The World Health Organization (WHO) estimated that one third to one half of mental health and substance use services were disrupted during the COVID-19 pandemic (1). Alcohol use disorder (AUD) treatment was among the most impacted services (1). In medical and hospital settings, addiction treatment was reduced partially due to furloughed staff, reduced hours, and redeployment of primary care and emergency providers to manage the swell of COVID-19 patients (2). Moreover, public health regulations that banned or discouraged in-person gatherings also prevented individuals from attending mutual-help groups that may be important to individuals in recovery (2). Given the temporary reduction in addiction treatment and service options (3), it is important to assess the extent that AUD treatment interference may be associated with problematic alcohol use during the COVID-19 pandemic.
The pandemic has posed challenges to traditional forms of addiction treatment. For example, some patients reported that therapy appointments were delayed or canceled and therapeutic relationships with their providers were harmed by pandemic-related stress (4, 5). In one study, 77% of adults in recovery from AUD felt the pandemic negatively impacted their recovery (6). To support patients, many addiction treatment programs and mutual-help groups have switched to providing services virtually (2, 4–6). Telemedicine can make addiction treatment more accessible (7–10), leading to increased patient attendance (2), decreased drop-out rates (11), and more flexibility to attend mutual-help groups (6). Yet, some patients may not find telemedicine to be as helpful, citing difficulties making personal connections, technological challenges, concentration problems, and a lack of a quiet environment to attend appointments (4, 6, 8, 11). Given these mixed reports, it is worthwhile to examine the potential impact of pandemic interference with AUD treatment on problematic alcohol use during the pandemic. Of note, a key literature gap in this area is the lack of exploration of moderating factors that may strengthen or weaken the association between treatment interference and problematic alcohol use.
Contextual influences and individual differences may moderate the association between AUD treatment interference and pandemic problematic alcohol use. Specifically, this association may be strengthened by high perceived stress, as stress is linked to maladaptive coping and problematic alcohol use, especially in the context of the pandemic (12–15). Conversely, resilience is a protective factor against problematic alcohol use (16–18) and thus may be a buffer against the adverse impact of AUD treatment interference. The identification of moderators of the AUD treatment interference and problematic alcohol use can help inform prevention and intervention efforts, such as the relevance of stress management and resilience training within addiction treatment (19).
In this study, we investigated the association between pandemic-related AUD treatment interference and problematic alcohol use and tested the moderating roles of perceived stress and resilience. We hypothesized that AUD treatment interference would be positively associated with problematic alcohol use. We further hypothesized that high perceived stress would strengthen the association between AUD treatment interference and problematic alcohol use, whereas high resilience would buffer against the adverse impact of AUD treatment interference on problematic alcohol use.
MethodParticipantsWe utilized baseline data from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) COVID-19 Pandemic Impact on Alcohol (C19-PIA) Study. The C19-PIA study was approved by the National Institutes of Health Intramural Institutional Review Board and is registered in clinicaltrials.gov (NCT04391816). Each participant gave informed consent for participation in the C19-PIA study. Details about the sampling strategy and study procedures were reported previously (13, 20, 21).
The flow diagram presented in Figure 1 illustrates the inclusion and exclusion of participants into the current analysis. First, as we conceptualized treatment interference to be most relevant during the first year of the COVID-19 pandemic, we excluded 93 participants who enrolled on or after March 11, 2021. Of the 398 participants who completed the C19-PIA baseline survey within the first year of the COVID-19 pandemic, 292 (73.4%) provided valid data on all study variables and were retained in the analytic sample. Four participants who did not specify the treatment interfered with by COVID-19 was related to alcohol use were excluded, yielding a final analytic sample of 288 adults. Most participants were current drinkers, and some met criteria for AUD prior to the pandemic. The history of AUD variable was assessed using the Structured Clinical Interview for DSM-IV or DSM-5 (22) as part of the NIAAA Natural History Protocol (NCT02231840), from which all participants were identified and subsequently contacted for participation in the C19-PIA Study. As the development of the pandemic did not follow a linear trend, the timing of enrollment into the C19-PIA Study was stratified into 3 phases while referencing infection statistics and local policies in the metro Washington DC area: June 3, 2020 to July 31, 2020 (Phase 1; 26.4%), August 1, 2020 to November 22, 2020 (Phase 2; 38.5%), and November 23, 2020 to March 3, 2021 (Phase 3; 35.1%). Enrollment phase was included in all adjusted analyses.

Figure 1. Flow diagram illustrating participant inclusion and exclusion in the current study.
