This work may not be copied, distributed, displayed, published, reproduced, transmitted, modified, posted, sold, licensed, or used for commercial purposes. By downloading this file, you are agreeing to the publisher’s Terms & Conditions.
Psychogenic nonepileptic seizures (PNES) are characterized by paroxysmal motor, nonmotor, or behavioral alterations resembling epileptic seizures without electroencephalogram (EEG) correlates,1 which are observed in 5%–10% of epilepsy outpatients and in 20%–40% of epilepsy inpatients.2 Functional neurological symptoms affect up to one-third of patients seeking neurologist evaluation. Depression, posttraumatic stress disorder, and panic disorder are the prevailing comorbid psychiatric diagnoses observed in patients with PNES.3–6
Functional neurological disorders encompass diverse phenotypes that can lead to substantial impairment. Among the most frequently encountered presentations are functional seizures, which are paroxysmal events resembling epileptic seizures without corresponding EEG activity,7 and functional movement disorders, characterized by the presence of abnormal, involuntary, hypokinetic, or hyperkinetic movements that cannot be explained by known underlying pathology.8 Some research highlighted microstructural changes in limbic and associative fiber bundles related to salience, defensive behaviors, and emotion regulation. Reduced integrity of the stria terminalis/fornix and medial forebrain bundle was found to be linked to disability and illness duration.9,10 Psychological interventions, including cognitive behavioral therapy (CBT), offer moderate improvement in quality of life for patients with functional seizures but do not improve seizure frequency.11,12 Studies13,14 have demonstrated that combining sertraline with CBT effectively reduces functional seizures, enhancing quality of life and functioning. Short-term psychodynamic psychotherapy has shown improvements across several domains. However, limited access to trained therapists poses a challenge to widespread use.15 Another study16 demonstrated significant benefits from retraining and control therapy (ReACT) based on habit reversal. Among patients with PNES, adherence to psychotherapy resulted in reduced PNES frequency, improved quality of life, and decreased emergency department visits. Providers should collaborate to develop novel interventions to promote adherence.17 According to a study,18 the application of high frequency repetitive transcranial magnetic stimulation (rTMS) targeting the right temporoparietal junction holds promise as a potential treatment strategy. However, further controlled studies are required to explore the potential effectiveness and neural mechanisms underlying its efficacy.18 Limitations of the studies include sample size, internal validity, and selection bias.
Despite progress made in treating functional neurological disorders, uncertainties persist regarding the most effective treatment setting, duration, frequency, and intensity. Additionally, preliminary studies have indicated the potential benefits of neuromodulation techniques such as rTMS.19,20 This report aims to contribute to the existing medical literature by adding a patient case and providing insights into the understanding of PNES and the potential treatments currently available.
Case ReportA 64-year-old man with a medical history of polio in infancy with right arm weakness, cluster headaches, and hypertension presented to the neurology clinic for gait disturbances. The patient stated he has had increased gait and balance issues that started 4 years ago. He had tingling in his feet, occasional double vision that could last for the whole day, multiple falls, and syncopal episodes from which he quickly recovered and was able to stand up almost immediately afterward. His social history included drinking 8–10 beers a day, but he quit 1 year ago as his gait got worse, tobacco smoker, and history of speed, marijuana, and cocaine use. He worked as a safety manager in the trucking industry. He had a history of cervical spine surgery. The physical examination was unremarkable except for right upper atrophy due to polio. His short- and long-term memory was intact. Magnetic resonance angiography (MRA) and magnetic resonance imaging (MRI) of the brain were ordered due to concerns for vertebrobasilar insufficiency.
The patient’s visit to the neurology clinic was 1 month after being admitted to the hospital for chest pain, wherein cardiac workup was negative. He also had been admitted to the psychiatric ward and diagnosed with anxiety. His difficulty with balance and instability was every day now. He endorsed a lot of stress at work. His MRI and MRA imaging tests were negative. Complete metabolic panel, complete blood count, thyroid stimulating hormone with reflex T4, rapid plasma reagin, vitamin B12, folate, serum protein electrophoresis, erythrocyte sedimentation rate, antinuclear antibody test, and electromyography were ordered, all of which were unremarkable. An MRI cervical and lumbar spine scan was ordered to assess for stenosis or structural abnormality, which was also negative.
