Multiple sclerosis (MS) is a debilitating autoimmune chronic disease in which the immune system of the body attacks the myelin of nerve cells, causing permanent damage to nerves (1). Although a combination of genetic and environmental factors such as viral illnesses or stress can trigger the onset of the disease, the underlying cause of MS is still unknown (2). Epstein–Barr virus (EBV) infection, ultraviolet B light, obesity, vitamin D insufficiency and deficiency, and smoking are among the environmental factors that cause the disease to flare up (3).
The estimated rate of people affected with MS is 2.8 million around the world, of whom nearly a million live in America (4). A study on data obtained from Global Burden of Disease (GBD) in 2019 showed that 59,345 cases affected with MS, and 22,439 deaths happened due to this disease (5).
Women are three times more likely to develop MS compared with men (6). The prevalence of MS in the Iranian population has been reported to be 30 per 100,000, with a higher prevalence (44.8 per 100,000) among women (7).
MS is an unpredictable disease that presents with different signs and symptoms. The main factor that causes neurological symptoms in this disease is a decrease in the myelin of nerve endings in the brain and spinal cord, and therefore neuronal death and the neurological symptoms are much prevalent (8). The most prevalent symptoms include low vision, weak muscle reflex, movement difficulties, and decreased co-ordination (9).
Women with MS experience more stress urinary incontinence (SUI) and urgency urinary incontinence (UUI), both of which restrict their physical activity and negatively affect their quality of life (10). A systematic review of 12 studies showed that the prevalence of lower urinary tract symptoms was 68.4%, with increased urinary frequency as a dominant problem (11). A cross-sectional study on 602 Iranian MS patients showed that the prevalence of lower urinary tract symptoms was 87.6%. While this range did not show any difference between men and women, SUI was more prevalent among women than men (12).
The causes of urinary problems in women with MS may be attributed to detrusor overactivity, voiding dysfunction, and bladder involuntary contractions (13). The potential role of pelvic muscle weakness in urinary problem, however, is not clear. Some evidence shows that MS does not affect pelvic muscles (14). Contrary to this evidence, Lucio et al. in their study on MS women with lower urinary tract problems found that a muscle training intervention could significantly decrease overactive bladder, voiding symptoms, and stress incontinence, which will improve the quality of life (15). Also, the negative effect of urinary problems such as overactive bladder on quality of life has been proven in a previous study (16).
1.1 Research questionGiven the limited research in the relationship between pelvic muscle strength, urinary incontinence, and quality of life, we aimed to investigate this association in Iranian women with MS. Our hypothesis was that reduced pelvic muscle strength in women with MS would lead to urinary incontinence and decrease quality of life.
2 Materials and methodsThis cross-sectional study included 87 reproductive-aged women with MS. All consenting women with MS disease were recruited, excluding single women and those with severe physical disabilities. MS diagnosis was confirmed using the 2017 Revised McDonald criteria (17). Data collection started in March 2020 and completed in September 2020.
2.1 Ethics approval and consent to participateThe Ethics Committee of Ahvaz Jundishapur University of Medical Sciences approved the design of the study (Ref ID: IR.AJUMS.REC.1395.518). Before data collection written informed consent was obtained from all eligible women. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional or regional) and with the Declaration of Helsinki 1975, as revised in 2013.
2.2 SettingWe screened women according to inclusion/exclusion criteria in an MS clinic (located in the Rehabilitation Faculty of Ahvaz Jundishapur University of Medical Sciences) in Ahvaz, Khuzestan province, southwest of Iran. This center registers all MS patients in Khuzestan province. At time of data collection, 2,300 individuals suffering from MS were registered in the MS society of Khuzestan, of whom 400 were reproductive-aged women living in Ahvaz. Two hundred women were involved in other research projects, and only 87 out of the 200 remaining women provided consent to participate in the present study.
2.3 Data collection methodsData collection instruments were as follows: a demographic questionnaire, the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF), and the Quality of Life Questionnaire (QOL-SF-36). The demographic questionnaire inquired about age, length of marriage, number of pregnancies, body mass index, length of disease, marital status, mode of birth, educational attainment, occupation, and disease relapse were incorporated in the demographic questionnaire.
