According to the findings of the Global Burden of Disease Study 2017, strokes rank as the second most prominent contributor to both mortality and disability worldwide (1). Among stroke cases, acute ischemic stroke stands out as the predominant form. AIS refers to a condition wherein the cerebral blood vessel experiences a sudden blockage, resulting in inadequate or disrupted blood supply to brain tissues. The impact of stroke is substantial, affecting patients, their families, and society at large. It is characterized by significant morbidity, a high prevalence of disability, elevated mortality rates, an increased risk of recurrence, and a considerable economic burden (2). The American Heart Association reports that the incidence of stroke will continue to increase by nearly 20% within 15 years, with a 30-day all-cause mortality rate as high as 10.5% (3). In China, studies have shown that approximately one-third of AIS patients develop death or disability within 3 months or 1 year (4).
Atrial fibrillation represents the prevailing type of arrhythmia (5) and stands as a significant contributor to various conditions, including stroke, heart failure, dementia, ischemic heart disease, and sudden death (6). Among these, stroke emerges as the most frequent and severe complication associated with AF. Individuals diagnosed with atrial fibrillation face a 4- to 5-fold greater risk of stroke compared to those without this condition (7). Furthermore, strokes resulting from atrial fibrillation exhibit higher rates of disability and mortality compared to non-atrial fibrillation-related strokes, and its in-hospital mortality rate is significantly higher than that of non-atrial fibrillation-related stroke patients (10.8% vs. 7.5%; unmatched population, 11.9% vs. 4.6%) (8).
Blood urea nitrogen and creatinine are biomarkers commonly utilized in clinical practice to assess renal function as they serve as end products of nitrogenous metabolism within the human body (9). Previous research findings have suggested that BUN/Cr can serve as an independent prognostic indicator for a negative patient outcome in cases of acute and chronic kidney injury (10), ischemic stroke (11), acute heart failure, and chronic heart failure (12, 13). As of late, evidence has emerged indicating that changes in the BUN/Cr ratio could independently predict outcomes in patients diagnosed with AIS during hospitalization (14). Nonetheless, there is a dearth of comprehensive investigations exploring the correlation between BUN/Cr and in-hospital mortality among individuals afflicted with both AIS and AF.
Therefore, in such a context, the primary objective of the current study was to evaluate the correlation between the BUN/Cr ratio and the rate of mortality during hospitalization within ICU for patients presenting with a combination of AIS and AF.
2 Materials and methods 2.1 Data sourceThis study is characterized as a retrospective cohort study utilizing data sourced from the Medical Information Mart for Intensive Care (MIMIC-IV 2.2) (15). The MIMIC-IV dataset, being a repository of clinical data derived from a single medical center, specifically the Beth Israel Deaconess Medical Center (BIDMC), encompasses extensive information regarding patients admitted to the ICU within the period spanning from 2008 to 2019. It is important to note that adherence to patient privacy regulations was strictly observed during the identification and utilization of this database, in accordance with the security measures outlined in the Health Insurance Portability and Accountability Act (HIPAA). One of the authors, Bowen Li (ID: 11800689), gained access to perform data extraction from the database upon successful completion of the Collaborative Institutional Training Initiative (CITI) examination. To prioritize patient privacy, all data were effectively anonymized, eliminating the necessity for informed consent. This study rigorously followed the guidelines set forth in the Statement for Strengthening the Reporting of Observational Studies in Epidemiology (STROBE), demonstrating a commitment to ensure thorough and transparent reporting of the study’s findings (16).
2.2 Study populationThe code used for the data extraction process can be accessed on GitHub (17). For our study, eligibility was determined by selecting patients who experienced their initial ICU admission and were diagnosed with both AIS and AF. The criteria for diagnosing AIS and AF were based on the International Classification of Diseases, Ninth and Tenth Revisions (ICD-9 and ICD-10). Specifically, the diagnosis of acute ischemic stroke was defined by the ICD-9 codes 34,660, 34,661, 34,662, 34,663, 43,301, 43,311, 43,321, 43,331, 43,381, 43,391, 43,401, 43,411, and 43,491, as well as the ICD-10 code I63. Atrial fibrillation is defined by ICD-9 code: 42731 and ICD-10 code: I48.
The inclusion criteria were as follows: (1) age ≥ 18 years old; (2) patients who were admitted to the ICU and had a duration of hospitalization exceeding 24 h; and (3) first ICU admission. The exclusion criteria for this study were as follows: (1) patients who had missing data for blood urea nitrogen and creatinine. Following the application of these criteria, the study included a total of 856 patients, as illustrated in Figure 1.

Figure 1. Flow chart of this study.
2.3 Data acquisitionThis study utilized the PostgreSQL database management system in conjunction with Structured Query Language (SQL) for data extraction: general characteristics, vital signs, laboratory data, comorbidities, scoring system, treatment, and length of stay (LOS hospital and LOS ICU). The study outcome of interest was in-hospital mortality. Participants were tracked from the day of ICU admission to either the day of in-hospital death or discharge, whichever occurred first.
2.4 Statistical analysisIn this study, 856 participants were evenly divided into three groups based on baseline calculated BUN/Cr, to make the numbers roughly equal. Continuous data, such as age and laboratory parameters, were presented as either the mean ± standard deviation or median (interquartile range) depending on their distribution. Categorical data, such as gender and comorbidities, were presented as a single number (percentage). To evaluate the disparities in baseline characteristics between different groups, appropriate statistical tests were utilized. The analysis employed the ANOVA or rank-sum test for continuous variables, depending on their distribution, and the chi-squared test or Fisher’s exact test for categorical variables. These statistical tests were chosen based on the nature of the data under examination and aimed to determine whether there were statistically significant variations in baseline characteristics among the groups.
