Sexually transmitted infections (STIs) represent a persistent and substantial public health challenge, affecting millions of people both in Brazil and globally (1). Estimates indicate that approximately 360 million cases of STIs occur worldwide each year, with 10 to 12 million cases registered in Brazil (2). Previous studies have shown that the burden of STIs is disproportionately high among adolescents and young adults, with higher rates observed in specific regions and populations (3, 4), underlining the importance of preventive strategies tailored to these groups. These data underscore the need for effective strategies for the prevention and control of these diseases, especially among young people and college students, who are among the most vulnerable groups (5).
Risky sexual behaviors, such as engaging in unprotected sex, having multiple partners, and drug use, play a fundamental role in the spread of STIs, particularly among adolescents and young adults aged 15 to 24 (6). These behaviors are influenced by a complex interaction of social, cultural, psychological, and biological factors that shape the maturation process and are closely related to the university environment (7). Studies have shown that the university environment often contributes to a sense of anonymity and freedom, which can lead to risky behaviors such as multiple sexual partners (8) and alcohol use (8–10). Furthermore, peer pressure and the desire for social acceptance are commonly cited as significant factors influencing these behaviors among young adults (11).
The university academic setting, characterized by greater individual freedom and changes in social interactions, often creates an atmosphere conducive to the emergence and consolidation of risky behaviors, such as alcohol consumption (9) and unprotected sex (5, 7). This vulnerability is exacerbated by inadequate preparation to deal with sexuality-related issues and insufficient knowledge of the topic (2, 6, 12). Investigations into medical students’ knowledge of sexual health revealed significant gaps in understanding about STIs transmission and prevention (13, 14). Despite being exposed to comprehensive medical curricula, many students report feeling unprepared to address sexual health topics effectively in clinical practice (15, 16).
In addition to individual vulnerability, it is also important to consider that health students bear an even greater responsibility, as they may be tasked with guiding the public on sexual and reproductive health during their training. This underscores the need for a consistent and early understanding of these issues. However, despite having access to extensive educational resources, medical students often struggle to translate their knowledge into safer behaviors (17–19). Previous studies have highlighted the discrepancy between medical students’ knowledge of sexual health and their actual clinical practices (14, 20). This gap between theoretical knowledge and practical behavior becomes a critical point of investigation, particularly for future doctors, who will be responsible for disseminating knowledge and promoting preventive practices.
Given the relevance of this topic and the pressing need to understand and address the factors contributing to the risky sexual behaviors of these future doctors, the present study aimed to describe the sexual behavior of medical students, analyze their sociodemographic profile, and assess their level of knowledge about HIV/AIDS and other STIs. The study also sought to identify potential correlations between knowledge and risky behaviors, with the goal of contributing to the development of more targeted and effective preventive interventions for this audience.
2 Methods 2.1 Study designA cross-sectional study was conducted from March 25 to May 25, 2021, in the city of Salvador, Bahia, Brazil.
2.2 Population and sampleThe target population consisted of medical students from a private higher education institution in Brazil.
The study sample included students from the first, third, and sixth years of the medical course, aged over 18, who were officially enrolled. This selection was intentional, aiming to evaluate the progression of knowledge about risky sexual behavior across the three academic cycles: basic (1st to 4th semesters), clinical (5th to 8th semesters), and internship (9th to 12th semesters). Students who reported not having had sexual relations at the time of the survey or provided incomplete responses to the questionnaire were excluded from the analysis.
The sample size was estimated considering a target population of 900 students enrolled at the institution. To ensure a 95% confidence level and a 5% margin of error, the sample size was estimated at 194 students, ensuring the statistical robustness needed for data analysis. Ultimately, 213 responses were obtained, representing a response rate of 23.7%, surpassing the initially estimated sample size and reinforcing the statistical validity of the results.
2.3 Procedures and measurementsData collection was conducted through a structured, anonymous, self-administered virtual questionnaire created using Google Forms. All enrolled students were invited to participate via an email invitation containing the link to access the questionnaire. The invitation was sent to the students’ institutional email, which is generated by the university upon enrollment. At this institution, each academic semester is associated with a specific institutional email list, which includes the email addresses of all students enrolled in that semester. As a result, an informational email with the questionnaire link was sent to each of these addresses, ensuring that the entire student body had access to the invitation to participate. Before accessing the questionnaire, students were required to provide formal consent via the Informed Consent Form (ICF) available on the form’s homepage.
Data collection was based on a questionnaire adapted from two previous studies: the Knowledge, Attitudes, and Practices Survey of the Brazilian population (PCAP) (21) and the Survey on Risk Behavior and Knowledge in University Students (19). The PCAP is a survey validated by the Brazilian Ministry of Health and is widely used to assess behavior and knowledge regarding STIs in Brazil (21). Since it has five independent sections that can be analyzed separately, it does not require a validation process for its adaptation (21). In this study, only sections 1 (socioeconomic conditions), 2 (knowledge of HIV/AIDS and other STI transmission), and 5 (drug use and sexual practices) were used.
The questionnaire comprised 39 objective questions, covering sociodemographic aspects (questions 1 to 8), STI transmission methods (questions 9 to 18), sexual behavior (questions 19 to 23), sexual experiences in the past 12 months (questions 24 to 34), and the use of licit and illicit drugs during sexual relations (questions 35 to 39).
To assess social, cultural, and economic aspects, data were collected on sex, age, marital status, religion, family income, and the educational level of both the family and the student.
Regarding the evaluation of sexual behavior, risky behavior was defined as the lifetime practice of two or more of the following sexual behaviors: (I) inconsistent condom use; (II) more than 10 sexual partners; (III) sexual intercourse after alcohol consumption; (IV) sexual intercourse after illicit substance use; and (V) sexual intercourse with a person little known or recently acquainted (22).
