Trauma represents the primary cause of mortality and morbidity in children. More than 90% of childhood trauma globally is attributable to blunt force trauma, with approximately 10% of cases involving abdominal and pelvic injuries. Among the abdominal traumas, the spleen is the most frequently injured internal organ in children (1, 2). Children are at a significantly increased risk of damage to abdominal organs compared to adults due to several factors, including thinner abdominal walls, greater force transmission, larger relative surface areas of the spleen and liver, as well as more flexible ribs and a relatively higher position of the diaphragm (3).
The management of splenic trauma has undergone significant changes over the past few decades, particularly in non-operative management (NOM). The scope of non-surgical treatment has gradually expanded from observation and monitoring alone to include angiography and angioembolization (AG/AE), with the central goal of preserving the spleen and its immune function, which is particularly important in pediatric patients. Given the critical role of the spleen in the immune system and the high risk of patients facing compromised immune function after splenectomy, spleen injury may not only be life-threatening at the time of patient admission. Still, it may also result in fatal complications due to the rupture of a delayed subcapsular hematoma or pseudoaneurysm (PSA). Furthermore, post-splenectomy infection (OPSI) represents a significant risk factor for late complications due to the loss of the spleen's immune defenses. The length of hospital stay is an important indicator of the patient's recovery and outcome. In pediatric closed splenic injuries, a prolonged hospital stay may be associated with more severe injuries, the presence of comorbidities, and different treatment options. Therefore, analysis of risk factors for prolonged hospital stays may help to optimize treatment strategies and improve patient prognosis.
Nonoperative management (NOM) has become the standard of care for hemodynamically stable patients with blunt splenic injuries (4). These patients are typically treated with strict bed rest and close monitoring of vital signs. The direct success rate of NOM currently exceeds 98% (5, 6). This study aimed to investigate the independent risk factors influencing the length of stay in pediatric closed splenic injuries and to analyze the key determinants in the choice of surgical treatment to optimize inpatient management and patient care and improve outcomes.
Methods Study designThis was a retrospective single-center cohort study of pediatric patients diagnosed with BSI. The study population comprised patients who were hospitalized or transferred to Wuhan Children's Hospital from January 1, 2020, to May 1, 2024, in Wuhan. The pediatric age group was defined as patients younger than 15 years old, in accordance with the age limit for hospitalization in Chinese pediatric hospitals. There were 83 patients in this group. Patients who were admitted to the hospital after 24 h post-injury (N = 16) or who did not have CT findings within 48 h post-injury (N = 15) were excluded from the analysis, resulting in a total of 52 patients included in the study (Figure 1).
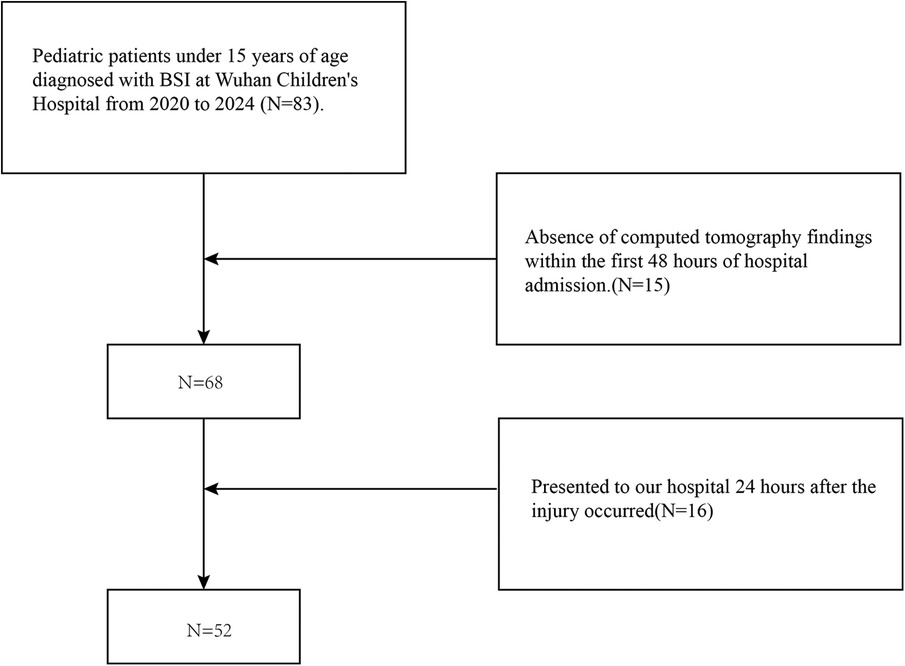
Figure 1. Flow chart of the study participants. BSI, blunt splenic injury.