The majority of the variables under investigation display a skewed distribution, and the missing values of all variables are less than 10%. The use of the median value to fill in missing data is an effective method for handling variables that are skewed. Accordingly, median replacement was employed to address this concern. To evaluate the association between BUN/Cr ratio and in-hospital mortality, we utilized both univariate and multivariate logistic regression approaches. We investigated the impact of BUN/Cr by considering it as both a categorical variable with three levels and a continuous variable. Our regression analysis encompassed four distinct models, providing a comprehensive assessment of the relationship under scrutiny. The multifactorial models were adjusted as follows: Model 1 was not adjusted; model 2 was adjusted for age and gender; model 3 was adjusted for model 2 plus LOS hospital, DBP, MBP, temperature, Spo2, WBC, platelets, anion gap, and international normalized ratio (INR); model 4 was adjusted for model 3 plus chronic pulmonary disease, malignant cancer, severe liver disease, Oxford acute severity of illness score (OASIS), Charlson Comorbidity Index, peripheral vascular disease, cerebral edema, tracheal intubation, thrombolysis, statins, anti-platelet agents, and anticoagulant drugs.
We also used a restricted cubic spline (RCS); this approach allowed us to flexibly explore potential non-linear relationships between BUN/Cr levels and in-hospital mortality. The reference value for interpreting the results of the RCS analysis was determined as the median of the predictor variables. Upon identification of a non-linear connection, we utilized a two-segment logistic regression model to evaluate the threshold impact of BUN/Cr on in-hospital mortality.
Furthermore, we used subgroup analyses to evaluate different groups of patients. These subgroups included age, gender, peripheral vascular disease, chronic pulmonary disease, malignant cancer, severe liver disease, cerebral edema, tracheal intubation, thrombolysis, statins, anti-platelet agents, and anticoagulant drugs.
In our research, a two-tailed test was performed, and a statistical significance was defined as a p-value less than 0.05. All the analyses were performed with the statistical software packages R (http://www.R-project.org, The R Foundation) and Free Statistics software version 1.8 (18).
3 Results 3.1 Baseline characteristicsThe study included 2074 patients in the ICU who suffered from AIS combined with AF. After applying the predetermined inclusion and exclusion criteria, 1,218 individuals were deemed ineligible and thus excluded from participating in this study. Among the excluded individuals, 1,082 individuals had previously been admitted to the ICU before their current admission, 111 individuals were under the age of 18 and had an ICU stay duration of less than 24 h, and 25 individuals did not have available data regarding their blood urea nitrogen or creatinine levels. In total, a cohort of 856 patients were included for the final data analysis. The detailed process is illustrated in Figure 1, providing a visual representation of the steps involved.
There were a total of 856 patients (age ≥ 18 years) with a median age of 78.0 years, of which 466 (54.4%) were female. Out of 856 patients, 182 (21.26%) died in the hospital. The BUN/Cr ratio was categorized into tertials based on the distribution of BUN/Cr among the patients, with 285, 285, and 286 cases in Q1 (<17.2), Q2 (17.2–22.41), and Q3 (>22.41). All the variables are listed in Table 1. Based on the analysis, we found significant differences in age, gender, heart rate, SBP, anion gap, bicarbonate, BUN, creatinine, glucose, sodium, congestive heart failure, renal disease, malignant cancer, acute physiology score III (APS III), simplified acute physiology score II (SAPS II), OASIS, and Charlson Comorbidity Index (p < 0.05). Patients with high levels of BUN/Cr ratio share common characteristics such as higher age, heart rate, BUN, glucose levels, APS III, SAPS II, and OASIS scores, as well as a history of malignant cancer and congestive heart failure. On the other hand, a history of renal disease shows an inverse relationship to the elevated BUN/Cr ratio levels (p < 0.05).
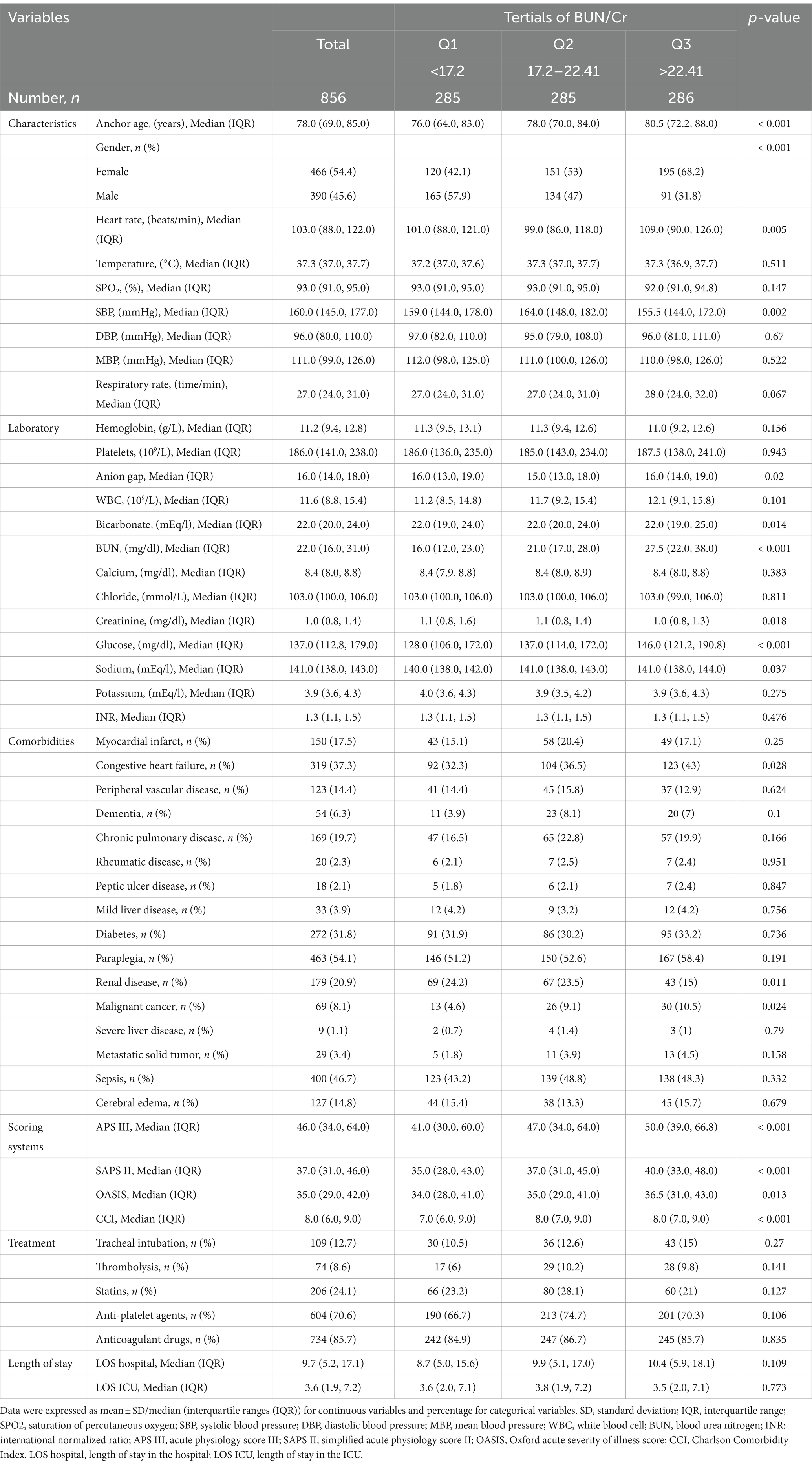
Table 1. Baseline characteristics related to in-hospital mortality.