MeasuresAUD treatment interferenceThe AUD treatment interference survey item was embedded as part of a list of beliefs and experiences related to the COVID-19 pandemic. Thus, all participants were asked to rate their degree of agreement with the question: “Coronavirus has directly or indirectly prevented me from getting or interfered with treatment for my alcohol or substance use disorder.” Response options for the five-point Likert scale were 1 “strongly disagree”, 2 “disagree”, 3 “neutral”, 4 “agree”, and 5 “strongly agree”. The item was accompanied by an optional qualitative question asking the participant to specify the treatment interference experienced.
Problematic alcohol useThe 10-item Alcohol Use Disorders Identification Test (AUDIT; 23) is a widely used self-report measure developed by the WHO to screen for past year problematic drinking. Total AUDIT scores were computed (α = 0.93; possible range from 0-40), with a score of ≥8 indicating problematic alcohol use.
Perceived stressThe 10-item Perceived Stress Scale (PSS; 24) is a validated self-report questionnaire that assesses the frequency of stress experienced over the past month. Total PSS scores were computed (α = 0.91; possible range from 0-40), with higher scores indicating higher perceived stress.
ResilienceThe 25-item Connor-Davidson Resilience Scale (CDRS; 25) is a self-report questionnaire of resiliency. Response options for the five-point Likert scale ranged from 0 “not true at all” to 4 “true nearly all the time”. Total CDRS scores were computed (α = 0.96; possible range from 0-100), with higher scores indicating higher resiliency.
AnalysesThree multiple linear regression models were utilized to test the direct association between AUD treatment interference and problematic alcohol use (model 1) and conditional associations moderated by perceived stress (model 2) and resilience (model 3). Unadjusted analyses were first conducted. Next, we conducted adjusted analyses controlling for the following covariates: age, sex, race, ethnicity, years of education, household income, marital status, study enrollment phase, and history of AUD. For any significant interactions, simple slope analyses were conducted to decompose the interactions and the interactions would be visualized to aid interpretation. Analyses were conducted in Stata 17.0 (26). Sensitivity analyses were also conducted among current drinkers only (n = 237) after excluding 51 individuals with an AUDIT score of 0.
ResultsDescriptive statistics are presented in Table 1. Among participants, 30.6% (n = 88) “strongly disagreed” that the pandemic had interfered with their AUD treatment, 55.2% (n = 159) “disagreed”, 6.6% (n = 19) were “neutral”, 4.5% individuals (n = 13) “agreed”, and 3.1% “strongly agreed” (n = 9). Examples of how COVID-19 interfered with AUD treatment included Alcoholics Anonymous meetings being online and being unable to see one’s therapist or enter inpatient treatment.
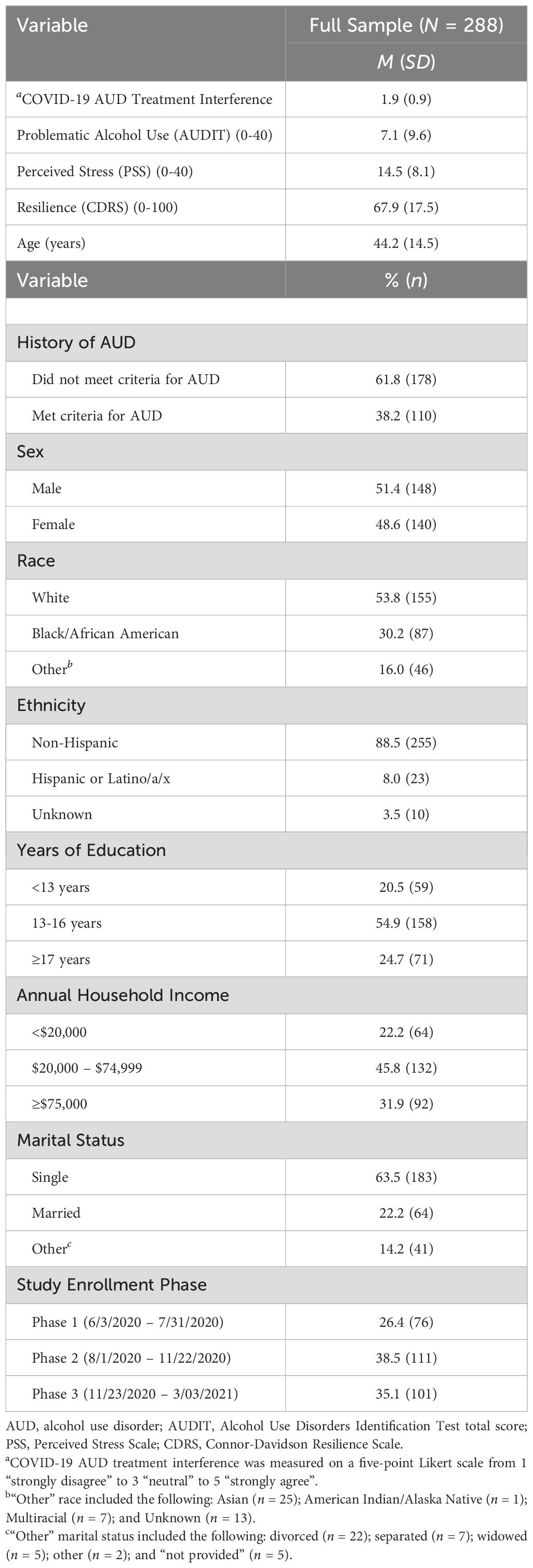
Table 1. Descriptive statistics of study variables.