Data collectionThe data about the patient and the nature of the injury were collated from the hospital's electronic case system, following the requisite approval from the ethical review board. Demographic data, including age, gender, and admission center, were collected. The clinical information obtained included vital signs, transfusion requirements, World Society of Emergency Surgery (WSES) ratings, Injury Severity Score (ISS), hemodynamic status, mechanism of injury, splenic injury grade, and other relevant injuries. Furthermore, the data set includes information on the type of treatment (conservative or surgical), length of stay in the intensive care unit (ICU), total length of stay (LOS), time in bed, and mortality.
The injury severity scores were determined by a team of physicians from the Department of Critical Care Medicine and the Department of Emergency Surgery.
The term “hemodynamic stability” is defined as a systolic blood pressure of 90 mmHg plus twice the child's age in years. It should be noted that the lower limit is below 70 mmHg plus twice the child's age in years, or 50 mmHg in some studies. Furthermore, a positive response to fluid resuscitation was defined as hemodynamic stability. This may be evidenced by a decrease in heart rate, a clear sensation, the return of a peripheral pulse, normal skin color, an increase in blood pressure and urine output, and an increase in extremity warmth (7). As these parameters vary with age, this is determined through a joint clinical judgment between emergency surgeons and pediatric critical care medicine physicians. The initial classification of the grade of injury was made by a pediatric radiologist with expertise in trauma imaging, who evaluated a CT scan within 48 h of the child's admission to the hospital according to the AAST classification system. Nonoperative treatment was defined as bed rest and monitoring of vital signs, including splenic embolization, as it is a less invasive procedure. Surgical treatment was defined as splenectomy or spleen-preserving surgery, which included partial splenectomy and splenectomy. The injury severity scores were determined by a team of physicians from the Department of Critical Care Medicine and the Department of Emergency Surgery. The primary objective of this study was to identify the factors that influence the length of hospitalization and the decision to perform surgery.
Statistical analysisAll statistical analyses were conducted using the R statistical software package (http://www.R-project.org) and EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc., Boston, MA). Descriptive statistics were calculated for each variable. Continuous variables were described as mean ± standard deviation (SD), whereas categorical variables were reported as frequencies and percentages (n, %). The appropriate statistical test for each variable was determined based on the distribution of the data, as assessed by the Kolmogorov-Smirnov Z-test. Continuous variables were analyzed using either independent t-tests or Mann-Whitney U-tests, while categorical variables were evaluated using chi-square and Fisher exact tests. Multivariate linear regression models were employed to ascertain the independent risk factors associated with prolonged length of stay (LOS). The independent risk factors for the selection of surgical treatment were determined using a multivariate logistic regression analysis, with a p-value of less than 0.05 considered to be statistically significant.The analysis uses a Generalized Additive Model (GAM) to examine the relationship between LOS and ISS.
Results Patient characteristicsFrom 2020 to 2024, a total of 70 blunt splenic injuries were admitted to our hospital. A total of 52 patients with BSI (65.4% male) were included in the study, with a mean age of 6.2 ± 2.8 years, a mean length of hospitalization of (14.0 ± 9.7) days, and a mean World Society of Emergency Surgery (WSES) classification of grade 2. The most common mechanism of trauma was motor vehicle accidents (34.6%). The additional patient demographics for the entire cohort are presented in Table 1.
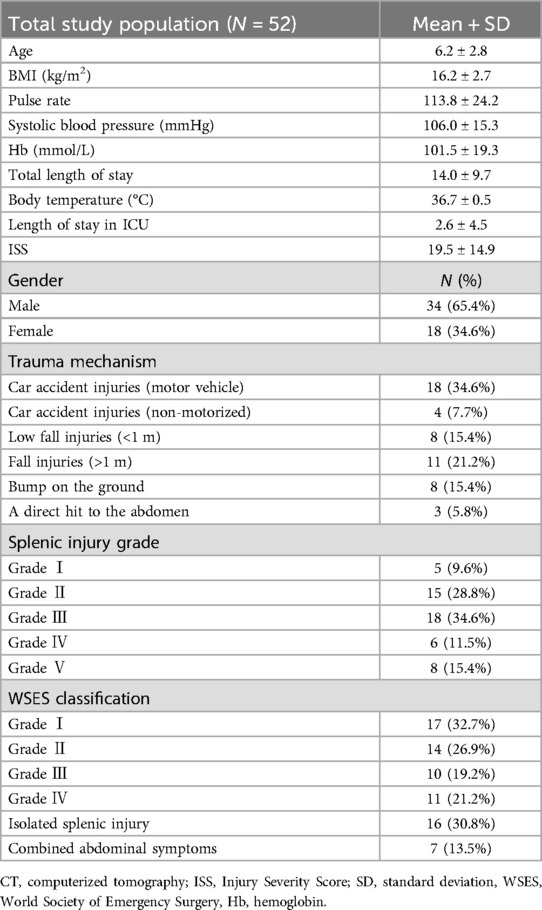
Table 1. Characteristics of the study population.