3.2 Univariate analysisAs depicted in Table 2, the univariate logistic regression analysis disclosed a positive correlation between in-hospital mortality and variables such as age, heart rate, temperature, respiratory rate, glucose level, sodium level, anion gap, WBC, renal disease, malignant cancer, metastatic solid tumor, APS III score, SAPS II score, OASIS score and Charlson Comorbidity Index, cerebral edema, and tracheal intubation. Conversely, variables including DBP, hemoglobin level, bicarbonate level, calcium level, LOS hospital, statins, and anticoagulant drugs exhibited an inverse association with in-hospital mortality.
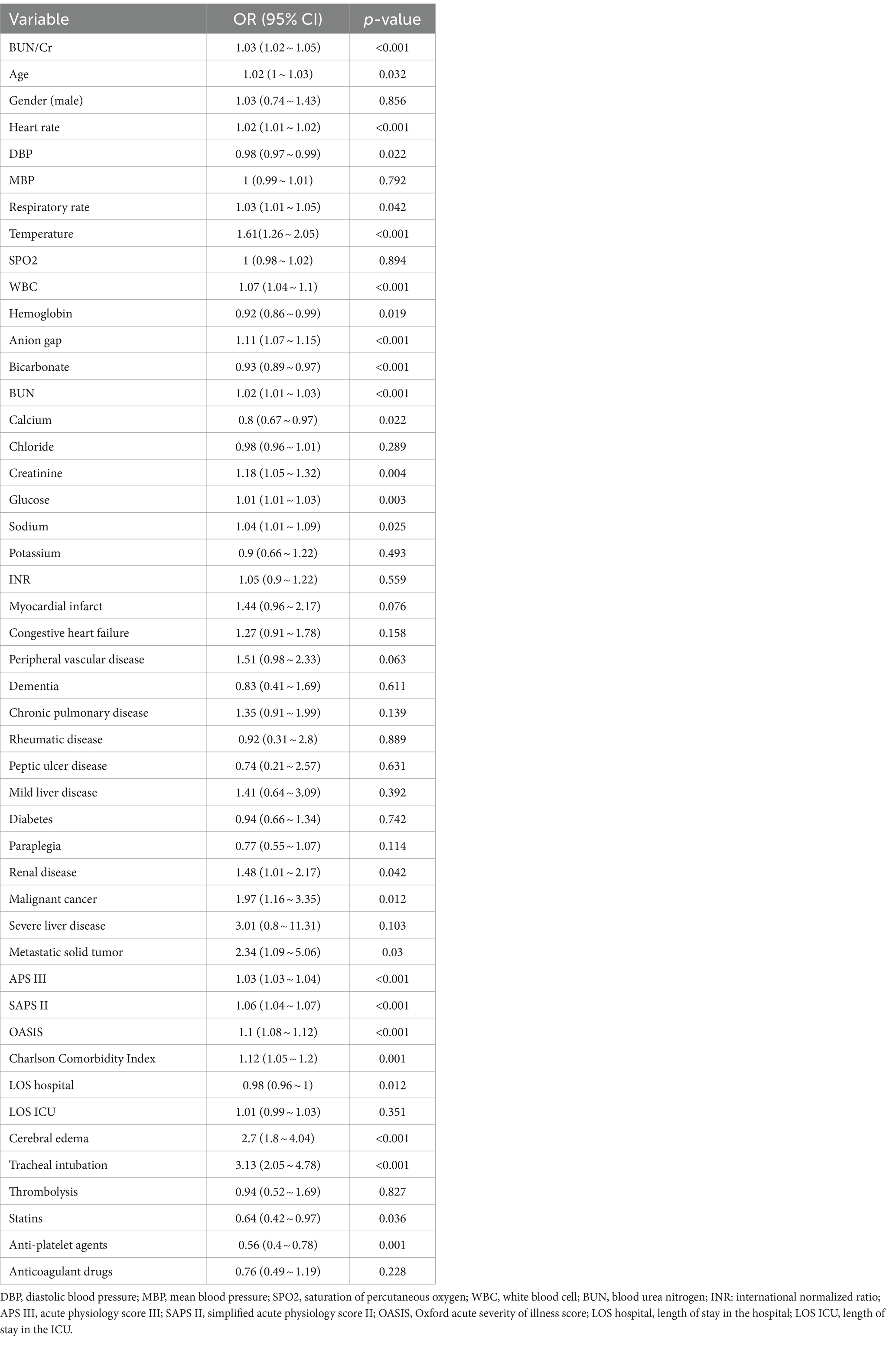
Table 2. Univariate logistic analysis between BUN/Cr and in-hospital mortality.