Knowledge about STIs and HIV/AIDS was assessed based on responses to questions 9 to 18. For each question, answers were classified as correct or incorrect according to a predefined standard. The option “I do not know” was treated as an incorrect response. Additionally, the level of knowledge was categorized into three levels: “good” (above 70% correct), “average” (50–70% correct), and “poor” (below 50% correct) (23).
2.4 Statistical analysisData were tabulated in Microsoft Excel and analyzed using IBM SPSS Statistics, version 25.0.
The data analysis employed both descriptive and inferential statistics. Continuous variables were expressed as means and standard deviations (M ± SD), and categorical variables as absolute and relative frequencies.
To verify the association between (I) knowledge level and student profile, (II) knowledge level and sexual behavior, and (III) sexual behavior and student profile, the chi-square test was applied. When the expected count in one or more cells of the contingency table was less than five, Fisher’s exact test was used. Associations were considered statistically significant at p < 0.05.
Additionally, Cramér’s V coefficient was calculated to assess the strength of the observed associations. Cramér’s V was interpreted according to conventional values: <0.1 indicated a weak association, between 0.1 and 0.3 indicated a moderate association, and > 0.3 indicated a strong association.
2.5 Ethical considerationsThis study was conducted in accordance with Resolutions 466/12 and 510/16 of the National Health Council. The project was approved by the Research Ethics Committee of the Bahiana School of Medicine and Public Health (protocol no. 40394920.3.0000.5544, report no. 4.612.617). The autonomy, confidentiality, and privacy of the participants were carefully maintained throughout the study. Data confidentiality and participant privacy were ensured by restricting access to information exclusively to the researchers involved. All study participants were fully informed about the research objectives and methods and provided their consent by digitally signing the ICF.
3 ResultsOut of the 213 responses, 20 were excluded as they came from students who had not yet initiated sexual activity, leaving a final sample of 193 medical students. No incomplete questionnaires were identified. Among these, there was a predominance of third-year medical students (69.4%), with a mean age of 22.3 ± 3.4 years. The majority were female (70.5%), single (92.2%), and non-religious (56.5%); among those who practiced a religion, Catholicism was the most prevalent (57.1%). Most students had no prior academic training (87.0%) and belonged to families with an income exceeding 10 minimum wages (58.0%; Table 1).
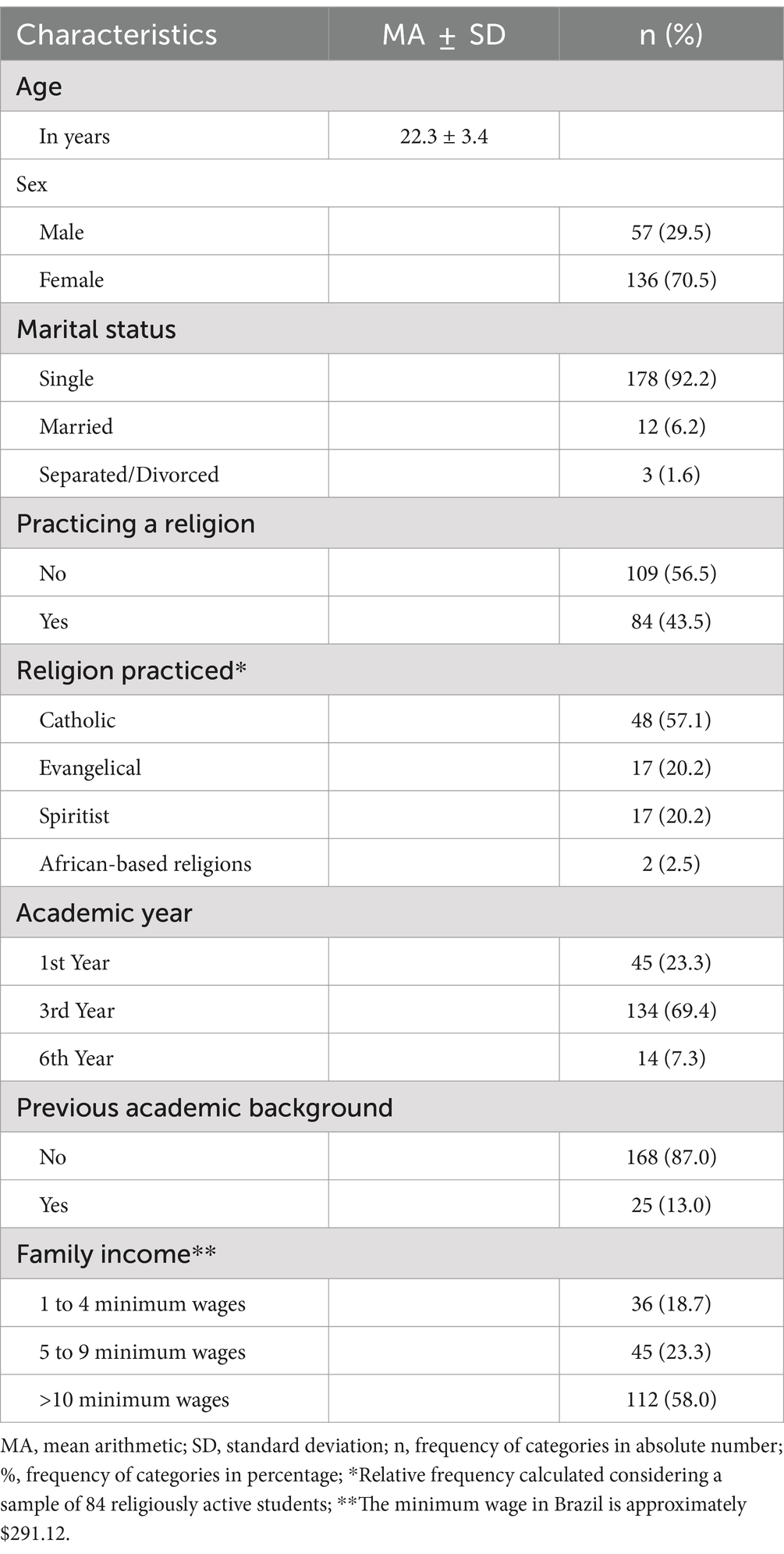
Table 1. Sociodemographic characteristics of study participants (n = 193).