Injury characteristicsA total of 69.2% of patients were polytraumatized, exhibiting higher Injury Severity Scores (ISS) (6.2 ± 3.1 vs. 25.4 ± 14.2, p < 0.001) and accelerated heart rates (99.5 ± 12.9 vs. 120.0 ± 25.4, p = 0.004) compared to non-polytraumatized patients. The mean hemoglobin (Hb) concentration on admission in BSI patients was 101.5 ± 19.3 mmol/L, with a mean ISS of 19.5 ± 14.9. A total of 3% of patients exhibited hemodynamic instability, with a significantly higher Injury Severity Score (ISS) in the stable group compared to the unstable group (17.7 ± 13.2 vs. 28.4 ± 19.4, p < 0.05). Additionally, the stable group demonstrated a higher temperature than the unstable group (36.8 ± 0.4 vs. 36.4 ± 0.5, p < 0.05). These patients were also more prone to manifestations of shock, which led to a higher rate of blood transfusion (20.9% vs. 77.8%; p < 0.001). The mean splenic injury grade on admission was 3.0, with 26.9% of patients exhibiting a higher injury grade (grades IV-V) as determined by CT imaging.
As can be seen in the Figure 2, the smoothed curve shows a gradual upward trend in hospital length of stay at lower ISS values, suggesting a corresponding increase in hospital length of stay as injury severity increases. In the medium to high ISS range (e.g., 40–60), the smoothed curve tends to flatten or even decrease slightly, possibly reflecting the lack of significant further prolongation of hospital time in patients with high ISS, suggesting that there may be other influences, such as the effects of more intensive care or increased mortality.
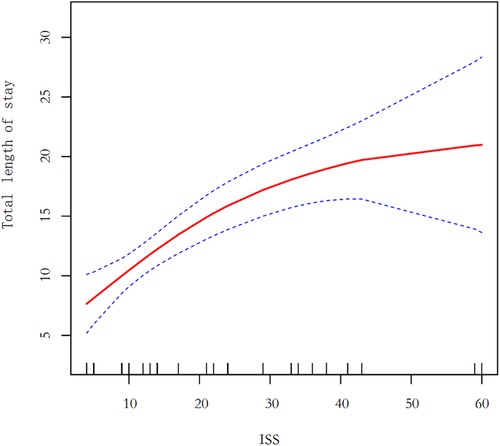
Figure 2. Generalized additive model. ISS, injury severity score.
Operative managementThe results are presented in tabular form. The mean and standard deviation (SD) were calculated for each variable. The Kruskal-Wallis rank sum test was used for continuous variables, while the Fisher exact probability test was employed for count variables with a theoretical number of less than 10.
ManagementA total of 88.5% of patients underwent non-operative management (NOM), with 11% of these cases involving embolization of the spleen for hemodynamic instability and arterial hemorrhage in Table 2. The remaining 11.5% underwent splenectomy or partial splenectomy for indications requiring surgical exploration, including comorbid gastrointestinal perforation, or peritonitis. The majority of patients who underwent surgical intervention were selected for this procedure due to the presence of comorbid abdominal symptoms (66.7%). One patient died as a result of brain injury. The surgical group exhibited higher transfusion requirements and ISS scores than the non-surgical group (21.7% vs. 100%, p < 0.001; 37.7 ± 16.1 vs. 17.2 ± 13.1, p < 0.001, respectively). The results of the multivariate logistic regression analysis indicated that the combination of abdominal symptoms, including gastrointestinal perforation, and peritonitis, was significantly associated with the decision to perform surgery [β (95% CI), P value/OR (95% CI), P value; p < 0.05] in Table 3.
