The use of music as therapy has ancient origins, initially intertwined with myths, cosmologies, and theories of the ancient world. In many myths and popular narratives, sound is often conceived as the primordial substance from which the universe originates. Early historical references include Egyptian medical papyri dating back to before 1,500 BCE, Book III of Plato’s Republic, and the Arab-Jewish medical tradition (1–8). Over time, musical therapies evolved from shamanic practices to tribal medicine and tarantism (9).
The development and formalization of music therapy (MT) began with the establishment of the first academic program at Michigan State University in 1944, followed by the creation of the National Association for Music Therapy in 1950 (10). This professionalization continued with the founding of the British Society for Music Therapy by Juliette Alvin in 1958, expanding the reach of MT in Europe. In 1985, in response to the increase in experiences and the growing proliferation of MT associations, the World Federation of Music Therapy (WFMT) was established. This organization has played a pivotal role in formalizing the discipline by defining ethical, deontological, and professional standards, as well as promoting a shared definition of MT at the international level (11). To support this process of disciplinary structuring, during the 9th World Congress of Music Therapy in 1999, five main models of MT practice were formally recognized, developed by authoritative figures in the scientific community such as Bonny (12), Priestley (13), Nordoff and Robbins (14), Benenzon (15), and Madsen (16).
With the evolution of MT methodologies, techniques have been further refined through the integration of neuroscientific knowledge and the use of new musical technological instruments. In this context, scientific reviews have highlighted that musical improvisation is a prevalent strategy in numerous MT methodologies, as it facilitates emotional expression and increases therapeutic effectiveness (17–19).
These characteristics are identifiable in the approaches of Priestley and Nordoff-Robbins, whose therapeutic models closely align with our clinical practice, being based on musical improvisation and the creation of compositions specifically tailored to the patient’s needs (20). In parallel, the work of Anne Riordan and Kenneth E. Bruscia has introduced dance as a complementary therapeutic element in musical improvisation, demonstrating how the integration of this dimension promotes improvements not only in emotional and social skills but also in the patient’s cognitive and motor abilities (21).
Although the use of musical improvisation promotes creative expression, it introduces a degree of unpredictability that may not be suitable for all patients. Indeed, the absence of a predictable structure can make it challenging to maintain a clear therapeutic focus, potentially compromising the effectiveness of the intervention.
Bruscia has also highlighted, from an applied perspective, a range of risks and limitations associated with the patient. These include the need for adequate cognitive and sensorimotor skills to engage in musical improvisation. There is also the risk of adverse psychological reactions to music, such as hallucinations, difficulties in auditory processing, and undesirable physical responses. Other side effects include withdrawal, obsessions, compulsions, and sensory overload. Lastly, the author advises paying attention to interpersonal dynamics that may be threatening to the patient (22).
To prevent the risks associated with improvisation in MT, it is essential to tailor sessions according to the patient’s psychophysical condition, ensuring safe participation and preventing frustration. It is equally important to carefully monitor adverse psychological reactions and side effects, selecting musical materials with precision, and adjusting the intensity of the treatment. The therapist must meticulously consider the patient’s sociocultural context, respecting musical traditions to prevent cultural dissonance that could undermine the effectiveness of the therapeutic intervention. Contextually, the integration of innovative musical technologies can significantly enhance the patient’s auditory processing and mitigate the impact of potentially disruptive sound stimuli.
Scientific reviews highlight how such technologies can significantly enhance the therapeutic potential of MT. Consequently, these technologies applied to electronic composition can be tailored to meet the specific needs of patients (23–27). Supporting this, Farnan defines composition as “custom designed” music (25). Jones supports the value of composition, emphasizing the need for further research on best-practice models for clinical objectives (26). Barta et al. demonstrate the value of real-time music composition in the rehabilitation of patients with Parkinson’s disease (27). These findings are supported by the review conducted by Vinciguerra et al., which demonstrates that MT improves motor function and cognitive abilities in patients diagnosed with Parkinson’s and Alzheimer’s diseases, as well as stroke. This result emphasizes the significance of musical temporal structures in enhancing motor coordination and memory. In addition to its applications in neurodevelopmental disorders, MT has also demonstrated significant non-pharmacological benefits in managing chronic neurological diseases such as multiple sclerosis. The authors highlighted the role of MT in enhancing emotional well-being and cognitive functions in multiple sclerosis patients, demonstrating its broad therapeutic potential in neurorehabilitation (28).
Another aspect considered in our study is the limited number of research studies on MT in a multisensory context. Although some reviewed studies report sound or compositional interactions in relation to the environment, there are no specific references concerning the interactions between the environment, musical activities, and intervention methodologies (29–34). Marti et al. evaluated the effectiveness of MT therapeutic protocols in a multisensory environment for the treatment of dementia (29). Maseda et al. and Latham et al. further explored the effectiveness of non-pharmacological interventions in multisensory environments on patients with dementia, using different therapeutic approaches. Maseda et al. explored the use of unstructured stimuli autonomously chosen by patients, while Latham et al. evaluated Simard’s Namaste Care program, which combines scents, lighting, sensory objects, and music to create a relaxing atmosphere, employing personalized playlists only when necessary (30, 31). However, the studies present methodological limitations, particularly regarding the interaction between multisensory stimulation and the musical component. Lee and Li reported a school study focused on the impact of therapeutic musical activities in a multisensory environment for children with multiple disabilities, aimed at promoting positive emotional development (32). Cappelen and Andersson introduced an interactive multisensory environment that integrates music composition, design with the therapeutic principles of music, MT, and sensory integration to promote health through technology (33). Challis et al. presented two case studies that question current trends in the design and allocation of resources for multisensory environments, emphasizing the creation of functional spaces rather than simple technology aggregates (34).
The literature review has identified significant biases in the field of MT, including the limited application of real-time personalized electronic composition techniques.
Moreover, most existing approaches focus on environmental setup and the use of musical instruments, without fully considering the role of the environment as a sensory amplifier (2, 12, 15, 22). When used correctly, the environment could function as a sensory “mixer,” modulating and enhancing the effectiveness of the intervention.
Finally, although the Euterpe Method (EM) has demonstrated its efficacy in the context of both neurorehabilitation and telerehabilitation (35, 36), subsequent reviews have raised both growing interest and significant criticisms (37–48). Specifically, Paterson et al. have emphasized the importance of implementing telerehabilitation interventions based on MT to address new challenges in modern medicine (39). Concurrently, Le Vu et al. have highlighted the complexity of implementing EM, as it requires interdisciplinary training for music therapists, an aspect that currently limits the method’s replicability and widespread adoption (41).
To address the identified biases, this article proposes targeted interventions aimed at enhancing replicability and interdisciplinary training for music therapists through the use of original EM algorithms and procedures. These algorithms include EM Hospital-based (providing specific clinical goals for each patient), EM Active (live music, real-time compositions, improvisation, interactive workshops), EM Receptive (listening to personalized compositions and electronic music), and EM Telerehabilitation (remote delivery of MT). Furthermore, integrating a multisensory space with compositional activities represents an innovative strategy to amplify MT’s effectiveness, improving the interaction between the environment and therapeutic intervention.
The integration of neuroscience, music, and technology not only opens new perspectives for personalized and clinically optimized therapeutic interventions, but also lays the groundwork for structured innovation in pediatric rehabilitation.
1.1 The Euterpe methodThe methodology referred to as Euterpe has a dual foundation. Culturally, Euterpe is one of the nine Muses of Greek mythology, the daughter of Zeus and Mnemosyne, and the protector of music. The name, derived from the Greek words ἐυ (good) and τέρπεω (pleasure), means “she who gives joy.” Pragmatically, it reflects the intent to develop a methodological approach tailored to the individual needs of patients and therapeutic goals, in close collaboration with the music therapist and the medical team.
EM is designed for children with neurodevelopmental disorders, actively involving parents, typically the mother, during therapy sessions.