Urinary incontinence during the past 4 weeks was assessed using ICIQ-SF questionnaire. Two initial questions (Question 1 and 2) were about demographic characteristics (age and sex), Questions 3, 4, 5 and 6 were about frequency of urinary incontinence, urinary leakage, effect of urinary incontinence on quality of life, and the time of urinary leakage, respectively. The total score of this questionnaire is between zero and 21, with higher scores indicating worse urinary incontinence (18). Hajebrahimi et al. (19) validated this questionnaire in Iran.
The quality of life of the participants was assessed using QOL-SF-36. This questionnaire has 36 questions and 8 subscales. The subscales include physical function (10 questions), role limitations due to physical problems (4 questions), vitality, energy/fatigue (3 questions), social functioning (2 questions), role limitations due to emotional problems (3 questions), bodily pain (2 questions), general mental health (6 questions), and general health perception (6 questions). Each subscale is scored from zero to 100, with higher scores indicating better quality of life. This questionnaire has two major domains including the physical component summary (PCS) and the mental component summary (MCS) (20). This questionnaire was validated by Montazeri et al. (21) in Iran.
2.4 ProceduresEligible women were requested to complete the three questionnaires. In case the women had any question, one of the researchers (ST) was available to help them.
To measure the strengths of pelvic muscle, the women were first placed in the lithotomy position. A perineometer covered by a plastic cover (condom) was placed in the vagina. Then, women were requested to contract their vagina and the perineum with maximal effort. The peak force reading on the device was recorded, and this procedure was repeated two more times. The average of three measurements was recorded as final pelvic muscle strengths. All measurements were conducted by a single trained researchers (ST).
The weight of participants was measured using a digital scale (Seca, Germany made) while they were barefooted and wearing light clothing. The height of the participants was measured using a stadiometer while they were standing barefooted. Body mass index (BMI) was calculated using a formula of weight (kg)/height (m2).
2.5 Data analysisQualitative data were reported using frequency and percentages while quantitative data were reported using mean and SD. Pearson Correlation coefficient was used to examine the correlation of pelvic muscle strengths with urinary incontinence and quality of life. The relationship between pelvic muscle strengths, stress incontinence, and quality of life were assessed using multiple linear regression (adjusting for confounding variables). SPSS version 25 was used for data analysis. p < 0.05 was considered statistically significant.
3 ResultsAccording to our results, most of the participants were of the reproductive age and had been married for 10 years. The average number of pregnancies was two, and the mean of their BMI was 26.38 ± 2.32. The duration of MS disease was around 5 years, and the distribution of normal vaginal delivery and cesarean section were similar among participants. Most women (42.5%) were housewives with secondary high school education. The economic status of most participants was moderate. While most participants (50%) had no recurrence of the disease, 43.7% reported at least one recurrence (Table 1).

Table 1. Characteristics of women with MS disease.
The mean score of pelvic muscle strength was 21.03 ± 8.45. Data revealed that women who had normal vaginal delivery had the highest perineal strength (23.91 ± 9.12) followed by those women who underwent cesarean section (21.65 ± 7.95). Women who had normal vaginal delivery plus episiotomy had the weakest perineal muscle strength (16.68 ± 5.66) (Data are not shown in Tables).
The characteristics of urinary leakage in the study participants are illustrated in Table 2. A substantial number of women (63.2%) reported urinary leakage, which mostly (57.5%) happened with sneezing. Also, a considerable proportion (33.3%) reported that they experienced urinary leakage three times a week.

Table 2. Urinary leakage in the study participants (N = 87).
The scores of quality-of-life domains are presented in Table 3. As this table shows, the lowest scores were related to role limitations due to the emotional problems, physical functioning, and general health (43.65 ± 32.17, 48.51 ± 25.97, and 46.85 ± 13.66, respectively), while role limitations due to physical health had a higher score (67.60 ± 17.71).