Unadjusted and adjusted estimates from the multiple regression models are presented in Table 2. Significant interactions are visualized in Figure 2. Model 1 showed that AUD treatment interference was positively associated with higher problematic alcohol use (b = 2.05, SE = 0.53, p < 0.001). Model 2 indicated that perceived stress moderated the association between AUD treatment interference and problematic alcohol use (b = 0.24, SE = 0.05, p < 0.001). Simple slope analyses showed that the association between AUD treatment interference and problematic alcohol use was not significant at a low level (1 SD below the mean) of perceived stress (b = -0.78, SE = 0.77, p = 0.308), but was significant at the mean (b = 1.15, SE = 0.53, p = 0.032) and a high level (1 SD above the mean) of perceived stress (b = 3.08, SE = 0.58, p < 0.001). Model 3 showed that resilience also moderated the association between AUD treatment interference and problematic alcohol use (b = -0.09, SE = 0.03, p = 0.001). Simple slope analyses showed that the association between AUD treatment interference and problematic alcohol use was significant at a low level of resilience (b = 3.09, SE = 0.63, p < 0.001) and at the mean of resilience (b = 1.48, SE = 0.54, p = 0.007). The association between AUD treatment interference and problematic alcohol use was not significant at a high level of resilience (b = -0.13, SE = 0.82, p = 0.874). The main effect of AUD treatment interference and moderated effects of perceived stress and resilience were replicated in the sensitivity analysis among current drinkers only.
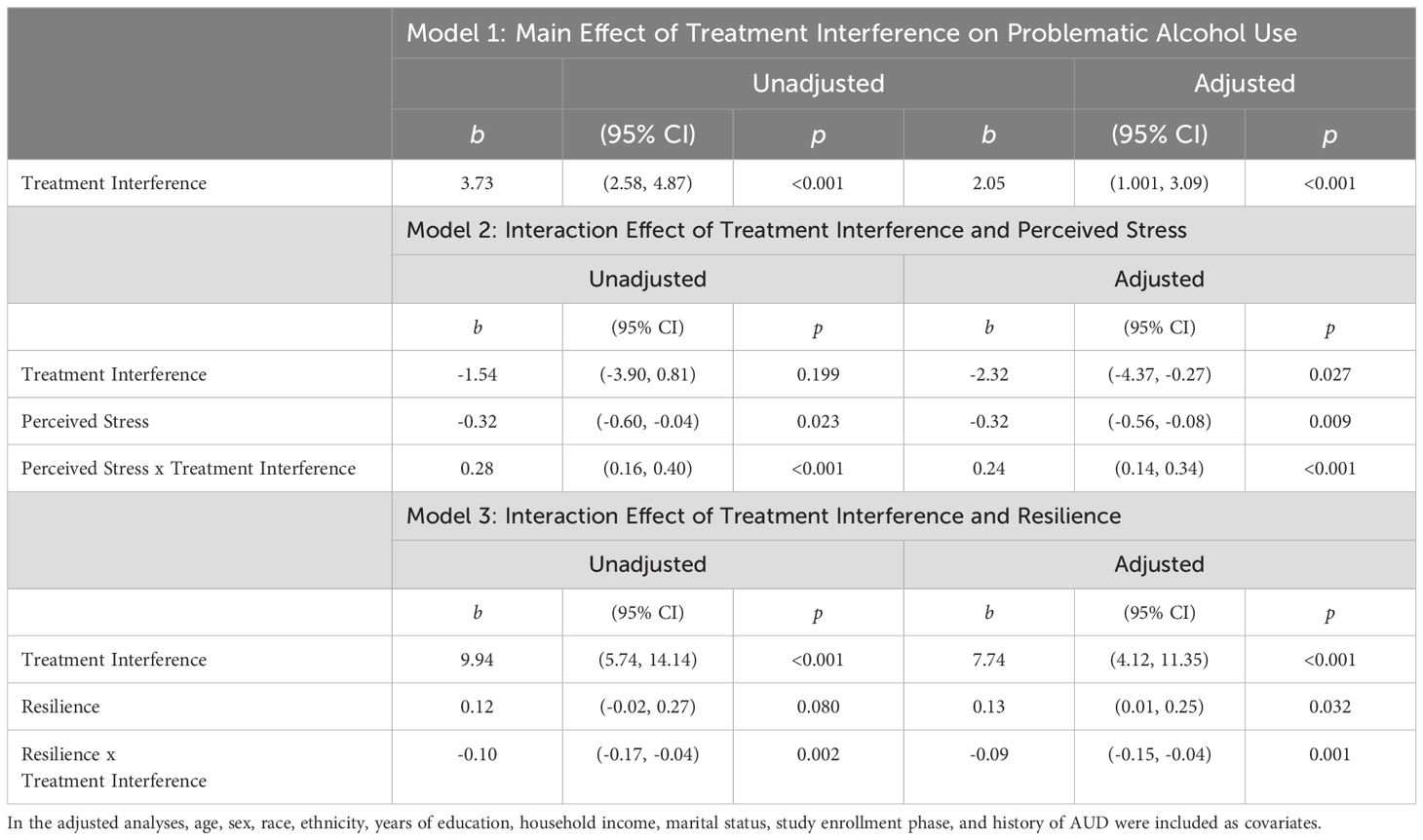
Table 2. Unadjusted and adjusted estimates from the multiple regression models on problematic alcohol use (N = 288).
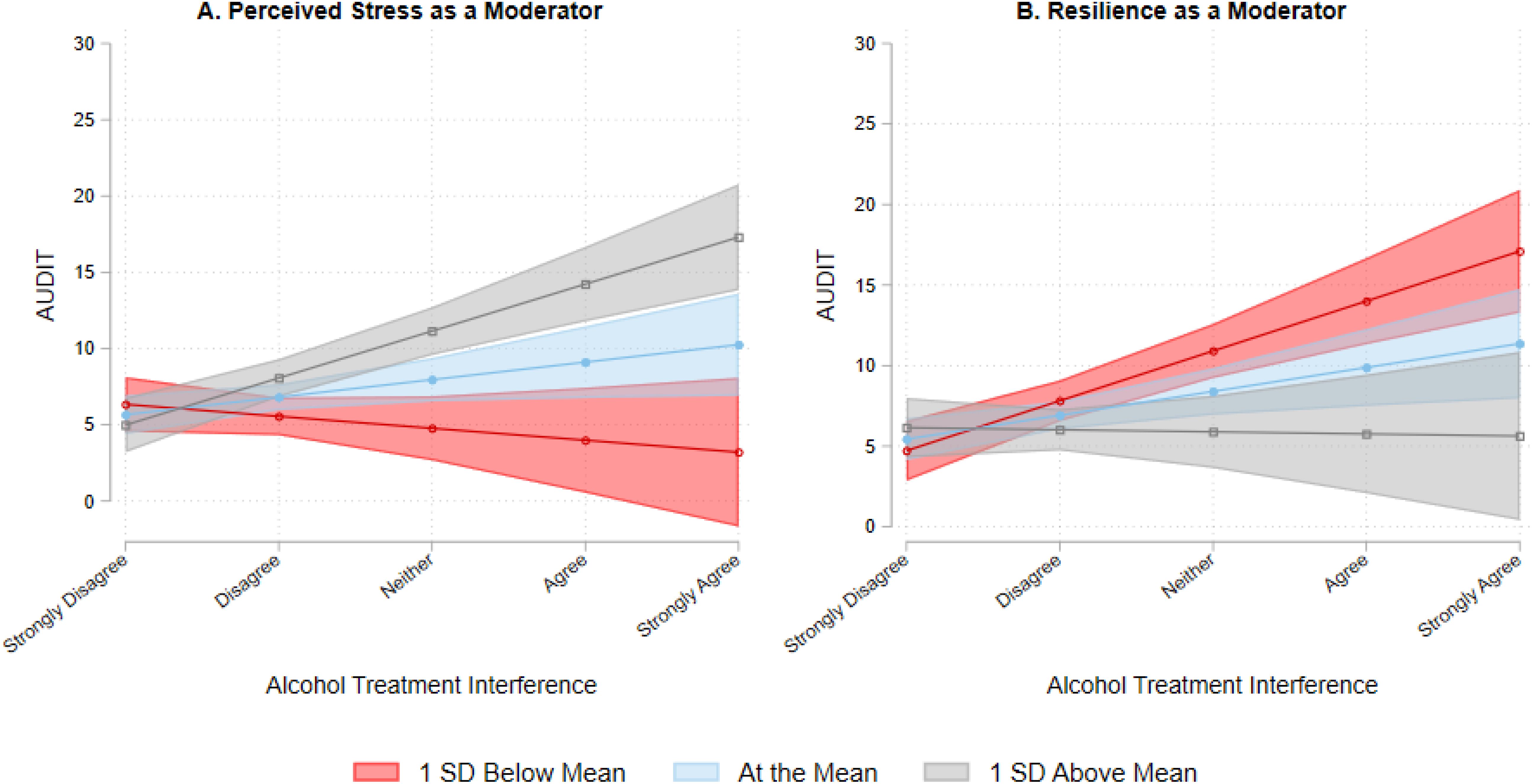
Figure 2. The association between alcohol treatment interference and problematic alcohol use with perceived stress (A) or resilience (B) as a moderator. AUDIT, Alcohol Use Disorders Identification Test.