EM uses original, customized Compositional Sound Interventions (CSI) and structured therapeutic activities based on specific algorithms. Music and CSI form the foundation for creating Personalized Therapeutic Compositions (PTCs), which constitute the core of EM therapy.
Therefore, PTCs can be defined as a series of articulated processes of specific sound stimuli, technically processed and adapted to the patient’s individual needs during therapy. These sound processes are simultaneously associated with multisensory stimulation within an enriched environment.
In order to delve deeper into the process of PTC realization and implementation, we feel it is essential to present a brief excursus.
As widely acknowledged, music has a significant impact on mood and emotions. This effect occurs because sound stimuli exert a sensory and psychological response in each individual, inducing a corresponding emotional reaction (49–51).
In support of the above, anthropologist Alan Parkhurst Merriam identifies 10 functions for music, representing opportunities to express emotions, thoughts and ideas (5).
Numerous musicological studies affirm that a musical work is structured as a series of more or less lengthy musical segments, arranged in a functional “hierarchy” that determines their role and importance (52, 53).
These studies suggest an affinity between personalized musical composition and the creation of a therapeutic context that resonates with the patient’s experiences, needs, and aspirations.
In the creation of PTCs, the compositional sound material derived from the patient’s “positive” reactions assumes a “hierarchical perceptual function.” This function reflects the patient’s ability to interpret and respond to musical stimuli according to their subjective perceptions, which are intimately tied to their somatosensory condition and psychophysiological state.
The implementation of the PTC develops through an articulated temporal flow, composed of “sound cells,” compositional structures, and specific timbres. These components impart a dialogic quality to the PTC, in which sound sequences alternate in a rhythm of “coming and going,” presenting the composition as a sound dialog of questions and answers, clearly distinguishing a “before” and “after.” This compositional development does not conform to predetermined musical forms, as it is solely guided by the therapeutic question: “Does this intervention improve the patient’s quality of life?” However, it is noteworthy, upon subsequent musicological analysis, that PTCs reveal similarities with pre-existing musical forms and musicological philosophies. This highlights how musical perception is an acquired anthropological construct, reflected in specific compositional processes. Below are examples that overlap with the compositional techniques of PTCs.
During EM therapy, a relevant example is guiding the patient to listen to silence and the sounds produced by the environment. This approach aligns with John Cage’s philosophical idea of 4′33″, a composition consisting entirely of silence, where the listener is confronted only with environmental sounds, the only tangible source of “music.” The absence of sound in favor of casual and incidental sounds (such as the audience’s breathing or noises inside and outside the auditorium) becomes the new sound material (54). Even more significant is Cage’s composition Imaginary Landscape No. 4, performed with 12 radios and 24 performers, where the listening result is always unique and unrepeatable due to the simultaneous overlap of sounds, words, and random noises from radio stations. This concept is similar to that of PTCs, with the distinction that every sound variation produced by the patient in the multisensory environment in which therapy takes place is recorded and played back as a new compositional incipit.
A similarity between the compositional structure of PTCs and Lerdahl and Jackendoff’s Generative Theory of Tonal Music lies in the use of generative principles to organize and interpret music. This theory, based on the hierarchy of tensions and relaxations, as well as processes of continuity and discontinuity, finds a parallel in PTCs, where sound events like the mother’s prosodic voice and the patient’s reactions alternate in a rhythmic loop, creating dynamic contrasts between tension and relaxation (55–57).
Additionally, minimalist styles from composers such as Terry Riley, Steve Reich, Philip Glass, and John Adams can be identified, as they conceptualize a “gradual musical process” based on repetition, variation, and structural prolongation of rhythmic and melodic segments (58).
Similarly, the cluster technique employed by György Ligeti (59) can be recognized. This approach consists of modifying through “addition” or “subtraction” complexes of chromatic and diatonic sounds, as nuances of a sound spectrum, creating micro-polyphonies that alternate in a compositional continuum.
Finally, the choice and use of electronic music for PTCs in EM therapy. It is important to note that electronic music originates from recording, listening, and developing electroacoustic instruments.
In fact, electronic composition is directly related to the sound material, unlike traditional composition, which uses symbolic writing (notation) to represent the gestures to be performed on a musical instrument to play a song.
The evolution of electronic composition has traversed research sector, progressing through stages such as phonography (a means of capturing and reproducing sounds while keeping them identical), radiophony (enabling real-time live transmissions over long distances), and electric and electronic lutherie (offering innovative musical instruments). The evolution of computers has made it possible to combine the characteristics of phonography, radiophony, and electronic lutherie into electronic composition. Finally, ongoing developments in computer technology, research, and new tools have consistently advanced the sector of electronic music, drawing attention and encouraging scientific studies across a wide range of disciplines, including MT.
Electronic music was born in Cologne in 1950 by Herbert Eimert. The growing interest in this domain among scholars led to the establishment of significant research centers, notably: the Studio di Fonologia Musicale, founded by Bruno Maderna and Luciano Berio in Milan in 1955 (60); the Équipe de mathématique et d’automatique musicales (EMAMu), founded by Xenakis in 1966 (61); and the Institut de coordination acoustique/musique (IRCAM), established by Boulez in Paris in 1975 (62).
Key advantages of using electronic music in MT include the creation of therapeutic orchestral scores with virtual instruments and real-time interaction with the patient. Additionally, electronic music enables customization of sounds and synthesis effects tailored to the patient’s psychophysiological conditions and clinical objectives.
Examining the context of the previous discussion regarding the scientific-musical excursus that encompasses the emerging forms derived from PTC and the importance of electronic composition, a reflection arises on the context in which MT interventions take place.
The spaces dedicated to musical listening in various contexts are continuously evolving, influenced by research on acoustic techniques. It is essential to deepen the understanding of the environments in which MT activities occur, as these contexts can significantly impact the effectiveness of the MT sessions.
According to Altenmüller and Schlaug, music is not merely an auditory input but represents one of the most enriched experiences in terms of emotional, sensory, and cognitive dimensions, influencing and modulating the activity of brain regions involved in multisensory and motor integration, including frontal, parietal, and temporo-occipital regions (63). This multisensory brain activation is closely associated with the phenomenon of neuroplasticity. Neuroplasticity, or cortical remapping, involves reconnecting previously disconnected brain areas through new neural connections or strengthening existing ones. This process occurs in response to learning new skills, memory formation, recovery from injuries, and experiences of sensory deprivation or environmental enrichment (64).
Based on these studies (63, 64), the environment is configured as a determining factor that influences and contributes osmotic ally to the effectiveness of therapeutic sessions, facilitating the interaction between external stimuli and the patient’s psychophysiological processes.
There is limited research investigating the correlation between sound and environment in MT practice. However, examined studies have shown that the acoustic environment can modulate individuals’ emotional and behavioral responses, thus impacting MT effectiveness (65, 66).
Our research aims to implement sound activities into MT, recognizing that these activities extend beyond mere sound production, engaging all the senses. According to a study by Lee and Li (32), multisensory musical experiences can promote greater participation and emotional engagement, thereby enhancing the therapeutic effects of music.
Furthermore, it is important to consider the role of physical and social environments in facilitating or hindering the therapeutic process. Research by Wigram, Pedersen, and Bonde has demonstrated that the design of spaces dedicated to MT can affect group dynamics and perceptions of social support, thereby improving the overall efficacy of the sessions (67).
Based on the above considerations, EM sessions are conducted in a specially designed environment known as the “Synesthesia Room” (SR), equipped with specific materials and instruments aimed at providing complex and appropriate sensory stimulation. The therapeutic activity, referred to as “Sound in Multisensory Stimulation,” integrates the environment through the control and customization of sound stimuli, facilitating the simultaneous overlay of multiple sensory stimuli. The goals of the therapy are to improve, motivate, create, implement, and learn behaviors in the socio-communicative, affective-relational, psychomotor, cognitive, and neuropsychological domains (68).