3.1 Sexual behavior of studentsAmong medical students who had initiated their sexual activity, 77.7% reported risky sexual behaviors. The first sexual intercourse occurred, on average, at 17.3 ± 2.4 years, with 72.0% reporting condom use at that time. Furthermore, 79.3% stated that they had had fewer than 10 sexual partners up to that point, and 69.8% used condoms during their last sexual encounter. However, 67.4% of the students had not engaged in sexual activity in the past 12 months. Among those who maintained a steady partner during this period (64.8%), 63.2% did not use condoms during their last encounter, and among those who did use condoms, 50.0% did not use them consistently. Among students without a steady partner, 69.8% used condoms in casual encounters in the past 12 months, but only 38.6% used them consistently. Additionally, 29.0% of students reported having sexual relations with individuals met online, and 32.6% engaged in sexual activity under the influence of substances such as alcohol (70.5%), marijuana (23.8%), cigarettes (18.7%), crack (1.0%), or cocaine (1.0%; Table 2).
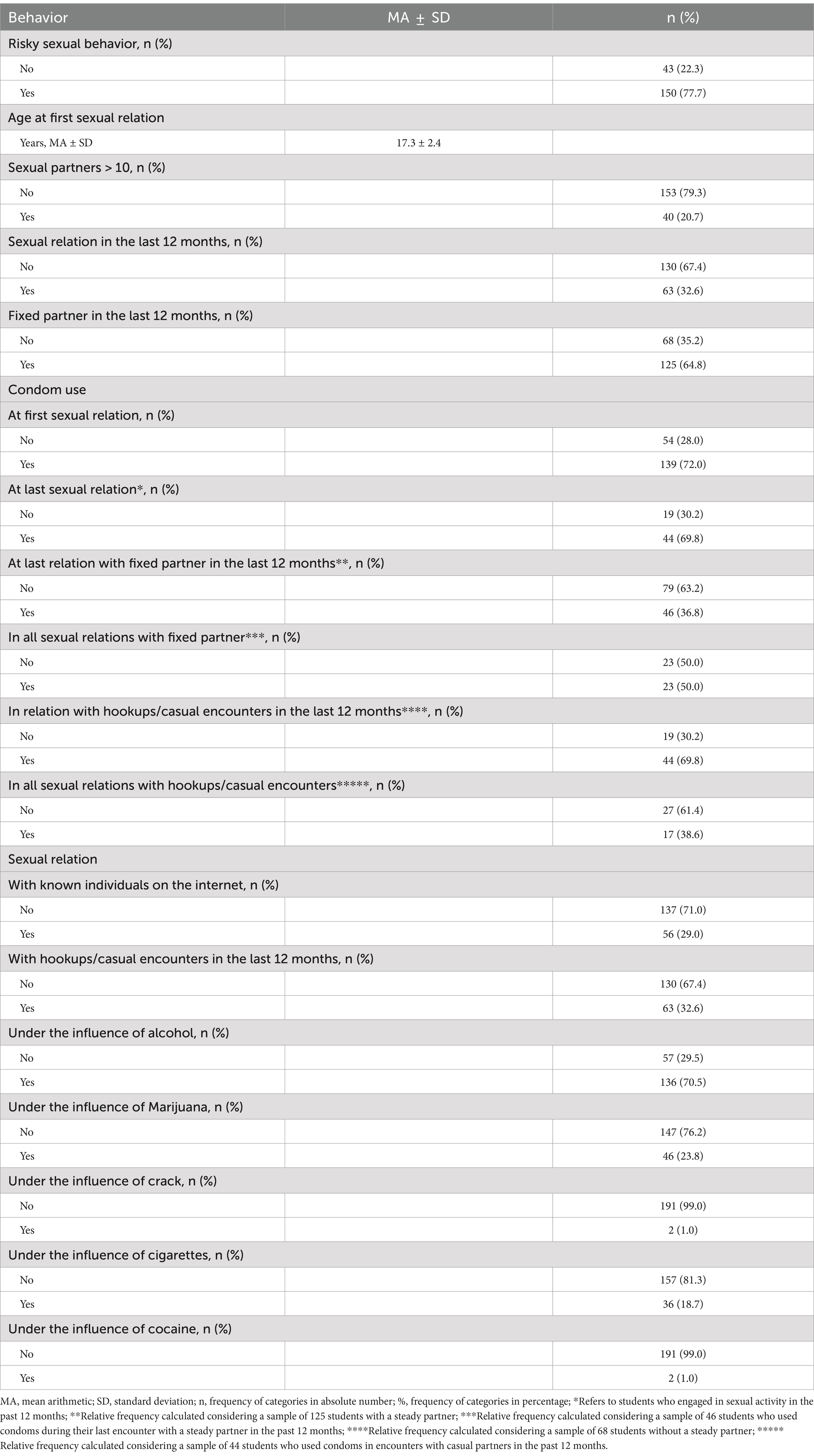
Table 2. Sexual behavior of study participants (n = 193).
