Dear Editor,
Obesity-associated lymphedematous mucinosis (OALM) is a relatively newly recognised entity resulting in pretibial mucinosis in obese individuals. It needs to be differentiated from other causes of pretibial mucinosis, particularly pretibial myxoedema, a feature of thyroid disease. Clinical findings, histopathological features, and laboratory workup can help to arrive at the correct diagnosis of this rare, under-recognised entity. So far, very few reports of OALM have been reported in English literature. We report two additional cases of this rare entity for the first time in Indian patients which were misdiagnosed clinically and on histopathology initially. Awareness of this entity is important to recognise this emerging lifestyle-related disease.
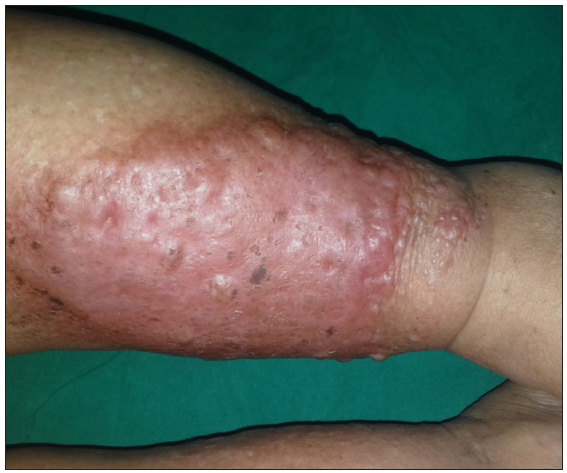
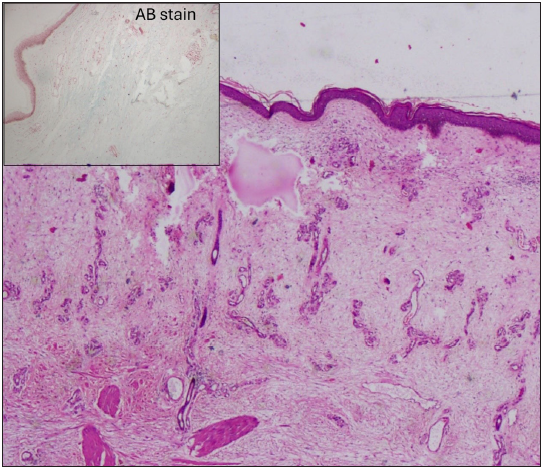
Case 1: A 70-year-old female, a known asthmatic and hypertensive, presented with a history of recurrent blisters of 3 years duration. On clinical examination, there were tense bullous lesions on the shin of the right leg that could not be ruptured, along with erythematous papules and nodules on an erythematous to oedematous skin [Figure 1a] and erythematous hyperpigmented papules on the right leg. A clinical differential diagnosis of pretibial bullous pemphigoid, inflammatory epidermolysis bullosa acquisita, and B-cell lymphoma leg type was made, and a biopsy was taken. Direct immunofluorescence was negative. Biopsy revealed an atrophic epidermis overlying oedematous fibromyxoid stroma with stellate fibroblasts and numerous vessels, and a histopathological diagnosis of cutaneous angiomyxoma was given [Figure 1b]. Alcian blue showed diffuse pale blue mucin deposition in the dermis. Due to discordance with clinical diagnosis, the case was discussed at a clinicopathological review meeting. After obtaining additional clinical information that the patient had a BMI of 40 kg/m2 and a thorough literature review, a final diagnosis of OALM was made.
Export to PPT
Export to PPT
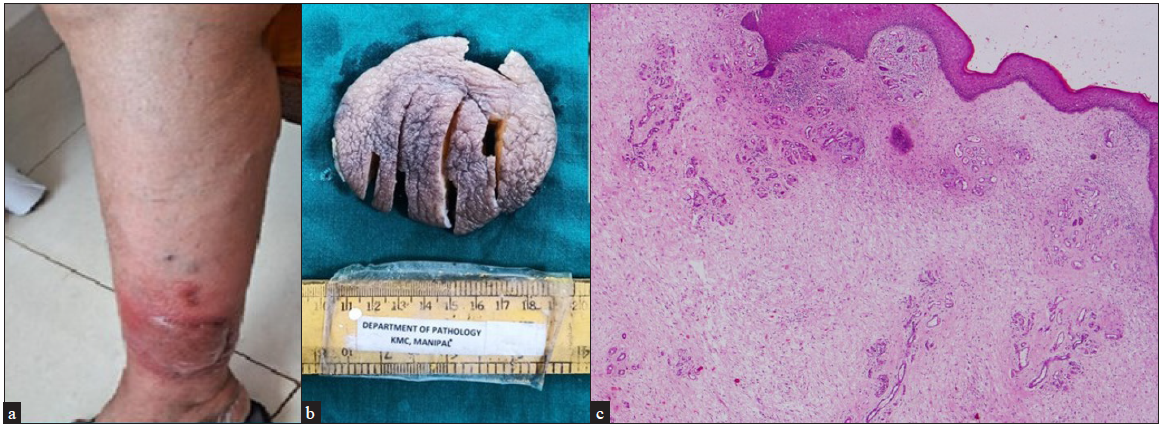
Case 2: A 74-year-old female with complaints of a lesion over the left leg of 2 years duration was referred to our surgery department for excision following a biopsy diagnosis of lymphangioma at an outside clinic. On clinical examination, an erythematous nodular plaque was noted on the left leg [Figure 2a]. No varicosities of veins in lower limbs were found. The excised plaque with an irregular nodular appearance measured 6×5.5×4 cm [Figure 2b]. Histopathological examination showed features similar to case 1 and focal acanthosis [Figure 2c]. No haemosiderin pigment deposition or extravasated RBCs were seen. A diagnosis of OALM was made after obtaining clinical information about the patient having a BMI of 35 kg/m2.
