The IUGA and ICS classify urinary incontinence (UI) as involuntary urine loss, with main types being stress (SUI), urgency (UUI), and mixed (MUI) incontinence. UI’s causes often relate to age, gender, BMI, and vaginal delivery history. Global UI rates differ by country and diagnostic practices. In China, adult female UI prevalence ranges widely, from 8.7 to 69.8% (1, 2). Treatment for SUI can encompass a variety of approaches, with the choice of therapy typically depending on the severity of symptoms, patient preferences, and willingness to undergo surgical treatment. The main treatment options include lifestyle modifications, Pelvic Floor Muscle Training (PFMT), physical therapy, pharmacological management, and surgical interventions.
Multiple guidelines, including those from the American College of Obstetricians and Gynecologists (ACOG), the International Consultation on Incontinence (ICI), and the National Institute for Health and Care Excellence (NICE) in the UK, mention Kegel exercises (Pelvic Floor Muscle Training) as an effective part of non-surgical treatment to help improve urinary incontinence (3–5). PFMT can strengthen the pelvic structure, yet many individuals with SUI struggle to execute PFMT properly, and the main challenge is maintaining long-term adherence to the treatment (6).
Drug therapy causes problems such as side effects and surgery exists associated with risks (7, 8). Expanding the currently available treatment options, and developing individualized treatment plans for patients according to a woman’s lifestyle, expectations, and goals for treatment, as well as her tolerance for potential adverse events is becoming increasingly important (9). Acupuncture may improve urinary incontinence through its effects on neural regulation (10), enhancing the pelvic floor muscles (6). Both electroacupuncture(EA) and manual acupuncture can effectively improve stress urinary incontinence, and older women and women after childbirth can also benefit from acupuncture treatment (11–14). However, the Cochrane review published in 2013 and 2022 believed that the evidence for the effect of acupuncture on stress urinary incontinence or improvement of overactive bladder symptoms was not clear, and the conclusions should be used with caution due to the generally low quality of the included studies (15, 16).
Electroacupuncture has been proven effective in improving stress urinary incontinence, but research has been limited. This systematic review and meta-analysis evaluate the effectiveness and safety of electroacupuncture in treating stress urinary incontinence and further assesses the efficacy of combining acupuncture with conventional treatment (PFMT) as a supplemental therapy.
2 Materials and methodsThe meta-analysis was registered in PROSPERO (CRD42022381409) and prepared according to preferred reporting items of systematic reviews and meta-analysis (PRISMA) (17).
2.1 Data sources and literature searchA comprehensive literature search was conducted from inception to January 2023, including databases such as PubMed, Embase, Cochrane, and CNKI. In the search strategy, a systematic approach was utilized with the following Medical Subject Headings (MeSH) and free-text keywords. The studies were not restricted to those published in English. Additionally, the references of related documents were searched to ensure their identification as comprehensively as possible.
2.2 Inclusion and exclusion criteriaInclusion criteria: (1) Participants: Women with stress urinary incontinence. (2) Interventions: electroacupuncture, acupuncture combined with PFMT. Types of interventions acupuncture therapies include penetrating the skin (acupuncture, electroacupuncture, and warm needling), control acupuncture (non-penetrating the skin), and PFMT individually; (3) Study design: Designed as a randomized controlled trial (RCT).
Exclusion criteria: (1) We excluded mixed incontinence and other types of incontinence; (2) Studies with additional interventions other than acupuncture or PFMT were excluded.
2.3 Study selectionThe literature screening was done independently by two authors (TJ, ZYD), Firstly screening the title and abstract, eliminating the literature that does not meet the requirements, and further reading the full text to screen literature. After the data extraction a meta-analysis was performed. Any disagreement was resolved by discussion until consensus was reached or by a third author (YG).
2.4 Data extraction and outcome measuresTwo independent reviewers (TJ, ZYD) extracted the data from the included studies. The extracted data included the first author’s name, year of publication, sample, participant characteristics (screening tools, age, severity), intervention characteristics, control characteristics, therapy duration, study outcomes. Any discrepancies were addressed through discussion, and consensus was achieved among the reviewers.
Primary outcome: Urine leakage 1 h (by urinal pad test), international consultation on incontinence questionnaire short form (ICIQ-SF), adverse events.
Secondary outcomes: 72-h incontinence episodes. Self-report (self-evaluation of therapeutic effects, severity of stress urinary incontinence).
SUI severity was defined based on baseline levels of urine leakage (mild, 1.1–9.9 g; moderate, 10–49.9 g; severe, ≥50 g) (18). To include a greater number of studies, the mean baseline levels were taken into consideration.
2.5 Risk of bias assessmentThe Risk of bias tool (19) was used to evaluate the quality of included studies. The items were as follows: (1) Random sequence generation (selection bias); (2) Allocation concealment (selection bias); (3) Blinding of participants and personnel (performance bias); (4) Blinding of outcome assessment (detection bias); (5) Incomplete outcome data (attrition bias); (6) Selective reporting (reporting bias); (7) Other bias. Quality assessments were performed independently by two authors. Any disagreements are resolved by a third investigator.
2.6 Data analysisReview Manager 5.3 and STATA version 16.1 (Stata Corp, College Station, Texas, USA), and SAS (Statistics Analysis System9.4, USA) were used to perform meta-analysis.
For continuous variables, we calculated the effect sizes as mean difference (MD) and 95% confidence interval (CI) between the acupuncture intervention and control arms. Categorical variables were pooled as risk ratio (RR) and 95% CI. For ordered categorical variables, effect size (logor) and standard error (selogor) were calculated by the cumulative ratio model and the generic inverse variance method was used to calculate OR and 95% CI (20, 21).
The random-effect model was employed by using Inverse Variance Method when the study of heterogeneity (I2) was larger than 50%; otherwise, a fix-effect model was employed by using the inverse variance method when the I2 was less than 50%.
The data reported by interquartile range for continuous outcomes was transformed into mean and standard deviation (22, 23), when it was necessary. The data reported as means and 95% confidence intervals were transformed by the following formula.
The data reported only in the form of means and standard deviations at baseline and after treatment are transformed by the following formula.
SD1C=SD1B2+SD1F2−2×R1×SD1B×SD1F¨.Subgroup analyses include population (diagnostic criteria, severity, age) and intervention (intervention types, acupoints belong to, duration).