3.2 Association between sexual behavior and student profileSignificant associations were found between risky sexual behaviors and various characteristics of the medical students’ profile. A strong correlation was noted between the number of sexual partners (p = 0.0001, Cramer’s V = 0.265), engaging in sexual activity in the past 12 months (p = 0.001, Cramer’s V = 0.519), and the absence of a steady partner (p = 0.001, Cramer’s V = 0.519), with an increase in other risky behaviors. Moreover, condom use proved to be a relevant factor, with a significant association between the absence of condom use during the last sexual encounter with a steady partner and other risky sexual behaviors (p = 0.0001, Cramer’s V = 0.234). Statistically relevant correlations were also identified between risky sexual behavior and the use of substances such as alcohol (p = 0.0001, Cramer’s V = 0.363), marijuana (p = 0.0001, Cramer’s V = 0.300), and cigarettes (p = 0.0001, Cramer’s V = 0.256) during sexual encounters. Other factors, such as gender, marital status, family income, academic profile, and religious practice, did not present significant associations (Table 3).

Table 3. Association between sexual behavior and the sociodemographic profile of study participants (n = 193).
3.3 Level of knowledge of students about STIs and HIV/AIDSWhen analyzing the level of knowledge about STIs and HIV/AIDS among all participants in the study, it was observed that the majority of students had knowledge classified as poor (49.2%) or fair (48.7%). This pattern remained consistent regardless of sexual behavior, with most students who engaged in risky behaviors classified as having poor (47.3%) or fair (50.7%) knowledge; similarly, those who did not exhibit risky sexual behaviors were also predominantly classified as having poor (55.8%) or fair (41.9%) knowledge, suggesting that while the level of knowledge is important, it did not appear to be the sole determining factor in the adoption of risky behaviors (Table 4).