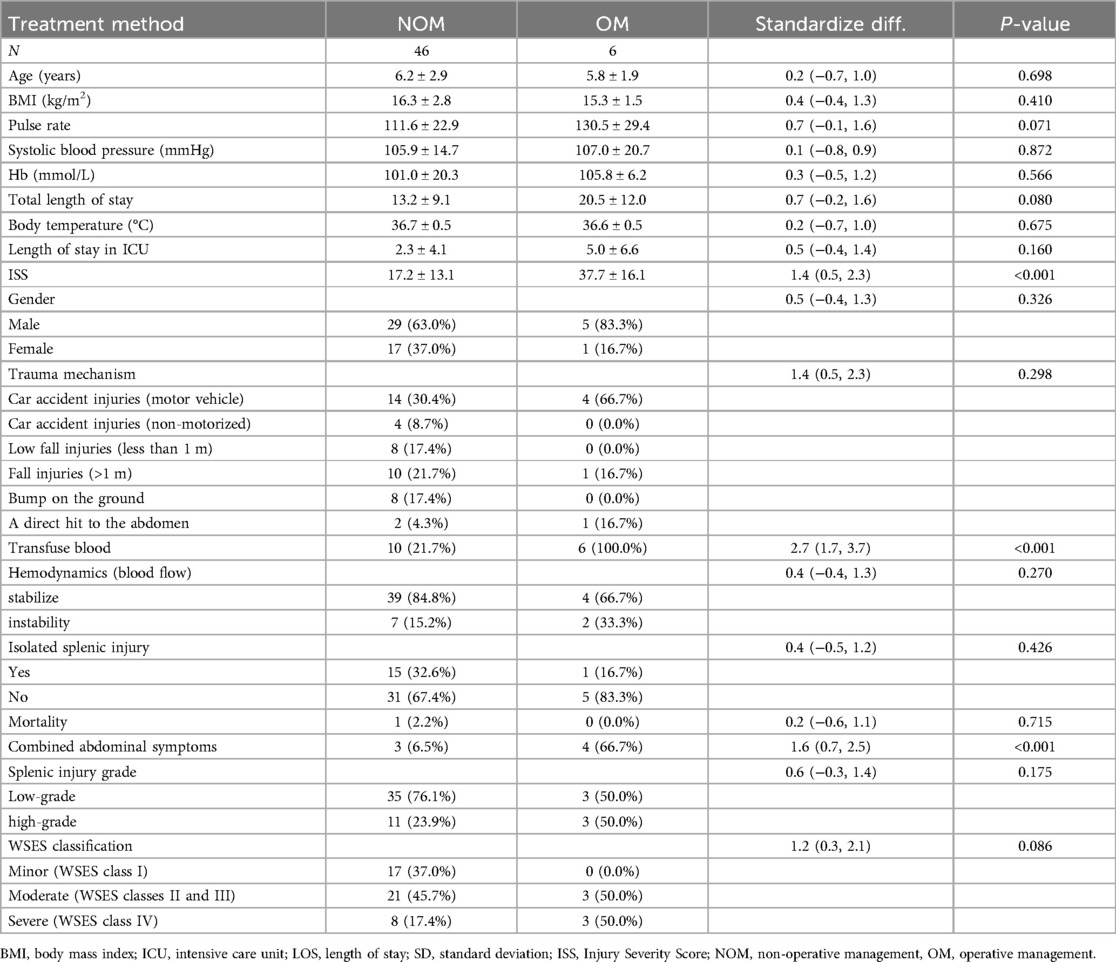
Table 2. Comparison of characteristics: NOM vs. OM in patients.
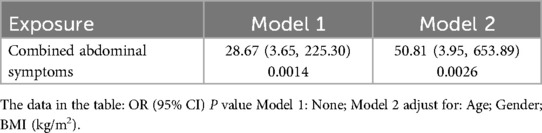
Table 3. Multivariate logistic regression analysis.
Treatment outcomesTwenty-four patients were admitted to the intensive care unit on admission and were on bed rest from the time of admission; patients were not active until discharge. With polytrauma, patients with high ISS scores had a longer hospital stay (all p < 0.05).
DiscussionIn managing pediatric closed splenic injuries, clinical judgment and early resuscitation are critical in choosing a management strategy. In patients who are initially hemodynamically unstable, non-surgical management only applies after effective resuscitation and hemodynamic stability have been achieved. This allows the preservation of splenic function and minimization of invasive manipulation while ensuring patient safety. Our results show that some patients can remain stable after resuscitation, resulting in a high success rate of non-surgical management. Surgery should be performed if the patient remains unstable after resuscitation or develops symptoms such as gastrointestinal perforation or peritonitis.
Comparison with existing literatureIn the original APSA 2000 version of the guidelines, it was determined that the grade of injury as defined by the AAST was a significant factor in determining the appropriate hospital disposition for children. Specifically, children with grade I to III injuries were admitted to the general ward, while those with grade IV injuries were admitted to the ICU (8). Some studies have demonstrated that children with uncomplicated grade I to II liver or spleen injuries, in the absence of other significant injuries, can be managed with medical observation and discharged from the emergency department without the need for blood transfusions or other specialized interventions (such as surgery) (9).
In contrast, the WSES guidelines (7) suggest that the treatment plan should not be determined based on the classification of splenic injury. Instead, they advocate for the use of physiological parameters as the primary reference data. The WSES classification system categorizes splenic injuries into three distinct groups: mild, moderate, and severe.
Mild splenic injuries are classified as WSES class I and include hemodynamically stable AAST-OIS class I-II blunt and penetrating lesions. Moderate splenic injuries are classified as WSES class II and include hemodynamically stable AAST-OIS grade III blunt and penetrating lesions. Severe splenic injuries are classified as WSES grade III and include hemodynamically stable AAST-OIS grade IV-V blunt and penetrating lesions. Severe splenic injury: The WSES grade IV encompasses hemodynamically unstable AAST-OIS grades I-V blunt and penetrating lesions. It is recommended that the first non-operative management (NOM) attempt be undertaken in patients who are hemodynamically stable and do not have other abdominal organ injuries that require surgical intervention, irrespective of the grade of injury. In contrast, surgical treatment is indicated in cases of hemodynamic instability or other indications for open surgery, such as peritonitis, injury to cavity organs, extra-intestinal clefts, and impaction.