3 Results 3.1 Literature searchThere were 417 studies retrieved from the database searches, and 96 duplicates were eliminated. Two reviewers conducted screening of titles and abstracts and full-text assessment independently. Ultimately, 11 studies were included in this review and meta-analysis. (Figure 1 and Supplementary Figure S2).
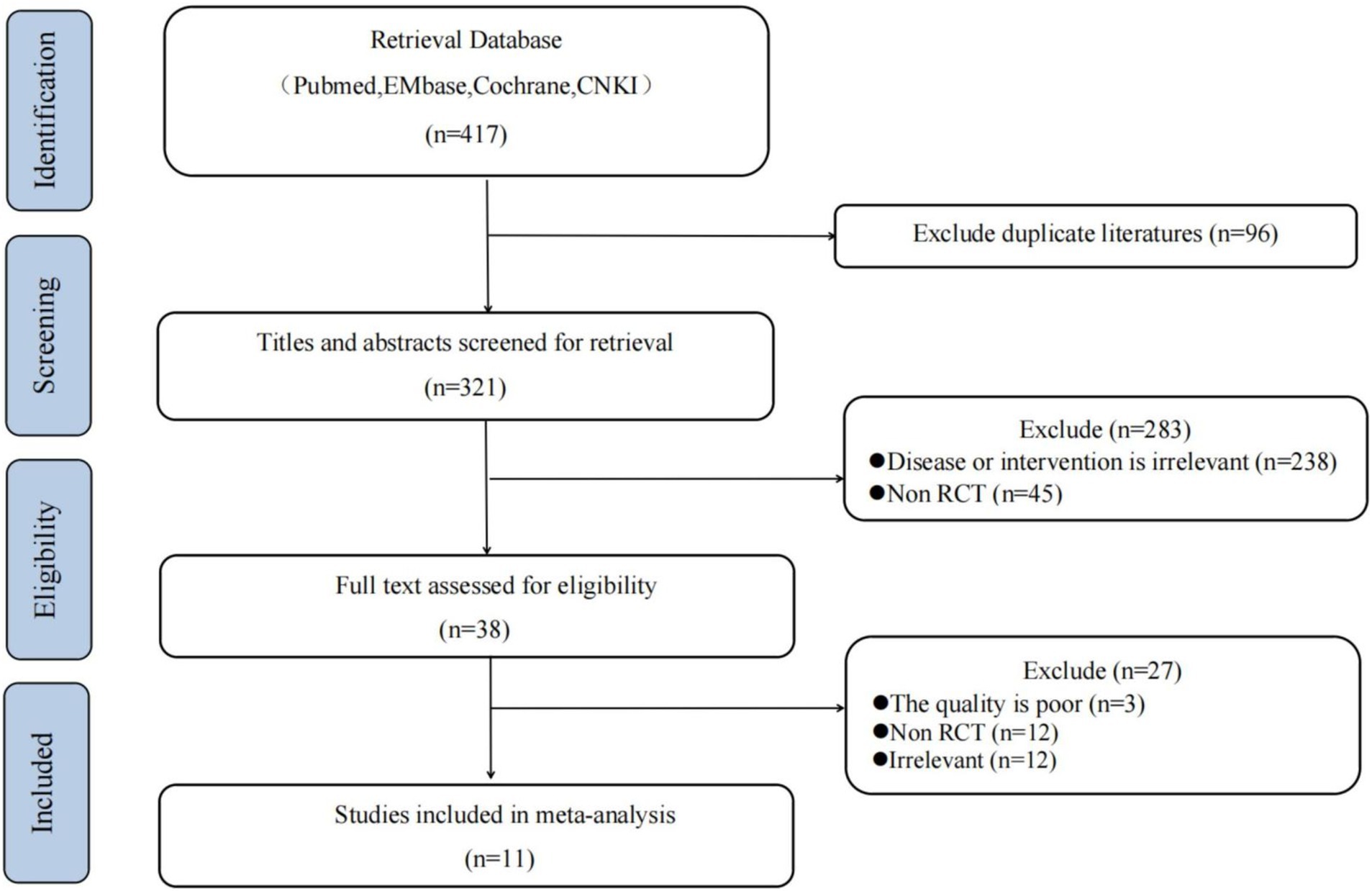
Figure 1. Flow chart of study.
3.2 Study characteristicsEleven studies were included in the analysis, published between 2017 and 2022, with sample sizes ranging from 42 to 504. All studies originated from China, with five studies comparing electroacupuncture (EA) with sham electroacupuncture (placebo EA), and six studies comparing acupuncture or manual acupuncture combined with PFMT with PFMT alone. The specific details are shown in Table 1.
