A 57-year-old female presented with nausea, vomiting, and headache over a year. The patient had no specific complaints except for gradual weight loss over the past year. Computed tomography scan (CT) was done. T2-weighted sagittal images show an ill-defined T2 hyperintense cystic space occupying a lesion in the occipital lobe. There is ipsilateral compression of the occipital horn of the ventricle and disproportionate perilesional edema with midline shift [Figure 1a]. A craniotomy was performed on the suspicion of a glioma. Intraoperatively, the tumor was yellowish white non-vascular, and soft surrounded by viscous yellow fluid. The bits of tumor tissue sent for squash diagnosis were yellow, firm, and difficult to squash and spread. Rapid hematoxylin and eosin stain was performed.
Export to PPT
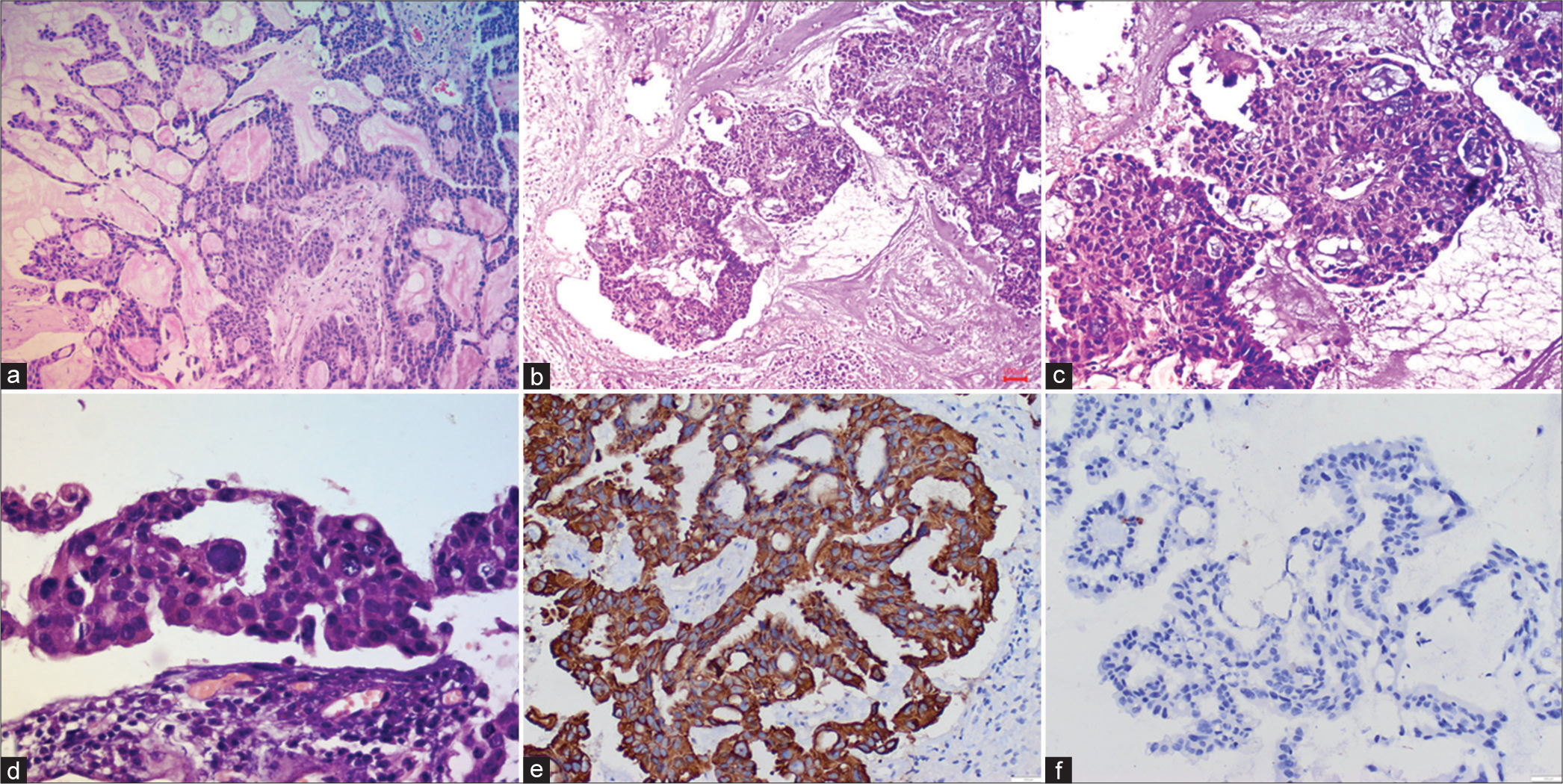
Definitive sections were sent for histopathology and immunohistochemical staining was done.
