The severe acute respiratory syndrome coronavirus (SARS-CoV-2) has a broad spectrum of clinical manifestations and has impacted over 77 million people globally since 2019. Around 66 million deaths were confirmed according to the World Health Organization (WHO) reports.[1] Coronavirus disease 2019 (COVID-19) is considered a multisystem disease as it affects the respiratory, cardiac, vascular, nervous, and renal systems. A study reported that COVID-19 has increased the incidence of heart failure and cardiovascular complications by 11.61 cases and 23.4 cases/1000 people.[2], respectively. Patients who recovered have experienced long-term lung damage such as inflammation and interstitial lung lesions which lead to breathlessness and dyspnea.[3-5] To address such complications, exercise rehabilitation programs such as high-intensity interval training (HIIT), supervised exercise, respiratory muscle training, and endurance training have shown significant improvements in symptoms such as dyspnea, breathlessness, even decreasing the risk of heart failure, and palpitations.[6-10]
Existing literature supports the effectiveness of exercise rehabilitation programs on a single system or whole-body system rather than focusing on these two isolated cardiac and respiratory stems together under one framework. There is a dearth of data regarding the effects of cardiopulmonary rehabilitation programs on both cardiac and respiratory systems in post-COVID-19 survivors. Hence, this systematic review addresses this gap by evaluating the effectiveness of comprehensive exercise rehabilitation programs that improve both the cardiac and respiratory functions together in COVID-19 patients.
METHODOLOGYThe Preferred Reporting Items for Systematic Reviews and Meta-Analysis 2020 guidelines were followed.
Search strategyThis systematic review considered the impact of rehabilitation programs that were found to improve cardiac and respiratory sequelae in COVID-19. A thorough search of literature was done on the PubMed, Cochrane Central Register of Controlled Trials, and TRIP databases. Medical subject headings terms were used to develop a search strategy (high-intensity interval training) OR (rehabilitation) OR (COVID-19) OR (exercise) AND (long COVID) were combined using the abovementioned Boolean operators [Table 1].
Table 1: Various databases searched.
Databases searched Boolean operators and keywords Total number of articles PubMed (high intensity interval training) OR (rehabilitation)) OR (COVID-19)) OR (exercise)) AND (long COVID)) Filters: from 2020 to 2024 35313 Cochrane Central Register of Controlled Trials (high intensity interval training) OR (rehabilitation)) OR (COVID-19)) OR (exercise)) AND (long COVID) in Title Abstract Keyword Filter: from January 1, 2020 to October 1, 2024 1984 Trip (high intensity interval training) OR (rehabilitation)) OR (Covid-19)) OR (exercise)) AND (long Covid) from_date: January 01, 2000 to_date: October 1, 2024 2066 39,363 Inclusion criteriaRandomized controlled trials (RCTs) that were published between 2020 and 2024 were included in this systematic review. Full-text manuscripts available in the English language were included in this study.
Exclusion criteriaNon-RCTs, cohort studies, cross-sectional studies, case–control studies, case series, case studies, or letter to the editor manuscripts were rejected. Patients who had pre-existing cardiovascular and respiratory health conditions and studies with an age group of <18 years old were excluded from the study.
Study selectionTwo reviewers (NJ and RS) independently evaluated titles and abstracts and articles that met the requirements, and were selected for full-text review. The full texts were then evaluated, retrieved, and assessed by the same two reviewers.
Data synthesisTwo independent researchers (NJ and KD) extracted the data, which included the authors information, the year of publication, study characteristics, sample size, and the type of article reviewed and findings which indicated improvement in cardiac and respiratory health as well as higher levels of VO2 max and heart rates in the intervention groups. In case of disagreements, the perspective of a third researcher (SK) was considered.