DiscussionParallel to research documenting how mental health treatment interference during the pandemic was associated with heightened psychological distress (27), the present research showed that AUD treatment interference was associated with higher problematic alcohol use. This is an important finding in light of recent research illustrating increased alcohol-related deaths in the United States during the pandemic (28). Possibly, interruption to AUD treatment could have contributed to increased alcohol-related morbidities (29), alcohol withdrawal (30), and alcohol use among individuals with AUD during the pandemic (31–33). The significant main effect of AUD treatment interference on problematic alcohol use supported the existence of an AUD treatment gap during the COVID-19 pandemic.
In this study, AUD treatment interference was assessed using a self-report item that gauged the subjective perception of whether individuals encountered disruption to treatment. To maximize generalizability of findings, we analyzed data from all participants who answered the question regardless of their prior AUD status as new problematic drinking behaviors could have emerged during the pandemic. While our sensitivity analysis ensured that the study findings were robust among current drinkers, replication and extension of our novel findings should be carried out in other clinical samples. Moreover, as telemedicine has become more widely adopted, research is needed to evaluate what type of addiction treatment may be effectively delivered online and identify ways to foster a sense of community using the online format. For some individuals, a return to in-person treatment sessions may be needed to optimize their AUD treatment experience.
Unique to the present investigation was the richness of the available data which allowed us to test perceived stress and resilience as moderators of the treatment interference and problematic alcohol use association. The significant interaction effects were consistent with our hypotheses: perceived stress