He was referred to a movement disorder clinic at a tertiary care center for further testing. No diagnosis was made. He was started on thiamine due to his alcohol history and started physical therapy, which helped significantly. The neurologist thought his symptoms might be explained by Wernicke–Korsakoff due to his alcohol history. Bupropion 150 mg daily was also added to his medications. The patient’s gait continued to worsen. Human immunodeficiency virus, vitamin E, serum copper, thiamine, celiac disease panel, angiotensin-converting enzyme level, and paraneoplastic cerebellar degeneration panel were ordered, and the patient was advised to avoid caffeine and alcohol since they made his symptoms worse. The patient also had 3 convulsive episodes and was started on lamotrigine. He had transitioned from the use of a cane to a front-wheeled walker in a few years. Psychogenic factors for his symptoms were suspected.Neuropsychology testing was ordered, which attributed his cognitive complaints to psychological factors and functional complaints to a somatoform disorder. He was diagnosed with functional/ psychogenic gait disorder and PNES. CBT was recommended, and the patient was reassured at all subsequent visits. He continued to see a psychiatrist for his depression and anxiety. He was diagnosed with conversion disorder and somatic symptom disorder.
DiscussionThis report presents a unique clinical scenario characterized by initial subjective symptoms such as gait and balance problems, occasional double vision, tingling sensations in the feet, syncope, and multiple falls. Extensive blood tests, imaging studies, and electromyography yielded normal results, except triceps brachii atrophy attributed to polio (Table 1). Subsequently, the patient received a diagnosis of anxiety disorder, which was followed by a worsening of somatic symptoms and ultimately the presentation of seizures, leading to a delayed diagnosis of PNES. PNES poses a complex and multifaceted challenge for health care professionals, necessitating a comprehensive understanding of their clinical, diagnostic, and therapeutic aspects. These seizures are observed in 5%–10% of epilepsy outpatients and 20%–40% of epilepsy inpatients.2 Notably, patients with functional neurological disorders, including PNES, utilize a significant amount of emergency and inpatient health care resources, surpassing the burden of other complex neurological conditions. Surprisingly, they receive limited inpatient rehabilitation and psychiatric care despite the high associated costs. The annual expenses associated with functional neurological disorders are substantial and growing at a faster rate than other neurological disorders, which underscores the need for medical education and health care policy reform to enhance care for this vulnerable population and reduce costly hospital admissions.6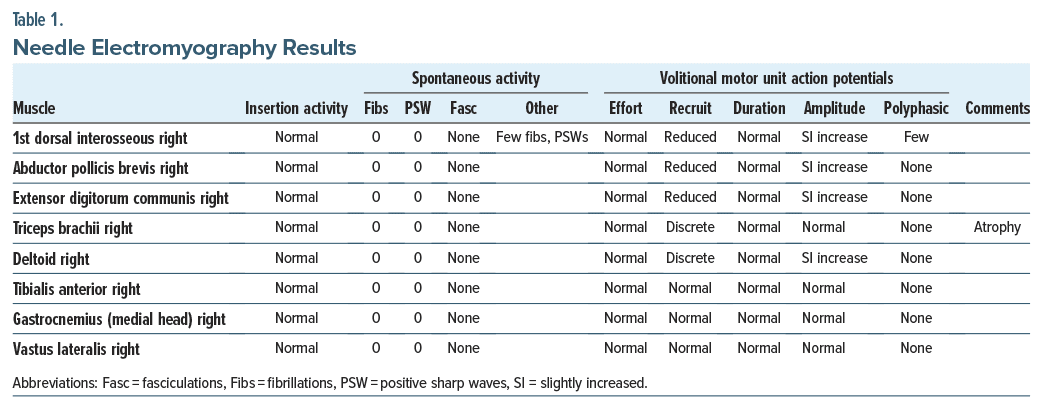