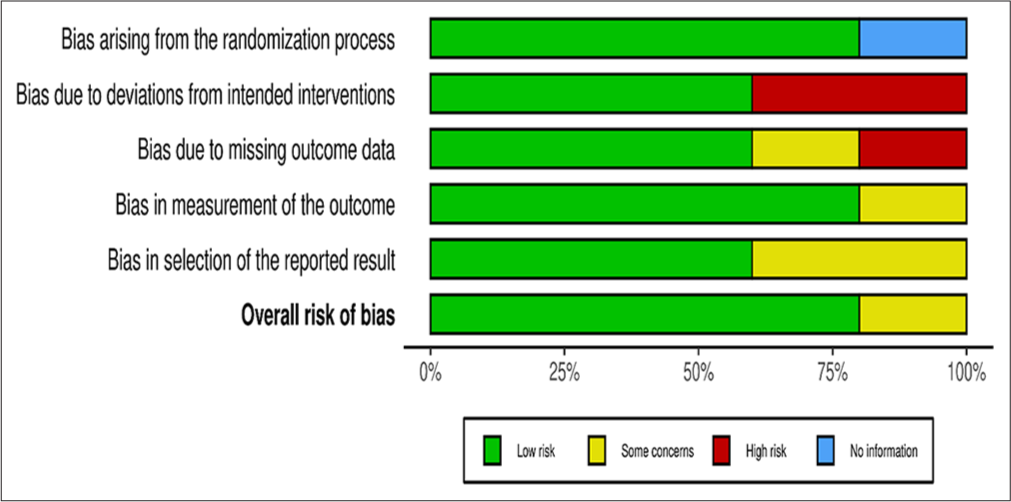
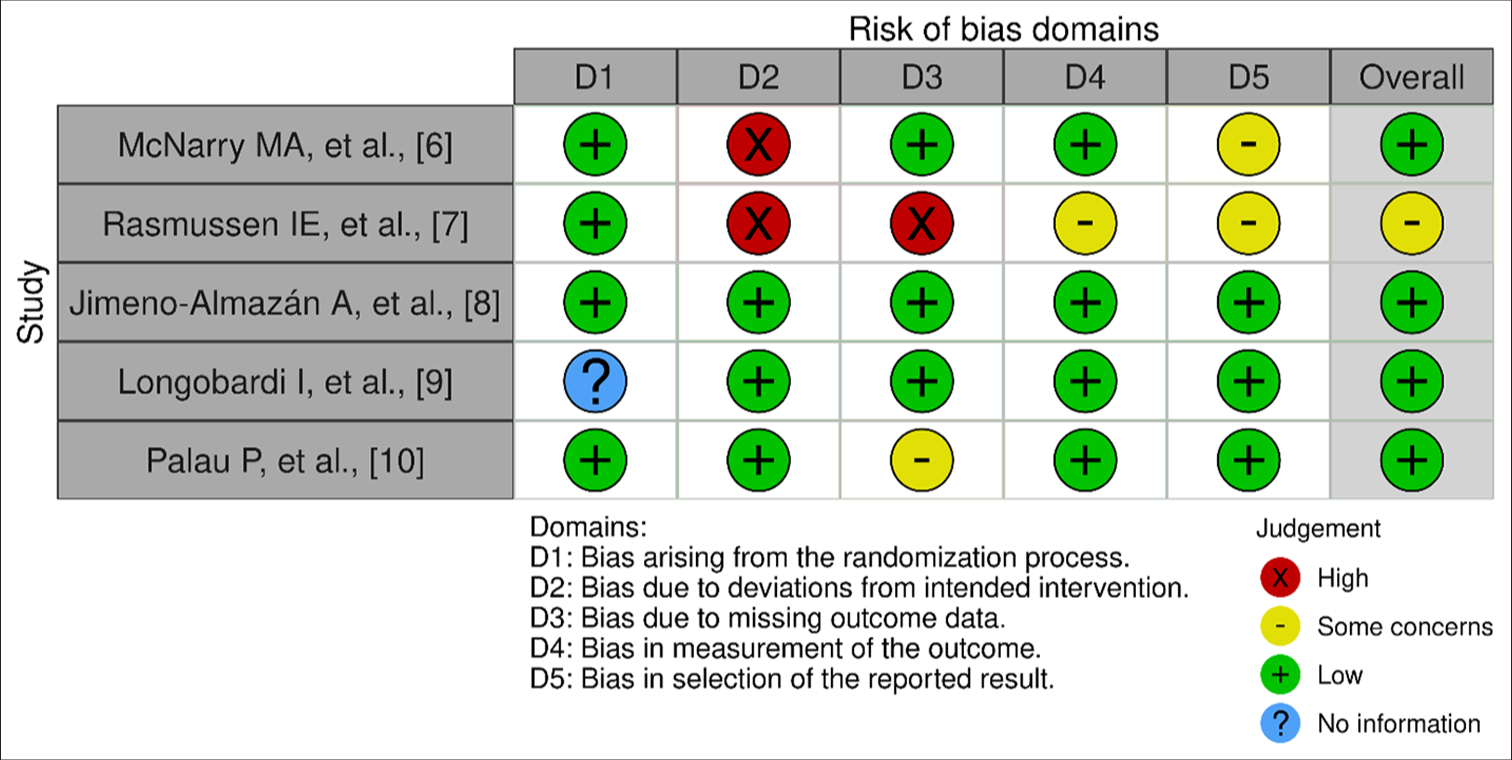
Quality assessmentThe Cochrane risk-of-bias method for randomized trials (RoB 2) was used and the quality assessment was done by two independent researchers (NS and KD) to assess risk of bias. Five domains were taken into consideration while creating traffic light plots and bar plots: randomization, deviation, missing outcome data, outcome measurement, and reported review selection were considered. All of the studies were rated as either high, no information or low risk of bias. A web-based application program, Robvis visualization tool was used for the visualization of the risk of bias assessment by developing traffic light plots and weighted bar plots for the risk of bias summary and figure.
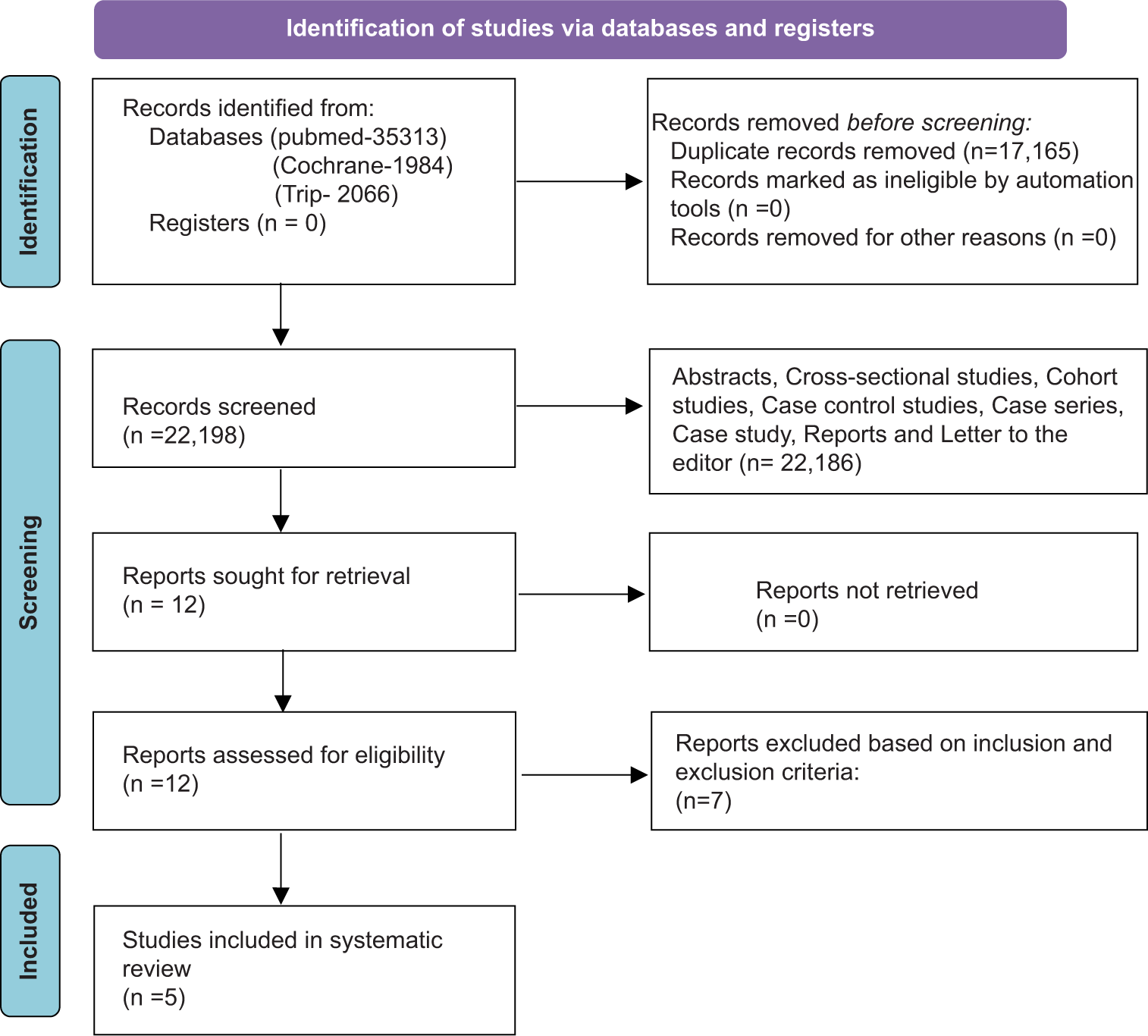
RESULTSThe systematic review consists of 5 RCTs. The articles identified through an extensive search on three databases generated 39,363 manuscripts. Among these, the duplicate records were removed (n = 17,165). Records screened during the research amounted to 22,198. Records were also excluded due to study design (n = 22,186). Ultimately twelve records were accessed for eligibility criteria and a total of seven records were excluded based on the inclusion and exclusion criteria. Finally, five records were included in the systematic review. The five RCTs involved a total of 291 participants [Figure 1]. These RCTs have shown significant improvements in the rehabilitation intervention groups. On the contrary, the control group showed no significant improvement.