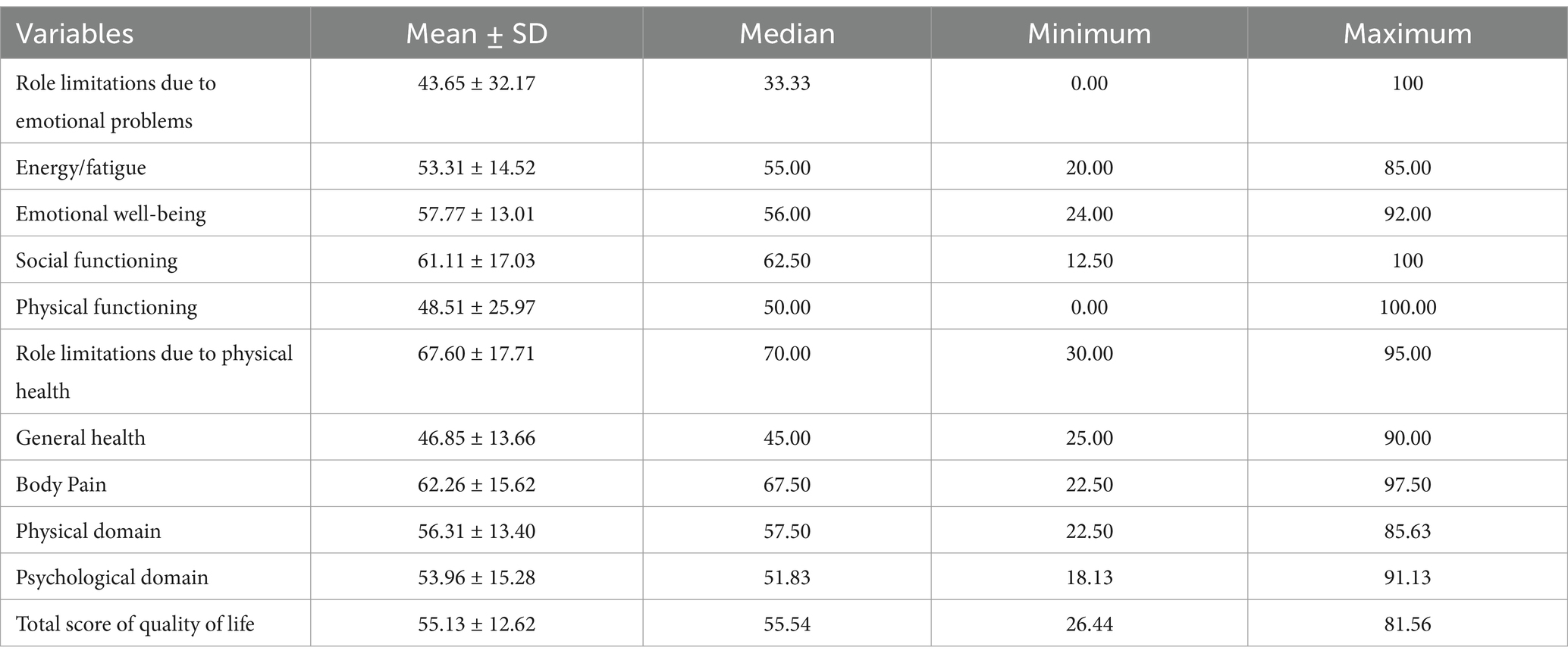
Table 3. The scores of quality of life and its subscales in women with multiple sclerosis (N = 87).
The Pearson Correlation coefficient was used to assess the correlation of pelvic muscle strength with urinary incontinence and quality of life. As Table 4 shows, pelvic muscle strength had a positive correlation with all domains of quality of life except for pain and role limitations due to emotional problems. There was an inverse significant correlation between urinary incontinence and all domains of quality of life except for pain (Table 4). An inverse correlation was also found between muscle strength and urinary incontinence (r = −0.838, p < 0.001) (Data are not shown in table).
