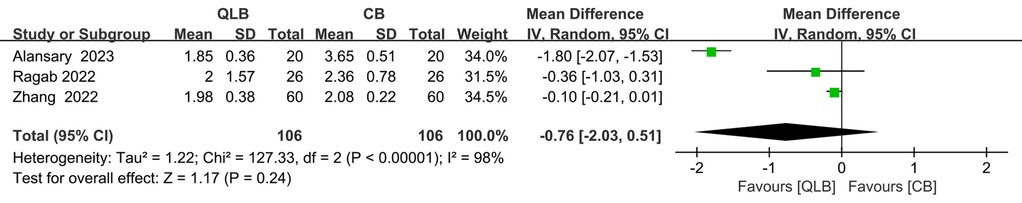
Figure 7. Forest plot of pain score 12 h after surgery.
Pain score 24 h after surgeryAt 24 h after surgery, there was no significant difference in pain scores between the two methods (SMD = 0.12; 95% CI = −0.30 to 0.54; P = 0.57; Figure 8), and this result was influenced by real heterogeneity (I2 = 87%, P < 0.01).
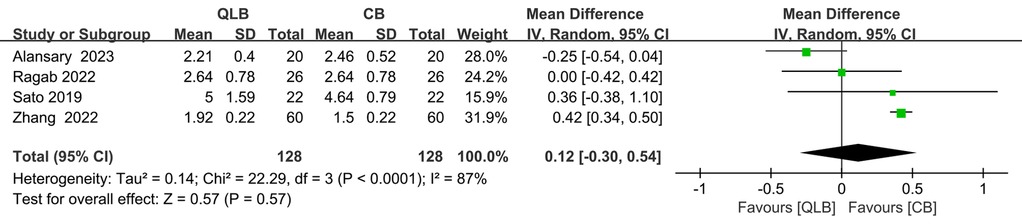
Figure 8. Forest plot of pain score 24 h after surgery.
Complications or side effects in the included studiesAll of the trials (13, 16–21) investigated the incidence of postoperative complications or by-effects, such as nausea, vomiting, hypotension, bradycardia, and urinary retention. Gözen Öksüz et al. (19) reported one case of nausea in the CB group. Celal Bulut İPEK et al. (18) identified 3 cases of postoperative urinary retention in the CB group. Tarek M. Ashoor et al. (17) detected 5 cases of urine retention, 3 cases of nausea and vomiting, 3 cases of hematoma, 2 cases of hypotension, and one case of bradycardia in the QLB group, while 9 cases of nausea and vomiting, 3 cases of urine retention, and one case of hypotension in the CB group. Yue Zhang et al. (21) reported 3 cases of nausea or vomiting in the CB group and 2 cases in the QLB group. Amin M. Alansary et al. (16) reported 7 cases of PONV in the CB group and 6 cases in the trans-incisional QLB (TiQLB) group. Makoto Sato et al. (13) and Safaa Gaber Ragab et al. (20) reported no complications. No significant difference was found between QLB and CB in the complications or side effects (RR = 0.94; 95% CI = 0.59 to 1.48; P = 0.77). In addition, there was no significant heterogeneity among the trials (I2 = 0%, P = 0.56; Figure 9).
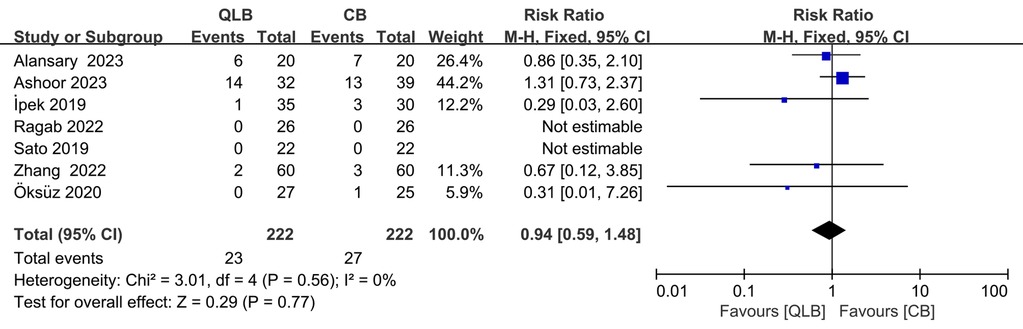
Figure 9. Forest plot of complications or side effects in the included studies.
DiscussionTo our knowledge, this was the first systematic review and meta-analysis to evaluate the postoperative analgesic effects of QLB and CB in pediatric abdominal surgeries. These results showed that compared with CB, QLB reduced the postoperative rescue analgesia rate by 0.37 during postoperative 24 h. Additionally, pain scores in the QLB group were lower than those in the CB group at 0.5 h and 24 h after surgery, and the results were statistically significant. However, it does not meet the criteria of a minimally clinically important difference, which is generally thought to be at least 1 point on the 11-point NRS (22). There were no significant differences in postoperative complications or side effects between the two groups.