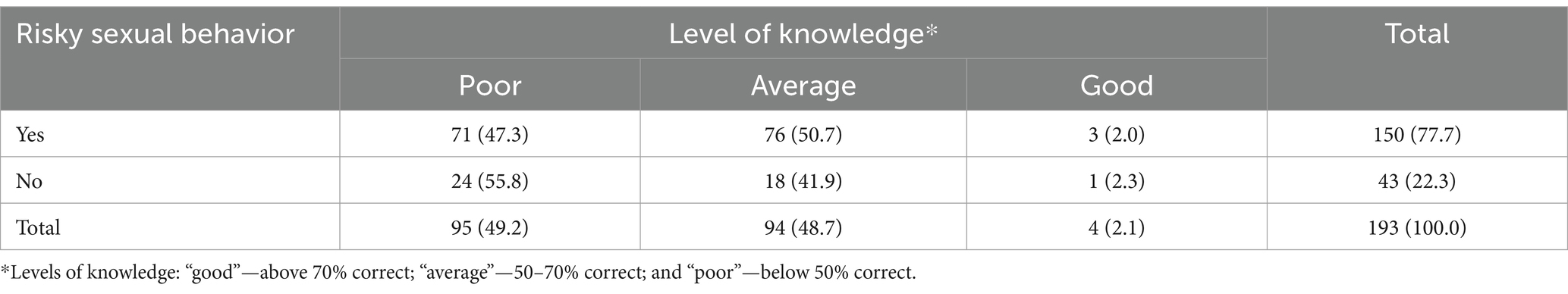
Table 4. Knowledge level of study participants about STIs and HIV/AIDS according to their sexual behavior (n = 193).
The analysis of the content addressed revealed that questions related to HIV/AIDS transmission, such as the use of condoms to prevent transmission and the fact that seemingly healthy individuals may be infected, had high correct response rates (96.9 and 98.4%, respectively). However, misconceptions persist, such as the transmission of diseases through not using condoms during sexual relations or sharing syringes or needles with others (99.9 and 97.9% incorrect responses, respectively) and regarding diseases that have a cure (83.4% incorrect responses), indicating significant knowledge gaps (Table 5).
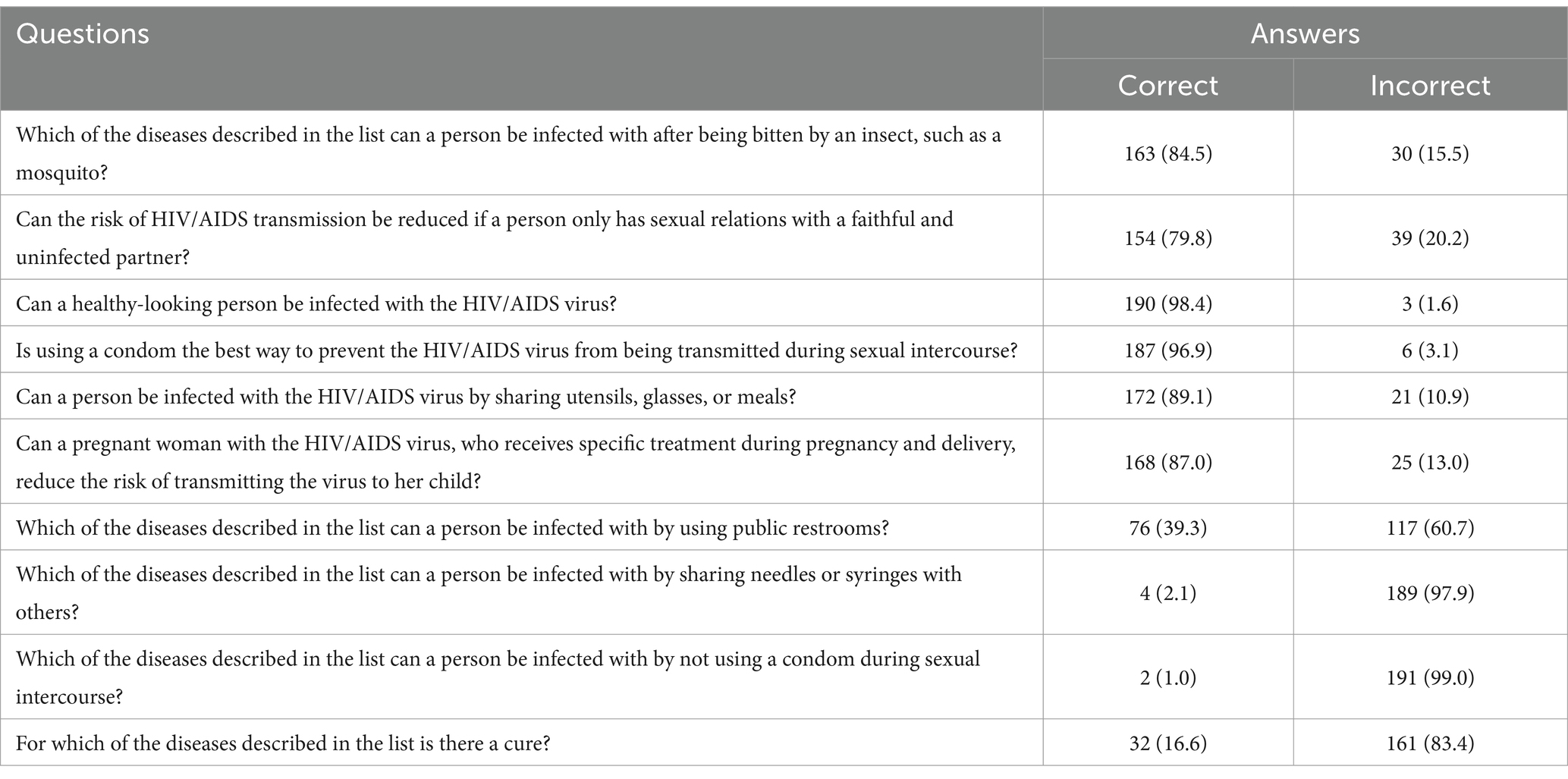
Table 5. Evaluation of knowledge about STIs and HIV/AIDS among study participants (n = 193).
3.4 Association between level of knowledge about STIs and HIV/AIDS and student profileThe analysis of the association between the level of knowledge about STIs and HIV/AIDS and the profile of medical students revealed no significant associations in most of the evaluated variables, except for the non-use of condoms in encounters with casual partners in the past 12 months (p = 0.021, Cramer’s V = 0.350). Individuals with lower knowledge levels used condoms less frequently (Table 6).
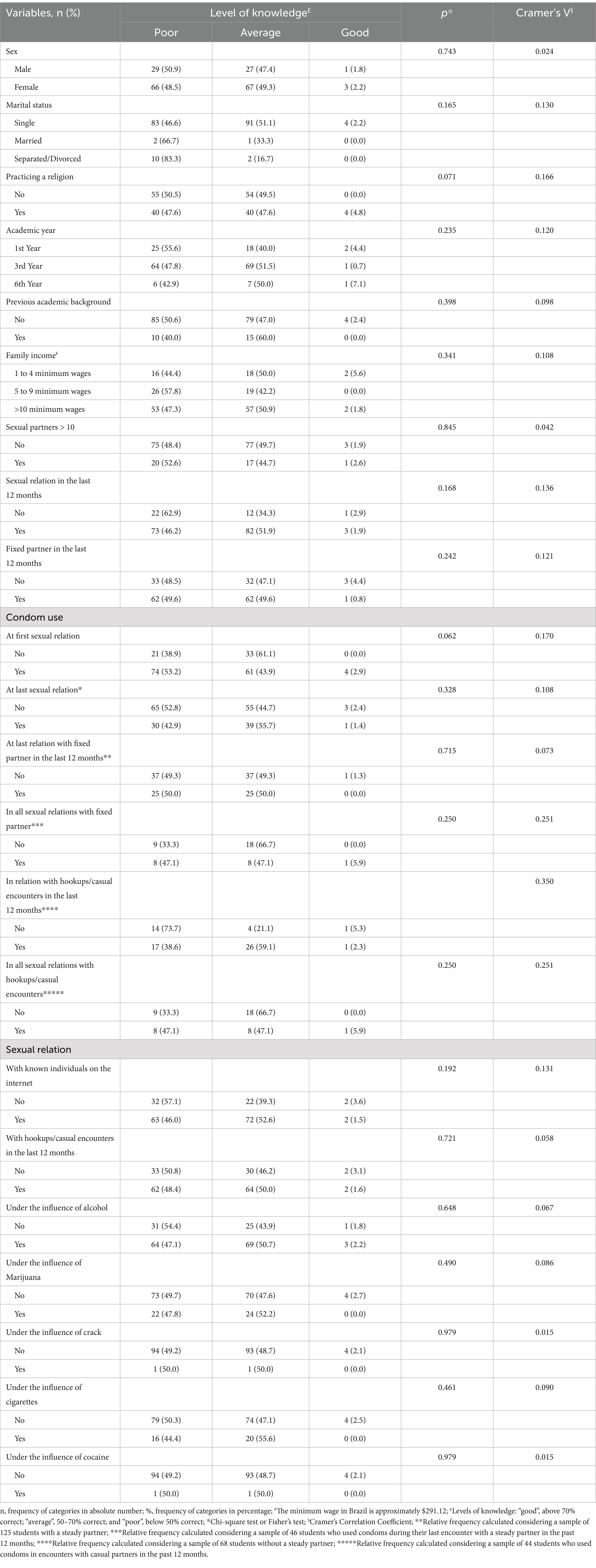
Table 6. Association between the level of knowledge about STIs and HIV/AIDS and the profile of study participants (n = 193).