Currently, the EM is employed in various clinical settings, including neurorehabilitation units, oncology departments in the Middle East and Europe, and MT associations.
1.2 The Euterpe method and the environmentThe SR is an environment specifically designed and structured for EM therapy, which employs multisensory integration simultaneously with MT activities, considering it an integral part of the therapy.
The environment and sensory have been the subject of study and research since the 19th century; however, it was in the 1970s that the first rooms equipped for sensory stimulation through visual, auditory, tactile, and olfactory modalities (e.g., the Snoezelen room) were designed and tested (69).
Recent studies have shown that sensory integration engages multiple brain regions, such as the neocortex, basal ganglia, thalamus, and cerebellum. Within this framework, the cerebellum plays a central role in sensory processing, while the anterior motor cortex orchestrates motor programming. Disruptions—whether structural, metabolic, or functional—within these regions, or along their neural pathways, can profoundly compromise sensory processing, contributing to a spectrum of neurosensory dysfunctions (70, 71).
To date, clinical trials have focused on patients with intellectual and developmental disabilities or cognitive disorders such as dementia (70–74). As highlighted by Breslin et al., the therapeutic use of multisensory environments also aims at relaxation, pain management, improved attention, and the reduction of maladaptive behaviors (73).
Furthermore, from a musical perspective, the interaction between sound, environment, and tools has been a subject of scientific interest. Two prominent figures in this field are R. Murray Schafer and Aleksandr Skrjabin. Schafer is known for his studies on the “soundscape,” focusing on the relationship between sound and the natural and urban environment (75). Skrjabin, on the other hand, developed synesthetic theories linking music to colors and tactile sensations, opening new perspectives on the multisensory interaction of music (76). Both authors provide strong theoretical foundations for understanding how sound can be meaningfully integrated into the therapeutic environment and the patient’s experience.
Based on this research, EM therapy has developed therapeutic sound and compositional activities aimed at interacting synergistically with the SR environment. The environment itself is characterized by structural and sensory flexibility, allowing rapid adaptability to the specific needs of the patient.
A distinctive feature of the EM space is its adaptability and ease of configuration, making it suitable for various environments, including the patients’ home settings. The concept of “Mobile Architecture,” applied to the method, allows for the dynamic customization of the therapeutic environment. This flexibility not only optimizes the use of available space but also ensures that EM sessions can be seamlessly integrated into different therapeutic contexts, enhancing both the efficiency and quality of therapy.
This concept of “environmental resilience” has been discussed by Kaplan and Kaplan, who emphasized the importance of a therapeutic setting that can dynamically adapt to the individual needs and preferences of the patient (77).
Therapeutic interventions are designed in unimodal, multisensory, and cross-modal manners to maximize therapeutic efficacy. A unimodal approach may involve the use of a single sensory modality, such as vision or hearing, while a multisensory approach involves the simultaneous activation of multiple senses. Cross-modal stimulation, which engages the interaction between multiple senses, has been associated with enhanced brain plasticity and learning (78).
The therapeutic space of the SR is configured and personalized with specific materials and software to meet the individual needs of each patient, considering factors such as age, pathology, clinical condition, and specific therapeutic requirements (Supplementary 1). This personalization allows the patient to decontextualize the hospital environment, enabling the child to feel like the protagonist within the therapeutic setting. The design of the SR, grounded in robust scientific research, demonstrates that MT interventions in multisensory environments enhance the cognitive, emotional, social, and affective well-being of patients.
2 Materials and equipmentTo ensure the proper conduction of EM MT sessions, the music therapist manages a range of devices and technological tools aimed at regulating sensory stimuli. It is important to note that the software specified is provided for informational purposes, and therefore, other programs may be used depending on expertise and specific usage needs. These tools include:
• Audio Management: A computer, using a Digital Audio Workstation, handles audio editing software such as Adobe Audition, Pro Tools, FMOD Studio, MPC Beats, Ableton Live, or similar programs. Audio playback is achieved through two active 2.1 systems, each composed of two tops with four speakers in a vertical array configuration and a subwoofer, totaling 1,200 W of maximum power. The setup is complemented by a 12-channel mixer, a 4 In/4 Out audio interface, dynamic and condenser microphones, as well as a sound pressure level meter (cf. Supplementary 2.1, 2.2).
• Video Management and Projection: Session recording and study are conducted using fixed and mobile cameras. Fixed cameras record in 4 K with HDR technology and a fixed 120° XY stereo microphone, while mobile cameras also allow 4 K recordings and are equipped with a mid-side stereo microphone. Projection equipment includes Full HD LED projectors and WVGA LED mini-projectors (cf. Supplementary 2.3).
• Lighting Management: Equipment comprises a lighting management station with DMX interface and RGBWA LED moving heads. Light management is carried out through a computer with ADJ MyDMX3 software to control color tones and light intensity (cf. Supplementary 2.4).
• Musical Instruments and Equipment: Various types of musical instruments are available for therapists and patients (cf. Supplementary 2.5), while olfactory stimulation is managed through essential oils and essence vaporizers. Additionally, a hammock is permanently installed to promote muscle relaxation and strengthen the patient-parent bond.
3 MethodsThis study adopts a hermeneutic approach to deeply analyze the methodologies and procedural algorithms of the EM, integrating original research with a well-established scientific and historical context (79, 80). A rigorous qualitative review of the existing literature on MT practices was conducted, selecting sources of proven relevance and methodological robustness (81). The analysis incorporated data extracted from our previous studies and research as well as clinical reports (35, 36).
To contextualize the results, the historical development of MT was traced, positioning the EM within this broader framework. Key historical references have provided a solid theoretical basis for understanding the evolution and adaptation of therapeutic practices over time (82, 83). The investigation revealed that the EM fits into a historical tradition of therapeutic music use, with ancient roots spread across various cultures (84, 85).
The hermeneutic approach enabled a deep understanding of the experiences of patients and therapists with the EM through the interpretation of qualitative data (80). To ensure an inclusive and participatory method, the principles of Mertens’ transformative approach were integrated (86), actively involving patients, parents, and therapists in the research process. This approach fostered the empowerment of participants and promoted continuous dialog between researchers and the involved subjects, ensuring that their experiences and perspectives were fully integrated into the analysis.
The integration of historical elements and the triangulation of data sources ensured methodological rigor and high validity (87, 88). This combined approach not only facilitated a deeper understanding of the role of the EM in contemporary MT but also highlighted its potential to significantly improve patient well-being and promote the future development of the discipline.
3.1 Study designThis section analyzes the data from two previously published studies, aiming to provide a more detailed and comparative view of the effectiveness of EM in the context of intensive pediatric rehabilitation.
The first study, conducted by Bompard et al., was a prospective single-center study designed to evaluate the feasibility of EM-based telerehabilitation during the SARS-CoV-2 pandemic.
The inclusion criteria consisted of children with developmental delays under the age of 12 who had previously undergone personalized MT sessions prior to the pandemic. Exclusion criteria included the absence of participation in the EM MT pathway during the previous hospitalization.
Participants, regularly enrolled in intensive rehabilitation programs, were assessed using the Gross Motor Function Classification System (GMFCS) to determine their functional status (89). Evaluations were conducted remotely by the pediatric neurologist in collaboration with the parents, both before the start of the program and upon its conclusion. Informed consent was obtained from the parents for data collection and analysis (35). The second study, conducted by Liuzzi et al., was a prospective single-center experimental investigation aimed at evaluating the effects of the intervention on key aspects of the children’s and their parents’ lives.
Inclusion criteria comprised children aged 0 to 10 years with cerebral palsy (90), hospitalized for 3 to 4 weeks for intensive rehabilitation. Children with severe hearing impairments or deafness were excluded. Participants were randomly assigned to an experimental group, which received MT based on the EM, and a control group, which followed the rehabilitation program without MT. Motor functionality was assessed using the GMFCS (89), and outcomes were measured through the administration of parent-report questionnaires at T0 (study initiation) and T1 (after 3 weeks). Informed consent was obtained from the parents, and an independent evaluator, blinded to the randomization, examined the results (36).