Our meta-analysis further supports a previous meta-analysis (23) including CB which suggests QLB is an effective postoperative analgesia technique for pediatric patients undergoing lower abdominal surgery. In a network meta-analysis (24), the author compared the RCTs included in the study in pairs and ultimately concluded that for pediatric inguinal surgery, the first rescue analgesia time for quadratus lumborum and transversus abdominis plane blocks is the longest, and the need for rescue analgesia is the least, compared with CB, ultrasound-guided II-IHB, and other block methods. In another meta-analysis (25) shows that, when used as analgesia for hypospadias repair, CB exhibited higher pain scores 24 h postoperatively, significantly shorter analgesia duration, and greater analgesia consumption compared with peripheral nerve blocks. The author found limited data suggesting that peripheral nerve block provides better analgesic quality than CB. These conclusions align with our findings.
Clinical implicationsCB is the most frequently utilized regional anesthesia technique among children, particularly suitable for surgical interventions situated beneath the umbilicus (T10 dermatome) (26, 27). This method offers safe access to the epidural space in pediatric patients (28, 29). However, a single CB may have a relatively short duration of analgesia, only around 4 to 6 h, which can often be considered insufficient (30, 31), while placing catheters in the tail area increases the risk of infection and prevents early activity (32). The reason for its short duration is the rich distribution of blood vessels, leading to the rapid absorption of the local anesthetics (33). Furthermore, it comes with potential drawbacks such as the risk of accidental dural puncture, bladder dysfunction, and so on. Due to the above disadvantages, the application of CB is limited.
QLB is not only applicable to pediatric abdominal surgeries but it has also been proven effective in lumbar disc herniation surgeries (34), total hip replacement surgeries (35), as well as adult abdominal surgeries such as laparoscopic cholecystectomy (36) and cesarean section (37). A cadaver study (38) involving the performance of anterior QLB, using a dye, has demonstrated that QLB can induce analgesia from T10 to L4, as evidenced by the colored lumbar nerve roots and occasionally some nerves in the TAP. Additionally, other studies have indicated that anterior QLB may extend cephalad beyond previous levels, reaching T7–T12 spinal nerve roots, which could be the reason for the effectiveness of QLB (7). In adults, the mean effective duration of sensory block was 14.1 h after unilateral anterior QLB at the L4 level with 20 ml of 0.375% ropivacaine (39). Previous research (40) reported that QLB had safety features with minimal complications and/or side effects and demonstrated that QLB was the most effective technique for providing postoperative analgesia in pediatric patients undergoing lower abdominal surgery. Compared with the conventional CB or opioid analgesics in pediatric patients, QLB had a better analgesic effect and minimal side effects (41), which is consistent with our results. Compared with CB, QLB reduced the rate of rescue analgesia.
In terms of adverse reactions, although we concluded that there was no statistical difference between the QLB group and the CB group, we should pay more attention to block-related complications rather than general postoperative complications, but unfortunately, the RCTS we included did not indicate it.
Implications for further researchThe aggregated data clearly shows that QLB leads to a significantly lower rate of postoperative rescue analgesia compared to CB. As such, it is imperative to delve into the clinical significance of this difference and explore its effects on perioperative care and the overall quality of recovery. The observed trends, such as improved pain scores and a decrease in the number of patients needing additional pain relief, point to crucial research areas. This knowledge has the potential to significantly influence the development, application, and success of enhanced recovery after surgery protocols (42–44).
Strengths and limitationsOur summary analysis is rooted in a well-considered and systematic search process, which involves independent verification and data extraction by two authors. This enables the analysis of seven studies, involving a total of 444 patients. The results derived from this large cohort are significant, as it is challenging to conduct large-scale pediatric trials required to address issues related to recovery characteristics.
However, the included studies and sample sizes were small. Small study effect bias and unpublished bias may exist. Through our results, although the difference is firm between the two groups, more studies are still needed in this area. The results of this study exhibited varying degrees of heterogeneity, prompting us to conduct a sensitivity analysis using the “one-by-one exclusion” method. Our meta-analysis revealed that a significant portion of this heterogeneity could be attributed to the article by Amin M. Alansary et al. (16). This could potentially stem from the unique approach employed in this RCT, where the author administered ultrasound-guided TiQLB to pediatric patients undergoing open renal surgery. The timing of the block, the type of surgery performed, and the specific technique used for the block all differed from those in other studies, contributing to the observed heterogeneity. In addition, in our article, the pain scores at most time points failed to reach statistical significance. This observation can likely be attributed to the comprehensive pain management protocols employed in these trials, which effectively mitigated pain levels among participants.