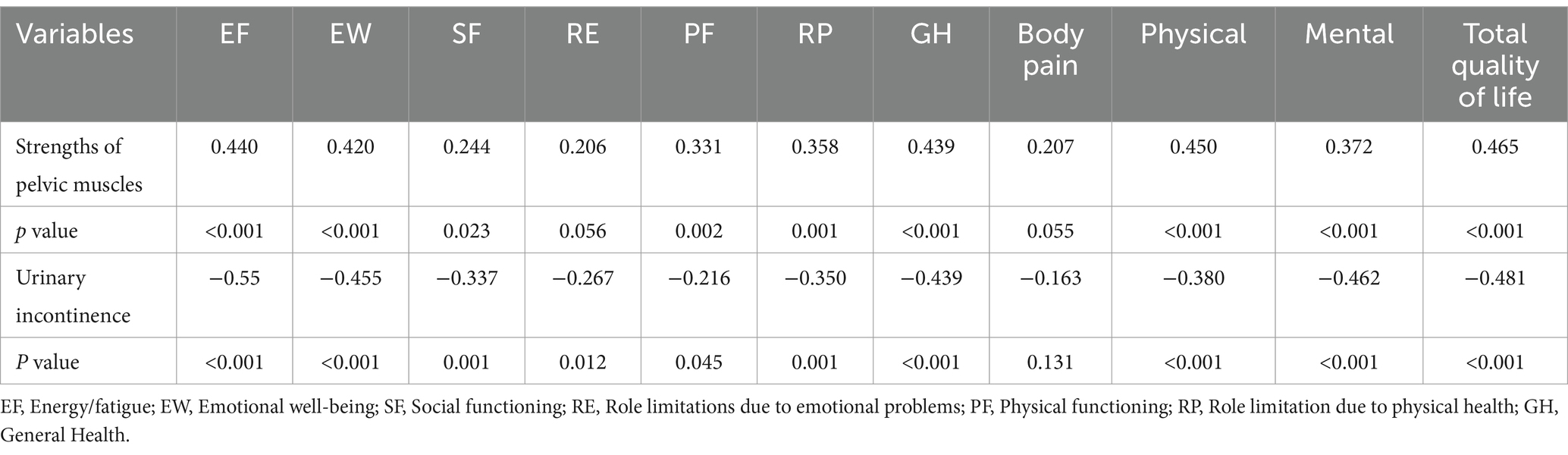
Table 4. Relationship between pelvic muscle strengths, urinary incontinence and quality of life.
The effect of physical and mental dimensions of quality of life on the strengths of pelvic floor muscles was assessed using the multiple linear regression (Table 5). As results indicated, a one-unit increase in the quality of physical life was associated with a 0.15-unit increase in the strength of pelvic floor muscles (p = 0.035). On the other hand, durations of marriage and the disease were inversely related to the strengths of the pelvic floor muscles. Also, a one-year increase in marriage duration was associated with a 0.24-unit decrease in strength (p = 0.027), while a one-year increase in disease duration was associated with a 0.509-unit decrease (p = 0.025). A one-unit increase in the number of normal vaginal deliveries was associated with a 4.072-unit increase in pelvic muscle strength, although this relationship did not reach statistical significant (p = 0.085).
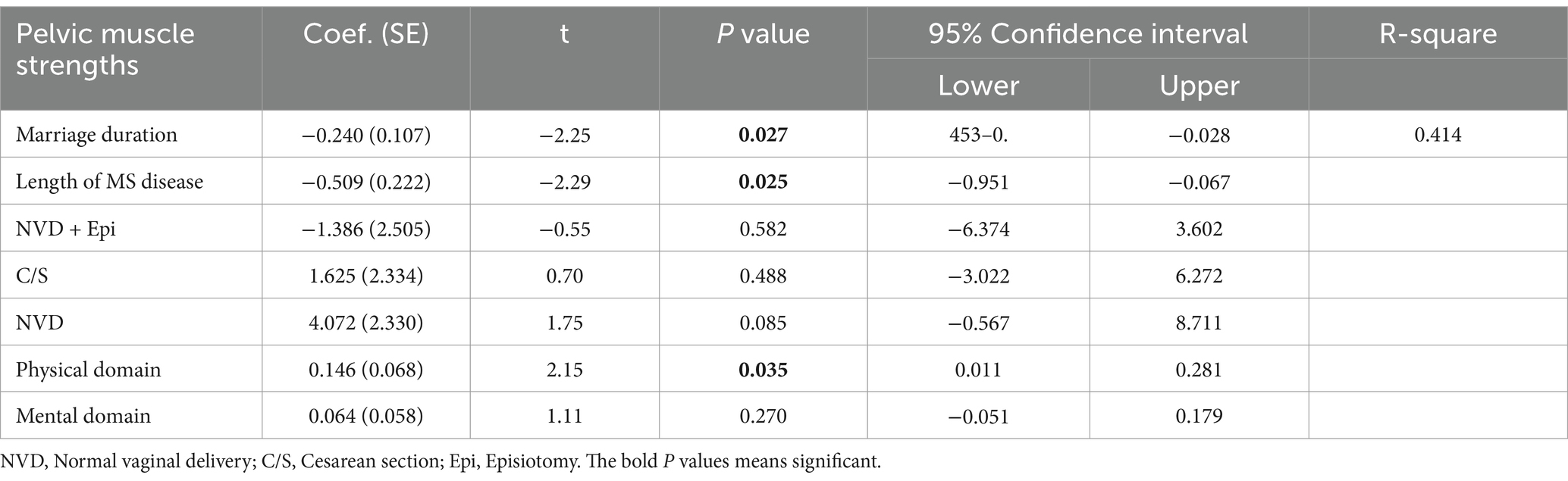
Table 5. Multiple linear regression for assessing pelvic muscle strength and urinary incontinence.