3.2 Euterpe method proceduresEM’s distinctive prerogative lies in the use of four original algorithms, each designed to address specific therapeutic aspects with scientific precision.
EM Hospital-based guides the process from patient selection to the definition of target objectives by the hospital team (Supplementary Figure 34; Figure 1).
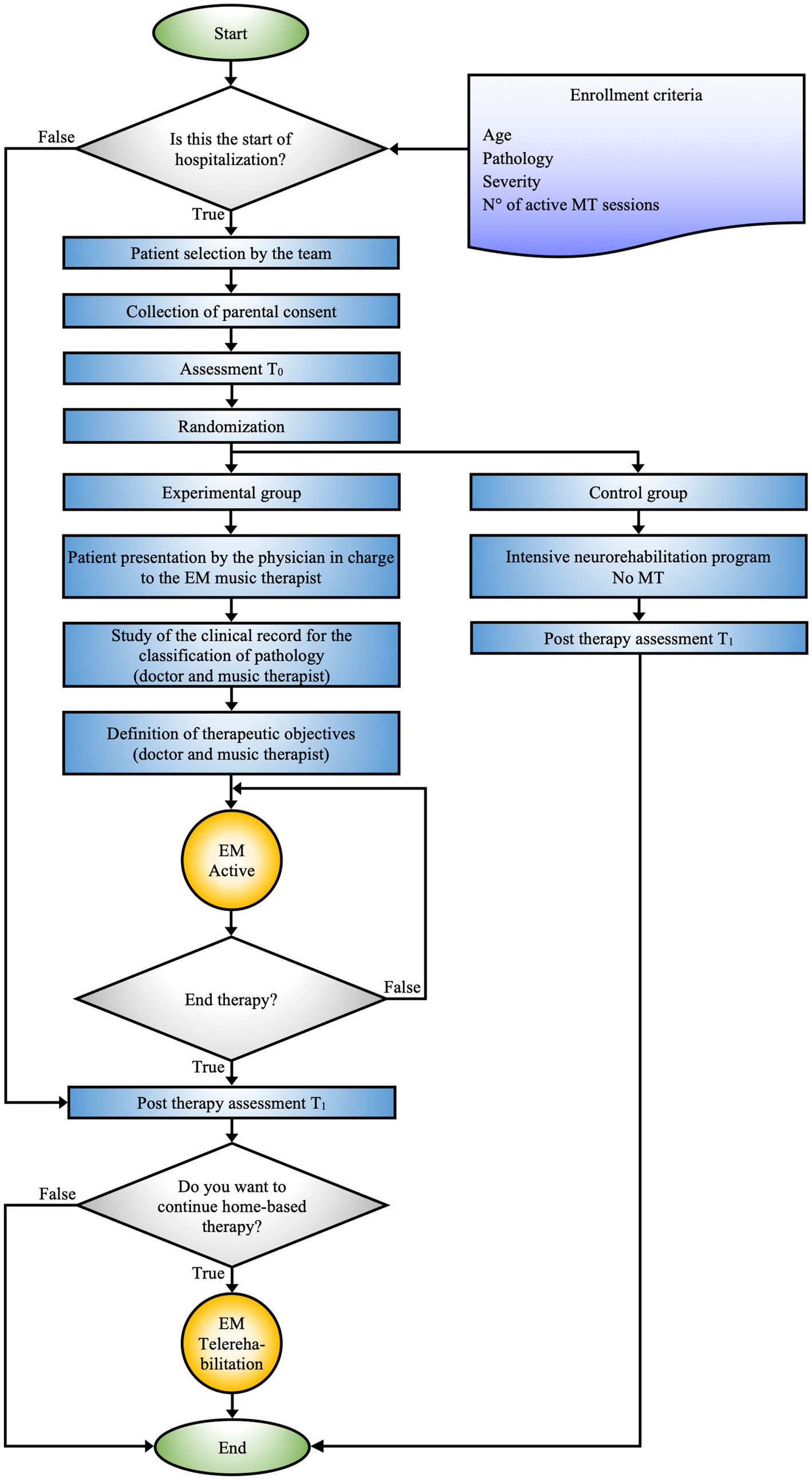
Figure 1. EM hospital-based schematic representation of the decision-making and therapeutic process adopted for patient management during hospitalization. The figure shows the integration between personalized MT and intensive rehabilitation programs, with a focus on tailoring the treatment to the specific clinical needs of the patients.
EM Active constitutes the core procedure of the EM, precisely delineating the modus operandi of MT activities (Figure 2).
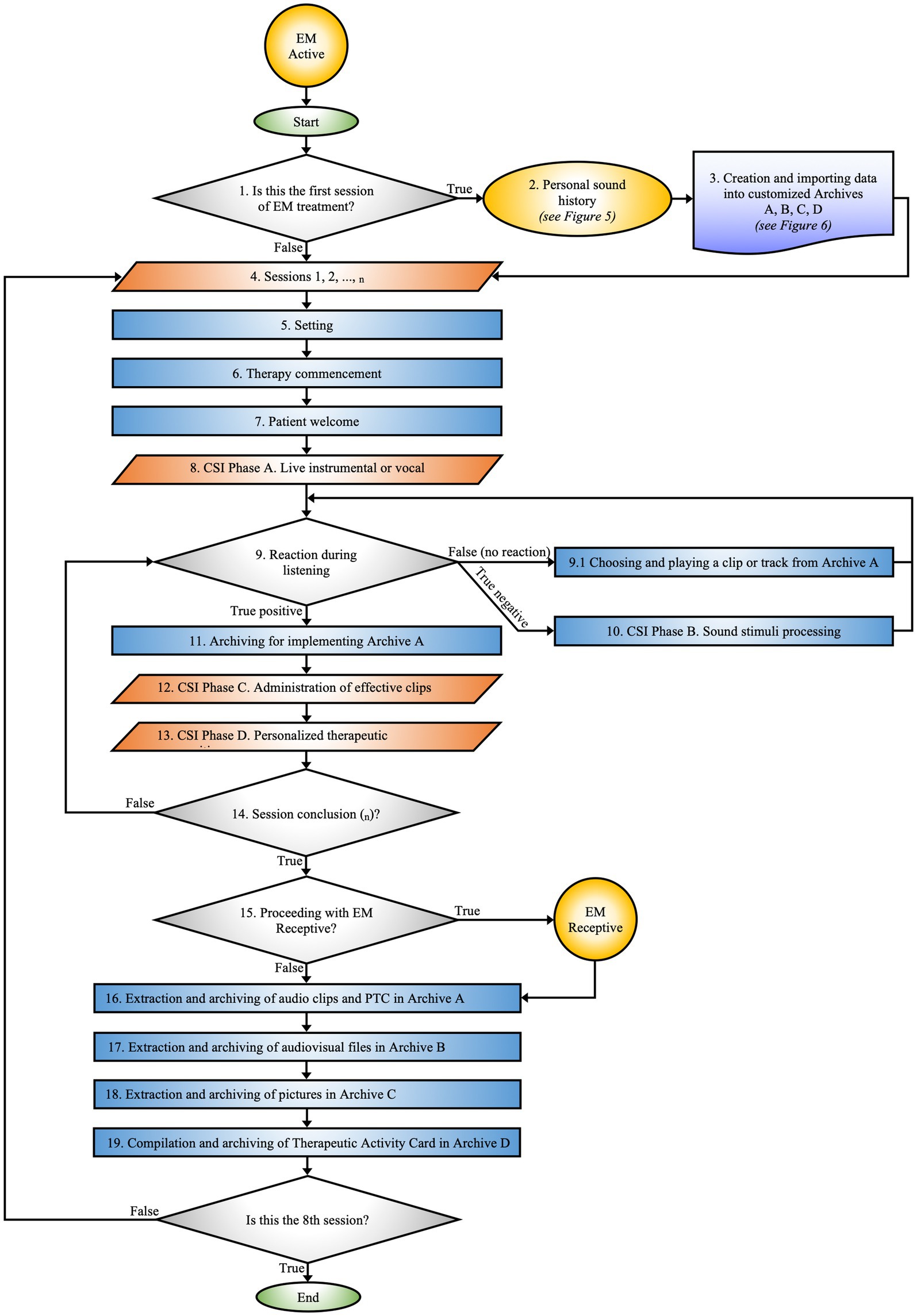
Figure 2. EM active. Maps the phases of the therapeutic process from the initial session to data archiving. The flow is guided by the patient’s responses to auditory stimuli.