ConclusionThe present meta-analysis mainly compared the analgesic effects of QLB and traditional CB, as well as side effects, to provide suggestions for selecting appropriate analgesic methods. The meta-analysis demonstrated that QLB was an effective postoperative analgesic method for the child undergoing lower abdominal surgeries and QLB might be used as an alternative to CB for pediatrics. Compared with CB, QLB provides lower pain scores in some periods or reduces the rate of postoperative rescue analgesia compared to CB. However, we identified relatively few RCTs and observed significant heterogeneity, future studies are required to provide more reliable evidence and confirm these results.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statementWritten informed consent was not obtained from individual(s), nor the minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article because all of the analyses were based on previously published studies and retrospective data, the need for ethical approval and informed consent was waived.
Author contributionsYZ: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft. JW: Formal analysis, Investigation, Methodology, Writing – review & editing. SQ: Formal analysis, Investigation, Writing – review & editing. PJ: Methodology, Supervision, Writing – review & editing. CB: Supervision, Writing – review & editing. YL: Conceptualization, Formal analysis, Methodology, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Mekonnen S, Ali Y. Efficacy of caudal neostigmine for postoperative pain relief: a systemic review and meta-analysis. Curr Pediatr Res. (2017) 21:403–9.
2. Boric K, Dosenovic S, Jelicic Kadic A, Batinic M, Cavar M, Urlic M, et al. Interventions for postoperative pain in children: an overview of systematic reviews. Paediatr Anaesth. (2017) 27:893–904. doi: 10.1111/pan.13203
PubMed Abstract | Crossref Full Text | Google Scholar
3. Brenner L, Marhofer P, Kettner SC, Willschke H, Machata AM, Al-Zoraigi U, et al. Ultrasound assessment of cranial spread during caudal blockade in children: the effect of different volumes of local anaesthetics. Br J Anaesth. (2011) 107:229–35. doi: 10.1093/bja/aer128
PubMed Abstract | Crossref Full Text | Google Scholar
4. Lees D, Frawley G, Taghavi K, Mirjalili SA. A review of the surface and internal anatomy of the caudal canal in children. Paediatr Anaesth. (2014) 24:799–805. doi: 10.1111/pan.12392
PubMed Abstract | Crossref Full Text | Google Scholar
5. Wiegele M, Marhofer P, Lönnqvist P-A. Caudal epidural blocks in paediatric patients: a review and practical considerations. Br J Anaesth. (2019) 122:509–17. doi: 10.1016/j.bja.2018.11.030
PubMed Abstract | Crossref Full Text | Google Scholar
6. Sethi N, Pant D, Dutta A, Koul A, Sood J, Chugh PT. Comparison of caudal epidural block and ultrasonography-guided transversus abdominis plane block for pain relief in children undergoing lower abdominal surgery. J Clin Anesth. (2016) 33:322–9. doi: 10.1016/j.jclinane.2016.03.067
PubMed Abstract | Crossref Full Text | Google Scholar
7. Blanco R, Ansari T, Riad W, Shetty N. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. (2016) 41:757–62. doi: 10.1097/AAP.0000000000000495
PubMed Abstract | Crossref Full Text | Google Scholar
8. Dam M, Hansen CK, Børglum J, Chan V, Bendtsen TF. A transverse oblique approach to the transmuscular quadratus lumborum block. Anaesthesia. (2016) 71:603–4. doi: 10.1111/anae.13453
PubMed Abstract | Crossref Full Text | Google Scholar
9. Öksüz G, Bilal B, Gürkan Y, Urfalioğlu A, Arslan M, Gisi G, et al. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg Anesth Pain Med. (2017) 42:674–9. doi: 10.1097/AAP.0000000000000645
PubMed Abstract | Crossref Full Text | Google Scholar
10. Pirrera B, Alagna V, Lucchi A, Berti P, Gabbianelli C, Martorelli G, et al. Transversus abdominis plane (TAP) block versus thoracic epidural analgesia (TEA) in laparoscopic colon surgery in the ERAS program. Surg Endosc. (2018) 32:376–82. doi: 10.1007/s00464-017-5686-7
PubMed Abstract | Crossref Full Text | Google Scholar
11. Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus lumborum block: anatomical concepts, mechanisms, and techniques. Anesthesiology. (2019) 130:322–35. doi: 10.1097/ALN.0000000000002524