4 DiscussionThis study evaluated the relationship of pelvic muscle strength with urinary incontinence and quality of life in Iranian female MS patients. The results of this study indicated that the strengths of pelvic muscles decreased in these patients, with 63.2% of them reporting urinary leakage happening with sneezing.
Similar to our findings, Zeca et al. (22) reported a 35% prevalence of urinary incontinence in 403 MS patients, predominantly female (72%), with higher prevalence in disabled and female patients. Another study conducted in Iran on MS patients showed that the prevalence of overactive bladder among MS patients was 36.4% (23), which is much lower than that obtained in the present study. This discrepancy may be because in the present study we did not measure overactive bladder and we enrolled only female patients with MS disease, while in the above-mentioned study, both male and female patients were recruited.
In line with our results, Murphy et al. in their study on 143 female MS patients, found that 55.9% of their patients had stress urinary incontinence, 70.6% had urgency urinary incontinence, and 44.8% had mixed urinary incontinence (10). Our data showed an inverse correlation between muscle strength and urinary incontinence in MS patients. These results were confirmed by Mubaraki et al. (24) in their study on 150 MS patients, the results showed that the prevalence of urinary incontinence and overactive bladder were significantly higher in MS patients with progressive MS patients.
Our results showed that pelvic muscle strengths had a positive correlation with all domains of quality of life except for pain and role limitations due to emotional problems. Furthermore, urinary incontinence had a reverse significant correlation with all domains of quality of life except for pain. Evidence show that the performance and the strength of core muscles are significantly decrease in MS patients (14). Also, depression, fatigue, and low quality of life are prevalent among MS patients, which be improved if they have regular physical activity (25). Lucio et al. (15) found that both the strength of perineal muscles and the quality of life decreased in female patients with MS, and the urinary incontinence is prevalent among them. They showed that perineal muscle training for 12-week could significantly improve the overactive bladder, urinary incontinence, and quality of life.
The results of multiple linear regression in our study showed that by one-unit increase in the quality of physical life, the strength of pelvic floor muscles increased by 0.15 units. Other studies evaluated the relationship of physical functioning with pelvic muscle strength. For instance, McClurg et al. (26) studied 37 patients with MS disease and found that 9 weeks of pelvic muscle training using electromyography biofeedback could significantly increase pelvic muscle strengths and reduce the urinary incontinence. In their study, Mahajan et al. (27) on 9,397 patients with MS disease found that 41, 41, and 42% of females had urinary, bowel, and sexual problems which are all related to pelvic muscle weakness. Our results are similar with those of McClurg et al. (26) and Mahajan et al. (27).
Our results showed that with increasing the duration of marriage and of disease duration, the strength of the pelvic floor muscles was decreased. The reason for this matter is women with longer duration of marriage obviously are older and evidence shows that the motor discharge rate and muscle size decreased in MS patients, which might worsen with aging if patients do not have regular physical activity (28). The structural and functional changes in MS disease may resulted from changes in primary motor cortex (M1) in the cortical areas, that may enhance with using neuromodulatory techniques (29). A recent study showed that MS women need more time for rehabilitation using electrotherapy, that it may contributed to the weakness of muscle in women (30).