3.3 Effects of the BUN/Cr ratio and in-hospital mortalityTable 3 presents both unadjusted and adjusted models for the analysis. The multivariate logistic regression model, with the second trisection of BUN/Cr serving as the reference group, revealed a noteworthy positive association between elevated BUN/Cr levels, treated as a continuous variable, and a heightened risk of in-hospital mortality among patients diagnosed with AIS and coexisting AF. After adjusting for confounders, in-hospital mortality could increase by 26% for each standard deviation increase in a patient’s BUN/Cr (OR: 1.26, 95% CI: 1.04–1.53, p = 0.019). When we used BUN/Cr as a categorical variable, we found that there was a higher risk of in-hospital mortality in Group 1(Q1 > 17.2) and Group 3 (Q3 > 22.41) compared to Group 2 (Q2: 17.2–22.41). This suggests that patients with BUN/Cr levels above 22.41 may have an increased probability of experiencing in-hospital mortality relative to those who fall within the range of 17.2–22.41. However, BUN/Cr in Group 1 (Q1 < 17.2) was not significantly associated with in-hospital mortality (p = 0.493).
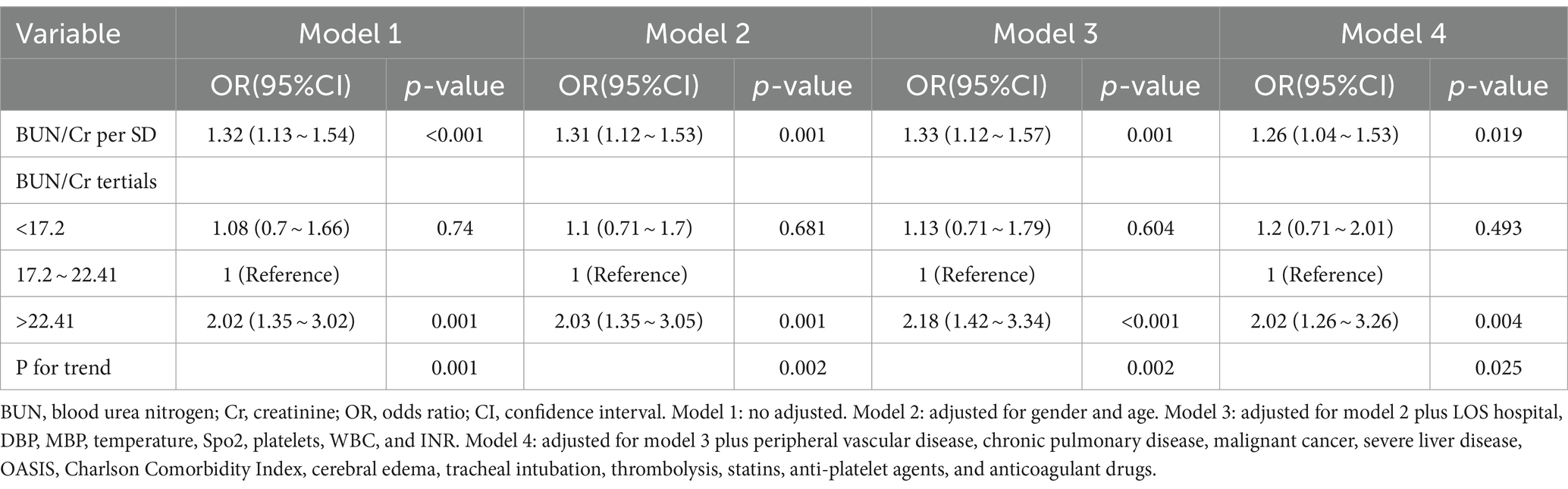
Table 3. Association between BUN/Cr and in-hospital mortality in multiple regression model.
In this study, we observed a non-linear relationship between BUN/Cr and patients with AIS combined with AF, and after adjusting for gender, age, LOS hospital, DBP, MBP, temperature, SPO2, platelets, WBC, INR, chronic pulmonary disease, malignant cancer, severe liver disease, peripheral vascular disease, OASIS, Charlson Comorbidity Index, cerebral edema, tracheal intubation, thrombolysis, statins, anti-platelet agents, and anticoagulant drugs, restricted cubic spline analysis showed a J-shaped association between BUN/Cr and in-hospital mortality (Figure 2, p = 0.027).

Figure 2. Adjusting factors included gender, age, LOS hospital, DBP, MBP, temperature, Spo2, platelets, WBC, INR, anion gap, peripheral vascular disease, chronic pulmonary disease, malignant cancer, severe liver disease, OASIS, Charlson Comorbidity Index, cerebral edema, tracheal intubation, thrombolysis, statins, anti-platelet agents, and anticoagulant drugs.
Based on our two-stage logistic regression analysis, we discovered an inflection point at 19.63 mg/dL for BUN/Cr (Table 4). There was no association between BUN/Cr levels (< 19.63 mg/dL) and in-hospital mortality in patients presenting with a combination of AIS and AF (p = 0.127), and specifically in patients with BUN/Cr > 19.63 mg/dL, there was a 4% rise in in-hospital mortality for each 1 mg/dL increase in BUN/Cr (OR: 1.04, 95% CI: 1.01–1.06, p = 0.012).
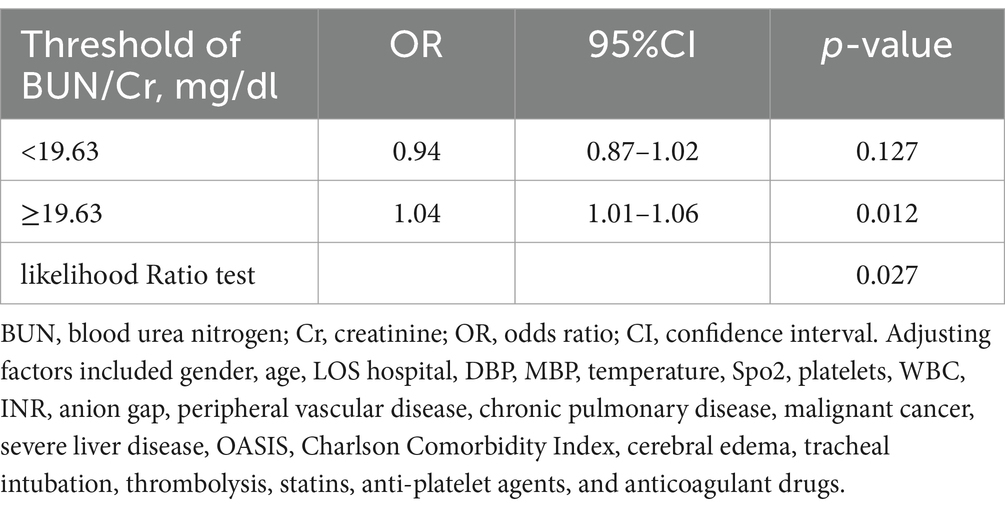
Table 4. Threshold analysis of BUN/Cr on in-hospital mortality using a two-segment regression model.