EM Receptive specifies the protocol for implementing rehabilitative activities on days when active MT sessions are not conducted in the hospital (Figure 3).
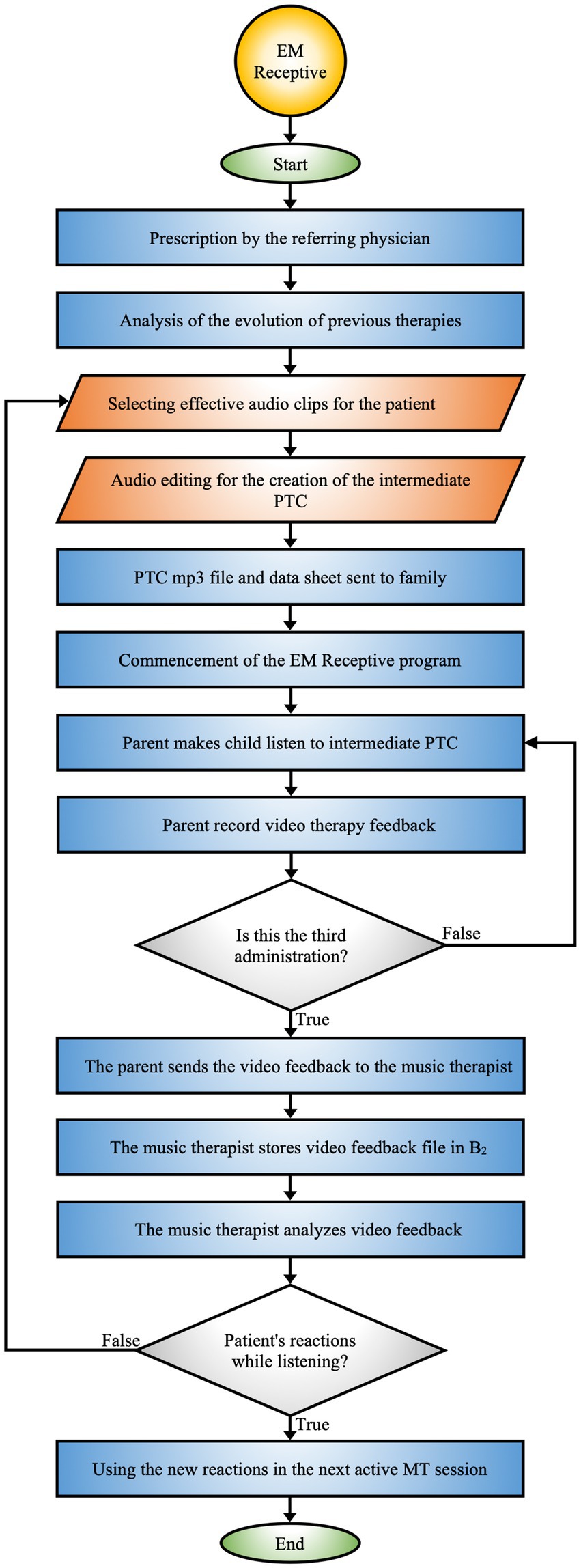
Figure 3. EM receptive. Protocol that integrates the collaboration between the hospital team, music therapist, and family to monitor and adapt the therapy based on the patient’s reactions.
EM Telerehabilitation provides therapeutic continuity of MT directly in the patient’s home environment, offering the possibility of treatment delivery even in remote or difficult-to-access geographic settings. It can be prescribed by the hospital team or requested by parents, offering a structured pathway for remote therapy (Figure 4).
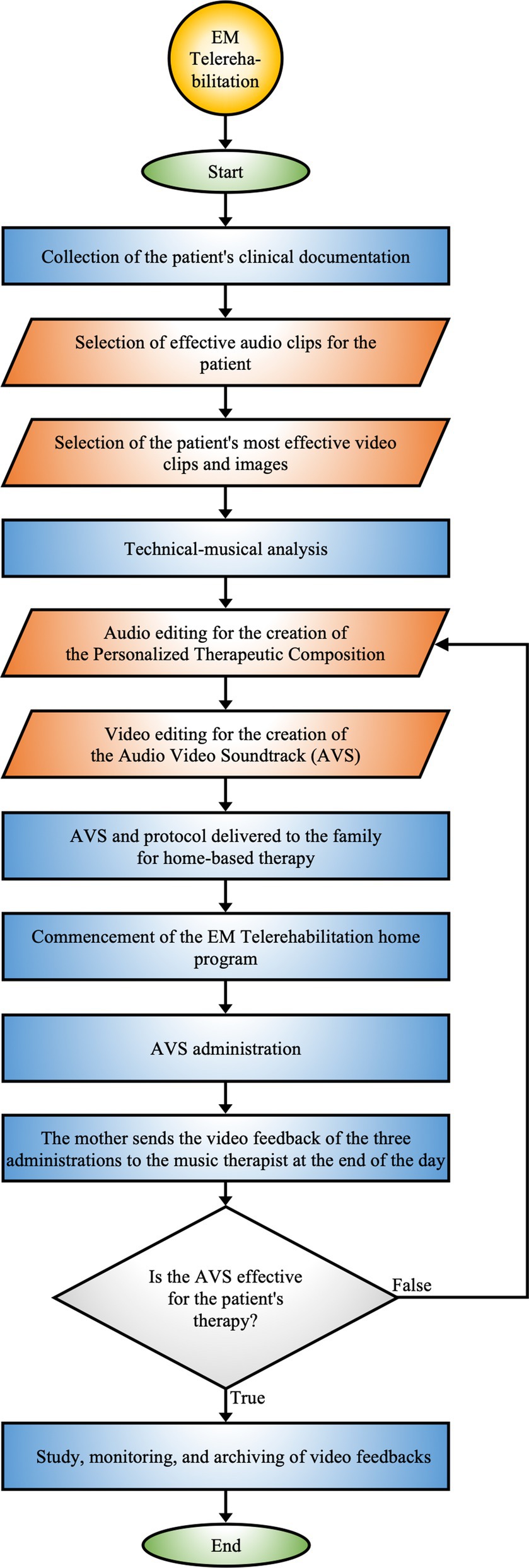
Figure 4. EM telerehabilitation. Process of home-based therapy utilizing personalized audio-video compositions, incorporating continuous monitoring and feedback to adapt the therapy according to patient responses.
3.3 EM Hospital-based procedureThe EM Hospital-based protocol (see Figure 1) represents a rigorously defined methodological approach aimed at formulating specific clinical objectives for each patient. This protocol is designed to enable its application in various clinical contexts while ensuring interconnection with subsequent algorithms.
The selection of patients for the EM therapy program is carried out by a multidisciplinary team, including physicians, psychologists, head nurses, nurses, and certified music therapists, ensuring an integrated therapeutic approach. The prescription of the EM program is based on inclusion criteria, considering variables such as age, pathology, severity of the condition, and the optimal number of necessary sessions, allowing for precise treatment personalization.
After the patient selection process and before the start of the EM program, parents provide privacy consent for the inclusion of their children in the scientific studies and for video recording of the sessions. Furthermore, questionnaires are provided to the parents, who complete them independently. This allows for a preliminary assessment of both the patient and the parent (T0).