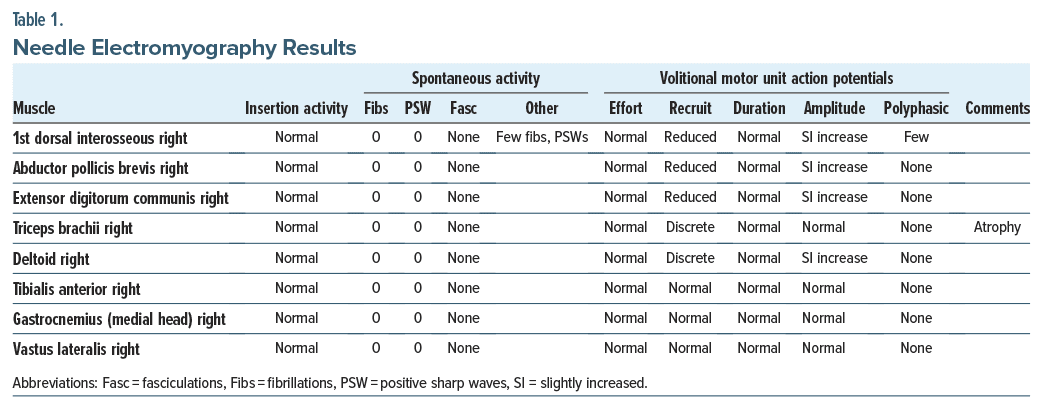
Table 2 shows pharmacologic and nonpharmacologic treatments described by previous studies. The pilot randomized controlled trial by La France et al14 revealed significant seizure reduction and improved comorbid symptoms and global functioning with CBT-informed psychotherapy for PNES with and without sertraline. There were no improvements in the sertraline-only or treatment-as-usual arms. This study14 supports the use of manualized psychotherapy for PNES and the successful training of mental health clinicians in the treatment. This finding is also supported by 2 other clinical trials and our case report, which showed CBT is more effective than standard medical care alone and would help reduce seizure frequency and improve psychiatric symptoms, psychosocial functioning, and quality of life.15,16 According to Fobian et al,21 ReACT is effective for pediatric PNES. ReACT also works quickly to reduce PNES, with participants reaching PNES cessation after fewer than 5 sessions on average. The success rate of ReACT is higher than in studies using CBT for PNES in adults.21 Mayor et al22 revealed psychodynamic interpersonal therapy reduced seizure frequency and health care utilization, but the study was uncontrolled. Kelley et al24 suggest that EMDR can be used as a treatment modality for trauma-based PNES; however, a larger sample size is required to establish the efficacy of this intervention. Paradoxical intention therapy sessions, hypnotherapy, mindfulness-based therapy, and combined therapy of presenting diagnosis, psychoeducation, seizure reduction behavioral techniques, and coping with past and present stressors are suggested by a few studies,19,20,22–24 but larger sample size studies and controlled studies are needed to evaluate the efficacy of these nonpharmacologic approaches. High-frequency rTMS on the right temporoparietal region is a promising safe, efficient, acceptable, and potentially effective treatment for functional limb weakness, leading to improvements in core symptoms and potentially other important outcome domains, and controlled studies are needed to validate the efficacy of the intervention.18,19