4 DiscussionThe present research revealed a high prevalence of inadequate knowledge about STIs and HIV/AIDS among the medical students participating in the study. This deficit is particularly concerning, considering the crucial role these future professionals will play in promoting health and preventing these diseases within the population.
The lack of knowledge about STIs and HIV/AIDS among medical students has also been demonstrated in other international studies (24–29). This knowledge gap is not only prevalent in developed countries but also in resource-limited settings, where there is often a lack of comprehensive sexual health education in medical curricula (25). The literature shows that inadequate and outdated information contributes to the perpetuation of myths and stigmas associated with STIs, which can result in sexual risk behaviors that compromise individual and collective health, as well as negatively impact the care of patients with HIV/AIDS and other STIs (25). Furthermore, it is necessary an integrated, multidisciplinary approach to sexual health education that spans the entire medical curriculum, ensuring that medical students not only acquire knowledge but also the skills to apply it in practice (24). This knowledge gap may reflect not only a lack of sexual education but also the absence of comprehensive curricular content. Moreover, it highlights the need for an integrated and multidisciplinary approach that transcends disciplines directly related to sexual health and permeates the entire medical curriculum (24).
Previous studies indicate that sociodemographic profiles can influence the adoption of risk behaviors, especially among young adults who are in a transitional phase characterized by greater independence and maturation. For instance, studies have shown that gender, sexual orientation, and cultural background can influence attitudes toward sexual health and the adoption of preventive behaviors (7, 22, 30, 31). Evidence suggests that among university students, women, despite having greater knowledge about STIs (7, 22), married individuals or those cohabiting with partners (32), people with lower socioeconomic status32, and those with higher levels of religiosity (30, 31) are more susceptible to sexual risk behaviors, such as inconsistent use of prevention methods, whether due to personal beliefs or inadequate sexual education. However, the present study did not demonstrate significant associations between the sociodemographic profile of participants and sexual risk behaviors, suggesting that other factors, such as social and academic contexts, may play a more relevant role in determining these practices. These results indicate the need to explore in future studies how different factors interact to influence sexual risk behavior among medical students.
When analyzing the sexual behavior of students, this study revealed that most exhibited some form of sexual risk behavior, particularly regarding inconsistent condom use in both stable and casual relationships. It was observed that condom use is considerably lower in stable relationships, corroborating the findings of other studies (32, 33). The inconsistency in condom use, particularly in stable relationships, is a significant risk factor since, even in monogamous relationships, there is always the possibility of exposure to STIs due to multiple factors, such as infidelity and lack of regular testing (34). In various countries, the adoption of sexual risk behaviors is often associated with negligence in adopting barrier methods in stable relationships, reflecting a false sense of security (35). These data suggest the need for interventions that promote awareness of the importance of consistent condom use, regardless of the type of relationship, as an essential part of a broader STI prevention strategy.
Another important point is that alcohol consumption (10) and the use of legal and illegal drugs (36), as well as the influence of the internet (37), have been identified as factors contributing to the adoption of sexual risk behaviors among youth. Studies indicate that alcohol consumption, which is more prevalent among men, is associated with the use of other psychoactive substances and engagement in sexual risk behaviors, such as lack of condom use and increased number of sexual partners. In this study, the majority of male individuals demonstrated sexual risk behavior and reported having sexual relations under the influence of alcohol, corroborating existing literature (10, 36). Additionally, the virtual environment and the use of dating apps have played an increasing role in facilitating sexual encounters (37), influencing the adoption of sexual risk behaviors and increasing exposure to STIs. The rise of online platforms for meeting potential sexual partners has been recognized as both a risk and an opportunity, as these platforms often promote risky sexual behaviors but can also be utilized for educational outreach (38).
Comparing the results of this study with research conducted in other countries, a similar trend in sexual risk behavior among medical students can be observed (26, 27, 29, 39). These findings reinforce the idea that, despite cultural and regional differences, medical students in various parts of the world are equally exposed to factors that make them vulnerable to risk behaviors, just like others in the same age group. This cross-cultural similarity suggests that medical curricula worldwide should address sexual health in a more comprehensive and context-specific manner (24). One of the main challenges for changing sexual behavior among medical students may be related to the dynamics of medical training itself. The intense workload, academic pressure, and lack of time to engage in educational activities can hinder awareness and the adoption of a healthy lifestyle and preventive practices. Studies have consistently shown that the demanding nature of medical education can lead to stress, burnout, and a reduction in the time available for engaging in health-promoting behaviors (40, 41). Furthermore, the institutional culture may not sufficiently value the importance of early sexual health education, contributing to students failing to recognize the seriousness of adopting risk behaviors. Therefore, it is essential for educational institutions to create spaces for debate and ongoing education on these topics, promoting a change in academic culture and reducing the vulnerability common in the studied age group. The implementation of pedagogical strategies that integrate interactive practices and real-life experiences, such as clinical simulations, debates, and workshops focused on awareness and prevention of STIs, may be useful in this process.
Such approaches can encourage students to reflect on their own sexual practices and reinforce preventive attitudes, as well as prepare them to interact with patients in a more empathetic and informed manner. This curricular reform, by combining theory and practice, has the potential to not only improve the knowledge of future doctors but also develop on psychoaffective skills, and in the long term, may contribute to reducing the rates of STI and HIV/AIDS transmission in society.
Finally, one of the main limitations of this study is its cross-sectional design, which prevents the establishing causal relationships between the analyzed factors and sexual risk behaviors. Furthermore, the use of self-administered questionnaires may have led to response bias, as participants may have underestimated their behaviors due to the sensitive nature of the topic. Another relevant limitation is that the sample consisted exclusively of medical students from a single institution, which may limit the generalization of results to other academic populations and regional contexts. Additionally, the data for this study were collected during the COVID-19 pandemic, a period marked by behavioral restrictions that could have influenced social interactions and sexual practices. Therefore, the results of this study should be interpreted in light of the context in which the data were collected. Future studies should consider more diverse samples and methodological approaches further explore the variables involved. Despite these limitations, this study contributes significantly to the field of medical education by identifying a knowledge gap regarding STIs and sexual risk behaviors among future physicians.