The entire sample is divided into two groups, experimental and control, through blind randomization. Subsequently, the physician and music therapist work closely to review the clinical history of the patients assigned to the experimental group to precisely define the therapeutic goals of the EM MT program. At the same time, the control group follows an intensive neurorehabilitation program without the EM MT intervention. Upon completion of the therapeutic path, which includes both intensive rehabilitation and MT sessions, T1 assessments are conducted for both groups to evaluate the effectiveness of the interventions and compare outcomes between the two groups.
Before discharge, if deemed necessary, the hospital team proposes that families from the experimental group continue the EM at home through the telerehabilitation program.
3.4 EM active procedureThe EM Active constitutes the detailed protocol for practical MT activities, designed according to the specific clinical needs and individualized treatment goals of each patient (Figure 2).
This process is carried out within the SR by a certified music therapist and a certified co-therapist. Activities may include learning exercises with musical instruments, improvisations, explorations of EmoTonePhonoSymbolisms (91), and sound elaborations, adapted to the patient’s needs and therapeutic progress. EM approach involves the administration of sensory stimuli using unimodal, multisensory, and cross-modal techniques, aimed at creating PTC.
3.4.1 Is this the first EM session?During the initial session, the music therapist informs the parent about the EM therapeutic path and outlines the objectives to be achieved during the rehabilitation intervention. The session comprises an observational assessment of the mother’s psychological state to encourage her active involvement in the therapeutic process and facilitate collaboration for subsequent stages.
3.4.2 Personal sound historyAfter reviewing the patient’s clinical history, the music therapist collects the “Personal Sound History” through the following procedure:
1. Questionnaire: A structured interview is employed to gather data on the patient’s sensory sensitivities, focusing on areas of vulnerability such as photosensitivity, auditory hyperreactivity, olfactory intolerances, tactile difficulties, and feeding issues. This information is essential for constructing a comprehensive sensory profile, which is indispensable for tailoring the therapeutic intervention (Figure 5).
2. Mother’s voice recording: The therapist records various linguistic elements of the mother, such as the prosody of the child’s name, baby talk, tenderness, positive reinforcement, and lullabies. The recording is done in a supportive environment to ensure that the mother feels comfortable and motivated.
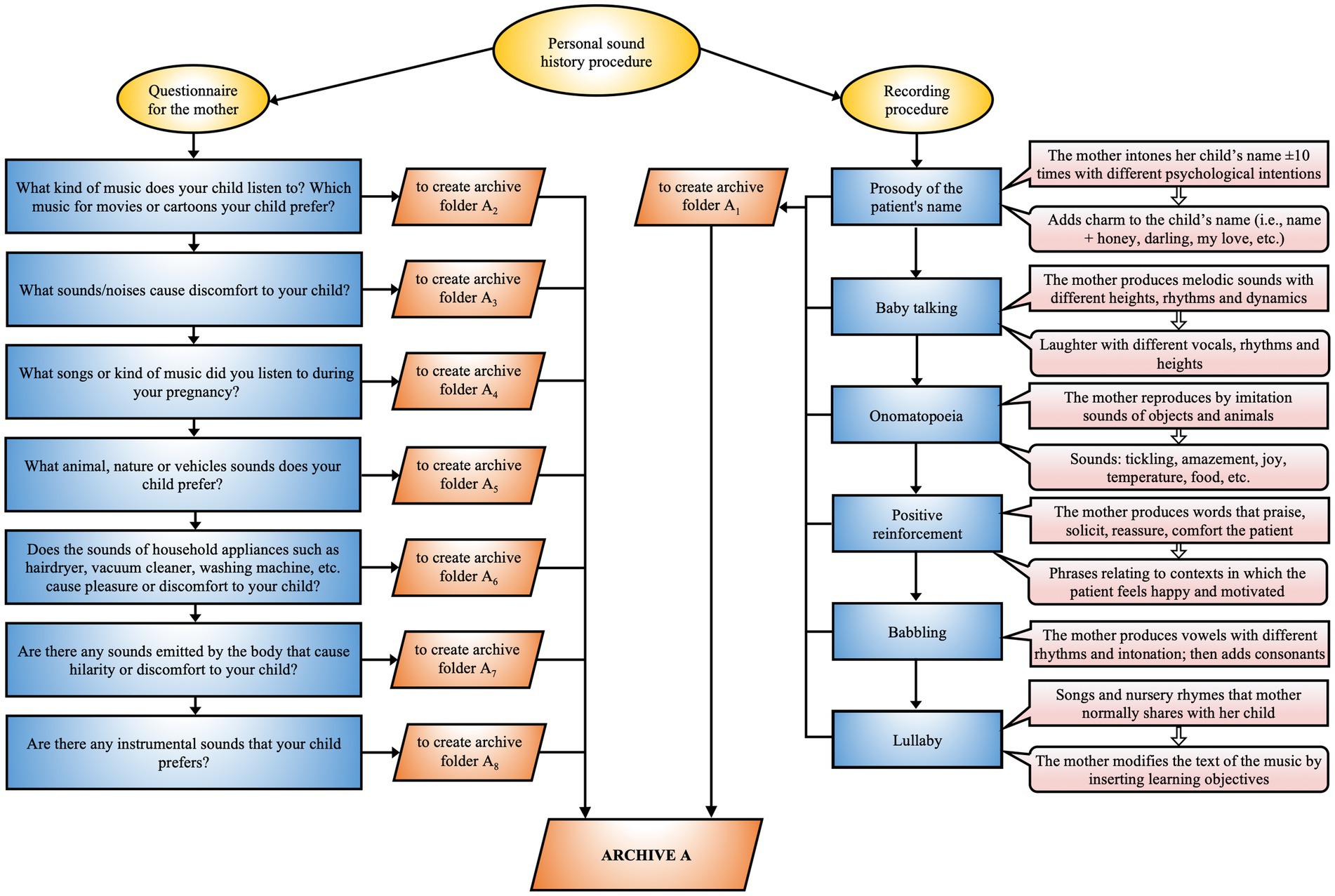
Figure 5. EM personal sound history. Procedure for acquiring the personalized sound history that integrates a questionnaire for the mother and a recording methodology aimed at identifying relevant auditory stimuli for optimizing the therapeutic process.
3.4.3 Creation and importing data into customized archives A, B, C, DThe music therapist analyzes the raw recording previously made with the patient’s mother, removing background noise and segmenting the audio files, which are then named according to their content. The selected files are used as auditory stimuli for therapy and as a notation of the compositional structure. The database, named after the patient, includes preferences derived from the questionnaire and is structured into four distinct archives (Figure 6; Supplementary 3.1):
1. Sound Archive A
• A0 Therapist’s Sound/Music
• A1 Family Sound
• A2 Music Known by the Patient
• A3 Discomfort Sound
• A4 Amniotic Sound
• A5 Sound Design
• A6 Electronic Noise
• A7 Body Sound
• A8 Live Music and Instruments Sound
• A9 Patient Reaction
2. Video Archive B
• B0 Video Archive per Session
• B1 Effective Video-Reactions
• B2 Receptive Procedure Video-Reactions
3. Pictures Archive C
• C0 Pictures Archive per Session
• C1 Effective Pictures
4. Therapeutic Activities Archive D
• Tables detailing the activities performed in each session (Supplementary Figure 14).