Table 3 shows the results of the studies by Leong et al27 and Blumer et al,28 which support the use of electroconvulsive therapy (ECT) in pseudoneurological symptoms. These studies provide preliminary evidence that ECT may be beneficial in the treatment of PNES-related symptoms. However, it is essential to recognize the limitations of these studies, including small sample sizes, lack of control groups, and retrospective designs. These limitations highlight the need for larger, well-designed clinical trials to confirm these findings and to better understand the role of ECT in the management of PNES. Additionally, it is crucial for future research to explore the mechanisms by which ECT may have a therapeutic effect on PNES and to assess its long-term safety and durability of response. Overall, while these studies offer promising insights, more comprehensive and rigorous investigations are required to establish ECT as a standard and evidence-based treatment option for individuals with PNES.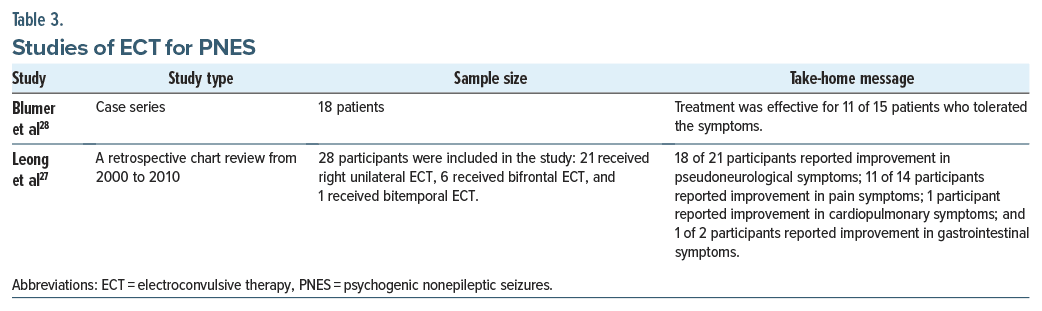
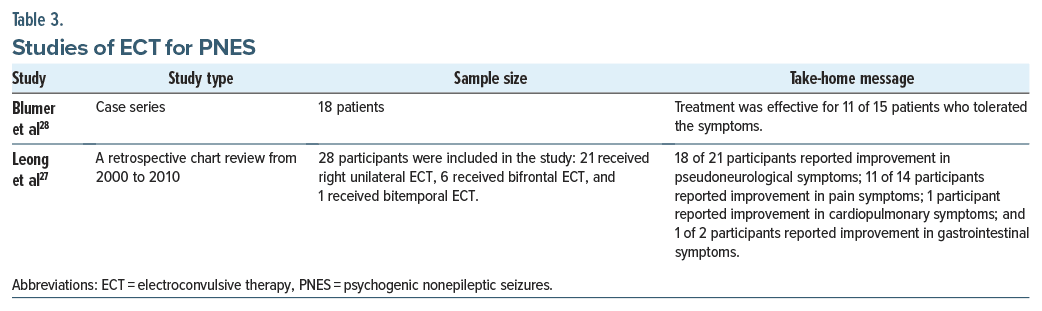
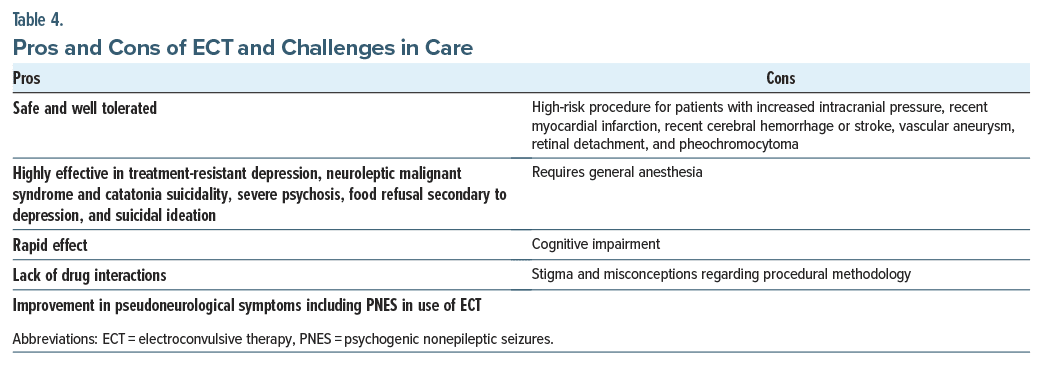
Table 4 lists the challenges in care and advantages of ECT to be taken into account when considering it as a reliable treatment option for PNES. ECT is a medical procedure that has been used for several decades in the treatment of various psychiatric conditions. Its effectiveness and safety have been the subject of both support and controversy. ECT is a medical procedure that offers distinct advantages, particularly in treating severe and treatment-resistant mental health conditions. However, it is not without its drawbacks, including the need for careful patient selection, the potential for cognitive side effects, and the presence of societal stigma. The decision to use ECT should be made on a case-by-case basis, weighing the potential benefits against the associated risks and considering the specific needs and circumstances of the patient. Additionally, ongoing research is necessary to further refine the use of ECT and minimize its limitations while maximizing its therapeutic potential.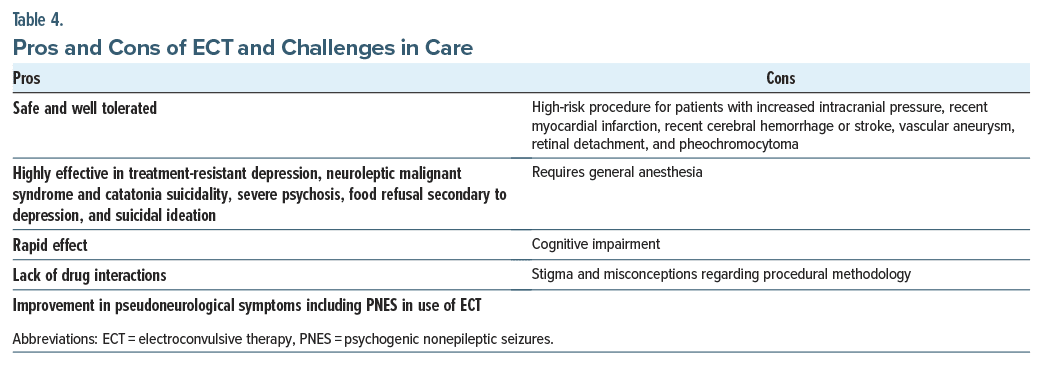
Improving the diagnosis and treatment of PNES presents a multifaceted challenge. One avenue of progress lies in the development of more precise diagnostic tools, such as biomarkers or advanced neuroimaging techniques, which could enhance the early and accurate identification of PNES cases. Additionally, raising awareness among both health care professionals and the general public is essential to combat the stigma surrounding PNES and facilitate timely diagnosis and appropriate treatment. Tailoring therapeutic approaches with targeted psychotherapies, designed specifically for PNES management, holds promise for improving outcomes by addressing the underlying psychological factors contributing to the condition. Exploring the potential effectiveness of pharmacologic interventions represents another avenue to broaden treatment options, particularly for individuals who do not respond adequately to psychotherapy alone. Despite these promising directions, challenges persist, including the absence of definitive biomarkers, variability in treatment responses among patients, underdiagnosis, and the need for further evidence-based treatments to comprehensively address the complexities of PNES management.