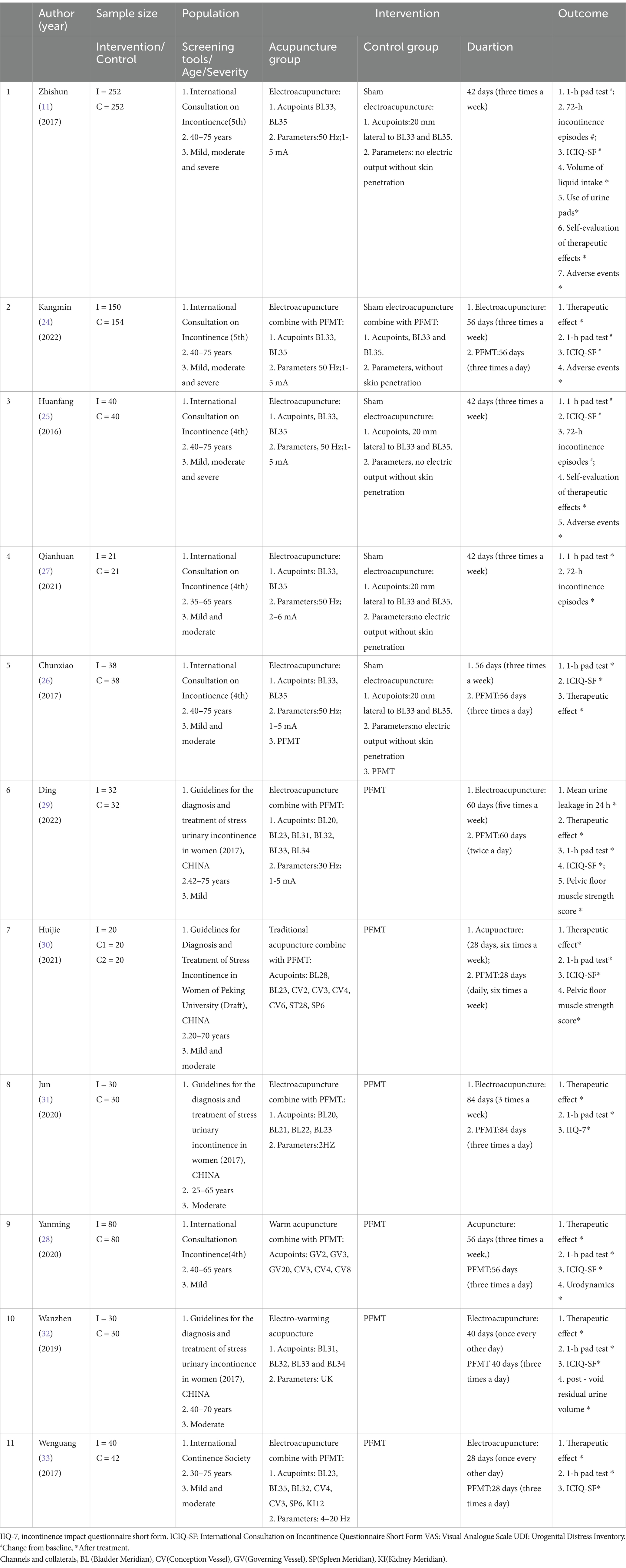
Table 1. Characteristics of the studies included.
3.3 Quality assessment of the included studies11 studies reported a random sequence generation method, six studies used a central randomization system or block randomization (11, 24–28), and in five studies randomization was done with the use of a random digit table (29–33). Six studies reported concealment of the allocation (11, 24–28). Four studies describe blinded method, one study was single-blinded (26), three were double-blind (11, 24, 25). Four studies reported blinding of outcome assessors (11, 24–26). No studies were found to have incomplete outcome data. Only three studies were registered on ClinicalTrials.gov (11, 24, 25), and we assessed them without selective reporting and other biases, all other studies were of unknown risk (Figure 2).
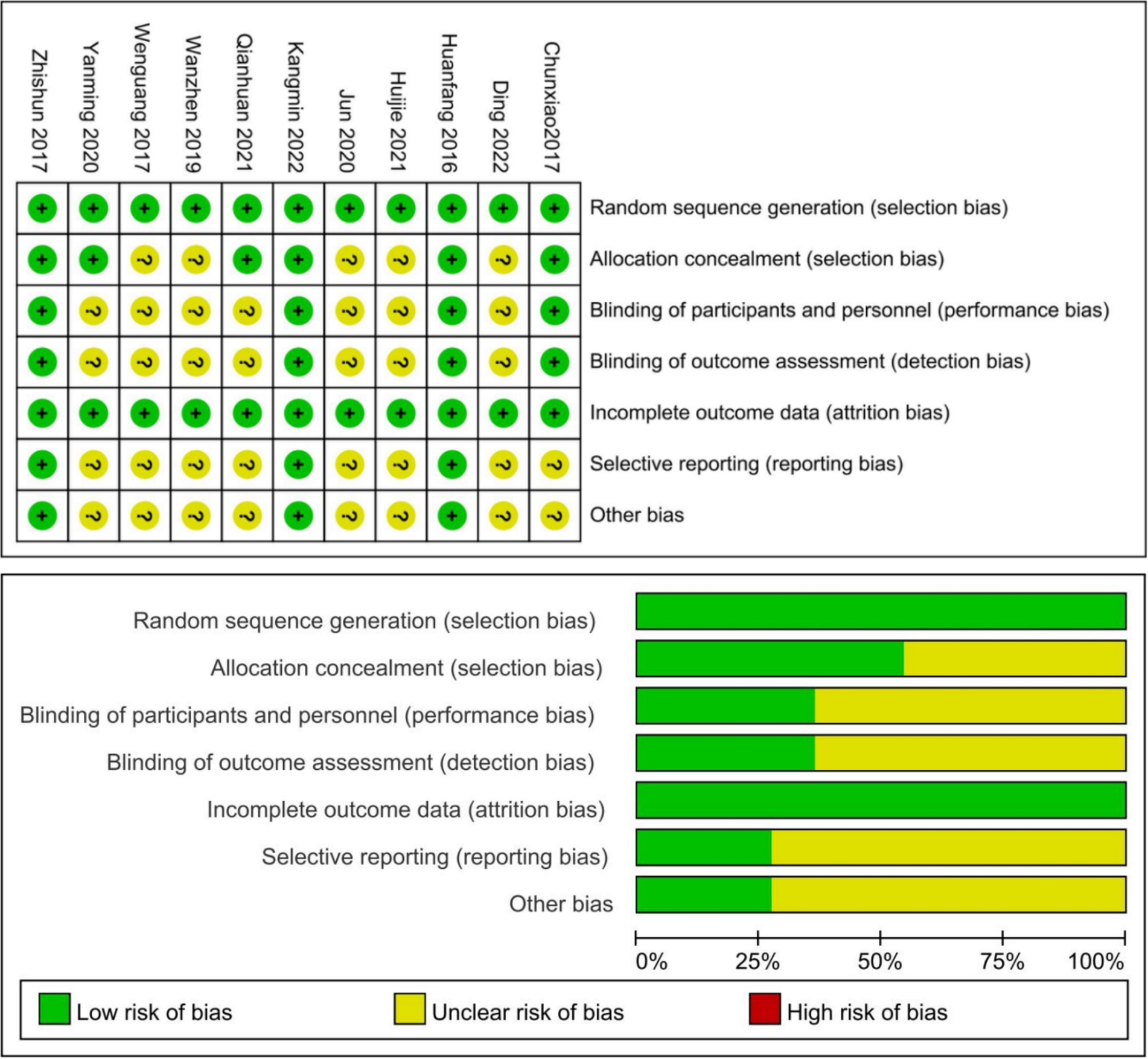
Figure 2. Risk of bias of the included studies.