3.4 Subgroup analysisAs shown in Figure 3, we performed subgroup analyses to assess the relationship between BUN/Cr and in-hospital mortality. No significant interaction was observed after subgroup analyses based on confounders such as age (<75 and ≥ 75 years old), gender, peripheral vascular disease, COPD, malignant cancer, severe liver disease, cerebral edema, tracheal intubation, thrombolysis, statins, anti-platelet agents, and anticoagulant drugs (all p-values for interaction >0.05).
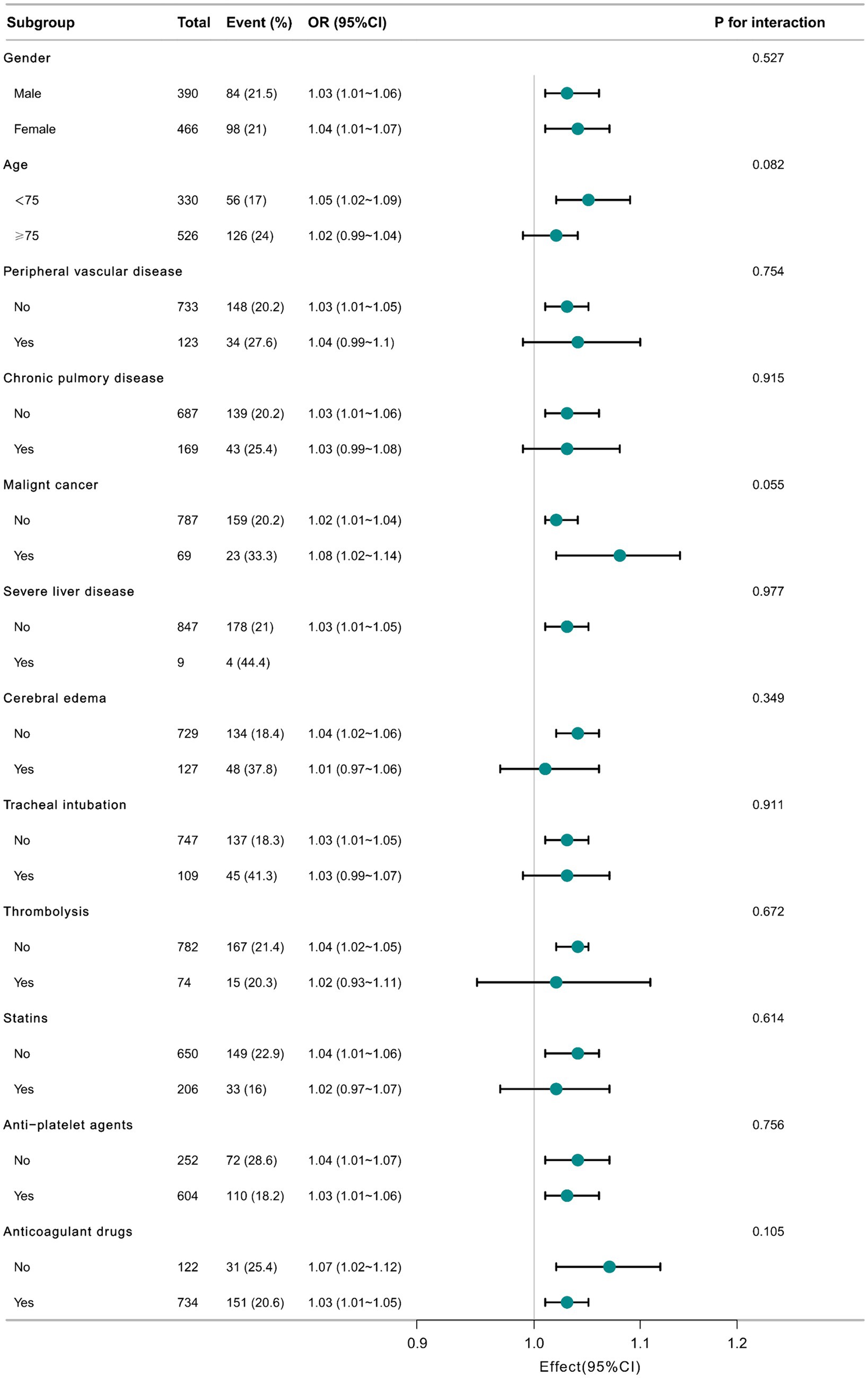
Figure 3. Relationship between BUN/Cr and in-hospital mortality in subgroup analysis.
4 DiscussionThrough multifactorial logistic regression modeling, our retrospective analysis revealed a positive correlation between BUN/Cr and in-hospital mortality among ischemic stroke patients with comorbid AF. Of particular interest, patients with higher BUN/Cr values exhibited increased risk of mortality.