Export to PPT
Risk of bias assessmentRobvis visualization tool is a web-based application program, designed for the visualization of risk of bias assessment as a part of a systematic review by developing traffic light plots, and weighted bar plots for risk of bias summary and figure [Figures 2 and 3].
Export to PPT
Export to PPT
Figure 2 shows a weighted bar plot for the risk of bias summary and Figure 3 shows a traffic light plot. The figure of the risk of bias was generated based on five domains. All the included RCTs underwent a quality assessment by the RoB 2 tool. Overall risk of bias for the five RCTs was found to be at a low risk 80% and 20% of the RCTs represented some concerns.
Bias arising from the randomization process (domain 1) 80% of the RCTs were at low risk, for the second domain bias due to deviations from intended interventions, 60% of the RCTs were found to be at low risk, for the third domain bias due to missing outcome data, 60% were at low risk, for the fourth domain bias due to measurement of the outcome, 80% were at low risk, and for domain 5 bias in the selection of reported results, low risk was found in 60% of the RCTs.
Details of studies showing the country of study, study design the number of intervention patients, the number of control group patients, intervention given, major findings, limitations, and outcome of the five RCTs have been depicted in Tables 2 and 3, respectively.
Table 2: Details of studies showing the country of study, study design the number of intervention patients, the number of control group patients, and intervention given.
Author, year Country Study design Intervention group Control group Intervention given Mcnarry et al., 2022[6] United Kingdom RCT 111 37 Aerobic Exercise, Respiratory Muscle Training, IMT, Physical Exercise, Strength Exercise. Rasmussen et al., 2023[7] Denmark RCT 14 14 12-week HIIT [High Intensity Interval Training] scheme: 3 training session on A Bicycle Ergometer [Aerobic Training]. Jimeno-Almazán et al., 2022[8] Spain RCT 19 20 Multicomponent Exercise Program based on concurrent training for 8weeks through supervised interventions [Resistance Training combined with Aerobic Training, Moderate Intensity Variable Training], monitored light Intensity continuous training]. Longobardi et al., 2023[9] Brazil RCT 25 25 HBET Program: A semi-Supervised Exercise Program conducted 3 times in a week for about 60–80 min per session. Exercise Cards and Videos, Aerobic Training, Strength Training, Active Stretching. Palau et al., 2022[10] Spain RCT 13 13 A Home-Based 12-week Program of IMT arm training using Threshold Inspiratory Muscle Trainer.Table 3: Details of studies showing major findings, limitations, and outcome.
Author, year Findings Limitations Outcome Mcnarry et al., 2022[6] VO2peak is increased by 5.2 mL/kg/min. Effect size=0.43. Small sample size with majority of female generalizability developed.Improvement analysis of VO2 peak and maximum heart rate (HR max) between the rehabilitation group and control group in each RCTs.