3.4 ResultsIn the comparison of Urine leakage1 hour and ICIQ-SF, pooled five high-quality studies results showed that (11, 24–27), there was a significant association between EA intervention and improvement in Urine leakage compared to sham EA (MD = 4.69, 95% CI 2.83 to 6.55, I2 = 62%). Compared with sham EA, EA can significantly improve ICIQ-SF in SUI patients (11, 24–26) (MD = 2.61, 95% CI 1.64 to 3.58, I2 = 65%). The results were robust for the sensitivity analyses. A comparison of the three studies found no heterogeneity in significant differences in patients’ self-reports of therapeutic effects (OR = 10.46, 95% CI 7.81 to 14.01, I2 = 0%).
In the comparison of adverse events, the data of 3 studies showed that EA did not increase the incidence of adverse events compared with placebo EA (RR = 1.08, 95% CI 0.50 to 2.35, I2 = 0%).
In a comparison of PFMT combined with acupuncture group and PFMT individually group, a total of 6 low-quality studies showed (28–33) that compared with PFMT individually, the combined use of acupuncture can improve the urine leakage 1 h in SUI patients, but there is obvious heterogeneity (MD = 1.91, 95% CI0.96 to 2.86, I2 = 80%). Five studies showed that the combined use of acupuncture could improve ICIQ-SF of SUI patients (28–30, 32, 33) (MD = 2.63, 95% CI1.60 to 3.65, I2 = 75%). The results were robust for the sensitivity analyses (Supplementary Figure S1). The comparison of four studies found no heterogeneity of significant differences in patients’ self-reported therapeutic effects (OR = 3.79, 95% CI 2.39 to 6.00, I2 = 0%) (28–31).
Subgroup analyses
The results of subgroup analyses by urine leakage 1 h are summarized as follows, in the three studies (28, 29, 33) that included subjects who tended to have mild stress urinary incontinence (MD = 1.46, 95% CI 0.82 to 2.10, I2 = 58%). In the three studies that tended to have moderate stress urinary incontinence, study heterogeneity increased and effect size increased (MD = 4.9, 95% CI 1.72 to 8.08, I2 = 77%) (31–33). There were also significant differences between subgroups (I2 = 77%, p = 0.04). In the subgroup analysis of different intervention types, the two studies of manual acupuncture were combined (28, 30) and no significant effect was found (MD = 1.11, 95% CI –0.61 to 2.83, I2 = 86%). In the subgroup analysis of the acupoints, the two studies involving the bladder meridian and others were combined (30, 33) and no significant effect was found (MD = 2.58, 95% CI –0.28 to 5.43, I2 = 88%).
The results of subgroup analyses by ICIQ-SF are summarized as follows, in the subgroup analysis of different intervention types, the two studies of manual acupuncture were combined (28, 30) and no significant effect was found(MD = 1.47, 95% CI –1.39 to 4.33, I2 = 93%), and 20–75 years old in the age subgroup (30, 33) no significant effect was found (MD = 2.10, 95% CI –0.15 to 4.34, I2 = 85%). In the subgroup analysis of acupoints, the two studies of bladder meridian combined with others were combined (30, 33) and no significant effect was found (MD = 2.10, 95% CI –0.15 to 4.34, I2 = 85%) (Tables 2–4).
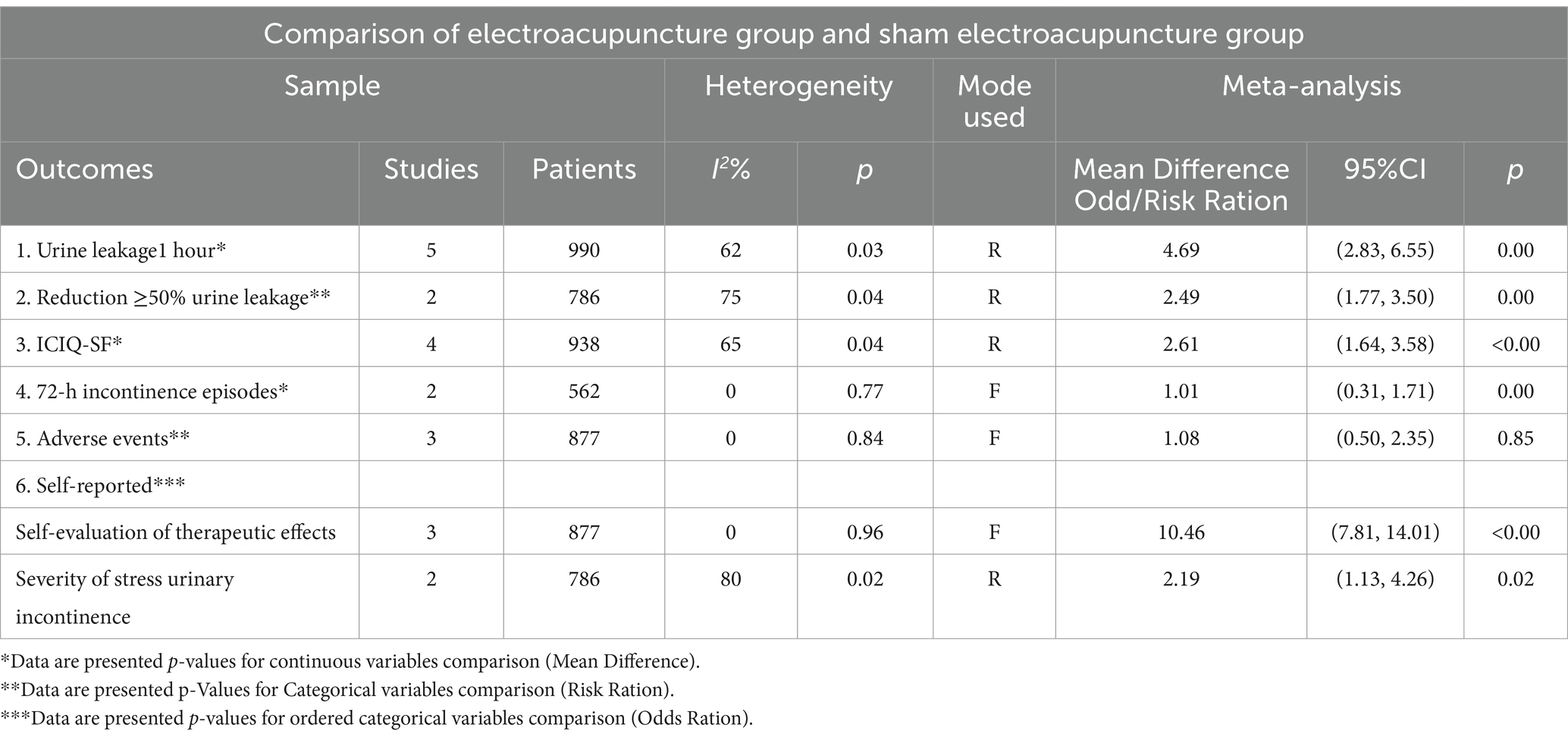
Table 2. Meta-analysis for electroacupuncture.