In a similar analysis of the National Trauma Data Bank (NTDB), Nanee and colleagues (10) examined the timing of surgical interventions for BLSI in children. They found that the failure of non-surgical treatment was based on physiological parameters rather than the anatomical severity of the injury.
This conclusion has also been corroborated by the most recent iteration of the APSA guidelines (2023) (4). The APSA guidelines (2023) additionally advise that patients with BLSI who have undergone transfusion of red blood cells but whose vital signs remain unstable should undergo surgical exploration and control of bleeding. Furthermore, to rule out other abdominal injuries that may have contributed to the instability of the patient, surgical exploration should be performed. Moreover, several studies have indicated that hemodynamic status on admission is not a significant prognostic indicator of NOM failure, and thus should not be regarded as an absolute contraindication to NOM (11–15). Our study also adheres to this perspective. As a result of advancements in medical technology, some of the previous therapeutic strategies have been enhanced. The implementation of effective life support techniques and vascular interventions will contribute to a gradual transition in the therapeutic strategies employed for blunt splenic injuries.
Clinical significanceNonoperative management (NOM) is a treatment option that avoids surgical intervention for patients with splenic trauma in the pediatric population. The failure rate for NOM in this patient group is reported to be between 2% and 5% (16, 17). It is noteworthy that evidence suggests that the rate of nonoperative management (NOM) failure is highest at four hours post-admission and then gradually declines over 36 h (16). In general, the majority (72.5%) of cases where NOM is unsuccessful appear to occur within the first week following trauma, with 50% occurring within the first 3–5 days (18). The presence of hemodynamic instability is typically discernible in patients upon admission or within 12 h of the injury (19). Patients with higher Injury Severity Scores (ISS) are more likely to fail nonoperative management (NOM). As evidenced in the literature, the two ISS values significantly associated with NOM failure are greater than 15 (14) or 25 (18). This finding is consistent with the increased risk of associated lesions at higher Injury Severity Scores (ISS). This finding was not reflected in my study data.
NOM appears to be more effective in children than in adults and is therefore more commonly used for pediatric splenic trauma in these patients. This has also been associated with reduced costs and length of hospital stay, reduced need for blood transfusions, vaccinations, and antibiotic treatments, as well as higher immunity and lower infection rates (8, 20–23). The reason for the superior outcomes of NOM in children compared to adults is unclear. However, it is postulated that this may be related to certain unique pediatric characteristics, including a thicker splenic envelope, a higher proportion of myoepithelial cells, and more effective contraction and retraction of small splenic arteries (24–29). Several studies have demonstrated low adherence to APSA guidelines in non-pediatric trauma centers. For further details, please see references (6, 22, 30–34). A higher probability of experiencing non-operative management (NOM) has been demonstrated in pediatric trauma patients treated in specialized centers when compared to those treated in adult trauma centers (22, 30–33). Furthermore, Mooney et al. and Todd et al. have shown that children with splenic injuries are more likely to undergo splenectomy or if treated in an adult trauma center (34, 35).
In children, however, the therapeutic strategy of preserving the spleen is preferred, as the spleen is the largest secondary lymphoid organ, which induces innate and adaptive immune responses against pathogens (36). Splenectomy can result in post-splenectomy-associated menacing infections (OPSI). OPSI is defined as fulminant sepsis, meningitis, or pneumonia caused by Streptococcus pneumoniae (in approximately 50% of cases) (37, 38) and to a lesser extent by Haemophilus influenzae type B and Meningococcus meningitis. OPSI is a medical emergency. The risk of OPSI and associated mortality is highest in the first year following splenectomy, particularly in young children. However, it remains elevated beyond 10 years and may persist throughout life. The incidence of OPSI ranges from 0.5% to 2%, with a mortality rate of 30% to 70%. The majority of deaths occur within the first 24 h. Prompt diagnosis and immediate treatment are essential for reducing mortality rates (37, 39–41). The overall risk of OPSI is higher and the mortality rate is greater in children under five years of age with splenic insufficiency or hypersplenism than in adults (37, 42). The risk in neonates exceeds 30% (39). There is evidence that an embolized spleen (in patients with hypersplenism) may maintain its function, but it is reasonable to assume that it is less effective and that vaccination should continue (43–45). The age of the patient at the time of surgery is directly correlated with the time interval between the onset of sepsis. Younger patients tend to present earlier than those who are older. It has been demonstrated that approximately 50% of all cases of OPSI occur within two years following surgery. However, it is important to note that the risk persists throughout the individual's lifetime (46).
At present, there is a paucity of data from global studies on the treatment and prognosis of pediatric splenic trauma. It is therefore of paramount importance that children are encouraged to opt for non-operative management (NOM) and avoid surgical treatment. This study is aligned with the treatment strategy outlined in the internationally recognized guidelines for non-operative management of traumatic splenic rupture, as proposed by the American Pediatric Surgical Association (APSA) Committee 2023.