Our results showed that women with normal vaginal delivery had the highest pelvic strength followed by women who underwent cesarean section. Women who had normal vaginal delivery plus episiotomy had the weakest pelvic muscle strengths. Also, results of multiple linear regression showed that the mode of delivery does not have a significant effect on the strength of the pelvic floor muscles. However, according to the regression model, it seems that if the sample size was larger, women with normal vaginal delivery will show stronger pelvic muscles.
Although in the present study, we did not have a control group, we conducted a study on 341 healthy women in 2017 and measured the strengths of their pelvic muscles. The results showed that the highest pelvic muscle strengths were belong to nulliparous (55.62 ± 15.86 cm H2O) followed by women who had vaginal delivery with intact perineum (53.88 ± 20.9), women who underwent elective cesarean section (52.9 ± 21.29), and those underwent an emergency cesarean section (48.97 ± 21.04). Results indicated that women who had vaginal delivery with episiotomy had the weakest pelvic strength (32.71 ± 14 cm H2O) (31). Results of the present study are almost in line with the results of a study we did on healthy women, except for the fact that the pelvic muscle strength of women with MS is about half of that of healthy women.
However, other studies reported conflicting results. For example, Fang et al. in their study on 21,302 participants found that women with elective cesarean section had significantly rapid, tonic, and endurance contractions of perineal muscles compared to vaginal delivery (32). Furthermore, Jansson et al. (33) in a study found that women with vaginal delivery experienced more stress incontinence 1 year after childbearing. Both above-mentioned studies did not mention about whether women with vaginal delivery underwent episiotomy, and there was not results of relationship of parity and muscle strengths or urinary incontinence.
4.1 Strengths and limitations of studyThis is the first time that we evaluated the strengths of pelvic muscle with urinary incontinence and quality of life among Iranian women with MS disease. This study has some limitations. First, we did not recruit women randomly, and only 87 women who gave consent were recruited in this study, which may affect generalizability of the results. Second, we did not have a control group, that may limit the ability to contextualize the observed reduction in pelvic muscle strengths compared with healthy women. And finally, we did not assess the bowl function of women.
5 ConclusionThe results of this study showed that pelvic muscle strengths decreased in the women with MS disease, and it had a positive correlation with all domains of quality of life except for pain and role limitations due to emotional problems. Also, urinary incontinence had a reverse significant correlation with all domains of quality of life except for pain. An inverse correlation was also found between muscle strength and urinary incontinence. Pelvic floor muscle strength was inversely related to the duration of marriage and the length of MS disease. Health providers are recommended to educate MS patients about the importance of pelvic muscle strength.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Ref ID: IR.AJUMS.REC.1395.518). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsPoA: Conceptualization, Funding acquisition, Investigation, Methodology, Software, Supervision, Visualization, Writing – review & editing. PaA: Conceptualization, Formal analysis, Methodology, Resources, Software, Supervision, Writing – original draft, Writing – review & editing. NM: Conceptualization, Methodology, Supervision, Validation, Visualization, Writing – review & editing. ST: Conceptualization, Investigation, Methodology, Project administration, Resources, Visualization, Writing – review & editing. MH: Conceptualization, Data curation, Investigation, Software, Visualization, Writing – review & editing.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was a research project financially supported by Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
AcknowledgmentsWe would like to thank all women who participated in this study.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AbbreviationsMS, Multiple sclerosis; ICIQ-UI SF, International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form; QOL-SF-36, Quality of Life Questionnaire; EBV, Epstein–Barr virus; GBD, Global Burden of Disease; SUI, Stress urinary incontinence; UUI, Urgency urinary incontinence; PCS, Physical component summary; MCS, Mental component summary.