The mean difference (MD) for VO2 peak was 2.42, the HR max value increased (MD = 5.33), and left ventricular mass (LVM) increased by MD = 6.8 indicating enhanced cardiovascular conditioning and functioning. Maximum voluntary ventilation (MD = 5.3) improved respiratory endurance along with increased stability in FEV1 and FVC.
Therefore, we can deduce that the intervention group demonstrated a significant improvement in respiratory as well as the cardiovascular system functions. On the contrary, the control group showed a lower less or no improvement as per the data [Table 4].
Table 4: pVO2 max values and the heart rate max values in each study conducted and the mean differences between the rehabilitation (intervention) group and the control group.
Authors VO2 peak (ml/kg/min) Heart rate max (beats/min) Rehabilitation Control Mean difference Rehabilitation Control Mean difference Mcnarry et al.[6] 42 36.8 5.2 Not available Not available Not available Rasmussen et al.[7] 27.8 24.7 3.1 Not available Not available Not available Jimeno-Almazan et al.[8] 38.9 36.1 2.8 144 135 9 Longobardi et al.[9] 22.2 21.3 0.9 154 143 11 Palau et al.[10] 18.9 18.8 0.1 136 140 -4 Total mean difference 2.42 Total mean difference 5.33 DISCUSSIONThis systematic review revealed that the exercise-based rehabilitation programs improved the cardiovascular and respiratory sequelae, such as dyspnea, chest pain, heart failure, pulmonary hypertension, and arrhythmias in post-COVID-19 survivors. This study showed that the effects of HIIT programs on cardiopulmonary health in post COVID-19 patients acted as a therapeutic management. This can greatly reduce the burden of disease in long COVID patients which is still a significant complication.[6]
Rasmussen et al. conducted a RCT including 28 participants, intervention (n = 14) and control (n = 14). The intervention group underwent supervised HIIT-based exercise programs for a 12-week duration. The inclusion criteria were patients confirmed COVID-19 by PCR more than 4 weeks and <6 weeks, aged ≥40, patients with atrial fibrillation and flutter, acute myocarditis, and those undergoing treatment with interleukin (IL)-6 receptor antagonists such as tocilizumab and sarilumab. The outcomes indicated that the intervention group showed a significant increase in LVM by MD of 3.1 and P = 0.04. The data were were not statistically significant due to high variability and insufficient statistical power despite the improvement in cardiorespiratory fitness (VO2 peak).[7]
Increased VO2 peak reflects the improvement in cardiorespiratory fitness.[11,12] No improvement in pulmonary function, such as diffusing capacity for carbon monoxide (DLCO) suggested that post-COVID lung changes were primarily associated with fibrosis and resistance to any modifications.[13]
Jimeno-Almazán et al., performed a RCT involving concurrent training at low and moderate intensity as an intervention whereas the control group followed general rehabilitation care according to the WHO guidelines.[8] The study showed notable improvements in VO2 max by an average of 2.1 ml/kg/min, which was clinically translating into better results in cardiopulmonary health.[14,15] In addition, 83.3% of patients reported relief in symptoms as compared to 5.4% standard care group. There was a reduction in heart rate (HR = 13.3%) and perceived exertion, indicating improved cardiovascular health. The control group has not experienced same level of improvement reflecting the superiority of the tailored exercise program over general rehabilitation in addressing cardiac and respiratory issues.[16]
A similar outcome noted in a study conducted by Palau et al. included home-based inspiratory muscle training (IMT) program as an intervention. The trial receded a significant enhancement in HR response suggested that IMT had positive effects on autonomic regulation and overall cardiac function. The study showed a significant increase in VO2 peak by 0.1 ml/kg/min, ventilatory efficiency increased by 18.9%, better performance and reduced breathlessness in long COVID patients, and the increase in the percentage of DLCO 72.8% showed improvement in lung function and breathing patterns during hyperpnea.[10] These results align with both Rasmussen et al. and Jimeno-Almazán et al.[7,8]
A study by Mcnarry et al. showed that VO2 peak was increased by 5.2 ml/kg/min (effect size = 0.43) in the rehabilitation group which was greater than the control group.[6] Similar results are seen in the study of Longobardi et al. (2023) where VO2 peak (MD = 4.46) and HR max (MD = 11 bpm) increased. These interventions improved the cardiovascular fitness in COVID-19 patients compared to the control group as they had a positive effect on the respiratory endurance and sufficiency as well as on the heart rate.[9]