MORPHOLOGY QUIZWhat is the diagnosis based on the clinical history, imaging findings, and photomicrographs [Figure 1] provided?
Glioma
Meningioma
Metastatic carcinoma
Lymphoma
Which of the following immunohistochemical panels would be most useful for diagnosis?
CK7, CK20, TTF-1, GATA3, PAX-8, CDX2
CK7, CK20, Calretinin, WT1
IDH1/2, ATRX, P53
GFAP, Vimentin, NeuN
Answers1. (c) Metastatic carcinoma
2. (a) CK7, CK20, TTF-1, GATA3, PAX-8, and CDX2
EXPLANATIONSquash smear cytology is a rapid and reliable method for intraoperative diagnosis of inflammatory and neoplastic brain lesions.[1]
Squash smears were moderately cellular and showed cohesive clusters and glandular arrangement of tumor cells against a thin mucoid background [Figure 1b-c]. The tumor cells had round to oval hyperchromatic nuclei and a moderate amount of cytoplasm. A focus shows calcification. The findings were suggestive of a non-glial lesion, possibly metastases. Histopathology sections showed well-formed glands and sheets of tumor cells with pools of mucin and psammoma bodies confirming the diagnosis of metastatic adenocarcinoma [Figure 2a-d].
Export to PPT
The most common tumors leading to brain metastases include lung and breast followed by renal tumors. In the present case, the tumor cells showed strong immunopositivity for CK7 and were immunonegative for CK20 [Figure 2e and f]. In a female patient, CK7-positive and CK20-negative adenocarcinomas warrant the search for primary in the lung, breast followed by the uterus (endometrial), pancreas, and gallbladder.
ADDITIONAL QUIZ QUESTIONS3. Which of the following is the most common intracranial tumor?
Gliomas
Metastases
Meningioma
Lymphoma
4. Which of the following is a differential diagnosis of metastases to the brain?
Abscess
Parasitic infestation
Primary tumor-glioma/ependymoma
All of the above
Answers3. (b) Metastas es
4. (d) All of the above
EXPLANATIONThe differential diagnosis of metastases to the brain includes primary tumors of the brain, parasites, and abscesses.
Squash cytology smears of glial tumors are cellular with specific cytomorphological features of the tumor cells. For instance, the squash smears of low-grade gliomas show sparse cellularity of tumor cells in a fibrillary background in contrast to high-grade gliomas which are characterized by hypercellularity, endothelial proliferation, necrosis, and mitoses. Necrosis is also often noted in cases of brain abscess, characteristically described as liquefactive necrosis. Fungal, tubercular, and parasitic infestation can also show necrotic background.
BRIEF REVIEW OF TOPICMetastases to the brain are a known complication in approximately 20% of malignancies.[2] Brain metastases are often detected in CT and magnetic resonance imaging scans and previously known cases of malignancy during routine investigations. In most cases, metastases travel through the hematogenous route from lung tumors, breast carcinomas, renal cell carcinomas, and melanomas by breaching the blood–brain barrier.[3] Metastases are usually noted as intra-axial, intraparenchymal masses with a varied range of radiological differential diagnoses including gliomas, abscesses, and infections. Furthermore, in approximately 15% of cases, a primary tumor is not found.[4] In the index case, in the absence of any specific complaints elsewhere and a mass lesion in the brain, the suspicion of metastases was unlikely on clinical and radiological examination.
These cases are challenging and the surgeon relies on intraoperative diagnosis for immediate surgical management. In such scenarios, squash cytology can be reliably used to differentiate between metastatic from primary central nervous system neoplasms.
The squash smear cytomorphology depends on the type of primary tumor (adenocarcinoma, small cell carcinomas, melanoma, lymphoma, etc.). An algorithmic approach and workup with immunohistochemical markers can be useful for the detection of the primary tumor.
Immunohistochemical panel for morphologically designated adenocarcinoma of unknown primary involves the cytokeratin status (CK7 and CK20). Further organ-specific markers can be tested after analysis of CK7 and CK20 expression.[5]
In the index case, CK7 immunopositivity was found; however, the patient was lost to follow-up and further markers were not done.
Extensive radiological examination and accurate subtyping of the primary tumor enable the pathologist to choose the apt immunohistochemistry marker panel and document the origin of the tumor.
SUMMARYThe awareness of metastatic carcinoma as a differential diagnosis on cytology and identification of cytomorphological features can guide the surgeon and management of the patient.
留言 (0)