strengthened the adverse impact of AUD treatment interference on problematic alcohol use and resilience exerted a protective effect. Clinical implications of this study include the need to foster positive coping strategies to mitigate the adverse impact of stress on drinking and to promote resilience as a buffer against problematic alcohol use (34, 35).
This study has several limitations. First, enrollment into the C19-PIA Study was on a rolling basis, and so variations in COVID-related restriction policies could have influenced the degree of AUD treatment interference. Second, a convenience sample was used and participants without income/education, resilience, or alcohol-related data were excluded. It is possible that participants with alcohol-related problems were less likely complete all measures which may introduce bias. To mitigate these concerns, future replications of the study findings in a larger clinical sample with a narrower study recruitment time frame and greater incentive for completing all study measures may be considered. Third, the AUD treatment interference construct was assessed using a single self-reported item and endorsement of treatment interference was low. This single item utilized a Likert scale and its use in regression analyses assumed that the intervals between response categories were equal. This measurement weakness can be addressed in future research with the use of more objective measures on treatment history, treatment type, and estimation of changes in the number of treatment sessions attended. Fourth, measures of perceived stress, resilience, and problematic alcohol use were also self-reported and may be vulnerable to recall or report bias. Extending the current findings, more research is needed to understand individual preferences for specific forms of addiction treatment delivery methods, such as in-person, telehealth, and hybrid formats (10), as well as the longer-term clinical outcomes after pandemic-related treatment interferences have subsided.