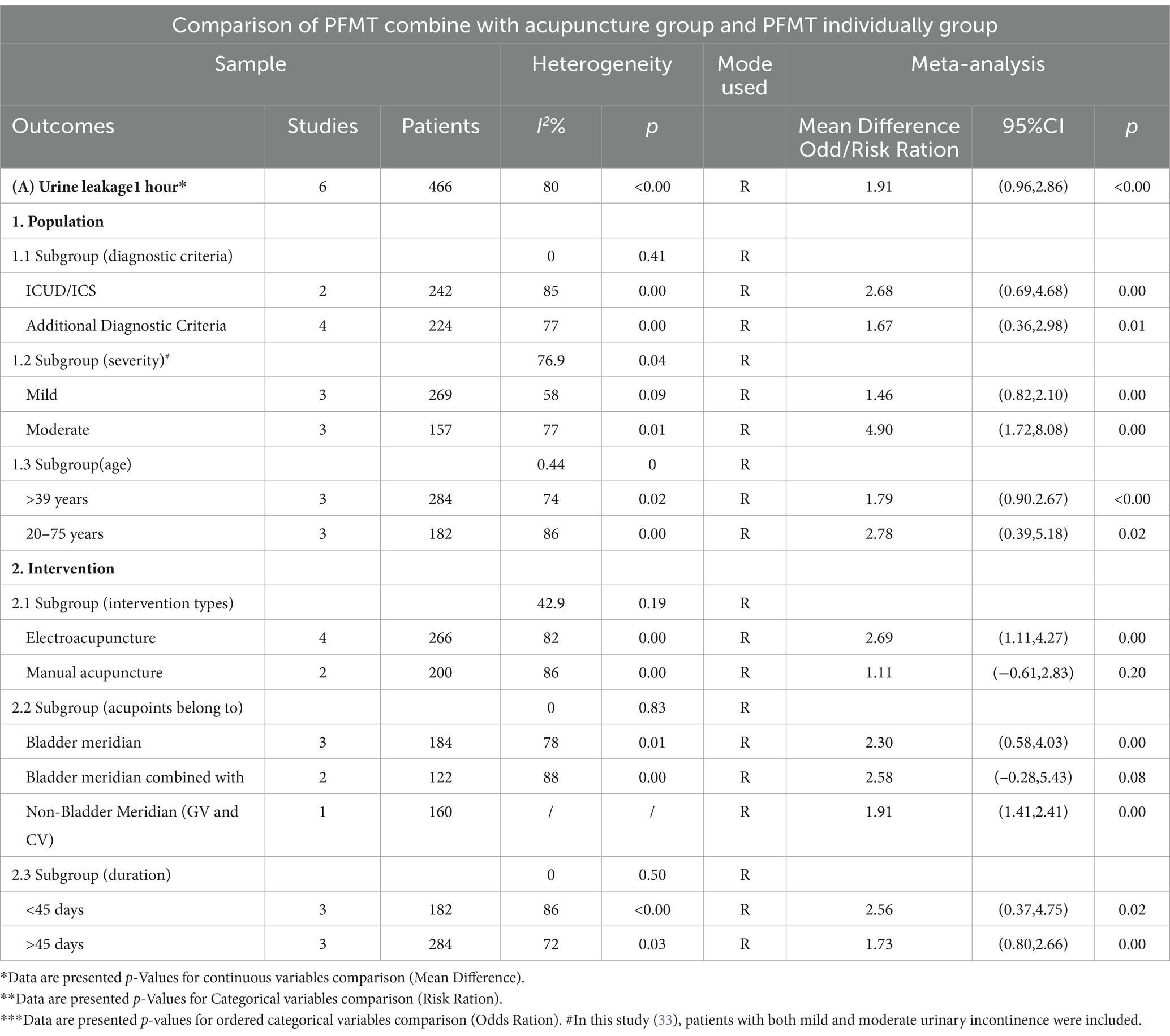
Table 3. Meta-analysis for PFMT combine with acupuncture.