Limitations and future directionsIt is important to acknowledge the limitations of this study. Firstly, it should be noted that this study was conducted at a single center, which may limit the generalizability of the results to fully reflect the actual situation in other centers or different populations. Secondly, the sample size was relatively small, which may have weakened the stability of the statistical analysis and increased the risk of the results being influenced by chance. Furthermore, as this study was based on existing clinical data, the completeness and consistency of certain variables may have been compromised, potentially impacting the precision of the analysis. Nevertheless, every effort was made to mitigate the impact of these limitations on the study results through the application of rigorous inclusion criteria and a comprehensive data review. A transparent presentation of these limitations can enhance the credibility of this study and inform the design of future multicenter, large-sample-size prospective studies.
Management pathwayBased on the results of our study, a suggested management pathway is outlined that focuses on making a quick decision on which treatment plan to pursue based on the patient's hemodynamic status at the time of admission in Figure 3, with an indication for AG/AE or surgery. The NOM was initially tested in all conditions, and further research is needed to assess the impact of additional injuries and to more accurately predict the length of hospital stay; however, the algorithm can be used as a guide for initial management of the program and may be expanded in the future with further research.
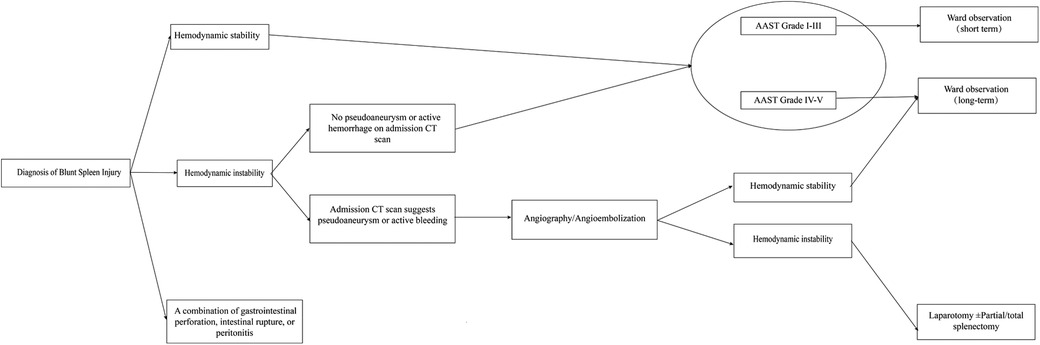
Figure 3. Suggested pathway for management of traumatic blunt splenic injury in children.
ConclusionOur study showed that non-operative management (NOM) is a safe and effective treatment strategy with a high success rate for most children with blunt splenic injury (BSI, especially those who are hemodynamically stable. In addition to reducing surgical complications, non-surgical management reduces children's pain. Surgery should be performed if the patient remains unstable after resuscitation or develops symptoms such as gastrointestinal perforation or peritonitis. Although non-surgical treatment has a high success rate in most patients, minimally invasive techniques such as interventional splenic embolization are effective in reducing the need for splenectomy in selected high-risk cases. Further studies should focus on the long-term efficacy of different treatment strategies and validate the potential of new imaging modalities in conservative management.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Ethics Committee, Wuhan Children's Hospital, Tongji Medical College, Huazhong University of Science and Technology, China. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributionsWW: Data curation, Methodology, Writing – original draft. HL: Investigation, Writing – review & editing. WZ: Formal Analysis, Investigation, Validation, Writing – review & editing. WL: Data curation, Software, Writing – review & editing. HB: Methodology, Supervision, Validation, Writing – review & editing. JY: Investigation, Methodology, Supervision, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
AcknowledgmentsThe authors sincerely thank the administrators of Wuhan Children's Hospital for their valuable contributions to this study. Administrators of the University Medical Center for their valuable contribution to this study.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AbbreviationsAAST, American Association for the Surgery of Trauma; APSA, American Paediatric Surgical Association; β, unstandardised regression coefficient; BSI, blunt splenic injury; CI, confidence interval; CT, computed tomography; NOM, non-operative management; Hb, haemoglobin; trauma; ICU, intensive care unit; ISS, Injury Severity Score; LOS, length of stay; N, number; OM, operative management; OPSI, overwhelming post-splenectomy infection; OR, odds ratio; SD, standard deviation; SPA, splenic pseudo-aneurysms; US, United States; WSES, World Society of Emergency Surgery; GAM, Generalized Additive Model.