5 ConclusionThe results of this study highlight the high prevalence of sexual risk behaviors among medical students, especially regarding inconsistent condom use in both stable and casual relationships. Furthermore, a significant gap in knowledge about STIs and HIV/AIDS was identified; however, the level of knowledge does not appear to be the only determining factor in the adoption of these behaviors. These findings suggest the need to emphasize the importance of promoting a healthy lifestyle among students, including the early introduction of sexual education in the medical curriculum, aiming not only to improve the knowledge of future professionals but also to contribute to the reduction of STI and HIV/AIDS transmission in the general population, fostering more conscious and effective clinical practice.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors upon reasonable request, without undue reservation.
Ethics statementThe studies involving humans were approved by Bahiana School of Medicine and Public Health. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsMN: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. LF: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. IF: Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing. KA: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. BA: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Intramural Research Program of the Oswaldo Cruz Foundation (Fiocruz). BA is a senior scientist from the Brazilian National Council for Scientific and Technological Development (CNPq 1D). KA is a postdoctoral researcher at Gonçalo Moniz Institute, Oswaldo Cruz Foundation. The funding source played no role in the study design; the data collection, analysis or interpretation; or the writing of the manuscript. The researchers retained complete independence in the conduct of the study.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Miranda, AE, Freitas, FLS, Passos, MRL, Lopez, MAA, and Pereira, GFM. Public policies on sexually transmitted infections in Brazil. Rev Soc Bras Med Trop. (2021) 54:e2020611. doi: 10.1590/0037-8682-611-2020
PubMed Abstract | Crossref Full Text | Google Scholar
2. Spindola, T, Fonte, VRF, Francisco, MTR, Martins, ERC, Moraes, PC, and Melo, LD. Sexual practices and risk behaviors for sexually transmitted infections among university students. Rev enferm UERJ. (2021) 29:e63117–7. doi: 10.12957/reuerj.2021.63117
Crossref Full Text | Google Scholar
3. Nagata, JM, Sajjad, OM, Dhama, S, and Santelli, JS. Progress and challenges of HIV and other STIs in adolescents and young adults. Lancet Child Adolesc Heal. (2022) 6:748–9. doi: 10.1016/S2352-4642(22)00256-5
PubMed Abstract | Crossref Full Text | Google Scholar
4. Boyer, CB, Agénor, M, Willoughby, JF, Mead, A, Geller, A, Yang, S, et al. A renewed call to action for addressing the alarming rising rates of sexually transmitted infections in U.S. adolescents and young adults. J Adolesc Health. (2021) 69:189–91. doi: 10.1016/j.jadohealth.2021.05.002
Crossref Full Text | Google Scholar
5. Ferreira Junior, S, Francisco, PMSB, and Loyola, AM. Vulnerability of the young university population to HIV/AIDS and other sexually transmitted infections. J Bras Doenças Sex Transm. (2023) 35:e23351361. doi: 10.5327/DST-2177-8264-2023351361
Crossref Full Text | Google Scholar
6. Gräf, DD, Mesenburg, MA, and Fassa, AG. Risky sexual behavior and associated factors in undergraduate students in a city in southern Brazil. Rev Saude Publica. (2020) 54:41–13. doi: 10.11606/s1518-8787.2020054001709
Crossref Full Text | Google Scholar
7. Fonte, VRF, Spindola, T, Francisco, MTR, Sodré, CP, André, NLNO, and Pinheiro, CDP. Young university students and the knowledge about sexually transmitted infections. Esc Anna Nery. (2018) 22:1–7. doi: 10.1590/2177-9465-ean-2017-0318
Crossref Full Text | Google Scholar
9. Brito, APA, Lima, AS, Rocha, AC, Gonçalves, BM, Freitas, DMCB, Oliveira, GJ, et al. Alcohol consumption habits and their impact on academic performance: analysis of ethanol patterns among health students. A cross-sectional study. Sao Paulo Med J. (2024) 142:e2023410. doi: 10.1590/1516-3180.2023.0410.r1.05062024
PubMed Abstract | Crossref Full Text | Google Scholar
10. Cho, HS, and Yang, Y. Relationship between alcohol consumption and risky sexual behaviors among adolescents and young adults: a Meta-analysis. Int J Public Health. (2023) 68:1–21. doi: 10.3389/ijph.2023.1605669
Crossref Full Text | Google Scholar
11. Keyzers, A, Lee, S-K, and Dworkin, J. Peer pressure and substance use in emerging adulthood: a latent profile analysis. Subst Use Misuse. (2020) 55:1716–23. doi: 10.1080/10826084.2020.1759642
Crossref Full Text | Google Scholar
12. Fonte, VRF, Spindola, T, Lemos, A, Francisco, MTR, and Oliveira, CSR. Knowledge and perception of risks related to sexually transmissible infections among young university students. Cogitare Enferm. (2018) 23:e55903
13. Lederer, AM, and Sheena, BS. A content analysis of college students’ gaps in knowledge about sexually transmitted infections. Health Educ J. (2021) 80:238–50. doi: 10.1177/0017896920959091
Crossref Full Text | Google Scholar
14. Warner, C, Carlson, S, Crichlow, R, and Ross, MW. Sexual health knowledge of U.S. medical students: a National Survey. J Sex Med. (2018) 15:1093–102. doi: 10.1016/j.jsxm.2018.05.019
Crossref Full Text | Google Scholar
15. Kemble, J, Köhler, T, Helo, S, Warner, JN, and Ziegelmann, M. Insufficient medical school sexual health curriculum leads to inadequately prepared trainees. J Sex Med. (2023) 20:133–4. doi: 10.1093/jsxmed/qdad060.207
Crossref Full Text | Google Scholar
16. Merhavy, ZI, Varkey, TC, Kotyk, T, and Zeitler, C. Sexual health preparedness among medical students. Medicni Perspekt. (2023) 28:129–40. doi: 10.26641/2307-0404.2023.4.294193
Crossref Full Text | Google Scholar
17. Askarian, M, Dehghani, Z, Danaei, M, and Vakili, V. Knowledge and practice of medical students on healthy lifestyle: a cross-sectional study in shiraz. J Heal Sci Surveill Syst. (2013) 1:77–82.