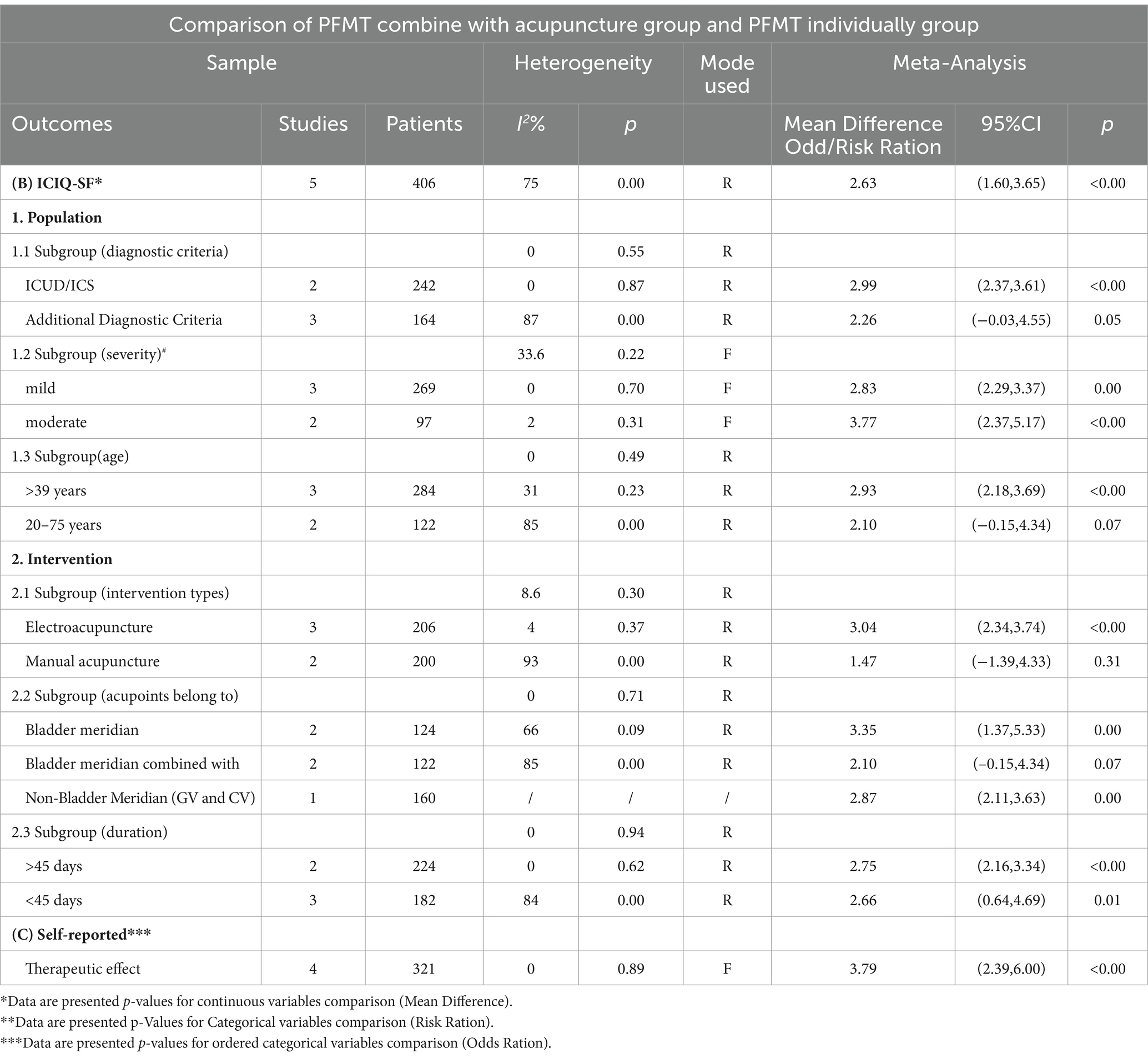
Table 4. Meta-analysis for PFMT combine with acupuncture.
4 Discussion 4.1 Main resultsBased on high-quality evidence, the outcome of this study indicates that the application of EA could ameliorate SUI patients’ symptoms and enhance their quality of life, there were also no significant differences in adverse event reporting. Additionally, the application of EA combined with PFMT was more effective than using PFMT individually, and the within-group was still substantial in different subgroups. In summary, these conclusions support the use of electroacupuncture as a potential non-surgical treatment method to improve symptoms and quality of life in patients with SUI. However, to ensure the generalizability and applicability of these findings, future research is needed to further explore and validate the optimal treatment protocols and long-term effects.
4.2 What ideas does our research provide for clinical applications?In contrast to the preceding meta-analyses (34, 35), the inclusion of the CNKI database search in our analysis was justified by the widespread use of acupuncture in China. Furthermore, it was essential to augment and enhance the evidence base, despite the fact that some of the studies included were of low quality. Our subgroup analysis indicated that the efficacy of acupuncture might be influenced by the severity of the disease, a finding that is corroborated by previous studies suggesting a correlation between the duration of urinary incontinence and the effectiveness of acupuncture (36).
Additionally, we observed that the effectiveness of manual acupuncture was slightly inferior to that of electroacupuncture, leading us to hypothesize that the efficacy might be related to electrical stimulation. In the subgroup analysis, no significant differences were found in either the subgroup of the bladder meridian combined with other meridians or the subgroup of manual acupuncture. This might be due to the manual acupuncture used in the study (30), which included mainly patients with mild to moderate stress urinary incontinence. We speculate that electroacupuncture could be more effective than manual acupuncture, especially for patients with moderate incontinence. However, this conclusion requires further research due to the limited number of studies available.
4.3 What progress does our research provide for future research?Challenges still exist in the establishment of acupuncture control groups in the present clinical studies. Control acupuncture is mainly included without skin penetration and more shallow insertion of needles in suitable acupoints, acupuncture without skin penetration might not blind the participants in the placebo group adequately, and central μ-opioid receptor binding potential, which had a similar effect as acupuncture, could be increased if the non-acupoints were shallowly punctured (37, 38). The different of control acupuncture type indirectly affects the evaluation of acupuncture effect (37, 39). Compared with the previous meta-analysis (40, 41), this meta-analysis was placebo-controlled all were without skin penetration in the comparison of the electroacupuncture group, and the placebo control group may have reduced the potential for bias in the results. In addition to these, our study compared the differences before and after treatment, which may have reduced the potential bias caused by inconsistent baseline levels.
Nevertheless, all included studies were conducted in China, where satisfactory therapeutic effects might involve patients’ expectancies, beliefs, and the psychosocial context (42, 43). Multi-center validation of institutions in different countries and regions was requisite to guarantee the external validity of the study findings. Lastly, despite acupuncture had been considered safe in most studies (44, 45), it was an invasive procedure after all, and relevant adverse events would be reported as necessary, though over half of the included studies did not report it.
4.4 Strengths and limitationsThrough detailed subgroup analyses based on inclusion criteria, intervention populations, and treatment duration, this study found that the efficacy of electroacupuncture combined with PFMT may be influenced by the severity of the condition. Due to the limited number of studies included, no significant intergroup differences were found between different types of acupuncture. However, it is speculated that the therapeutic effect of electroacupuncture might be superior to manual acupuncture. These results can assist physicians in selecting the most appropriate treatment methods for patients with varying degrees of SUI, especially when considering the use of electroacupuncture as an adjunctive treatment.