The BUN/Cr ratio possesses considerable clinical utility due to its ease of acquisition and ability to serve as a marker for both neurohumoral activity and renal function. Literature preceding this study has consistently demonstrated the importance of BUN/Cr in prognosticating the likelihood of ischemic stroke occurrence. Akimoto et al. showed that the cause of the development of cerebral infarction may be due to the disproportionate increase in BUN/Cr in patients with cerebral infarction (19). Within the domain of AIS research, Deng et al. unearthed a compelling link between BUN/Cr and the occurrence of 3-month mortality, particularly evident in individuals with elevated HDL levels (20). In addition, Kunal Bhatia et al. elucidated the independent prognostic capacity of a BUN/Cr ratio surpassing 15 mg/dL in predicting neurological deterioration within the acute ischemic stroke population (21). Previous studies have examined the possibility that an increased BUN/Cr may be associated with a poorer prognosis in critically ill patients. Huang et al. reportedly found a non-linear correlation in patients with acute myocardial infarction, and according to the KM curve, the highest in-hospital mortality was observed when BUN/Cr ≥18.34 mg/dL (22). Furthermore, a research conducted by Zhu et al. performed a study involving 509 hospitalized individuals afflicted with acute heart failure. Their research elucidated that the BUN/Cr ratio could independently anticipate all-cause mortality, while a heightened BUN/Cr ratio was indicative of an adverse prognosis (23).
Recently, several studies have also identified a role for BUN/Cr as a prognostic factor in cardiovascular system disorders. Activation of the neurohormonal system, which inhibits the reabsorption of urea nitrogen, includes vasopressin, the renin-angiotensin-aldosterone system (RAAS), and the sympathetic nervous system. Thus, BUN/Cr, serving as a biomarker of neurohormonal activity, has exhibited associations with prognostic endpoints related to cardiac dysfunction (9, 24, 25). The measurement of BUN/Cr ratio has been found to provide valuable insights into the prognosis and outcomes of individuals with cardiac dysfunction. Its relationship with various prognostic endpoints highlights its potential as a useful biomarker for assessing cardiac health and predicting clinical outcomes in this context. A study by Qin et al. found that higher levels of urea nitrogen were associated with an increased incidence of atrial fibrillation in women. This finding adds to the evidence that urea nitrogen is also a risk factor for atrial fibrillation in older adults (26).
Stroke is globally recognized as the second most prevalent cause of mortality and a significant contributor to disability. Among different types of strokes, ischemic stroke stands out as the most frequent, constituting approximately 87% of all reported cases (27). Indeed, AF is widely recognized as a significant risk factor for ischemic stroke. It has been reported that more than 20% of ischemic stroke cases are attributable to cardiac thromboembolism resulting from atrial fibrillation (28). Furthermore, the prevalence of atrial fibrillation among stroke patients continues to rise annually. Individuals with atrial fibrillation may face an annual incidence rate of ischemic stroke reaching up to 18.2%, given the concurrent presence of diverse risk factors (29). It is true that strokes linked to atrial fibrillation are more likely to result in fatality or disability than strokes with other causes, and they have the highest in-hospital mortality rate among ischemic strokes (8). Moreover, prompt recognition and management of atrial fibrillation can help prevent thromboembolic events, which are strongly associated with the occurrence of stroke. Therefore, early detection and swift implementation of appropriate emergency interventions hold paramount significance for individuals affected by the combined occurrence of ischemic stroke and AF. These proactive measures are instrumental in minimizing the risks of disability and fatality.
The precise underlying mechanism linking BUN/Cr to in-hospital mortality in patients presenting with acute ischemic stroke and concomitant atrial fibrillation remains uncertain. In light of this uncertainty, we propose several potential mechanisms that may contribute to this association. BUN/Cr represents a vital metric for the evaluation of dehydration, and its significance is particularly noteworthy within the demographic of ischemic stroke patients. Given its association with a high likelihood of unfavorable outcomes upon hospital discharge, dehydration emerges as a prevalent occurrence among such individuals. Dehydration is known to decrease cerebral perfusion and disrupt neuroplasticity (30, 31), consequently exhibiting a correlation with recurrent embolic strokes and thrombotic events, including venous thromboembolism, subsequent to an acute stroke. The BUN/Cr ratio can provide insight into heightened dehydration levels and may serve as a valuable clinical marker for assessing the progression of an acute stroke. Furthermore, emerging evidence suggests a significant bidirectional correlation between the heart and the kidneys. On the one hand, diminished renal function can contribute to the development of atrial fibrillation through elevated RAAS activity, inflammation, and the promotion of cardiovascular conditions such as coronary artery disease (CHD) and heart failure. On the other hand, atrial fibrillation can be induced by RAAS activation, thromboembolism, hypoperfusion, inflammation, and the onset of other cardiovascular disorders (32). This intricate interplay underscores the complex relationship between these two vital organ systems. According to researchers, there is a suggestion that urea nitrogen could potentially serve as a marker for the “renal response” triggered by neurohormonal activation. Consequently, it may provide insights into the underlying pathophysiological processes associated with cardiovascular disease (CVD) (33). Engin Akgul et al. found that BUN and Cr levels were higher, respectively, in the postoperative AF group, suggesting that renal insufficiency (RI) paves the way for many other potentially life-threatening diseases in patients (34). At the same time, there is growing evidence indicating a potential association between BUN/Cr levels and oxidative stress as well as endothelial dysfunction in patients. These additional mechanisms could contribute to the observed relationship and shed further light on the underlying physiological processes.
Our investigation corroborates the aforementioned findings, where our current study demonstrates a curvilinear correlation between BUN/Cr and patients who exhibit acute ischemic stroke alongside comorbid atrial fibrillation. Notably, a J-shaped relationship was identified, signifying that heightened BUN/Cr values were linked to a heightened likelihood of in-hospital mortality among individuals diagnosed with AIS and AF, consistent with previous research findings on BUN/Cr. The BUN/Cr ratio is easily obtainable from clinical practice, and these observations serve to emphasize the substantial prognostic value of the BUN/Cr ratio within this particular cohort of patients, enabling timely identification of high-risk patients and the development of better treatment strategies.
4.1 Strengths and limitationsOur study possesses several notable strengths that contribute to advancing the current understanding in this field.
First, based on the information we have gathered so far, the present study is the first to reveal the association between BUN/Cr and in-hospital mortality in patients with AIS combined with AF. The findings derived from our investigation unveiled a non-linear relationship, specifically manifested as a J-shaped association, between BUN/Cr and in-hospital mortality. Notably, as BUN/Cr exceeded the threshold of 19.63 mg/dL, there was a gradual and progressive escalation in the risk of mortality. These findings may serve as a theoretical underpinning and provide supportive evidence for the therapeutic management of these patients.
