Dear Editor,
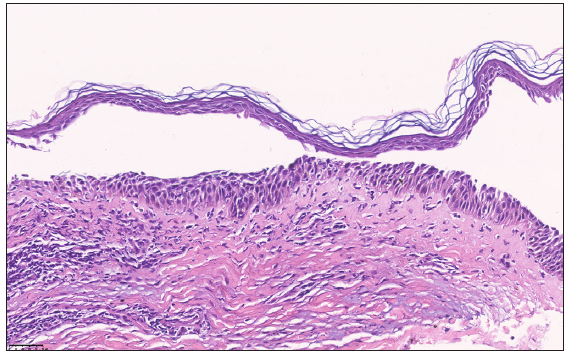
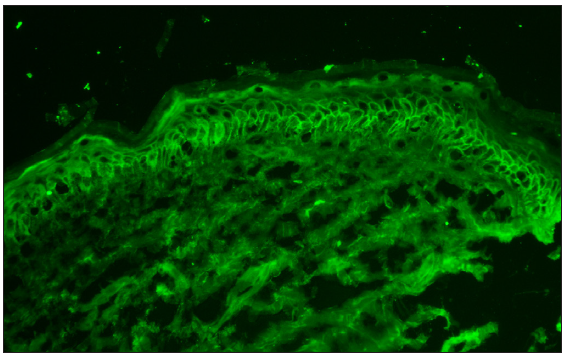
A 67-year-old otherwise healthy man presented with a 2-week history of mildly pruritic, erythema annulare centrifugum-like lesions involving the trunk and extremities. He had a medical history of pemphigus foliaceous (PF) localised on the chest since 5 years and had been irregularly taking oral prednisolone and topical clobetasol. The patient discontinued the treatment 6 months ago because he was worried about the side effects of corticosteroids. There were no identifiable inciting factors such as drug intake, recent infection or arthropod bite before the onset of the new lesions. Physical examination revealed an indurated, eroded, crusted plaque on the chest [Figure 1a]. Also, numerous demarcated, annular, erythematous plaques on the trunk and limbs were noted [Figures 1b and 1c]. There were no signs of mucous membrane involvement. An initial diagnosis of generalised tinea corporis was considered. However, a potassium hydroxide preparation of scrapings from the lesions was negative for fungal organisms. The results of laboratory studies, including full blood count, biochemistry, and antinuclear antibody profile were all within normal limits. Histopathological examination of a biopsy specimen taken from one of the erythema annulare centrifugum-like lesions showed mid-epidermal clefts containing acantholytic cells [Figure 2a]. Direct immunofluorescence on the normal-appearing perilesional skin revealed intercellular IgG and C3 staining in the epidermis [Figure 2b]. The ELISA test for anti-desmoglein autoantibodies was positive for desmoglein (Dsg)1 (74.0 U/mL, normal level<20) but negative for Dsg3. Taken together, a definitive diagnosis of erythema annulare centrifugum-like PF was established. The patient was prescribed oral prednisone 40 mg daily and topical mometasone furoate 1% cream. The erythema annulare centrifugum-like lesions disappeared completely and there was a partial clearance of the localised lesions on the chest after 4 weeks of treatment [Figures 3a and 3b].

Export to PPT

Export to PPT

Export to PPT
Export to PPT
Export to PPT

Export to PPT
PF is an acquired autoimmune vesiculobullous disorder that is characterised by granular layer acantholysis and antibodies to desmoglein 1 (Dsg1). Clinically, recurrent flaccid vesicles and bullae on an erythematous base are seen which are susceptible to rupture, resulting in crusted, scaling erosions.1 PF commonly presents with generalised involvement of the chest, back, and face. Rarely, it may be restricted to the initial site for a long period.2 Herein, we report a patient with previously localised PF on the chest, later developing new erythema annulare centrifugum-like lesions in which histology, immunofluorescence findings, and autoantibodies were compatible with PF.
Several cases have been described with an erythema annulare centrifugum-like clinical rash and direct immunofluorescence pattern compatible with pemphigus. The disease has been termed ‘erythema annulare centrifugum-like acantholytic dermatosis (EAAD)’ and some authors have proposed that it should be considered a novel acantholytic disease.3 However, Holahan HM et al. suggested EAAD may be a morphological variant of PF.4 Histopathologically, erythema annulare centrifugum-like PF or EAAD typically demonstrates subcorneal acantholysis or eosinophilic spongiosis without apparent acantholysis.4 Interestingly, the annular lesions of our patient showed mid-epidermal acantholysis. A similar case exhibiting erythema annulare centrifugum-like lesions accompanied by mid-epidermal acantholysis was documented and subsequently diagnosed as PF by immunoblotting.5 Thus, DIF staining pattern with intercellular deposition of IgG and C3 and ELISA identification of Dsg1 are essential for confirming the diagnosis.
Since a heterogeneous group of cutaneous diseases can present with erythema annulare centrifugum-like morphology, differential diagnoses are numerous and challenging. Diagnosis is made primarily by clinical and histological findings. In addition, other investigations such as microbiology and serology may be necessary to establish the cause of annular skin eruptions.
To the best of our knowledge, new erythema annulare centrifugum-like PF with previously localised PF has not been reported before. We also emphasise the importance of including PF in the differential diagnosis of erythema annulare centrifugum-like lesions.
留言 (0)