Export to PPT
Thyroid function tests in both patients were normal. Both patients were advised weight loss.
Pretibial mucin deposition is a characteristic feature of pretibial myxoedema seen in autoimmune thyroid disease, usually Graves’ disease. OALM and stasis mucinosis are conditions associated with the deposition of pretibial mucin in the absence of thyroid disease.1 Pretibial mucinosis occurring in obese patients was first described by Tokuda et al. in 2006 in the absence of thyroid disease, and the condition was named ‘Chronic obesity lymphedematous mucinosis.’2 Subsequently, Rongioletti et al. in 2009 described a series of five cases of similar condition and coined the term ‘Obesity-associated lymphedematous mucinosis’ and described the distinctive clinical and histopathological features.3 Subsequently, there are very few case reports described in the literature.4 It is characterised clinically by the presence of skin coloured to erythematous, semi-translucent papules and nodules that may progress to plaques on the legs bilaterally, particularly the shins, usually sparing the ankle and feet. Blisters may be seen occasionally. Histopathology shows mucin deposition in the superficial portion of the dermis, along with angioplasia with an increase in small blood and/or lymphatic vertically running vessels with linear or stellate fibroblasts.5
The pathogenesis of mucin deposition in OALM is hypothesised to be due to lymphatic stasis that occurs secondary to obesity, which is rich in protein-rich fluid, stimulating the production and deposition of mucin by fibroblasts.6 Also, ischaemia due to venous insufficiency results in hypoxia, which stimulates dermal fibroblasts to produce mucin. This entity may be misdiagnosed, as it is often under-recognised, as in both our cases, clinically and histopathologically. This is due to the lack of awareness of this entity. Because of the vascular proliferation and myxoid stroma, OALM can be confused with cutaneous angiomyxoma histologically.7Table 1 shows the clinical and histopathological features differentiating OALM, stasis mucinosis, pretibial myxoedema, and superficial angiomyxoma.1,2,7 Awareness of this under-recognised entity is important to avoid misdiagnosis and to institute appropriate therapy.
Table 1: Clinical and histopathological features differentiating Obesity associated lymphedematous mucinosis (OALM), stasis mucinosis, pretibial myxoedema, and superficial angiomyxoma
Obesity-associated lymphedematous mucinosis Pretibial myxoedema in thyroid disease Stasis mucinosis Superficial angiomyxoma Clinical features Appearance of lesionsSkin coloured to erythematous papules, nodules, plaques, and occasionally blisters on an oedematous to erythematous skin over the legs.
Ankle and feet are usually spared
Non-pitting oedema, plaques, and nodules on the anterior and lateral aspects of the legs
Dorsa of feet involved
Blue-violet, smooth, pebbly, and partially blanchable nodules and plaques, sometimes painful, overlying telangiectasia may be present. Asymptomatic solitary or multiple nodules in the head, neck, or trunk region Obesity + +/- +/- +/- Thyroid auto- antibodies - + - - Venous insufficiency +/- - + - Histopathological features Mucin depositionSuperficial: papillary and reticular dermis
Mild to moderate
Deep in the reticular dermis and subcutis
Abundant
Superficial, peri-eccrine, and around pilosebaceous units
Abundant
+, mucin pools in the reticular dermis and subcutis with a lobulated outline Epidermal changes Atrophy with effacement of rete ridges Hyper orthokeratosis, follicular plugging with acanthosis, and papillomatosis may be seen. It may be associated with eczema/ulceration of the skin Epidermoid cysts and nests of basaloid cells in 30% of cases Angioplasia upper dermis+, prominent
vertically running vessels are seen
_ +, mild Proliferation of small vessels Haemosiderin deposition +/- - +/- - Dermal fibrosis with collagen bundle separation +/- + +/- - Stellate/linear fibroblasts + + + +, plumper cells with eosinophilic cytoplasm may be seen Inflammatory infiltrate+/-
Perivascular, lymphocytes
+/- mast cells Absent Mixed inflammatory infiltrate with neutrophils
留言 (0)