Second, to discern the non-linear correlation between BUN/Cr and in-hospital mortality among individuals afflicted with AIS concomitant with AF, the methodology employed in this investigation encompassed the utilization of restricted cubic spline analysis.
Third, to improve statistical robustness and minimize the incidence of chance events, we used BUN/Cr as both a continuous and categorical variable. This approach improves the reliability of the final results through a more comprehensive analysis.
In addition, we undertook a threshold effect analysis to investigate the potential threshold value that may exist in the correlation between BUN/Cr and in-hospital mortality. We also conducted a subgroup analysis to examine the correlation between BUN/Cr and in-hospital mortality within specific subgroups.
Our study also has some limitations. First, the laboratory data utilized in this study were prospectively collected on the initial day of ICU admission; therefore, we were unable to analyze ongoing changes in the BUN/Cr ratio.
Second, despite controlling for certain known confounding factors, it is important to acknowledge that our study outcomes might have been influenced by other unmeasured or unidentified variables.
Third, it is essential to acknowledge that this study was conducted as a single-center retrospective analysis. Due to the limited study population to a specific country and intensive care unit, the representativeness of patients included is relatively poor, resulting in an inherent risk of selection bias that cannot be completely avoided. Due to the nature of retrospective studies, the sample size is relatively limited and there is confounding bias. However, we used multiple logistic regression analysis to correct for the effects of confounding factors, to improve the scientific validity of the research results. Nevertheless, further validation is required through multicenter prospective studies with larger sample sizes and longer time spans.
Fourth, it is important to note that while we can observe an association between BUN/Cr and in-hospital mortality, we cannot establish a direct causal relationship between the two variables. Nevertheless, there is substantial evidence indicating a statistically significant correlation between BUN/Cr and in-hospital mortality.
Fifth, due to limitations in the database itself, the study did not include specific criteria for patients to be admitted to the ICU and the most common causes of death in this group.
5 ConclusionIn this study, we observed that BUN/Cr within 24 h of admission to the ICU for patients with AIS combined with AF was J-shaped associated with in-hospital mortality. The risk of in-hospital mortality increases when the BUN/Cr ratio > 19.63 mg/dL. Therefore, more attention should be paid to patients with high BUN/Cr levels, who may have higher in-hospital mortality. This will benefit clinicians and contribute to better decision-making.
Data availability statementThe data analyzed in this study was obtained from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database, the following licenses/restrictions apply: to access the files, users must be credentialed users, complete the required training (CITI Data or Specimens Only Research) and sign the data use agreement for the project. Requests to access these datasets should be directed to PhysioNet, https://physionet.org/, doi: 10.13026/6mm1-ek67.
Ethics statementEthical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributionsBL: Conceptualization, Data curation, Formal analysis, Writing – original draft. JuaL: Data curation, Writing – review & editing. XM: Data curation, Writing – review & editing. SY: Data curation, Writing – review & editing. FT: Data curation, Writing – review & editing. XS: Data curation, Writing – review & editing. JunL: Supervision, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Tangshan Science Program Project (21130224C), the Hebei Medical Research Project (20221533), and the National College Student Innovation and Entrepreneurship Training Program (202310081031).
AcknowledgmentsWe would like to thank the Massachusetts Institute of Technology and Beth Israel Deaconess Medical Center for providing the MIMIC-IV database. The authors thank Dr. Liu Jie (People’s Liberation Army of China General Hospital, Beijing, China) for helping with the data availability statement.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Krishnamurthi, RV, Ikeda, T, and Feigin, VL. Global, regional and country-specific burden of Ischaemic stroke, intracerebral Haemorrhage and subarachnoid Haemorrhage: a systematic analysis of the global burden of disease study 2017. Neuroepidemiology. (2020) 54:171–9. doi: 10.1159/000506396
PubMed Abstract | Crossref Full Text | Google Scholar
2. Roth, GA, Johnson, CO, Nguyen, G, Naghavi, M, Feigin, VL, Murray, CJ, et al. Methods for estimating the global burden of cerebrovascular diseases. Neuroepidemiology. (2015) 45:146–51. doi: 10.1159/000441083
Crossref Full Text | Google Scholar
3. Turcato, G, Cappellari, M, Follador, L, Dilda, A, Bonora, A, Zannoni, M, et al. Red blood cell distribution width is an independent predictor of outcome in patients undergoing thrombolysis for ischemic stroke. Semin Thromb Hemost. (2017) 43:030–5. doi: 10.1055/s-0036-1592165
Crossref Full Text | Google Scholar
4. Wu, S, Wu, B, Liu, M, Chen, Z, Wang, W, Anderson, CS, et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. (2019) 18:394–405. doi: 10.1016/s1474-4422(18)30500-3
PubMed Abstract | Crossref Full Text | Google Scholar
5. Svennberg, E, Engdahl, J, Al-Khalili, F, Friberg, L, Frykman, V, and Rosenqvist, M. Mass screening for untreated atrial fibrillation: the Strokestop study. Circulation. (2015) 131:2176–84. doi: 10.1161/circulationaha.114.014343