The study has several limitations, firstly, high heterogeneity was found in the comparison of acupuncture combined with PFMT, and this heterogeneity still persisted in subgroup analyses. The number of studies in this meta-analysis did not report details about the methodology. Based on the poor quality of the included studies, the sources of heterogeneity include not only clinically related heterogeneity, but methodology-related heterogeneity is also an essential factor of high statistical heterogeneity. The key point to high-quality evidence is to establish a study design with reliable evidence quality (46). Secondly, the publication bias cannot be assessed by funnel plot since the number of included studies was insufficient in the meta-analysis. Thirdly, the onset of SUI may be influenced by factors such as age, obstetric history, BMI, hormonal levels, chronic diseases, and lifestyle. We recommend that future research should provide detailed definitions and control over these factors. Doing so can enhance the quality and reliability of the studies, assist in identifying the SUI patient population most suitable for acupuncture treatment, and optimize treatment plans. This will contribute to improving therapeutic outcomes and providing stronger evidence to support clinical practices.
5 ConclusionThe results of this meta-analysis indicate that EA is more effective in improving the clinical symptoms and quality of life of patients with SUI compared to sham electroacupuncture, without increasing the risk of adverse events. Moreover, the therapeutic effect of SUI treated with electroacupuncture combined with PFMT yields a more positive response than PFMT alone. There are significant differences in treatment response among patients with varying severities of stress urinary incontinence, which deserves attention. Additionally, even though acupuncture is generally considered safe, detailed reporting on adverse events associated with acupuncture is necessary. Overall, electroacupuncture therapy alone or as an adjunctive treatment in combination with pelvic floor muscle training is beneficial for patients with stress urinary incontinence, offering additional clinical treatment options.
Data availability statementThe datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author contributionsTJ: Conceptualization, Data curation, Methodology, Writing – original draft, Formal analysis, Validation. Z-YD: Conceptualization, Data curation, Writing – original draft. YS: Conceptualization, Formal Analysis, Supervision, Writing – review & editing. Y-QZ: Writing – review & editing. H-BZ: Writing – review & editing, Conceptualization, Supervision, Methodology. YG: Conceptualization, Writing – review & editing, Data curation, Writing – original draft, Formal analysis, Methodology.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the 2023 Zhejiang Provincial Science and Technology Program of Traditional Chinese Medicine (No. 2024ZL977).
AcknowledgmentsWe are thankful to the authors who made detailed data available for this meta-analysis.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1499905/full#supplementary-material
References1. Xue, K, Palmer, MH, and Zhou, F. Prevalence and associated factors of urinary incontinence in women living in China: a literature review. BMC Urol. (2020) 20:159. doi: 10.1186/s12894-020-00735-x
PubMed Abstract | Crossref Full Text | Google Scholar
2. Haylen, BT, de Ridder, D, Freeman, RM, Swift, SE, Berghmans, B, Lee, J, et al. An international Urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. (2010) 29:4–20. doi: 10.1002/nau.20798
PubMed Abstract | Crossref Full Text | Google Scholar
3. Palmer, MH, Cockerell, R, Griebling, TL, Rantell, A, van Houten, P, and Newman, DK. Review of the 6th international consultation on incontinence: primary prevention of urinary incontinence. Neurourol Urodyn. (2020) 39:66–72. doi: 10.1002/nau.24222
PubMed Abstract | Crossref Full Text | Google Scholar
4. National Institute for Health and Care Excellence (NICE) in the United Kingdom. Urinary incontinence and pelvic organ prolapse in women: management. London: National Institute for Health and care excellence (NICE) (2019).
6. Wang, S, and Zhang, S. Simultaneous perineal ultrasound and vaginal pressure measurement prove the action of electrical pudendal nerve stimulation in treating female stress incontinence. BJU Int. (2012) 110:1338–43. doi: 10.1111/j.1464-410X.2012.11029.x
PubMed Abstract | Crossref Full Text | Google Scholar
7. Rautenberg, O, Zivanovic, I, Kociszewski, J, Kuszka, A, Münst, J, Eisele, L, et al. Current treatment concepts for stress urinary incontinence. Praxis. (2017) 106:829e–36e. doi: 10.1024/1661-8157/a002843
Crossref Full Text | Google Scholar
8. Dmochowski, RR, Sand, PK, Zinner, NR, Gittelman, MC, Davila, GW, Sanders, SW, et al. Comparative efficacy and safety of transdermal oxybutynin and oral tolterodine versus placebo in previously treated patients with urge and mixed urinary incontinence. Urology. (2003) 62:237–42. doi: 10.1016/s0090-4295(03)00356-x
PubMed Abstract | Crossref Full Text | Google Scholar
10. Li, Q-Q, Shi, G-X, Xu, Q, Wang, J, Liu, C-Z, and Wang, L-P. Acupuncture effect and central autonomic regulation. Evid Based Complement Alternat Med. (2013) 2013:267959:1–6. doi: 10.1155/2013/267959
PubMed Abstract | Crossref Full Text | Google Scholar
11. Liu, Z, Liu, Y, Xu, H, He, L, Chen, Y, Fu, L, et al. Effect of Electroacupuncture on urinary leakage among women with stress urinary incontinence: a randomized clinical trial. JAMA. (2017) 317:2493–501. doi: 10.1001/jama.2017.7220
PubMed Abstract | Crossref Full Text | Google Scholar
12. Sun, B, Liu, Y, Su, T, Sun, Y, and Liu, Z. Electroacupuncture for stress-related urinary incontinence in elderly women: data analysis from two randomised controlled studies. BMJ Support Palliat Care. (2022) 12:e164–70. doi: 10.1136/bmjspcare-2019-002034
PubMed Abstract | Crossref Full Text | Google Scholar
13. Chen, F, Zhou, J, Wu, W, and Qian, X. Study on the therapeutic effect of floating needle therapy combined with pressing acupoint embedding for female stress urinary incontinence after childbirth: a randomized trial. Ann Palliat Med. (2021) 10:7786–93. doi: 10.21037/apm-21-1382
PubMed Abstract | Crossref Full Text | Google Scholar
14. Kim, JH, Nam, D, Park, MK, Lee, ES, and Kim, SH. Randomized control trial of hand acupuncture for female stress urinary incontinence. Acupunct Electrother Res. (2008) 33:179–92. doi: 10.3727/036012908803861122
PubMed Abstract | Crossref Full Text | Google Scholar
15. Wang, Y, Zhishun, L, Peng, W, Zhao, J, and Liu, B. Acupuncture for stress urinary incontinence in adults. Cochrane Database Syst Rev. (2013) CD009408. doi: 10.1002/14651858.CD009408.pub2
Crossref Full Text | Google Scholar
16. Hargreaves, E, Baker, K, Barry, G, Harding, C, Zhang, Y, Kandala, N-B, et al. Acupuncture for treating overactive bladder in adults. Cochrane Database Syst Rev. (2022) 2022:CD013519. doi: 10.1002/14651858.CD013519.pub2
PubMed Abstract | Crossref Full Text | Google Scholar
17. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
PubMed Abstract | Crossref Full Text | Google Scholar
18. Smither, AR, Guralnick, ML, Davis, NB, and See, WA. Quantifying the natural history of post-radical prostatectomy incontinence using objective pad test data. BMC Urol. (2007) 7:2. doi: 10.1186/1471-2490-7-2
PubMed Abstract | Crossref Full Text | Google Scholar
19. Higgins, JPT, Altman, DG, Gøtzsche, PC, Jüni, P, Moher, D, Oxman, AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
PubMed Abstract | Crossref Full Text | Google Scholar
20. Zhang, TS, and Xiong, X. Meta-analysis methods for ordered data and their implementation using SAS. Evid Based Med. (2012) 12:125–8.