18. Pierre, G, Umutoni, A, Nzeyimana, Z, and Dzinamarira, T. Assessment of risky sexual behaviors among university students in Kigali, Rwanda. Int J HIV/AIDS Prev Educ Behav Sci. (2019) 5:141. doi: 10.11648/j.ijhpebs.20190502.19
Crossref Full Text | Google Scholar
19. Sales, WB, Caveião, C, Visentin, A, Mocelin, D, Costa, PM, and Simm, EB. Risky sexual behavior and knowledge of STIs/AIDS among university health students. Rev Enferm Ref. (2016) IV Série:19–28. doi: 10.12707/RIV16019
Crossref Full Text | Google Scholar
22. Amare, T, Yeneabat, T, and Amare, Y. A systematic review and Meta-analysis of epidemiology of risky sexual behaviors in college and university students in Ethiopia, 2018. J Environ Public Health. (2019) 2019:1–8. doi: 10.1155/2019/4852130
PubMed Abstract | Crossref Full Text | Google Scholar
23. Guimarães, MDC, Magno, L, Ceccato, MGB, Gomes, RRFM, Leal, AF, Knauth, DR, et al. HIV/AIDS knowledge among MSM in Brazil: a challenge for public policies mark. Rev Bras Epidemiol. (2019) 22:E190005. doi: 10.1590/1980-549720190005.supl.1
Crossref Full Text | Google Scholar
24. Coleman, E, Elders, J, Satcher, D, Shindel, A, Parish, S, Kenagy, G, et al. Summit on medical school education in sexual health: report of an expert consultation. J Sex Med. (2013) 10:924–38. doi: 10.1111/jsm.12142
PubMed Abstract | Crossref Full Text | Google Scholar
25. Mani, SB, Bral, DO, Soltanianzadeh, Y, Choxi, S, Weissinger, P, Michaelsen, VE, et al. Evaluating attitudes toward and knowledge of human immunodeficiency virus and sexually transmitted infections in first-year medical students. J Student-Run Clin. (2018) 4:1–12. doi: 10.59586/jsrc.v4i1.32
Crossref Full Text | Google Scholar
26. Coronado, PJ, Delgado-Miguel, C, Rey-Cañas, A, and Herráiz, MA. Sexual and reproductive health in Spanish university students. A comparison between medical and law students. Sex Reprod Healthc. (2017) 11:97–101. doi: 10.1016/j.srhc.2016.11.004
PubMed Abstract | Crossref Full Text | Google Scholar
27. Rogowska-Szadkowska, D, and Chlabicz, S. Does the poor HIV/AIDS knowledge among medical students may contribute to late diagnosis? Przegl Epidemiol. (2010) 64:41–5.
28. Turhan, O, Senol, Y, Baykul, T, Saba, R, and Yalçin, AN. Knowledge, attitudes and behaviour of students from a medicine faculty, dentistry faculty, and medical technology vocational training school toward HIV/AIDS. Int J Occup Med Environ Health. (2010) 23:153–60. doi: 10.2478/v10001-010-0008-5
PubMed Abstract | Crossref Full Text | Google Scholar
29. Subotic, S, Vukomanovic, V, Djukic, S, Radevic, S, Radovanovic, S, Radulovic, D, et al. Differences regarding knowledge of sexually transmitted infections, sexual habits, and behavior between university students of medical and nonmedical professions in Serbia. Front Public Health. (2022) 9:692461. doi: 10.3389/fpubh.2021.692461
PubMed Abstract | Crossref Full Text | Google Scholar
30. Štulhofer, A, Šoh, D, Jelaska, N, Bacak, V, and Landripet, I. Religiosity and sexual risk behavior among Croatian college students, 1998-2008. J Sex Res. (2011) 48:360–71. doi: 10.1080/00224499.2010.494257
PubMed Abstract | Crossref Full Text | Google Scholar
31. Gyimah, SO, Tenkorang, EY, Takyi, BK, Adjei, J, and Fosu, G. Religion, HIV/AIDS and sexual risk-taking among men in Ghana. J Biosoc Sci. (2010) 42:531–47. doi: 10.1017/S0021932010000027
PubMed Abstract | Crossref Full Text | Google Scholar
32. Gomes, NL, and Lopes, CS. Panorama of risky sexual behaviors in the Brazilian adult population – PNS 2019. Rev Saude Publica. (2022) 56:61. doi: 10.11606/s1518-8787.2022056004007
PubMed Abstract | Crossref Full Text | Google Scholar
33. Wildsmith, E, Manlove, J, and Steward-Streng, N. Relationship characteristics and contraceptive use among dating and cohabiting young adult couples. Perspect Sex Reprod Health. (2015) 47:27–36. doi: 10.1363/47e2515
PubMed Abstract | Crossref Full Text | Google Scholar
34. Lehmiller, JJ. A comparison of sexual health history and practices a
留言 (0)