PubMed Abstract | Crossref Full Text | Google Scholar
6. January, CT, Wann, LS, Calkins, H, Chen, LY, Cigarroa, JE, Cleveland, JC Jr, et al. 2019 Aha/Acc/Hrs focused update of the 2014 Aha/Acc/Hrs guideline for the Management of Patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Rhythm Society in collaboration with the Society of Thoracic Surgeons. Circulation. (2019) 140:e125–51. doi: 10.1161/cir.0000000000000665
PubMed Abstract | Crossref Full Text | Google Scholar
7. Bancroft, T, Lim, J, Wang, C, Sander, SD, and Swindle, JP. Health care resource utilization, costs, and persistence in patients newly diagnosed as having Nonvalvular atrial fibrillation and newly treated with dabigatran versus warfarin in the United States. Clin Ther. (2016) 38:545–556.e6. doi: 10.1016/j.clinthera.2016.01.008
PubMed Abstract | Crossref Full Text | Google Scholar
8. Vinding, NE, Kristensen, SL, Rørth, R, Butt, JH, Østergaard, L, Olesen, JB, et al. Ischemic stroke severity and mortality in patients with and without atrial fibrillation. J Am Heart Assoc. (2022) 11:e022638. doi: 10.1161/jaha.121.022638
PubMed Abstract | Crossref Full Text | Google Scholar
9. Murata, A, Kasai, T, Matsue, Y, Matsumoto, H, Yatsu, S, Kato, T, et al. Relationship between blood urea nitrogen-to-creatinine ratio at hospital admission and long-term mortality in patients with acute decompensated heart failure. Heart Vessel. (2018) 33:877–85. doi: 10.1007/s00380-018-1135-3
PubMed Abstract | Crossref Full Text | Google Scholar
10. Tanaka, S, Ninomiya, T, Taniguchi, M, Tokumoto, M, Masutani, K, Ooboshi, H, et al. Impact of blood urea nitrogen to creatinine ratio on mortality and morbidity in hemodialysis patients: the Q-cohort study. Sci Rep. (2017) 7:14901. doi: 10.1038/s41598-017-14205-2
PubMed Abstract | Crossref Full Text | Google Scholar
11. Schrock, JW, Glasenapp, M, and Drogell, K. Elevated blood urea nitrogen/creatinine ratio is associated with poor outcome in patients with ischemic stroke. Clin Neurol Neurosurg. (2012) 114:881–4. doi: 10.1016/j.clineuro.2012.01.031
PubMed Abstract | Crossref Full Text | Google Scholar
12. Matsue, Y, van der Meer, P, Damman, K, Metra, M, O'Connor, CM, Ponikowski, P, et al. Blood urea nitrogen-to-creatinine ratio in the general population and in patients with acute heart failure. Heart. (2017) 103:407–13. doi: 10.1136/heartjnl-2016-310112
PubMed Abstract | Crossref Full Text | Google Scholar
13. Zhen, Z, Liang, W, Tan, W, Dong, B, Wu, Y, Liu, C, et al. Prognostic significance of blood urea nitrogen/creatinine ratio in chronic Hfpef. Eur J Clin Investig. (2022) 52:e13761. doi: 10.1111/eci.13761
PubMed Abstract | Crossref Full Text | Google Scholar
14. Jiang, WF, and Deng, ML. Prognostic impact of blood urea nitrogen/creatinine ratio changes in patients with acute ischemic stroke. Clin Neurol Neurosurg. (2022) 215:107204. doi: 10.1016/j.clineuro.2022.107204
PubMed Abstract | Crossref Full Text | Google Scholar
15. Johnson, AEW, Bulgarelli, L, Shen, L, Gayles, A, Shammout, A, Horng, S, et al. Mimic-iv, a freely accessible electronic health record dataset. Sci Data. (2023) 10:1. doi: 10.1038/s41597-022-01899-x
PubMed Abstract | Crossref Full Text | Google Scholar
16. von Elm, E, Altman, DG, Egger, M, Pocock, SJ, Gøtzsche, PC, and Vandenbroucke, JP. The strengthening the reporting of observational studies in epidemiology (Strobe) statement: guidelines for reporting observational studies. Lancet. (2007) 370:1453–7. doi: 10.1016/s0140-6736(07)61602-x
Crossref Full Text | Google Scholar
17. Johnson, AE, Stone, DJ, Celi, LA, and Pollard, TJ. The Mimic code repository: enabling reproducibility in critical care research. J Am Med Inform Assoc. (2018) 25:32–9. doi: 10.1093/jamia/ocx084
PubMed Abstract | Crossref Full Text | Google Scholar
18. Yang, Q, Zheng, J, Chen, W, Chen, X, Wen, D, Chen, W, et al. Association between preadmission metformin use and outcomes in intensive care unit patients with Sepsis and type 2 diabetes: a cohort study. Front Med. (2021) 8:8. doi: 10.3389/fmed.2021.640785
PubMed Abstract | Crossref Full Text | Google Scholar
19. Akimoto, T, Ito, C, Kato, M, Ogura, M, Muto, S, and Kusano, E. Reduced hydration status characterized by disproportionate elevation of blood urea nitrogen to serum creatinine among the patients with cerebral infarction. Med Hypotheses. (2011) 77:601–4. doi: 10.1016/j.mehy.2011.06.044
Crossref Full Text | Google Scholar
20. Deng, L, Wang, C, Qiu, S, Bian, H, Wang, L, Li, Y, et al. Association between blood urea nitrogen-to-creatinine ratio and three-month outcome in patients with acute ischemic stroke. Curr Neurovasc Res. (2019) 16:166–72. doi: 10.2174/1567202616666190412123705
PubMed Abstract | Crossref Full Text | Google Scholar
21. Bhatia, K, Mohanty, S, Tripathi, BK, Gupta, B, and Mittal, MK. Predictors of early neurological deterioration in patients with acute Ischaemic stroke with special reference to blood urea nitrogen (bun)/Creatinine Ratio & Urine Specific Gravity. Indian J Med Res. (2015) 141:299–307. doi: 10.4103/0971-5916.156564
Crossref Full Text | Google Scholar
22. Huang, S, Guo, N, Duan, X, Zhou, Q, Zhang, Z, Luo, L, et al. Association between the blood urea nitrogen to creatinine ratio and in-hospital mortality among patients with acute myocardial infarction: a retrospective cohort study. Exp Ther Med. (2023) 25:36. doi: 10.3892/etm.2022.11735
PubMed Abstract | Crossref Full Text | Google Scholar
23. Zhu, X, Cheang, I, Liao, S, Wang, K, Yao, W, Yin, T, et al. Blood urea nitrogen to creatinine ratio and long-term mortality in patients with acute heart failure: a prospective cohort study and meta-analysis. Cardiorenal Med. (2020) 10:415–28. doi: 10.1159/000509834
留言 (0)