These findings aligned with the results of the study of Nantakool et al. which showed that the beneficial effects of exercise rehabilitation programs on the cardiopulmonary fitness in post-COVID-19 patients. These improvements could possibly be explained by the mechanism of central and peripheral adaptations, for example, the increase in endothelial functions and arterial compliance as well as an improved cardiac reserve.[13]
A study by Torres and Gradidge showed that rehabilitation programs significantly improved the cardiopulmonary functions in patients post-COVID-19 as compared to the control group. However, this systematic review did not consider the effect of the COVID vaccine on these patients, and hence, it could be a possible confounding variable.[12]
Thirupathi et al. showed that exercise intensity should be prescribed to COVID-19 patients according to the severity of the disease to obtain maximum benefit instead of causing adverse physiological effects. It also revealed that low-to-moderate exercise intensity showed good results in mild to moderate COVID-19 patients.[17]
An observational quasi-experimental study by Szarvas et al. showed that post-COVID-19 patients benefitted from the complex cardiopulmonary rehabilitation programs and improved their quality of life. These programs also improved the exercise tolerance of these patients with an adaptation of the cardiovascular system.[18] A study by Nopp et al. concluded that daily individualized interdisciplinary rehabilitation programs for 6 weeks could improve the quality of life, decrease dyspnea, and increase walking capacity in 58 patients suffering from severe post-COVID-19 syndrome.[3]
A narrative review by AkbariRad et al. recommended that cardiopulmonary rehabilitation is a necessity in the management of COVID-19 patients, especially those who were admitted in the intensive care unit. It also revealed that these rehabilitation programs could alleviate the development of complications, reduce mechanical ventilation time, the risk of being readmitted, mortality rate, and the length of the hospital stay. This aligned with the results of this study that the purpose of cardiopulmonary rehabilitation programs is to improve physical recovery from post-COVID-19 complications.[19]
Many studies have emerged to understand the post-COVID-19 long-term impacts on the cardiovascular and respiratory systems individually but few studies have been done to study the simultaneous effect of these rehabilitation interventions on cardiac and respiratory systems. More studies are required to devise new management strategies to reduce these aftermath effects, but larger and better-defined RCTs are needed to understand the details of exercise rehabilitation programs on both cardiac and pulmonary systems.[20,21]
Aerobic exercises such as walking (e.g., a 6-min walk and brisk walking) or cycling enhance cardiovascular and respiratory functioning as it increases the stroke volume, cardiac output, and lung volume, which leads to the reduction of the heart’s workload and improves the blood circulatory system, optimizing oxygen delivery and ventilation-perfusion matching. These adaptations increase the cardiac efficiency and allow a higher HR max during physical activity while reducing excessive heart rate.
Regular exercise training also strengthens respiratory muscles, attenuates dyspnea, and raises VO2 peak, which reduce systemic inflammation and provide an anti-inflammatory effect that shows improvement in vascular health. It supports cardiac function and prevents further damage to lung tissues. For post-COVID individuals, exercise helps in balancing the autonomic and reducing inflammatory markers such as C-reactive protein and IL. Through these mechanisms, exercise rehabilitation programs benefit cardiovascular and respiratory health.[22,23]
CONCLUSIONThe SARS-CoV-2 pandemic has affected a huge number of people worldwide since 2019 and its ongoing impacts are still being seen among many COVID-19 survivors. The intervention programs in this systematic review have shown considerable progress in improving cardiovascular and respiratory health conditions. The analyses validate and fill the research gap by bringing into consideration the effectiveness of comprehensive exercise rehabilitation programs, treating both the aspects of cardiac and respiratory complications andresulting in long-term recovery. Future research should prioritize the development of effective rehabilitation programs that address the cardiopulmonary complications. This review highlights exercise-based rehabilitation interventions as one of the most effective solutions to reduce the chronic symptoms and strengthen both the cardiac and respiratory health in post-COVID-19 patients.
留言 (0)