References2. Cree, BAC. Multiple sclerosis In: JCM Brust, editor. Current diagnosis and treatment in neurology. New York: Lange Medical Books/McGraw-Hill Medical (2007)
4. Walton, C, King, R, and Rechtman, L. Rising prevalence of multiple sclerosis worldwide: insights from the atlas of MS. Mult Scler J. (2020) 26:1816–21. doi: 10.1177/1352458520970841
PubMed Abstract | Crossref Full Text | Google Scholar
5. Qian, Z, Li, Y, Guan, Z, Guo, P, Zheng, K, Du, Y, et al. Global, regional, and national burden of multiple sclerosis from 1990 to 2019: findings of global burden of disease study 2019. Front Public Health. (2023) 11:1073278. doi: 10.3389/fpubh.2023.1073278
PubMed Abstract | Crossref Full Text | Google Scholar
6. Orton, S-M, Herrera, BM, Yee, IM, Valdar, W, Ramagopalan, SV, Sadovnick, AD, et al. Sex ratio of multiple sclerosis in Canada: a longitudinal study. Lancet Neurol. (2006) 5:932–6. doi: 10.1016/S1474-4422(06)70581-6
PubMed Abstract | Crossref Full Text | Google Scholar
7. Azimi, M, YektaKooshali, MH, Shohani, M, Khorshidi, A, and Mahmudi, L. Epidemiology of multiple sclerosis in Iran: a systematic review and meta-analysis. PLoS One. (2019) 14:e0214738. doi: 10.1371/journal.pone.0214738
PubMed Abstract | Crossref Full Text | Google Scholar
9. Koriem, KMM. Multiple sclerosis: new insights and trends. Asian Pac J Trop Biomed. (2016) 6:429–40. doi: 10.1016/j.apjtb.2016.03.009
Crossref Full Text | Google Scholar
10. Murphy, AM, Bethoux, F, Stough, D, and Goldman, HB. Prevalence of stress urinary incontinence in women with multiple sclerosis. Int Neurourol J. (2012) 16:86–90. doi: 10.5213/inj.2012.16.2.86
PubMed Abstract | Crossref Full Text | Google Scholar
11. Dandan, HBA, Coote, S, and McClurg, D. Prevalence of lower urinary tract symptoms in people with multiple sclerosis. Int J MS Care. (2020) 22:91–9. doi: 10.7224/1537-2073.2019-030
PubMed Abstract | Crossref Full Text | Google Scholar
12. Nazari, F, Shaygannejad, V, Mohammadi Sichani, M, Mansourian, M, and Hajhashemi, V. The prevalence of lower urinary tract symptoms based on individual and clinical parameters in patients with multiple sclerosis. BMC Neurol. (2020) 20:24. doi: 10.1186/s12883-019-1582-1
PubMed Abstract | Crossref Full Text | Google Scholar
14. Lourenco, GA, Nogueira, LAC, Rocco, R, Fragoso, YD, and Alves-Leon, SV. Multiple sclerosis does not affect the muscular strength of the pelvic floor during pregnancy a case control study. Multiple Scler. (2021) 49:102746. doi: 10.1016/j.msard.2021.102746
PubMed Abstract | Crossref Full Text | Google Scholar
15. Lucio, AC, Perissinoto, MC, Natalin, RA, Prudente, A, Damasceno, P, and Levi, D’a A. A comparative study of pelvic floor muscle training in women with multiple sclerosis: its impact on lower urinary tract symptoms and quality of life. Clinics. (2011) 66:1563–8. doi: 10.1590/S1807-59322011000900010
PubMed Abstract | Crossref Full Text | Google Scholar
16. Quarto, G, Autorino, R, Gallo, A, De Sio, M, D'Armiento, M, Perdonà, S, et al. Quality of life in women with multiple sclerosis and overactive bladder syndrome. Int Urogynecol J Pelvic Floor Dysfunct. (2007) 18:189–94. doi: 10.1007/s00192-006-0131-9
PubMed Abstract | Crossref Full Text | Google Scholar
17. Tgompson, AJ, Banwell, BL, Barkhof, F, Carrol, WM, Coetzee, T, Comi, G, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. (2018) 17:162–73. doi: 10.1016/S1474-4422(17)30470-2
PubMed Abstract | Crossref Full Text | Google Scholar
18. Avery, K, Donovan, J, Peters, TJ, Shaw, C, and Gotoh, M. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. (2004) 23:322–30. doi: 10.1002/nau.20041
PubMed Abstract | Crossref Full Text | Google Scholar
19. Hajebrahimi, S, Nourizadeh, D, Hamedani, R, and Pezeshki, MZ. Validity and reliability of the international consultation on incontinence questionnaire-urinary incontinence short form and its correlation with urodynamic findings. Urol J. (2012) 9:685–90.