In conclusion, results from this study suggest the existence of an AUD treatment gap during the COVID-19 pandemic with treatment interruption linked to higher problematic alcohol use. Findings also highlight the importance of considering the moderating roles of contextual (e.g., perceived stress) and individual (e.g., resilience) factors in the association between AUD treatment interference and problematic alcohol use. To improve preparedness for future public health crises, the prioritization of cognitive-behavioral skills to improve stress management and promote resilience may be warranted to prevent problematic alcohol use or relapse to alcohol use (19). More broadly, the utilization of brief, mass-delivered interventions and lay-provider service delivery may also be an integral part of a comprehensive mental health response to future public health emergencies (36). While the shift to telehealth addiction treatment may have helped with improving access and convenience for some patients (8), more research is needed to examine individual preferences for various forms of AUD treatment and track the outcomes of these treatments in the post-pandemic world.
Data availability statementThe datasets presented in this article are not readily available because of ethical concerns regarding patient privacy and original patient consent. Data may be made available by requests directly to the corresponding authors. Requests to access the datasets should be directed to Jeremy Luk, amVyZW15Lmx1a0BuaWguZ292 and Vijay Ramchandani, dmlqYXlyQG1haWwubmloLmdvdg==.
Ethics statementThe studies involving humans were approved by National Institutes of Health Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided verbal informed consent to participate in this survey study.
Author contributionsRV: Conceptualization, Formal analysis, Writing – original draft. JL: Conceptualization, Formal analysis, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BS: Conceptualization, Project administration, Writing – review & editing. EM: Conceptualization, Writing – review & editing. UZ: Conceptualization, Writing – review & editing. MS: Conceptualization, Data curation, Project administration, Writing – review & editing. DG: Conceptualization, Writing – review & editing. VR: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing. ND: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by NIAAA Division of Intramural Clinical and Biological Research (Z1A AA000130, Z1A AA000466) and a National Institute of Allergy and Infectious Diseases (NIAID) Intramural Targeted Anti-COVID (ITAC) Award.
AcknowledgmentsWe would like to thank the study participants and the clinicians, staff, and post-baccalaureate research assistants who helped collect or manage this data. We would also like to thank other members of the Human Psychopharmacology Laboratory, the Office of the Clinical Director, the Clinical NeuroImaging Research Core, and the Section on Sensory Science and Metabolism at NIAAA for their support.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. World Health Organization. Mental health and COVID-19: early evidence of the pandemic’s impact: scientific brief, 2 March 2022. Geneva, Switzerland: World Health Organization (2022). Available at: https://iris.who.int/handle/10665/352189. License: CC BY-NC-SA 3.0 IGO.
2. Melamed OC, DeRuiter WK, Buckley L, Selby P. Coronavirus Disease 2019 and the impact on substance use disorder treatments. Psychiatr Clinics. (2022) 45:95–107. doi: 10.1016/j.psc.2021.11.006
PubMed Abstract | Crossref Full Text | Google Scholar
3. Lensch AC, Hairston E, Carter G, Jones HE. Pregnant patients using opioids: Treatment access barriers in the age of COVID-19. J Addict Med. (2022) 16:e44–7. doi: 10.1097/ADM.0000000000000826.