PubMed Abstract | Crossref Full Text | Google Scholar
12. Chin KJ, McDonnell JG, Carvalho B, Sharkey A, Pawa A, Gadsden J. Essentials of our current understanding: abdominal wall blocks. Reg Anesth Pain Med. (2017) 42:133–83. doi: 10.1097/AAP.0000000000000545
PubMed Abstract | Crossref Full Text | Google Scholar
13. Sato M. Ultrasound-guided quadratus lumborum block compared to caudal ropivacaine/morphine in children undergoing surgery for vesicoureteric reflex. Paediatr Anaesth. (2019) 29:738–43. doi: 10.1111/pan.13650
PubMed Abstract | Crossref Full Text | Google Scholar
14. Dam M, Hansen CK, Poulsen TD, Azawi NH, Wolmarans M, Chan V, et al. Transmuscular quadratus lumborum block for percutaneous nephrolithotomy reduces opioid consumption and speeds ambulation and discharge from hospital: a single centre randomised controlled trial. Br J Anaesth. (2019) 123:e350–8. doi: 10.1016/j.bja.2019.04.054
PubMed Abstract | Crossref Full Text | Google Scholar
15. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. (2005) 5:13. doi: 10.1186/1471-2288-5-13
PubMed Abstract | Crossref Full Text | Google Scholar
16. Alansary AM, Badawy A, Elbeialy MAK. Ultrasound-guided trans-incisional quadratus lumborum block versus ultrasound-guided caudal analgesia in pediatric open renal surgery: a randomized trial. Korean J Anesthesiol. (2023) 76:471–80. doi: 10.4097/kja.22774
PubMed Abstract | Crossref Full Text | Google Scholar
17. Ashoor TM, Zain EM, Reyad MK, Hasseb AM, Esmat IM. Ultrasound-guided techniques for perioperative analgesia in pediatric lower abdominal surgeries: quadratus lumborum block with bupivacaine versus caudal bupivacaine and neostigmine. Pain Physician. (2023) 26:137–47. doi: 10.36076/ppj.2023.26.137
PubMed Abstract | Crossref Full Text | Google Scholar
18. İpek CB, Kara D, Yılmaz S, Yeşiltaş S, Esen A, Dooply SSSL, et al. Comparison of ultrasound-guided transversus abdominis plane block, quadratus lumborum block, and caudal epidural block for perioperative analgesia in pediatric lower abdominal surgery. Turk J Med Sci. (2019) 49:1395–402. doi: 10.3906/sag-1812-59
PubMed Abstract | Crossref Full Text | Google Scholar
19. Öksüz G, Arslan M, Urfalıoğlu A, Güler AG, Tekşen Ş, Bilal B, et al. Comparison of quadratus lumborum block and caudal block for postoperative analgesia in pediatric patients undergoing inguinal hernia repair and orchiopexy surgeries: a randomized controlled trial. Reg Anesth Pain Med. (2020) 45:187–91. doi: 10.1136/rapm-2019-101027
PubMed Abstract | Crossref Full Text | Google Scholar
20. Ragab SG, El Gohary MM, Abd El Baky DL, Nawwar KMA. Ultrasound-guided quadratus lumborum block versus caudal block for pain relief in children undergoing lower abdominal surgeries: a randomized, double-blind comparative study. Anesth Pain Med. (2022) 12:e126602. doi: 10.5812/aapm-126602
PubMed Abstract | Crossref Full Text | Google Scholar
21. Zhang Y, Wang YP, Wang HT, Xu YC, Lv HM, Yu Y, et al. Ultrasound-guided quadratus lumborum block provided more effective analgesia for children undergoing lower abdominal laparoscopic surgery: a randomized clinical trial. Surg Endosc. (2022) 36:9046–53. doi: 10.1007/s00464-022-09370-z
PubMed Abstract | Crossref Full Text | Google Scholar
22. Myles PS, Myles DB, Galagher W, Boyd D, Chew C, MacDonald N, et al. Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth. (2017) 118:424–9. doi: 10.1093/bja/aew466
PubMed Abstract | Crossref Full Text | Google Scholar
23. Zhao WL, Li SD, Wu B, Zhou ZF. Quadratus lumborum block is an effective postoperative analgesic technique in pediatric patients undergoing lower abdominal surgery: a meta-analysis. Pain Physicia. (2021) 24:E555–63.
24. Hung TY, Bai GH, Tsai MC, Lin YC. Analgesic effects of regional analgesic techniques in pediatric inguinal surgeries: a systematic review and network meta-analysis of randomized controlled trials. Anesth Analg. (2024) 138:108–22. doi: 10.1213/ANE.0000000000006341
PubMed Abstract | Crossref Full Text | Google Scholar
25. Zhu C, Wei R, Tong Y, Liu J, Song Z, Zhang S, et al. Analgesic efficacy and impact of caudal block on surgical complications of hypospadias repair: a systematic review and meta-analysis. Reg Anesth Pain Med. (2019) 44:259–67. doi: 10.1136/rapm-2018-000022
留言 (0)