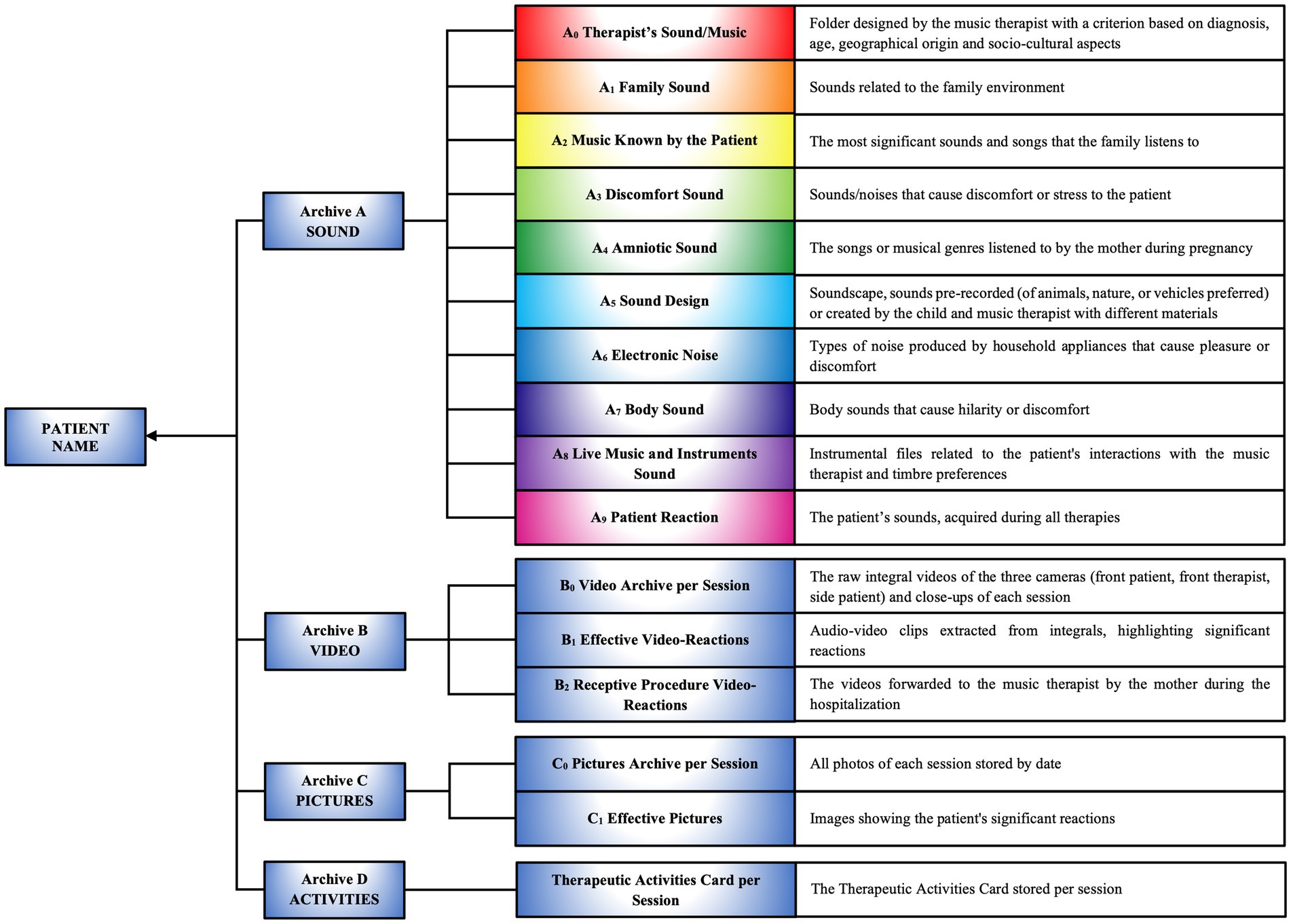
Figure 6. Creation and importing data into customized archives A, B, C, D. Structure of personalized archives containing data on the patient’s sounds, videos, images, and therapeutic activities, organized into categories to support the personalized therapeutic compositional process.
3.4.4 Sessions 1, 2,.., nAll sessions are video recorded, an essential step to ensure an accurate evaluation of the patient’s responses and provide an in-depth retrospective analysis of the therapeutic process. This practice also facilitates rigorous documentation and optimizes the design of personalized musical compositions.
The program involves a minimum of eight sessions, conducted three times per week during the patient’s hospital stay. The duration of each session, typically ranging from 30 to 40 min, is adjusted based on the patient’s age and specific needs. Each session follows a therapeutic structure composed of sequential phases and steps, specifically tailored for each encounter.
3.4.5 SettingThe sessions take place within the SR, a space designed to provide a highly flexible and resilient environment, capable of adapting to various age groups and specific psychophysiological conditions of the patients. This adaptability ensures maximum safety for both the patient and the parent during the therapeutic sessions.
The MT team is responsible for preparing the SR through a series of interventions:
• Cleaning and sanitizing of the surroundings, materials, and musical instruments
• Setting up the workstation
• Organizing sound material for playback, and balancing output signals from software and mixer
• Placement of aids for video recording, control of gain levels, and framing
• Connection and checking of LED lights and mobile LED heads, wired to the DMX interface
• Preparation of software for the touchscreen monitor (digital flipchart)
• Preparation of the projector for augmented reality
• Changing of hammock sheets
• Thorough handwashing and donning of brightly colored clothing by the therapist and co-therapist.
3.4.6 Therapy commencementDuring this phase, the music therapist and co-therapist define and coordinate their roles and responsibilities with respect to the patient and the therapy within the therapeutic environment.
3.4.7 Patient welcome 3.4.7.1 Step 1. Patient observation and feedback with the parentThe therapist assesses the psychophysiological condition of the patient and the parent before starting the therapy, using professional behaviors.
3.4.7.2 Step 2. Patient introduction to the multisensory spaceThe therapist welcomes the patient and the parent, guiding them through the multisensory environment (SR), which is rich in colors, scents, sounds, and images, and encourages them to explore the space. Constant monitoring and guidance by the therapist are essential to ensure the child’s safety and facilitate a smooth transition into the environment.
3.4.7.3 Step 3. Review of the previous sessionBefore beginning the MT session, the therapist reviews the activities of the previous session with the parent, checking for any changes in the child’s behavior and monitoring therapeutic progress. This feedback process ensures that the therapeutic plan remains appropriate to the patient’s psychophysiological needs and promotes parental involvement in achieving clinical objectives.
3.4.8 Compositional sound interventions—phase A. Live instrumental or vocalCSI are structured therapeutic approaches that employ personalized musical and auditory techniques to achieve specific clinical objectives. The CSI process is divided into four phases:
A. Live Instrumental or Vocal
B. Sound Stimuli Processing
C. Administration of Effective Clips
D. Personalized Therapeutic Composition (PTC).
Phase A. Live Instrumental or Vocal has as its main objective the accurate monitoring of the patient’s responses to assess his emotional and psychophysiological state. The therapist observes and documents every verbal and non-verbal response of the patient to establish a clinical baseline, which is essential for early detection of signs of discomfort or specific needs that may require targeted interventions. Therapy begins with silence, conceived as an active element (54), intended to facilitate and promote the patient’s adaptation within the therapeutic space.
This silence fosters concentrated attention and a gradual anticipation of auditory intervention, allowing the music therapist to establish initial non-invasive contact in a secure and trusting environment. Subsequently, the therapist uses the sound of their own breath, alternated with silence, to synchronize with the patient’s breathing cycle, generating interest and attention. The music therapist introduces hand-clapping sounds, synchronized with the patient’s breathing, and uses a sound level meter to identify the auditory threshold. At this stage, soft and warm vocal sounds, imitating the mother’s voice, are emitted at an intensity of 30–35 dB. These sounds are used to initiate active interaction and modulate emotions in synchrony with the patient’s heart rate and breathing variations (92–94).
Next, the real-time use of a musical instrument gradually introduces auditory stimuli with varying intensities, including consonant and dissonant intervals, glissandi, harmonics, and fragments of familiar songs or cartoon themes (95–98). The administration of such auditory stimuli often reveals significantly stronger responses in many patients when the clarinet is used. These patients exhibit a keen interest in following the sound trajectory in sync with the movement of the instrument, suggesting a deeper sensory and cognitive engagement in musical perception.
Additionally, it is noteworthy that the alternation between a familiar melody and intervals of silence induces predictive anticipation of the melody’s return in patients, suggesting an active expectation that predisposes them to emotional responses.