PubMed Abstract | Crossref Full Text | Google Scholar
4. DeJong CA, Verhagen JGD, Pols R, Verbrugge CA, Baldacchino A. Psychological impact of the acute COVID-19 period on patients with substance use disorders: We are all in this together. Basic Clin Neurosci. (2020) 11:207–16. doi: 10.32598/bcn.11.covid19.2543.1
PubMed Abstract | Crossref Full Text | Google Scholar
5. Huhn AS, Strain EC, Jardot J, Turner G, Bergeria CL, Nayak S, et al. Treatment disruption and childcare responsibility as risk factors for drug and alcohol use in persons in treatment for substance use disorders during the COVID-19 crisis. J Addict Med. (2022) 16:e8–e15. doi: 10.1097/ADM.0000000000000813
PubMed Abstract | Crossref Full Text | Google Scholar
6. Scarfe ML, Haik AK, Rahman L, Todi AA, Kane C, Walji A, et al. Impact of COVID-19 on alcohol use disorder recovery: A qualitative study. Exp Clin Psychopharmacol. (2022) 31:148–62. doi: 10.1037/pha0000560
PubMed Abstract | Crossref Full Text | Google Scholar
7. Kruse CS, Lee K, Watson JB, Lobo LG, Stoppelmoor AG, Oyibo SE. Measures of effectiveness, efficiency, and quality of telemedicine in the management of alcohol abuse, addiction, and rehabilitation: Systematic review. J Med Internet Res. (2020) 22:e13252. doi: 10.2196/13252
PubMed Abstract | Crossref Full Text | Google Scholar
8. Mark TL, Treiman K, Padwa H, Henretty K, Tzeng J, Gilbert M. Addiction treatment and telehealth: Review of efficacy and provider insights during the COVID-19 pandemic. Psychiatr Serv. (2022) 73:484–91. doi: 10.1176/appi.ps.202100088
PubMed Abstract | Crossref Full Text | Google Scholar
9. Sugarman DE, Busch AB, McHugh RK, Bogunovic OJ, Trinh CD, Weiss RD, et al. Patients’ perceptions of telehealth services for outpatient treatment of substance use disorders during the COVID-19 pandemic. Am J Addict. (2021) 30:445–52. doi: 10.1111/ajad.13207
PubMed Abstract | Crossref Full Text | Google Scholar
10. Tomlinson MF, McCann-Pineo M, Thomas MP, Polydorou S. Demographic differences in services utilization across in-person, (2019), telehealth, (2020), and hybrid, (2021) outpatient substance use services in New York. J Subst Use Addict Treat. (2023) 150:209047. doi: 10.1016/j.josat.2023.209047
PubMed Abstract | Crossref Full Text | Google Scholar
11. Lin LA, Casteel D, Shigekawa E, Weyrich MS, Roby DH, McMenamin SB. Telemedicine-delivered treatment interventions for substance use disorders: A systematic review. J Subst Abuse Treat. (2019) 101:38–49. doi: 10.1016/j.jsat.2019.03.007
PubMed Abstract | Crossref Full Text | Google Scholar
12. Koob GF, Powell P, White A. Addiction as a coping response: Hyperkatifeia, deaths of despair, and COVID-19. Am J Psychiatry. (2020) 177:1031–7. doi: 10.1176/appi.ajp.2020.20091375
PubMed Abstract | Crossref Full Text | Google Scholar
13. Luk JW, Stangl BL, Schwandt ML, Gunawan T, Joseph PV, Momenan R, et al. A person-centered approach to capture health disparities and multidimensional impact of COVID-related stressors. Am Psychol. (2023) 78:321–32. doi: 10.1037/amp0001044
PubMed Abstract | Crossref Full Text | Google Scholar
14. McKnight-Eily LR, Okoro CA, Strine TW, Verlenden J, Hollis ND, Njai R, et al. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic—United States, April and May 2020. Morbid Mortal Weekly Rep. (2021) 70:162–6. doi: 10.15585/mmwr.mm7005a3
PubMed Abstract | Crossref Full Text | Google Scholar
15. Schmidt RA, Genois R, Jin J, Vigo D, Rehm J, Rush B. The early impact of COVID-19 on the incidence, prevalence, and severity of alcohol use and other drugs: A systematic review. Drug Alcohol Depend. (2021) 228:109065. doi: 10.1016/j.drugalcdep.2021.109065
PubMed Abstract | Crossref Full Text | Google Scholar
16. Cusack SE, Bountress KE, Sheerin CM, Dick DM, Amstadter AB. The longitudinal buffering effects of resilience on alcohol use outcomes. psychol Trauma: Theory Res Pract Policy. (2021) 15(6):1000–1011. doi: 10.1037/tra0001156
PubMed Abstract | Crossref Full Text | Google Scholar
17. Wingo AP, Ressler KJ, Bradley B. Resilience characteristics mitigate tendency for harmful alcohol and illicit drug use in adults with a history of childhood abuse: A cross-sectional study of 2024 inner-city men and women. J Psychiatr Res. (2014) 51:93–9. doi: 10.1016/j.jpsychires.2014.01.007
PubMed Abstract | Crossref Full Text | Google Scholar