21. Tang, L, Zhai, X, Wang, P, and He, N. Proper application of the cumulative odds logit model in ordered data. J Xuzhou Med College. (2010) 30:577–9.
22. Luo, D, Wan, X, Liu, J, and Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res. (2018) 27:1785–805. doi: 10.1177/0962280216669183
PubMed Abstract | Crossref Full Text | Google Scholar
23. Wan, X, Wang, W, Liu, J, and Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14:135. doi: 10.1186/1471-2288-14-135
PubMed Abstract | Crossref Full Text | Google Scholar
24. Tang, K, Su, T, Fu, L, Chen, Z, Liu, G, Hou, W, et al. Effect of Electroacupuncture added to pelvic floor muscle training in women with stress urinary incontinence: a randomized clinical trial. Eur Urol Focus. (2023) 9:352–60. doi: 10.1016/j.euf.2022.10.005
PubMed Abstract | Crossref Full Text | Google Scholar
25. Xu, H, Liu, B, Wu, J, Du, R, Liu, X, Yu, J, et al. A pilot randomized placebo controlled trial of Electroacupuncture for women with pure stress urinary incontinence. PLoS One. (2016) 11:e0150821. doi: 10.1371/journal.pone.0150821
PubMed Abstract | Crossref Full Text | Google Scholar
26. Yu, C, Zhang, D, and Chen, C. Clinical observation of Electroacupuncture combined with pelvic floor muscle training in treating female stress urinary incontinence in 38 cases. J Jiangsu Univ Trad Chin Med. (2017) 49:51–3.
27. Wang, Q, Wang, J, and Wu, J. Clinical study on Electroacupuncture treatment for female stress urinary incontinence. World J Integrated Trad Western Med. (2021) 16:693–5. doi: 10.13935/j.cnki.sjzx.210420
Crossref Full Text | Google Scholar
28. Chen, Y. Observation on the therapeutic effect of acupuncture regulating Du-Ren method for female stress urinary incontinence. Modern J Integrated Trad Chin Western Med. (2020) 29:1517–21.
29. Qi, D, Liu, L, Liu, T, Hu, X, Zhao, J, Sun, X, et al. Observation on the therapeutic effect of acupuncture for female mild to moderate stress urinary incontinence. Shanghai J Acupunct Moxibust. (2022) 41:589–93. doi: 10.13460/j.issn.1005-0957.2022.06.0589
Crossref Full Text | Google Scholar
30. Chen, H, Li, B, Li, Y, and Zhang, C. Clinical study on the treatment of female stress urinary incontinence with floating needle combined with Kegel training. J Clin Acupunct Moxibust. (2021) 37:19–23. doi: 10.19917/j.cnki.1005-0779.021197
Crossref Full Text | Google Scholar
31. Deng, J, Feng, B, Chen, X, and Feng, S. Clinical observation on the treatment of female stress urinary incontinence with spleen-kidney yang deficiency by electro-warm needling at back shu points combined with pelvic floor muscle exercise. J Guangzhou Univ Trad Chin Med. (2020) 37:1485–90. doi: 10.13359/j.cnki.gzxbtcm.2020.08.014
Crossref Full Text | Google Scholar
32. Su, W, Zhong, W, and Tang, C. Clinical study on the treatment of female stress urinary incontinence with "Baliu acupoints" combined with Kegel exercises. Trad Chin Med Guide. (2019) 25:106–107+115. doi: 10.13862/j.cnki.cn43-1446/r.2019.06.030
Crossref Full Text | Google Scholar
33. Hou, W, Ming, S, Tang, K, Shen, R, and Chen, Y. Research on the therapeutic effect of electroacupuncture for mild and moderate female stress urinary incontinence. Shanghai J Acupunct Moxibust. (2017) 36:956–9. doi: 10.13460/j.issn.1005-0957.2017.08.0956
Crossref Full Text | Google Scholar
34. Cui, Y, Ma, Q, Zhang, Y, Wei, G, and Zhou, Z. The efficacy and safety of acupuncture in treating stress urinary incontinence in women from a Meta-analysis of four randomized controlled trials. Arch Esp Urol. (2023) 76:40–9. doi: 10.56434/j.arch.esp.urol.20237601.3
PubMed Abstract | Crossref Full Text | Google Scholar
35. Han, X, Shen, H, Chen, J, and Wu, Y. Efficacy and safety of electrical stimulation for stress urinary incontinence in women: a systematic review and meta-analysis. Int Urogynecol J. (2022) 33:789–99. doi: 10.1007/s00192-021-04928-2
PubMed Abstract | Crossref Full Text | Google Scholar
36. Wan, OYK, Cheung, RYK, Law, MPM, Lee, LL, Wang, RCC, and Chan, SSC. Effect of additional acupuncture to pelvic floor exercise on urinary incontinence: a randomized controlled trial. Neurourol Urodyn. (2022) 41:1097–108. doi: 10.1002/nau.24918
留言 (0)