ConclusionComplexities of diagnosing and managing PNES highlight the importance of considering psychogenic factors in patients with unexplained physical symptoms. The interdisciplinary approach involving neurology and psychiatry allows for a comprehensive evaluation and tailored therapeutic interventions. More controlled studies are needed to explore targeted psychotherapies and their benefit in treating PNES patients.
Published Online: October 31, 2024. https://doi.org/10.4088/PCC.24cr03753
© 2024 Physicians Postgraduate Press, Inc.
Prim Care Companion CNS Disord 2024;26(5):24cr03753
Submitted: April 2, 2024; accepted July 17, 2024.
To Cite: Tammineedi SN, Mukesh S, Singer E, et al. Psychogenic nonepileptic seizures: a complex diagnosis and comprehensive review. Prim Care Companion CNS Disord. 2024;26(5):24cr03753.
Author Affiliations: Kamineni Institute of Medical Sciences, Nalgonda, Telangana, India (Tammineedi); Liaquat University of Medical and Health Sciences, Jamshoro, Pakistan (Mukesh); Department of Emergency Medicine, The University of Texas MD Anderson Cancer Center, Houston, Texas (Singer); Department of Medicine, University of Conakry, Faculty of Sciences and Technics of Health, Dixin, Conakry, Guinea (Diallo); Touro University College of Osteopathic Medicine, Henderson, Nevada (Tar); Caribbean Medical University, Willemstad, Curaçao (Kapil); Faculty of Medicine, University of Medicine and Pharmacy at Ho Chi Minh City, Vietnam (Le Duc); Department of Radiology, Kuwait Institute for Medical Specializations, Kuwait City, Kuwait (Fathi); Medical College, Gandhinagar, Gujarat, India (Chhayani); Stroke Program at LIJ Forest Hills, Department of Neurology, Zucker School of Medicine at Hofstra/Northwell, Hempstead, New York (Arora); Department of Geriactrics, Hackensack University Medical Center, Hackensack, New Jersey (Jain); Department of Neurology, Medical University of South Carolina, Columbia, South Carolina (Singla).
Corresponding Author: Sai Niharika Tammineedi, MBBS, Kamineni Institute of Medical Sciences, Narketpally, Nalgonda, Telangana 508254, India ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: None.
Previous Presentation: Presented as a poster at the American Medical Association Research Symposium; October 18, 2023; virtual.
Patient Consent: Informed consent was received from the patient to publish the case report, and information has been de-identified to protect anonymity.
留言 (0)