PubMed Abstract | Google Scholar
20. Ware, JE, and Sherbourne, CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. (1992) 30:473–83. doi: 10.1097/00005650-199206000-00002
Crossref Full Text | Google Scholar
21. Montazer, A, Goshtasebi, A, Vahdaninia, M, and Gandek, B. The short form health survey (SF-36): translation and validation study of the Iranian version. Qual Life Res. (2005) 14:875–82. doi: 10.1007/s11136-004-1014-5
PubMed Abstract | Crossref Full Text | Google Scholar
22. Zeca, C, Riccitelli, GC, Disanto, G, Singh, A, Digesu, GA, Panicari, L, et al. Urinary incontinence in multiple sclerosis: prevalence, severity and impact on patients' quality of life. Eur J Neurol. (2016) 23:1228–34. doi: 10.1111/ene.13010. Epub 2016 Apr 27
PubMed Abstract | Crossref Full Text | Google Scholar
23. Azadvari, M, Emami Razavi, SZ, Shahrooei, M, Moghadasi, AN, Azimi, A, and Farhadi-Shabestani, HR. Bladder dysfunction in Iranian patients with multiple sclerosis. J Multidiscip Healthc. (2020) 13:345–9. doi: 10.2147/JMDH.S244697
PubMed Abstract | Crossref Full Text | Google Scholar
24. Mubaraki, AA, Alnemari, MA, Aljuaid, SO, Altalhi, FM, Alamri, YM, and Altowairqi, SO. The prevalence and impact of urinary incontinence on multiple sclerosis patients in Taif City, Saudi Arabia. Cureus. (2024) 16:e57010. doi: 10.7759/cureus.57010
PubMed Abstract | Crossref Full Text | Google Scholar
25. Dalgas, U, Stenager, E, Jakobsen, J, Petersen, T, Hansen, HJ, Knudsen, C, et al. Fatigue, mood and quality of life improve in MS patients after progressive resistance training. Multiple Scler J. (2010) 16:480–90. doi: 10.1177/1352458509360040
PubMed Abstract | Crossref Full Text | Google Scholar
26. McClurg, D, Lowe-Strong, A, and Ashe, RG. The benefits of pelvic floor muscle training in people with multiple sclerosis and lower urinary tract dysfunction. J Assoc Chart Physiother Womens Health. (2008) 103:21–8.
27. Mahajan, ST, James, R, and Frasure, H. Pelvic floor disorders and multiple sclerosis: are patients satisfied with their care? Int J MS Care. (2014) 16:20–5. doi: 10.7224/1537-2073.2012-052
PubMed Abstract | Crossref Full Text | Google Scholar
29. Nardone, R, Versace, V, Sebastianelli, L, Brigo, F, Golaszewski, S, Christova, M, et al. Transcranial magnetic stimulation and bladder function: a systematic review. Clin Neurophysiol. (2019) 130:2032–7. doi: 10.1016/j.clinph.2019.08.020
PubMed Abstract | Crossref Full Text | Google Scholar
30. Altunan, B, Gundogdu, AA, Ozcaglayan, TIK, Unal, A, and Turgut, N. The effect of pelvic floor exercise program on incontinence and sexual dysfunction in multiple sclerosis patients. Int Urol Nephrol. (2021) 53:1059–65. doi: 10.1007/s11255-021-02804-y
PubMed Abstract | Crossref Full Text | Google Scholar
31. Afshari, P, Dabagh, F, Iravani, M, and Abedi, P. Comparison of pelvic floor muscle strength in nulliparous women and those with normal vaginal delivery and cesarean section. Int Urogynecol J. (2017) 28:1171–5. doi: 10.1007/s00192-016-3239-6
PubMed Abstract | Crossref Full Text | Google Scholar
32. Fang, J, Ye, J, Huang, Q, Lin, Y, Weng, Y, and Wang, M. Risk factors of pelvic floor muscle strength in south Chinese women: a retrospective study. BMC Pregnancy Childbirth. (2022) 22:624. doi: 10.1186/s12884-022-04952-0
PubMed Abstract | Crossref Full Text | Google Scholar
33. Jansson, MH, Franzén, K, Tegerstedt, G, Hiyoshi, A, and Nilsson, K. Stress and urgency urinary incontinence one year after a first birth—prevalence and risk factors a prospective cohort study. AOGS. (2021) 100:2193–201. doi: 10.1111/aogs.14275
留言 (0)