References1. Dodgion CM, Gosain A, Rogers A, St Peter SD, Nichol PF, Ostlie DJ. National trends in pediatric blunt spleen and liver injury management and potential benefits of an abbreviated bed rest protocol. J Pediatr Surg. (2014) 49(6):1004–8. doi: 10.1016/j.jpedsurg.2014.01.041
PubMed Abstract | Crossref Full Text | Google Scholar
4. Williams RF, Grewal H, Jamshidi R, Naik-Mathuria B, Price M, Russell RT, et al. Updated APSA guidelines for the management of blunt liver and spleen injuries. J Pediatr Surg. (2023) 58(8):1411–8. doi: 10.1016/j.jpedsurg.2023.03.012
PubMed Abstract | Crossref Full Text | Google Scholar
5. Bairdain S, Litman HJ, Troy M, McMahon M, Almodovar H, Zurakowski D, et al. Twenty-years of splenic preservation at a level 1 pediatric trauma center. J Pediatr Surg. (2015) 50(5):864–8. doi: 10.1016/j.jpedsurg.2014.08.022
PubMed Abstract | Crossref Full Text | Google Scholar
6. Aoki M, Katsura M, Matsumoto S, Matsushima K. Persistent disparities between trauma center types in the management of children with high-grade blunt splenic injuries. World J Surg. (2024) 48(3):568–73. doi: 10.1002/wjs.12072
PubMed Abstract | Crossref Full Text | Google Scholar
7. Coccolini F, Montori G, Catena F, Kluger Y, Biffl W, Moore EE, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg. (2017) 12:40. Published 2017 August 18. doi: 10.1186/s13017-017-0151-4
PubMed Abstract | Crossref Full Text | Google Scholar
8. Stylianos S. Evidence-based guidelines for resource utilization in children with isolated spleen or liver injury. The APSA trauma committee. J Pediatr Surg. (2000) 35(2):164–9. doi: 10.1016/S0022-3468(00)90003-4
PubMed Abstract | Crossref Full Text | Google Scholar
9. Plumblee L, Williams R, Vane D, Zhang J, Jensen A, Naik-Mathuria B, et al. Isolated low-grade solid organ injuries in children following blunt abdominal trauma: is it time to consider discharge from the emergency department? J Trauma Acute Care Surg. (2020) 89(5):887–93. doi: 10.1097/TA.0000000000002899
PubMed Abstract | Crossref Full Text | Google Scholar
10. Nance ML, Holmes JH 4th, Wiebe DJ. Timeline to operative intervention for solid organ injuries in children. J Trauma. (2006) 61(6):1389–92. doi: 10.1097/01.ta.0000244167.45002.58
PubMed Abstract | Crossref Full Text | Google Scholar
11. Bee TK, Croce MA, Miller PR, Pritchard FE, Fabian TC. Failures of splenic nonoperative management: is the glass half empty or half full? J Trauma. (2001) 50(2):230–6. doi: 10.1097/00005373-200102000-00007
PubMed Abstract | Crossref Full Text | Google Scholar
13. Nix JA, Costanza M, Daley BJ, Powell MA, Enderson BL. Outcome of the current management of splenic injuries. J Trauma. (2001) 50(5):835–42. doi: 10.1097/00005373-200105000-00010
PubMed Abstract | Crossref Full Text | Google Scholar
14. Peitzman AB, Heil B, Rivera L, Federle MB, Harbrecht BG, Clancy KD, et al. Blunt splenic injury in adults: multi-institutional study of the eastern association for the surgery of trauma. J Trauma. (2000) 49(2):177–89. doi: 10.1097/00005373-200008000-00002
PubMed Abstract | Crossref Full Text | Google Scholar
15. Malhotra AK, Latifi R, Fabian TC, Ivatury RR, Dhage S, Bee TK, et al. Multiplicity of solid organ injury: influence on management and outcomes after blunt abdominal trauma. J Trauma. (2003) 54(5):925–9. doi: 10.1097/01.TA.0000066182.67385.86
PubMed Abstract | Crossref Full Text | Google Scholar
16. Holmes JH 4th, Wiebe DJ, Tataria M, Mattix KD, Mooney DP, Scaife ER, et al. The failure of nonoperative management in pediatric solid organ injury: a multi-institutional experience. J Trauma. (2005) 59(6):1309–13. doi: 10.1097/01.ta.0000197366.38404.79
PubMed Abstract | Crossref Full Text | Google Scholar
17. Sharma OP, Oswanski MF, Singer D, Raj SS, Daoud YA. Assessment of nonoperative management of blunt spleen and liver trauma. Am Surg. (2005) 71(5):379–86. doi: 10.1177/000313480507100503
PubMed Abstract | Crossref Full Text | Google Scholar
18. McIntyre LK, Schiff M, Jurkovich GJ. Failure of nonoperative management of splenic injuries: causes and consequences. Arch Surg. (2005) 140(6):563–9. doi: 10.1001/archsurg.140.6.563
PubMed Abstract | Crossref Full Text | Google Scholar