When the therapist introduces unfamiliar sounds, such as harmonics perceived as whistles, motor excitement and emotional surprise are observed, highlighting an innate curiosity toward new auditory stimuli. With controlled and repeated exposure to these sounds, patients develop progressive adaptation, demonstrating increased tolerance and predictive capacity, accompanied by moments of laughter. This process suggests sensory and cognitive adaptation, where acquired familiarity with unfamiliar sounds not only reduces initial surprise but also enriches the patients’ emotional and social experience.
Supporting this, many studies highlight that the temporal dynamics of auditory signals contain significant information (99–103). The brain is thought to actively anticipate forthcoming auditory stimuli in consideration of prior contextual information; this process is known as predictive coding. This mechanism, essential for learning and language comprehension, as well as for musical processing of pitch and rhythm, has been extensively documented by various authors in audiology (104–111).
3.4.9 Reactions during listeningIn this step, the music therapist manages and controls the Digital Audio Workstation to synchronize and adapt sounds in real-time to the activities carried out by the co-therapist with the patient. This setup facilitates real-time musical composition and effective synchronization of therapeutic activities. The primary goal is to observe, evaluate, and understand the patient’s reactions to novel auditory stimuli.
3.4.9.1 Choosing and playing a clip or track from archive aIf the patient does not exhibit any response during exposure to the audio clips, several possibilities should be considered:
• The musical stimulus may be inadequate for the patient’s specific needs
• The patient’s emotional or physical state may be influencing their responsiveness
• The patient may be disengaged or distracted
• A lack of response could suggest the need for further diagnostic evaluations for a more in-depth analysis.
3.4.10 CSI phase B. Sound stimuli processingDuring exposure to new auditory stimuli, it is essential to adopt a sensitive therapeutic approach, particularly if the stimuli elicit negative reactions. In such cases, it is necessary to immediately cease sound administration and monitor the patient’s responses, which may manifest through facial expressions, body movements, vocal tone variations, or other signs of discomfort. If the negative stimulus stems from sounds or words essential to the patient, such as the mother’s voice or natural sounds (soundscape), it is fundamental to process and adapt the sounds using appropriate techniques until acceptance is achieved. This issue is especially pertinent for long-term hospitalized patients who may experience alterations in sensory or relational learning (112).
Sound processing and modification techniques include amplitude adjustment, compression, delay, echo, and pitch correction. Key parameters for developing new real-time auditory stimuli that address the emotional and psychological needs of the patient include intensity, spatiality, directionality, speed, and frequency (Supplementary 3.4).
The therapist employs two playback methods to assess the efficacy of the sound stimuli: one involves the sequential presentation of processed musical clips, while the other overlays effective clips with unknown sounds.
The goal is to facilitate the acceptance of unfamiliar sounds, such as traffic and thunder, to improve quality of life and develop skills in managing environmental sound stimuli.
3.4.11 Archiving for implementing archive AThe music therapist extracts the patient’s positive reactions from the raw audio recordings of the ongoing therapy. The acquired clips are timestamped, named according to content, and archived in the A9 Patient Reactions folder. The process ensures that the therapist has immediate access to new sound material for use in the subsequent step of therapy.
3.4.12 CSI phase C. Administration of effective clipsIn this phase, a sequence of auditory stimuli organized in rhythmic patterns, based on the patient’s vocal reactions, is presented. The rhythmic patterns, designed as cyclic structures, regulate the temporal flow of music through the use of elements such as tempo, accents, rhythmic subdivisions, and meter (Figure 7I).
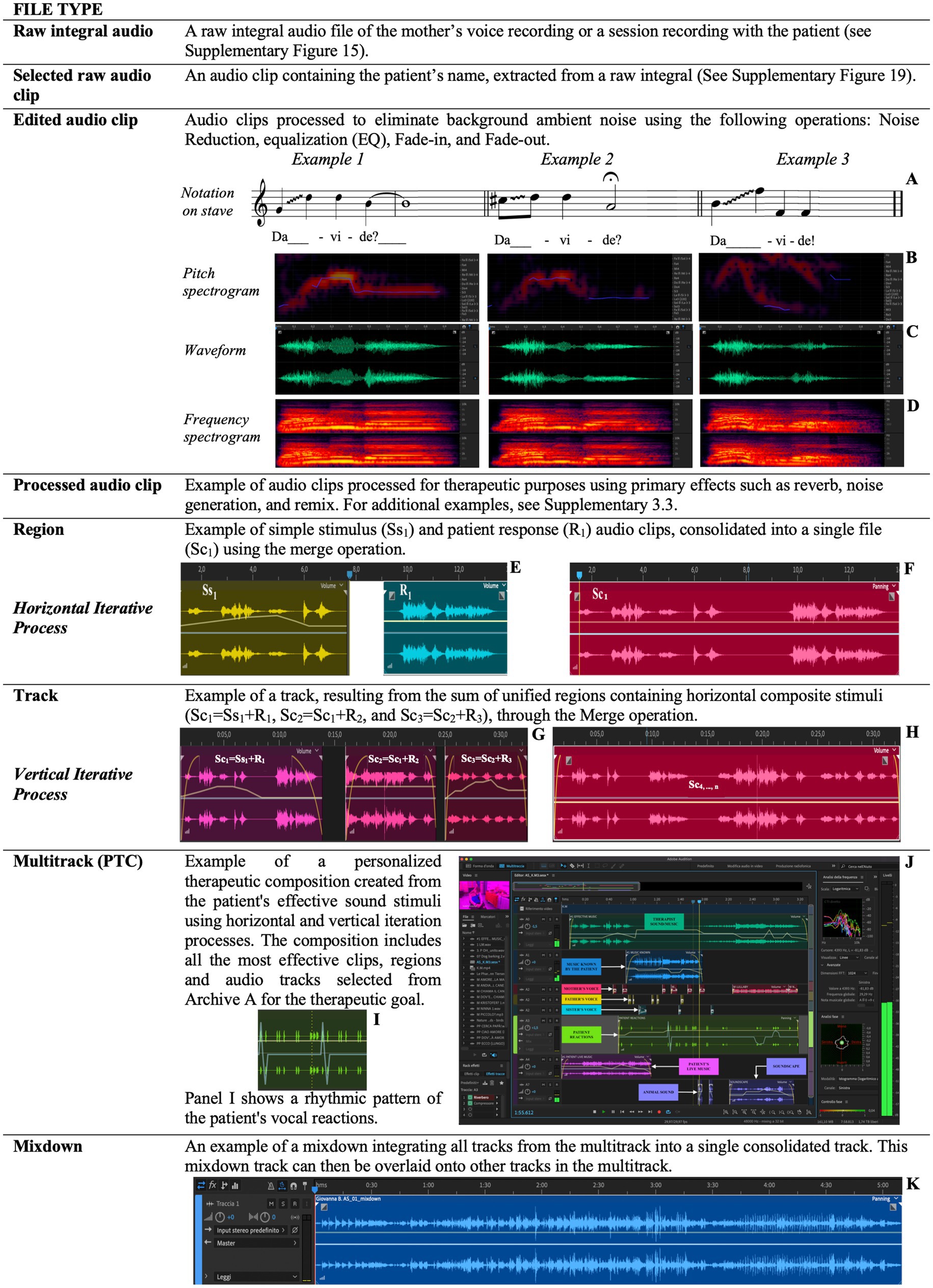
Figure 7. This figure explicates the technical and compositional steps involved in creating and managing sound stimuli, integrating patient responses, and progressively developing a therapeutic pathway through iterative processing and personalized composition. Examples of vocal clip notations on the musical stave (A) alongside their pitch spectrograms (B), waveforms (C), frequency spectrograms (D). Consolidation of two sound clips, i.e., Ss1 and R1 (E), into a single new file (F). Consolidation of the Sc1, Sc2 and Sc3 clips (G) in the track (H). A rhythmic patte
留言 (0)