18. Sheerin CM, Bountress KE, Hicks TA, Lind MJ, Aggen SH, Kendler KS, et al. Longitudinal examination of the impact of resilience and stressful life events on alcohol use disorder outcomes. Subst Use Misuse. (2021) 56:1346–51. doi: 10.1080/10826084.2021.1922454
PubMed Abstract | Crossref Full Text | Google Scholar
19. Luk JW, Thompson MF. Mapping dialectical behavior therapy skills to clinical domains implicated in contemporary addiction research: A conceptual synthesis and promise for precision medicine. Cogn Behav Pract. (2024). doi: 10.1016/j.cbpra.2024.07.002
Crossref Full Text | Google Scholar
20. Luk JW, Stangl BL, Gunawan T, Schwandt ML, Morris JK, Axelowitz JC, et al. Changes in alcohol-related behaviors and quality of life during the COVID-19 pandemic: Impact of alcohol use disorder diagnosis and treatment history. J Clin Psychiatry. (2022) 84:22br14462. doi: 10.4088/JCP.22br14462
PubMed Abstract | Crossref Full Text | Google Scholar
21. Luk JW, Leiter N, Stangl BL, Gunawan T, Schwandt ML, Goldman D, et al. Associations of history of alcohol use disorder with loneliness, social support, and mental health during the COVID-19 pandemic. Psychiatry Res. (2024) 335:115826. doi: 10.1016/j.psychres.2024.115826
PubMed Abstract | Crossref Full Text | Google Scholar
22. First MB. Structured clinical interview for the DSM (SCID). Encyclopedia Clin Psychol. (2015), 1–6. doi: 10.1002/9781118625392.wbecp351
Crossref Full Text | Google Scholar
23. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. (1993) 88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
PubMed Abstract | Crossref Full Text | Google Scholar
24. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
Crossref Full Text | Google Scholar
26. StataCorp. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC (2021).
27. Ligus K, Fritzson E, Hennessy EA, Acabchuk RL, Bellizzi K. Disruptions in the management and care of university students with preexisting mental health conditions during the COVID-19 pandemic. Trans Behav Med. (2021) 11:802–7. doi: 10.1093/tbm/ibab020
PubMed Abstract | Crossref Full Text | Google Scholar
29. Murthy P, Narasimha VL. Effects of the COVID-19 pandemic and lockdown on alcohol use disorders and complications. Curr Opin Psychiatry. (2021) 34:376–85. doi: 10.1097/YCO.0000000000000720
PubMed Abstract | Crossref Full Text | Google Scholar
30. Sharma RA, Subedi K, Gbadebo BM, Wilson B, Jurkovitz C, Horton T. Alcohol withdrawal rates in hospitalized patients during the COVID-19 pandemic. JAMA Netw Open. (2021) 4:e210422. doi: 10.1001/jamanetworkopen.2021.0422
PubMed Abstract | Crossref Full Text | Google Scholar
31. Hutchison M, Aldalur A, Maisto SA, Chiang A, Abar B, Stecker T, et al. Alcohol use during COVID-19 in adults with severe untreated AUD. Alcohol Treat Q. (2022) 40:299–310. doi: 10.1080/07347324.2022.2060156
PubMed Abstract | Crossref Full Text | Google Scholar
32. Carlyle M, Leung J, Walter ZC, Juckel J, Salom C, Quinn CA, et al. Changes in substance use among people seeking alcohol and other drug treatment during the COVID-19 pandemic: Evaluating mental health outcomes and resilience. Subst Abuse: Res Treat. (2021) 15. doi: 10.1177/11782218211061746
PubMed Abstract | Crossref Full Text | Google Scholar
33. Kim JU, Majid A, Judge R, Crook P, Nathwani R, Selvapatt N, et al. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. Lancet Gastroenterol Hepatol. (2020) 5:886–7. doi: 10.1016/S2468-1253(20)30251-X
PubMed Abstract | Crossref Full Text | Google Scholar
34. Corbin WR, Farmer NM, Nolen-Hoekesma S. Relations among stress, coping strategies, coping motives, alcohol consumption and related problems: A mediated moderation model. Addictive Behav. (2013) 38:1912–9. doi: 10.1016/j.addbeh.2012.12.005
PubMed Abstract | Crossref Full Text | Google Scholar
35. Hodder RK, Daly J, Freund M, Bowman J, Hazell T, Wiggers J. A school-based resilience intervention to decrease tobacco, alcohol and marijuana use in high school students. BMC Public Health. (2011) 11:1–10. doi: 10.1186/1471-2458-11-722
PubMed Abstract | Crossref Full Text | Google Scholar
36. Gruber J, Prinstein MJ, Clark LA, Rottenberg J, Abramowitz JS, Albano AM, et al. Mental health and clinical psychological science in the time of COVID-19: Challenges, opportunities, and a call to action. Am Psychol. (2021) 76:409–26. doi: 10.1037/amp0000707
留言 (0)