19. Thompson SR, Holland AJ. Evolution of non-operative management for blunt splenic trauma in children. J Paediatr Child Health. (2006) 42(5):231–4. doi: 10.1111/j.1440-1754.2006.00843.x
PubMed Abstract | Crossref Full Text | Google Scholar
20. McVay MR, Kokoska ER, Jackson RJ, Smith SD. Throwing out the “grade” book: management of isolated spleen and liver injury based on hemodynamic status. J Pediatr Surg. (2008) 43(6):1072–6. doi: 10.1016/j.jpedsurg.2008.02.031
PubMed Abstract | Crossref Full Text | Google Scholar
21. Martin K, Vanhouwelingen L, Bütter A. The significance of pseudoaneurysms in the nonoperative management of pediatric blunt splenic trauma. J Pediatr Surg. (2011) 46(5):933–7. doi: 10.1016/j.jpedsurg.2011.02.031
PubMed Abstract | Crossref Full Text | Google Scholar
23. Bond SJ, Eichelberger MR, Gotschall CS, Sivit CJ, Randolph JG. Nonoperative management of blunt hepatic and splenic injury in children. Ann Surg. (1996) 223(3):286–9. doi: 10.1097/00000658-199603000-00009
PubMed Abstract | Crossref Full Text | Google Scholar
24. Muehrcke DD, Kim SH, McCabe CJ. Pediatric splenic trauma: predicting the success of nonoperative therapy. Am J Emerg Med. (1987) 5(2):109–12. doi: 10.1016/0735-6757(87)90085-4
PubMed Abstract | Crossref Full Text | Google Scholar
25. Delius RE, Frankel W, Coran AG. A comparison between operative and nonoperative management of blunt injuries to the liver and spleen in adult and pediatric patients. Surgery. (1989) 106(4):788–93.2799654
PubMed Abstract | Google Scholar
26. Lynch JM, Ford H, Gardner MJ, Weiner ES. Is early discharge following isolated splenic injury in the hemodynamically stable child possible? J Pediatr Surg. (1993) 28(10):1403–7. doi: 10.1016/S0022-3468(05)80336-7
PubMed Abstract | Crossref Full Text | Google Scholar
27. Konstantakos AK, Barnoski AL, Plaisier BR, Yowler CJ, Fallon WF Jr, Malangoni MA. Optimizing the management of blunt splenic injury in adults and children. Surgery. (1999) 126(4):805–13. doi: 10.1016/S0039-6060(99)70139-X
PubMed Abstract | Crossref Full Text | Google Scholar
29. Rodrigues CJ, Sacchetti JC, Rodrigues AJ Jr. Age-related changes in the elastic fiber network of the human splenic capsule. Lymphology. (1999) 32(2):64–9.10389113
PubMed Abstract | Google Scholar
30. Leinwand MJ, Atkinson CC, Mooney DP. Application of the APSA evidence-based guidelines for isolated liver or spleen injuries: a single institution experience. J Pediatr Surg. (2004) 39(3):487–90. doi: 10.1016/j.jpedsurg.2003.11.014
PubMed Abstract | Crossref Full Text | Google Scholar
31. Murphy EE, Murphy SG, Cipolle MD, Tinkoff GH. The pediatric trauma center and the inclusive trauma system: impact on splenectomy rates. J Trauma Acute Care Surg. (2015) 78(5):930–4. doi: 10.1097/TA.0000000000000610
PubMed Abstract | Crossref Full Text | Google Scholar
32. Sims CA, Wiebe DJ, Nance ML. Blunt solid organ injury: do adult and pediatric surgeons treat children differently? J Trauma. (2008) 65(3):698–703. doi: 10.1097/TA.0b013e3181574945
PubMed Abstract | Crossref Full Text | Google Scholar
33. Stylianos S, Egorova N, Guice KS, Arons RR, Oldham KT. Variation in treatment of pediatric spleen injury at trauma centers versus nontrauma centers: a call for dissemination of American pediatric surgical association benchmarks and guidelines. J Am Coll Surg. (2006) 202(2):247–51. doi: 10.1016/j.jamcollsurg.2005.10.012
PubMed Abstract | Crossref Full Text | Google Scholar
34. Mooney DP, Rothstein DH, Forbes PW. Variation in the management of pediatric splenic injuries in the United States. J Trauma. (2006) 61(2):330–3. doi: 10.1097/01.ta.0000226167.44892.1d
PubMed Abstract | Crossref Full Text | Google Scholar
35. Todd SR, Arthur M, Newgard C, Hedges JR, Mullins RJ. Hospital factors associated with splenectomy for splenic injury: a national perspective. J Trauma. (2004) 57(5):1065–71. doi: 10.1097/01.TA.0000103988.66443.0E
PubMed Abstract | Crossref Full Text | Google Scholar
36. Casciani F, Trudeau MT, Vollmer CM Jr. Perioperative immunization for splenectomy and the surgeon’s responsibility: a review. JAMA Surg. (2020) 155(11):1068–77. doi: 10.1001/jamasurg.2020.1463
留言 (0)